Abstract
Objective
To repeat and update our previous evaluation (2005) of Europe’s national pandemic influenza preparedness plans and assess the progress that has been made.
Methods
We assessed published national pandemic influenza preparedness plans from the European Union countries, from the two acceding countries (Bulgaria and Romania) and from Norway, Switzerland and Turkey. Plans were eligible for inclusion if formally published before 30 September 2006. We referred to WHO guidelines and used a systematically applied data extraction form. We considered plans in relation to border control measures, antiviral drugs and vaccines.
Findings
Twenty-nine countries had plans that were included in the analysis, compared with 21 countries in 2005. Substantial differences existed in countries’ plans for border control measures, and many plans diverged from WHO guidelines. Likewise, countries’ plans on antiviral drugs and vaccines varied and operational planning remained weak.
Conclusion
Although progress has been made in the completeness of plans, problems remain unsolved regarding national plans’ divergence from international recommendations, persisting strategic incoherence and operational limitations in relation to potentially scarce resources. Border control plans also show gaps and inconsistencies, and these are likely to be politically volatile during a pandemic.
Résumé
Objectif
Renouveler et mettre à jour notre précédente évaluation (2005) des plans nationaux européens de préparation à la grippe pandémique et évaluer les progrès réalisés.
Méthodes
Nous avons évalué les plans nationaux de préparation à la grippe pandémique publiés par les pays de l’Union européenne, par deux pays en voie d’accession à l’UE (Bulgarie et Roumanie) et par la Norvège, la Suisse et la Turquie. Pour être inclus dans l’étude, les plans devaient avoir été formellement publiés avant le 30 septembre 2006. Nous nous sommes référés aux recommandations de l’OMS et nous avons utilisé un formulaire d’extraction des données systématiquement appliqué. Nous avons examiné le contenu des plans en ce qui concerne les contrôles aux frontières, les antiviraux et les vaccins.
Résultats
Les plans de vingt-neuf pays ont été inclus dans l’analyse contre vint-et-un en 2005. Ces plans présentaient des différences substantielles à propos des mesures de contrôle aux frontières et beaucoup d’entre eux s’écartaient des recommandations de l’OMS. De même, le volet médicaments antiviraux et vaccins des plans était traité de manière variable et le volet planification opérationnelle restait peu développé.
Conclusion
Malgré les progrès réalisés en matière de complétude, il reste à résoudre des problèmes de divergence des plans avec les recommandations internationales, d’incohérence persistante sur le plan stratégique et de limitation de la planification opérationnelle, en relation éventuellement avec un manque de moyens. En ce qui concerne les contrôles aux frontières, les plans présentent aussi des lacunes et des incohérences et sont susceptibles d’être modifiés en fonction de considérations politiques pendant une pandémie.
Resumen
Objetivo
Repetir y actualizar nuestra evaluación anterior (2005) de los planes nacionales de preparación para una gripe pandémica elaborados en Europa y determinar los avances conseguidos.
Métodos
Se evaluaron los planes nacionales de preparación para una gripe pandémica publicados en los países de la Unión Europea, en los dos países en fase de adhesión (Bulgaria y Rumania) y en Noruega, Suiza y Turquía. El requisito para incluir los planes era que hubiesen sido publicados oficialmente antes del 30 de septiembre de 2006. Empleamos como referencia directrices de la OMS y utilizamos un formulario de obtención de datos que se aplicó sistemáticamente. Los planes fueron analizados en relación con las medidas de control fronterizo, los medicamentos antivirales y las vacunas.
Resultados
Veintinueve países disponían de planes que fueron incluidos en el análisis, en comparación con 21 países en 2005. Se observaron diferencias sustanciales entre los planes de los países en lo relativo a las medidas de control fronterizo, y muchos de los planes se apartaban de las directrices de la OMS. Diferían también entre los países los planes referentes a los antivirales y las vacunas, y la planificación operacional seguía siendo deficiente.
Conclusión
Aunque los planes son ahora más completos, siguen sin resolver los problemas que entrañan la divergencia de los planes nacionales respecto a las recomendaciones internacionales, la persistente incoherencia estratégica y las limitaciones operacionales asociadas a unos recursos potencialmente escasos. Los planes de control fronterizo muestran también lagunas e incongruencias, y probablemente serán políticamente volátiles en caso de pandemia.
ملخص
Abstract
الەدف
إعادة وتحديث التقيـيم الذي أجراە الباحثون عام 2005 للخطط الوطنية الأوروبية للتأەُّب للأنفلونزا الجائحية ولتقيـيم التقدُّم الـمُحْرز.
