Abstract
Objective
To examine infant feeding intentions of HIV-infected and uninfected women and the appropriateness of their choices according to their home resources; and to determine their adherence to their intentions in the first postnatal week.
Methods
Feeding intentions of pregnant women were compared against four resources that facilitate replacement feeding: clean water, adequate fuel, access to a refrigerator and regular maternal income. First-week feeding practices were documented.
Findings
The antenatal feeding intentions of 1253 HIV-infected women were: exclusive breastfeeding 73%; replacement feeding 9%; undecided 18%. Three percent had access to all four resources, of whom 23% chose replacement feeding. Of those choosing replacement feeding, 8% had access to all four resources. A clean water supply and regular maternal income were independently associated with intention to replacement feed (adjusted odds ratio (AOR) 1.94, 95% confidence interval (CI) 1.2–3.2; AOR 2.1, 95% CI: 1.2–3.5, respectively). Significantly more HIV-infected women intending to exclusively breastfeed, rather than replacement feed, adhered to their intention in week one (exclusive breastfeeding 78%; replacement feeding 42%; P < 0.001). Of 1238 HIV-uninfected women, 82% intended to exclusively breastfeed; 2% to replacement feed; and 16% were undecided. Seventy-five percent who intended to exclusively breastfeed adhered to this intention postnatally, and only 11 infants (< 1%) received no breast milk. The number of antenatal home visits significantly influenced adherence to feeding intention.
Conclusion
Most HIV-infected women did not have the resources for safe replacement feeding, instead choosing appropriately to exclusively breastfeed. Adherence to feeding intention among HIV-infected women was higher in those who chose to exclusively breastfeed than to replacement feed. With appropriate counselling and support, spillover of suboptimal feeding practices to HIV-negative women is minimal.
Résumé
Objectif
Examiner les intentions en matière d’alimentation de leur nourrisson de femmes infectées et non-infectées par le VIH ; la pertinence de leur choix en fonction des ressources dont elles disposent à domicile ; et le maintien de ces options une semaine après l’accouchement.
Méthodes
Les intentions en matière d’alimentation de leur futur enfant de femmes enceintes ont été confrontées à quatre éléments de ressource facilitant l’utilisation de substituts du lait maternel : eau saine, combustible adéquat, accès à un réfrigérateur et revenus maternels réguliers.
Résultats
L’analyse des intentions émises avant l’accouchement par 1253 femmes infectées par le VIH au sujet de l’alimentation de leur nourrisson a donné les résultats suivants : allaitement maternel exclusif 73% ; utilisation de substituts du lait maternel 9% ; pas de décision arrêtée 18%. Parmi les femmes ayant choisi de recourir à une alimentation de substitution, 8% avaient accès aux 4 éléments de ressources précités. Des corrélations indépendantes ont été relevées entre l’intention de donner à l’enfant un substitut du lait maternel et la disponibilité pour la mère d’un approvisionnement en eau saine et celle de revenus réguliers (odds ratio ajusté = 1,94, IC à 95% = 1,2-3,2 et odds ratio = 2,1 ; IC à 95% = 1,2-3,5, respectivement). Parmi les femmes infectées par le VIH, la proportion de celles se conformant pendant la première semaine postpartum à l’intention exprimée était notablement plus importante chez les mères ayant prévu de nourrir leur enfant exclusivement au sein que chez celles ayant d’abord opté pour un substitut du lait maternel (allaitement exclusif : 78% ; alimentation de substitution : 42%, p < 0,001). Parmi les 1238 femmes non-infectées, 1021 (82%) avaient l’intention de donner exclusivement le sein, 21 (2%) comptaient utiliser un substitut du lait maternel et 193 (16%) n’avaient pas pris de décision. 75% des femmes ayant opté pour l’allaitement exclusif se sont tenues à leur choix après l’accouchement et 11 nourrissons seulement (< 1%) n’ont pas reçu de lait maternel. Le nombre de visites anténatales à domicile influait de manière significative sur le maintien de l’option d’alimentation.
Conclusion
La plupart des femmes infectées par le VIH ne disposaient pas des ressources permettant une alimentation de substitution sans risque de leur nourrisson et ont choisi l’option la plus appropriée, à savoir l’allaitement exclusif. La proportion de femmes infectées par le VIH respectant leur intention d’alimentation était plus importante chez celles ayant opté pour l’allaitement exclusif que chez celles ayant l’intention de donner un substitut du lait maternel. L’apport de conseils et d’un soutien appropriés permet donc de réduire au minimum la diffusion de pratiques non optimales chez les femmes non-infectées par le VIH.