الطريقة
قيَّم الباحثون الخطط الوطنية المنشورة الخاصة بالتأەُّب للأنفلونزا الجائحية من بلدان الاتحاد الأوروبي، من البلدَيْن المنضمَّين حديثاً للاتحاد (بلغاريا ورومانيا)، ومن النرويج وسويسرا وتـركيا. وقد كانت الخطط قابلة للإدماج في الدراسة إذا كانت قد نشرت رسمياً قبل 30 أيلول/سبتمبر 2006. وقد رجع الباحثون إلى الدلائل الإرشادية لمنظمة الصحة العالمية واستخدموا طريقة منەجية لاستخلاص المعطيات. وقد أخذوا في الحسبان الخطط المتعلقة بإجراءات المكافحة على الحدود والأدوية المضادة للفيروسات واللقاحات.
الموجودات
لقد كان لدى 29 بلداً خطط أدمجت في التحليل، بالمقارنة مع 21 بلداً في عام 2005. وقد كانت ەناك اختلافات جوەرية بين خطط البلدان لإجراءات المكافحة على الحدود، وكان الكثير من الخطط بعيدا عن الدلائل الإرشادية لمنظمة الصحة العالمية. وبالمثل، فإن خطط البلدان المتعلقة بالأدوية المضادة للفيروسات وباللقاحات كانت متفاوتة وكان التخطيط الميداني لايزال ضعيفاً.
الاستنتاج
رغم أن ەناك تقدُّماً قد أُحرز في استكمال الخطط، فلاتزال ەناك مشكلات تحتاج للحل فيما يتعلق بابتعاد الخطط الوطنية عن التوصيات الدولية، واستمرار التنافر في الاستـراتيجيات والقيود التشغيلية في ما يتعلق بندرة الموارد المحتملة. كما اتضح أن خطط المكافحة على الحدود تعاني من الثغرات والتناقضات، وأنەا قد تەدد بحدوث توتـر سياسي أثناء الجائحة.
Introduction
With the emergence of the H5N1 avian influenza virus in Asia and outbreaks on the European continent and elsewhere, concerns about a human influenza pandemic are growing. In April 2005, WHO expressed concern about the general lack of global preparedness for pandemic influenza,1 and updated its 1999 global influenza preparedness plan to outline the components that each country’s plan should include to ensure an effective response.2 The Ministerial Meeting and Donor Conference that took place on 6–8 December 2006 in Bamako, Mali, drew attention to the urgent need for international organizations and the donor community to share emerging good practices, notably those coming from Europe, in order to guide the global response.3
In 2005, WHO published a checklist to facilitate preparedness planning. Its aim was to maintain essential services, to reduce disease transmission and the socioeconomic consequences of a pandemic and to minimize cases, hospitalizations and deaths.4 The European Commission (EC) updated its planning in line with the revised WHO definitions of pandemic phases and the creation of the European Centre for Disease Prevention and Control (ECDC). A subsequent WHO document2 urged every country “to develop or update a national influenza preparedness plan” and suggested that “each national authority should play its part towards achieving the international harmonization of preparedness measures”.
We previously analysed European national strategic preparedness plans for pandemic human influenza published before November 2005. This study’s findings showed considerable variation between different countries’ plans, and important gaps in many.5 These differences and gaps included border control issues, antiviral drugs and vaccines – all issues that are likely to test health systems’ responses because of scarce resources or the need for international coordination, coherence and cooperation. During the Austrian Presidency of the European Union (EU), January to June 2006, these issues were predicted to be particularly politically sensitive by policy-makers. We repeated our evaluation of national preparedness plans in Europe to assess progress made between November 2005 and November 2006, and analyse these three important strategic planning elements.
Methods
We sought plans from the 25 EU countries, the two acceding countries (Bulgaria and Romania), and three non-EU countries (Norway, Switzerland and Turkey). We evaluated each plan by methods similar to those described above, using the WHO checklist4–6 but expanding our assessment of the three areas of strategic interest.2,7,8 Plans in the public domain were identified and sourced through the ECDC, WHO, internet-based searches and countries’ health ministries. Plans were eligible for inclusion if formally published before 30 September 2006. All plans not available in either English or French were translated into English by public health specialists fluent in the original language. We assessed national strategic plans and, where clear links were documented, national operational plans.
A data extraction tool was designed, piloted, modified and finalized. We selected variables with particular reference to WHO guidelines on vaccines, antiviral drugs and border control, and used 142 criteria to assess plans. We also recorded priority populations for antiviral drugs and vaccines, whether the sizes of populations were defined (and if so, what these sizes were) and whether certain populations were ranked more highly than others in terms of favoured access. We recorded antiviral stockpile sizes if mentioned. Preparedness plans were scored independently by two researchers; where differences arose, agreement was reached through review and discussion.
Results
We identified 29 plans from a range of sources (Table 1, available at: http://www.who.int/bulletin/volumes/85/12/06-039834/en/index.html). We translated 12 plans into English. Overall scores for key pandemic preparedness criteria concerned with border control, vaccine policies and antiviral policies are presented in Figs. 1, 2 and 3.
Table 1. European national preparedness plans for pandemic human influenza.
| Country | Date of plan | Length (pages) | Original language | Source | Websites | Documents |
||
|---|---|---|---|---|---|---|---|---|
| Strategic plan | Operational plan | Plan with elements of both | ||||||
| Austria | September 2005 | 76 | German | ECDC website (direct link) | http://www.bmgf.gv.at/cms/site/attachments/3/6/8/CH0019/CMS1126084167391/pandemieplanh3neu.pdf | – | – | Yes |
| Belgium | July 2006 | 52 | French | ECDC website (via MoH website) | http://www.influenza.be | – | – | Yes |
| Bulgaria | October 2006 | 100 | English | UNDG website (direct link) | http://www.undg.org/documents/7926-Bulgaria_National_Influenza_Plan.pdf | – | – | Yes |
| Cyprus | September 2005 | 96 + 11 (tabulated appendices) | Greek | ECDC website (via MoH website) | http://www.moh.gov.cy/moh/moh.nsf/All/4CCD90ECED95DD174225718800218F00?OpenDocument | – | – | Yes |
| Czech Republic | April 2004 | 53 | English | WHO web (direct link) | http://www.who.int/csr/disease/influenza/nationalpandemic/en/index.html | – | – | Yes |
| Denmark | April 2006 | 57 + 97 (appendix) | Danish | ECDC website (via MoH website) | http://www.sst.dk/Forebyggelse/Sygdomsforebyggelse_og_vaccination/Smitsomme_sygd/Influenza/Pandemiberedskab.aspx?lang=da | – | Yes (appendix) | Yes |
| Estonia | March 2006 | 55 | Estonian | ECDC website (direct link) | http://www.sm.ee/est/HtmlPages/Sotsiaalministeeriumigripipandeemiaksvalmisolekuplaanaprill2006a/$file/Sotsiaalministeeriumi%20gripipandeemiaks%20valmisoleku%20plaan%20aprill%202006%20a.doc | – | – | Yes |
| Finland | 2006 | 202 | Finnish | WHO Regional Office for Europe Website (direct link) | http://www.euro.who.int/flu/related/20060822_1 (WHO web page) http://www.stm.fi/Resource.phx/publishing/documents/6425/index.htx (plan location) | – | – | Yes |
| France | January 2006 | 68 | French | ECDC website (direct link) | http://www.grippeaviaire.gouv.fr/IMG/pdf/Plan_pandemie_grippale_janvier_2006.pdf http://www.sante.gouv.fr/dossiers/grippe_aviaire/fiches_techniques.htm (Appendices, accessed 31/08/06) | – | Yes (appendices) | Yes |
| Germany | March 2005 | 90 (in 3 parts) | German | ECDC (via MoH website) | http://www.rki.de/cln_011/nn_879788/DE/Content/InfAZ/I/Influenza/Influenzapandemieplan.html | – | – | Yes |
| Greece | October 2005 | 44 | English | ECDC website (via MoH website) | http://www.keel.org.gr/keelpno/National_plan.pdf | – | – | Yes |
| Hungary | October 2005 | 22 | English | MoH website | http://www.eum.hu/index.php?akt_menu=2652&hir_reszlet=8 | – | – | Yes |
| Ireland | 2002 | 119 | English | Fluwiki (via MoH website) | http://www.fluwikie.com/pmwiki.php?n=Geographic.Ireland (Fluwiki web page) http://www.dohc.ie/publications/influenza_pandemic.html (MoH web page) | – | – | Yes |
| Italy | 2006 | 32 | English | ECDC (direct link) | http://www.ccm.ministerosalute.it/imgs/C_17_pubblicazioni_511_allegato.pdf | – | – | Yes |
| Latvia | October 2005 | 16 | Latvian | ECDC (direct link) | http://phoebe.vm.gov.lv/faili/gripa/info_20051018.pdf | – | – | Yes |
| Lithuania | September 2005 | 7 | English | ECDC (direct link) | http://www.vvspt.lt/aktai/gripas/2005%2009%2020%20GRIPO%20PLANO%20VERT.doc | – | – | Yes |
| Luxembourg | July 2006 | 24 (in 2 parts) | French | ECDC (via MoH website) | http://www.grippeaviaire.public.lu/ | – | Yes | – |
| Netherlands | October 2005 | 59 + 246 (appendices) | Dutch | WHO Regional Office for Europe Website (via MoH website) | http://www.euro.who.int/flu/related/20060822_1 (WHO web page) http://www.infectieziekten.info/index.php3?lokatie=http%3A//www.infectieziekten.info/protocol.php3%3Fpagid%3D142 (MoH web page) | Yes | Yes | Yes |
| Norway | February 2006 | 145 + appendices | Norwegian | Fluwiki (direct link) | http://www.fluwikie.com/pmwiki.php?n=Geographic.Norway | Yes | Yes | – |
| Poland | August 2005 | 80 | English | UNDG website (direct link) | http://www.undg.org/content.cfm?id=1575 | – | – | Yes |
| Portugal | January 2006 | 23 | Portuguese | ECDC (direct link) | http://www.dgs.pt/upload/membro.id/ficheiros/i007770.pdf | – | – | Yes |
| Romania | October 2005 | 23 | Romanian | MoH contacted in person | Not applicable (paper copy obtained) | – | – | Yes |
| Slovakia | November 2005 | 103 | English | ECDC (via MoH website) | http://www.health.gov.sk/redsys/rsi.nsf/0/D2869A65B5F83280C12570EC00517352?OpenDocument | – | – | Yes |
| Slovenia | July 2006 | 66 | Slovenian | Ministry of Health, Slovenia | Yes | |||
| Spain | May 2005 | 43 | English | ECDC (direct link) | http://www.msc.es/ciudadanos/enfLesiones/enfTransmisibles/docs/PlanGripeIngles.pdf | Yes | – | – |
| Sweden | November 2005 | 23 + 32 | Swedish | ECDC (via MoH website) | http://www.socialstyrelsen.se/Publicerat/2005/8972/2005-130-7.htm http://www.socialstyrelsen.se/Publicerat/2005/8660/2005-131-7.htm http://www.socialstyrelsen.se/Publicerat/2005/8662/2005-130-2.htm | – | – | Yes |
| Switzerland | May 2006 | 249 (in 3 parts) | French | MoHweb | http://www.bag.admin.ch/influenza/01120/01134/index.html?lang=fr | Yes (parts 1 and 2) | Yes (part 3) | – |
| Turkey | June 2006 | 184 | English | ECDC (direct link) | http://www.grip.saglik.gov.tr/eng/index.html | – | – | Yes |
| United Kingdom | October 2005 | 177 | English | ECDC (direct link) | http://www.dh.gov.uk/assetRoot/04/12/17/44/04121744.pdf (Department of Health plan); http://www.hpa.org.uk/infections/topics_az/influenza/pandemic/documents/HPAPanFluContPlanSept06.pdf (UK Health Protection Agency Plan) | – | – | Yes |
MoH, Ministry of Health; ECDC, European Centre for Disease Prevention and Control; UNDG, United Nations Development Group.
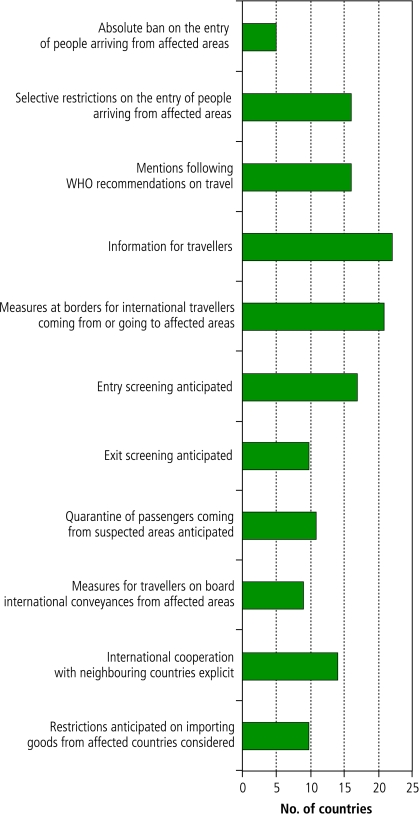
Fig. 1.
Border control measures mentioned in European national preparedness plans, by number of countries
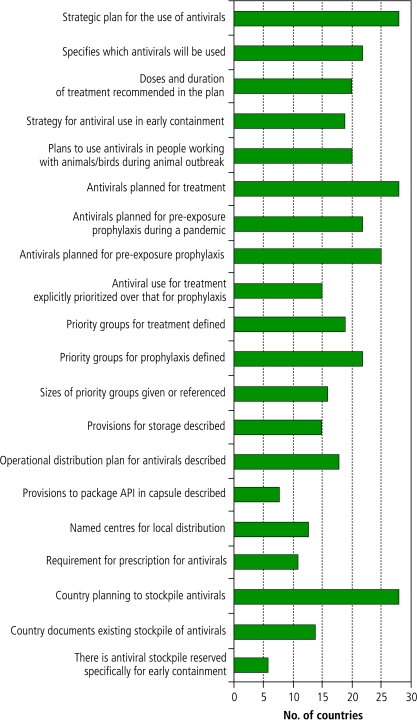
Fig. 2.
Vaccine strategy measures mentioned in European national preparedness plans, by number of countries
Fig. 3.
Antiviral drug strategy measures mentioned in European national preparedness plans, by number of countries
API, active pharmaceutical ingredient.
Border control
Strategic planning in relation to border control varied in terms of completeness of issues considered and approaches discussed (Fig. 1). Travel restrictions, for example, were anticipated by 16 countries, whereas two countries explicitly advised against such measures. Notably, five countries envisaged an absolute ban on cross-border travel, while 16 countries expressed an intention to follow WHO travel advice. Only a minority of plans detailed the legal foundation for possible restriction of cross-border population movements.
The need for information and guidance on travel was widely acknowledged. However, planning for implementation of travel-related public health measures was less coherent. Many countries diverged from WHO guidance; for example, 17 countries favoured the introduction of specific entry screening measures.9 Two countries planned to use thermal screening, and four planned to screen for symptoms. Although WHO guidance favours exit screening over entry screening, only 10 countries planned to implement exit screening.
Only nine countries had plans that addressed how travellers on board international conveyances from affected areas would be managed. Eight recommended separating sick travellers from others, and four aimed to provide masks to passengers, crew members or both. Border quarantine was advocated by 11 countries, mostly for travellers en route from an affected area, but most acknowledged that this strategy would be limited in scope. Thirteen countries addressed the issue of imported goods during a pandemic, with most referring to restrictions on poultry imports.
Only about half of the countries explicitly planned to coordinate their strategies with those of neighbouring countries.
Vaccines
All but one country had plans for pandemic vaccination; Fig. 2 highlights the key issues of these plans. Broadly, plans included details on sourcing vaccines, on which populations should be vaccinated first and on provisions to distribute and administer vaccine. Eighteen countries stated explicitly that they planned to vaccinate their whole population. Only three countries did not stipulate groups to be given priority when vaccine is in short supply.
The definition of priority groups was broadly consistent, with health-care workers named as a priority group in 26 countries. “Essential” workers were given priority in 23 countries, and 19 countries prioritized older people and populations at risk of serious complications. In practice the groups given highest priority were health-care workers in 16 countries, essential workers in four countries and people at risk of serious complications in three countries. Eight countries that defined priority groups for vaccination did not rank them explicitly. Sixteen countries estimated the size of priority groups. Some plans specifically prioritized vaccination of children, employees and people thought likely to pose a risk to vulnerable groups. Most plans explicitly prioritized groups in order to maintain health-care services and societal functions and to protect those at highest risk of death, yet the ethical reasoning for priority-setting was rarely explicit (Box 1).
Box 1. Ethics and priority-setting.
An influenza pandemic will raise many ethical challenges, including allocation of scarce resources and the needs to balance individual freedom against the common good, economic losses against the need to contain the disease, and health workers’ duty to provide care against self-interest.a,b Although national preparedness plans provide an important opportunity for transparent communication with the public, most of those examined for this analysis failed to discuss these issues. Plans usually stated that their goal was to decrease morbidity and mortality and ensure that society still functions. However, the lack of ethical reasoning, especially regarding resource allocation, might cause confusion when policies and practices need to be justified to an anxious population.
Finland and Norway discussed ethical concerns and expressed differing views. The Finnish plan suggested that beyond early containment of the disease, “long-term preventative medication with antivirals of essential personnel would not be justifiable and would create a feeling of unfairness within the population”. The Norwegian plan stated that “health care personnel who are continually exposed to the disease [should] receive the highest priority because they are crucial in providing care for a greater number of patients and because they have a higher risk of being infected.”
Vaccination strategies revealed important gaps. A minority of plans referred to or included operational guidelines for factors such as provisions for vaccine storage, distribution mechanisms and vaccine administration. Only three countries referred to existing generic plans for mass vaccination. Nine countries described how vaccine will be delivered to priority groups, including four that stated the need for local administrations to determine in advance which individuals should be vaccinated first. Few details were provided on who would be responsible for vaccination and where it would be done.
The plans of Belgium, France, Germany, Hungary, Italy, the Netherlands, Romania and the United Kingdom stated that these countries are capable of manufacturing vaccine. Four countries (Denmark, Norway, Sweden and Switzerland) intended to develop vaccine production capacity. Twenty-one countries planned to secure vaccine pre-purchase agreements, and four countries said such agreements were already in place. Five explicitly indicated that they have arranged to buy H5N1 vaccine; two countries, Finland and Switzerland, had placed orders for vaccine to cover their entire population.
Antiviral drugs
Although most countries had antiviral strategies, these varied considerably (Fig. 3). All countries but one advocated the use of antiviral drugs for treatment. Although treatment was generally clearly defined, use of antivirals for prophylaxis was less so. For some plans, distinctions between pre-exposure and post-exposure prophylaxis often were not clear. Just over half of the countries planned to supply antivirals for early containment, and 20 recommended specific treatment and prophylaxis strategies for animal workers. Five countries anticipated a need to supply antiviral drugs to their citizens abroad.
Plans for dosage and duration for treatment and prophylaxis were generally consistent with manufacturers’ recommendations. Twenty-two countries specified which antivirals they intended to use, with half advising the possible use of M2-membrane protein inhibitors (amantadine and rimantadine) in addition to neuraminidase inhibitors (oseltamivir and zanamivir) for prophylaxis or as a second-line drug.
Treatment was explicitly given priority over prophylaxis by 15 countries, which mostly outlined plans for antiviral use according to WHO pandemic phase. They noted that in phase 6, prophylaxis probably will not be feasible and might result in drug resistance. The other countries did not distinguish between use of antivirals for treatment and prophylaxis.
Priority groups for antiviral treatment were stated by 19 countries, 16 of which indicated the size of these groups. Seventeen countries planned to treat patients at the greatest risk of complications. Patients with severe disease and complications were top-priority in eight countries, while health-care workers were top-priority in two countries. France and Switzerland suggested that they had sufficient stockpiles to treat all patients.
Twenty-two plans advised offering pre-exposure prophylaxis; of these, 21 suggested health-care workers as recipients, and 17 suggested essential workers. Only 12 countries explicitly ranked priority groups for prophylaxis. Some plans discouraged seasonal use of antivirals because this would rapidly deplete stockpiles. Norway prioritized prophylaxis for continuously exposed health-care workers over treatment of sick patients in order to maintain a functioning health service.
Twenty-five plans recommended post-exposure prophylaxis. Thirteen stated that this strategy should be used only in the early phases for contacts of cases and exposed animal workers. Only one country estimated the number of contacts who might need antiviral drugs.
The operational management of antiviral storage, distribution and administration remained underdeveloped in most plans. Sixteen countries planned to devolve all or parts of these responsibilities to local administrations. Only 13 mentioned distribution centres such as influenza pandemic centres, hospital pharmacies and community pharmacies, but these were not discussed in detail. Few plans mentioned the need for prescriptions. Eight plans addressed the need for security measures at antiviral drug distribution centres.
Most plans stated an intention to stockpile antiviral drugs, with 14 plans noting that a stockpile had been secured. Eleven plans quantified their existing stockpile and nine defined a target stockpile, usually assuming an attack rate of 25–30% of the population.
Discussion
Europe became better prepared for pandemic human influenza than it was before the study period.5,6,10,11 Between November 2005 and November 2006, more countries published national strategic plans, and many countries and international agencies (such as the ECDC) have made considerable efforts to support planning through regional workshops, country visits and analyses of preparedness status.12 An increased number of plans consider an early containment strategy that offers prophylaxis to contacts and discuss the need to protect people who work with animals. Clarity and links to operational implementation also have improved. More countries prioritize the use of antivirals for treatment and prophylaxis, enhancing strategic clarity.
A recent World Bank report emphasizes the need for clear procedures and systems to manage rapid reporting and responses to human influenza, notably to ensure a rapid containment response. Our findings show that even in Europe, which may be better prepared than some regions,3 considerable gaps and inconsistencies persist and several areas of operational planning have not been addressed. For example, only half the countries have developed storage, distribution and administration strategies for vaccines and antivirals. The issue of how to deliver antivirals within 48 hours to individual patients remains largely unresolved. The recent increase in national antiviral stockpiles by many countries perhaps highlights this gap. Many countries are devolving responsibility to local administrations but providing little guidance. Consequently, they risk inconsistencies in practice, inequalities in provision of goods, chaotic service responses and public anxiety during a pandemic.
Likewise, although most countries have prioritized groups for vaccination and antivirals, details of how these policies would be put into action are still scarce. Plans do not always specify types of antiviral drugs to be used, and drug resistance is a concern with monotherapy.13 If international policies change in response to this risk, delivery systems need to be even more robust. The size of priority groups is often unclear because their scope is not clearly defined. Additionally, groups are often much larger than the actual (or intended) stockpile could accommodate. Some countries attempt to resolve this issue by building stockpiles large enough that priority-setting is not an issue, but use of antiviral prophylaxis is likely to deplete stocks quickly. For example, our analysis of whether four countries have sufficient publicly acknowledged antiviral stockpiles to meet the needs stated in their plans suggest that shortfalls will occur (Fig. 4), despite assumptions that probably underestimate demand.
Fig. 4.
Potential demand and stockpiles for antiviral drugs for four European Union countries
Assumptions: stockpiles have been made public,a attack rate of 25%, treatment needed for 50% infected. Estimates for pre-exposure prophylaxis requirements are for health care workers only, and do not include other groups mentioned in the plans.b Norway has committed to procuring an additional 12 million doses of rimantadin/amantadin for prophyaxis alone; this is not included here.
a Stockpile size sources: Bulgaria, BBC Monitoring International Reports, 12 January 2006; Cyprus, Cyprus Mail, 25 January 2006; Norway, Norway National Pandemic Preparedness Plan, 2006; United Kingdom, Reuters, March 2006.
b Population data taken from Eurostat website (available at: http://epp.eurostat.ec.europa.eu/portal/page?_pageid=1996,39140985&_dad=portal&_schema=PORTAL&screen=detailref&language=en&product=Yearlies_new_population&root=Yearlies_new_population/C/C1/C11/caa10000). Health-care worker figures taken from WHO, World health statistics 2006 (Geneva: WHO; 2006).
Governments need to balance policy in the face of uncertainty. Although considerable funds have been committed to stockpiling antivirals, many countries may have insufficient supplies. Moreover, if resistance emerges rapidly, then the expected public health benefits might not accrue. The ability of combination therapy to prevent resistance remains debatable,14 although the ineffectiveness of adamantanes in preventing transmission, the rapid development of resistance to these drugs and probable associated harms imply that neuraminidase inhibitors will require supplementation with other drugs.15 However, combination treatment would further stretch resources and compound logistical challenges.
If vaccine development cannot take advantage of the window of opportunity offered by antiviral drugs, further concerns arise. An effective vaccine is unlikely to be available for 3–6 months after a pandemic begins. Even if it can be made quickly enough,16 demand will outstrip supply. Six billion people worldwide could benefit from protection, but manufacturing capacity is currently about 300 million doses. Recent findings showing cross-protection with influenza virus from avian to human strains17,18 have led some countries to stockpile H5N1 vaccine in the hope that it could offer protection against an emergent pandemic strain.
Across Europe, plans for border control measures are inconsistent, especially in relation to screening practices and travel restrictions; such plans frequently diverge from WHO guidelines. These inconsistencies might reflect a lack of evidence. Recent research suggesting that very strict travel measures might delay a country’s exposure to a pandemic may also have affected plans.19,20 In view of the political volatility attached to differences in national approaches, increased coherence is advisable.
In preparing for the next pandemic, governments face challenges that are beyond their purview and over which they have little control. Important lessons have been learned from SARS, and the international governance structure of public health has improved, particularly in surveillance capacity, coordination and cooperation. However, response capacity and coherence remain relatively weak. These problems arise because risk management, even more than risk assessment, remains under sovereign states’ control21 despite the authority provided through the new International Health Regulations.22 For example, Indonesia recently stopped sharing human genetic samples of H5N1 with foreign laboratories because its government wanted to retain control of the intellectual property rights of the virus strain23 and secure early public health protection for its citizens. The potential delays in vaccine production that could result from such unilateral action could have far-reaching implications testing assumptions about global solidarity.24
Our evaluation’s limitations are similar to those of our previous study.5,6,25 Although our survey provides only a snapshot, it is based on a similar analysis from a year earlier so that changes and advances can be documented. Our results, as with earlier findings, agree largely with analyses done by other investigators using different methods.12,15,26 A second limitation is that plans are only one element in a preparedness strategy, albeit an important one. By revisiting plans after a year, we have at least shown that policy-makers have addressed some previously neglected issues. A further limitation is the subjective nature of our assessment. We have tried, through independent review, to address this issue. However, variations in format, terminology and language mean that any evaluation of plans must be subjective.
Governmental commitment across Europe in preparing for a pandemic seems strong, and Europe has strengthened its plans since our last evaluation. However, the remaining gaps and inconsistencies need urgent attention. Although pandemic influenza will test health systems in many unforeseen ways, coherent regional planning should ensure that responses are coordinated, evidence-based and coherent in order to effectively protect public health. ■
Funding: This work was undertaken through an unrestricted educational grant from F Hoffmann-La Roche.
Competing interests: Richard Coker has received funding and reimbursements on pandemic influenza preparedness research from F Hoffmann-La Roche, and from several European Union institutions and national governments.
University of Toronto Joint Centre for Bioethics. Ethical considerations in preparedness planning for pandemic influenza. Toronto: University of Toronto; 2005.
Singer PA, Benatar SR, Bernstein M, Daar AS, Dickens BM, MacRae SK, et al. Ethics and SARS: lessons from Toronto. BMJ 2003;327:1342-4.
References
- 1.58th World Health Assembly, 7 April 2005 Geneva: WHO; 2005.
- 2.WHO global influenza preparedness plan, the role of WHO and recommendations for national measures before and during pandemics Geneva: WHO; 2005 (WHO/CDS/CSR/GIP/2005.5).
- 3.Responses to avian and human influenza threats (draft report), July-December 2006. New York: UN System Influenza Coordinator & World Bank; 2006.
- 4.Checklist for influenza epidemic preparedness. Geneva: WHO; 2005 (WHO/CDS/CSR/GIP/2005.4).
- 5.Mounier-Jack S, Coker RJ. How prepared is Europe for pandemic influenza? Analysis of national plans. Lancet. 2006;367:1405–11. doi: 10.1016/S0140-6736(06)68511-5. [DOI] [PubMed] [Google Scholar]
- 6.Mounier-Jack S, Coker R. How prepared is Europe for pandemic influenza? An analysis of national plans. London: London School of Hygiene and Tropical Medicine; 2006. [DOI] [PubMed] [Google Scholar]
- 7.Cumulative number of confirmed human cases of avian influenza A/(H5N1) reported to WHO. Geneva: WHO; 2006. Available at: http://www.who.int/csr/disease/avian_influenza/country/cases_table_2006_04_12/en/index.html
- 8.Guidelines on the use of vaccines and antivirals during influenza pandemic. Geneva: WHO; 2004 (WHO/CDS/RMD/2004.8).
- 9.World Health Organization Writing Group Nonpharmaceutical interventions for pandemic influenza, international measures. Emerg Infect Dis. 2006:12. doi: 10.3201/eid1201.051370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pandemic influenza preparedness in the EU. Stockholm: European Centre for Disease Prevention and Control (ECDC); 2007. Available at: http://www.ecdc.eu.int/pdf/Pandemic_preparedness.pdf
- 11.3rd Joint EC/ECDC/WHO Workshop on Pandemic Influenza Preparedness in Uppsala Castle, Sweden, 15-17 May 2006. Stockholm: ECDC; 2006. Available at: http://www.ecdc.eu.int/documents/Uppsala060516/index.html
- 12.Technical report: pandemic influenza preparedness in the EU. Status report as of Autumn 2006. Stockholm: ECDC; 2007.
- 13.Pandemic influenza: science to policy. London: Royal Society; 2006. Available at: http://www.royalsoc.ac.uk/document.asp?id=5574
- 14.Tsiodras S, Mooney JD, Hatzakis A. Role of combination antiviral therapy in pandemic influenza and stockpiling implications. BMJ. 2007;334:293–4. doi: 10.1136/bmj.39105.428981.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jefferson T, Demicheli V, Di Pietrantonj C, Rivetti D. Amantadine and rimantadine for influenza A in adults. Cochrane Database Syst Rev. 2006;2:CD001169. doi: 10.1002/14651858.CD001169.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jefferson T. Influenza vaccination: policy versus evidence. BMJ. 2006;333:912–5. doi: 10.1136/bmj.38995.531701.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Suguitan AL, McAuliffe J, Mills KL, Jin H, Duke G, Lu B, et al. Live, attenuated influenza A H5N1 candidate vaccines provide broad cross-protection in mice and ferrets. PLoS Med. 2006;3:e360. doi: 10.1371/journal.pmed.0030360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gillim-Ross L, Subbarao K. Can immunity induced by the human influenza virus N1 neuraminidase provide some protection from avian influenza H5N1 viruses? PLoS Med. 2007;4:e91. doi: 10.1371/journal.pmed.0040091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brownstein JS, Wolfe CJ, Mandl KD. Empirical evidence for the effect of airline travel on inter-regional influenza spread in the United States. PLoS Med. 2006;3:e401. doi: 10.1371/journal.pmed.0030401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ferguson NM, Cummings DA, Fraser C, Cajka JC, Cooley PC, Burke DS. Strategies for mitigating an influenza pandemic. Nature. 2006;442:448–52. doi: 10.1038/nature04795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee K, Fidler DP. Avian and pandemic influenza: progress and problems with global health governance. Global Public Health. 2007;2:215–34. doi: 10.1080/17441690601136947. [DOI] [PubMed] [Google Scholar]
- 22.Fidler DP. Germs, governance, and global public health in the wake of SARS. J Clin Invest. 2004;113:799–804. doi: 10.1172/JCI21328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aglionby J, Jack A.Indonesia withholds genetic samples of bird flu virus. London Financ Times5 February2007. Available athttp://www.ft.com/cms/s/bd900a94-b55d-11db-a5a5-0000779e2340.html [Google Scholar]
- 24.Coker R, Mounier-Jack S. Pandemic influenza preparedness in the Asia-Pacific region. Lancet. 2006;368:886–9. doi: 10.1016/S0140-6736(06)69209-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nicoll A, Kaiser R. Limitations of recently published review of national influenza pandemic plans in Europe. Euro Surveill 2006;11:E060427 3. [DOI] [PubMed]
- 26.Coker R, Mounier-Jack S. Further thoughts on the limitations of a recently published review of national influenza pandemic plans in Europe. Euro Surveill 2006;11:E060504 3. [DOI] [PubMed]