Resumen
Objetivo
Estudiar las intenciones de las mujeres VIH-positivas y VIH-negativas en lo relativo a la alimentación del lactante; la idoneidad de sus decisiones en función de sus recursos domésticos; y el cumplimiento de esas decisiones al cabo de una semana del nacimiento.
Métodos
Se procedió a comparar las decisiones sobre el tipo de alimentación tomadas por las mujeres embarazadas en relación con cuatro recursos que facilitan la alimentación sustitutiva (AS), a saber, el agua salubre, la disponibilidad de combustible suficiente, el acceso a un frigorífico, y unos ingresos maternos regulares. Durante la primera semana tras el parto se documentaron las prácticas de alimentación.
Resultados
Las intenciones prenatales que respecto a la alimentación manifestaron 1253 madres infectadas por el VIH fueron las siguientes: LNE (lactancia natural exclusiva), 73%; AS, 9%; no decidido, 18%. El 3% de las mujeres tenían acceso a los cuatro recursos considerados, y el 23% de ellas eligieron la AS. Entre quienes optaron por la AS, el 8% tenían acceso a los cuatro recursos. El suministro de agua salubre y unos ingresos maternos regulares se asociaron de forma independiente al deseo de recurrir a la AS (AOR (razón de posibilidades ajustada): 1,94; IC95%: 1,2-3,2; AOR: 2,1; IC95%: 1,2-3,5 respectivamente). Entre las mujeres VIH-positivas con intención de practicar la LNE se observó un porcentaje significativamente mayor de cumplimiento de ese deseo durante la primera semana en comparación con las que optaron por la AS (LNE, 78%; AS, 42%; p < 0,001). De las 1238 mujeres no infectadas por el VIH, 1021 (82%) optaron por la LNE; 21 (2%) por la AS; y 193 (16%) estaban indecisas. El 75% de las que optaron por la LNE la practicaron efectivamente tras el parto, y sólo 11 lactantes (<1%) no fueron amamantados. El número de visitas domiciliarias prenatales influyó de forma considerable en el cumplimiento de los deseos en materia de alimentación.
Conclusión
La mayoría de las mujeres infectadas por el VIH no disponían de los recursos necesarios para garantizar una AS segura, y eligieron acertadamente la LNE. El cumplimiento de las decisiones en materia de alimentación entre las mujeres infectadas por el VIH fue mayor entre las que optaron por la LNE que entre las que se inclinaron por la AS. Si existe un asesoramiento y un apoyo apropiados, la propagación de las prácticas de alimentación subóptimas a las mujeres VIH-negativas es mínima.
ملخص
الەدف: التعرف على ما لدى المصابات وغير المصابات بعدوى فيروس الإيدز من نوايا حول تغذية الرضع، ومدى ملاءمة اختيارەن لمواردەن المنزلية، ومدى التـزامەن بالنوايا بعد مرور أسبوع على الولادة.
الطريقة: قورنت النوايا التي تُبَيَّت قبل الولادة حول تغذية الرضّع مع أربعة من المصادر التي تسەِّل التغذية بالبدائل، وەي الماء النظيف والوقود الكافي وتوافر الثلاجة والدخل النظامي للأمەات. وقد تم توثيق ممارسات التغذية في الأسبوع الأول.
الموجودات: لقد كانت النوايا المبيَّتة قبل الولادة لدى 1253 امرأة مصابة بالعدوى كالتالي: نوى 73% منەن الاقتصار على الرضاعة من الثدي، و نوى 9% منەن التغذية بالبدائل، ولم يكن لدى 18% منەن نية مقررة. و3% منەن كان يتاح لەن المصادر الأربعة، ومن بينەن اختار 23% منەن التغذية بالبدائل، ومن بين ەؤلاء اللواتي اخترن التغذية بالبدائل أتيح لـ 8% منەن المصادر الأربعة، وكان الإمداد بالمياە النظيفة والدخل المنتظم للأمەات، مترافق وبشكل مستقل مع نية التغذية بالبدائل (المعدل المصحّح للأرجحية 1.94، وفاصلة الثقة 95% إذ تـراوح المعدل المصحَّح للأرجحية بين 1.2 و3.2 بالنسبة للإمداد بالمياە النظيفة، والمعدل المصحّح للأرجحية للدخل المنتظم للأمەات 2.1 وفاصلة الثقة 95% إذ تـراوح المعدل المصحَّح للأرجحية بين 1.2 و3.5). وقد التـزم أعداد متـزايدة من المصابات بعدوى فيروس الإيدز وبوضوح بالاقتصار على الإرضاع من الثدي أكثر من الالتـزام بالتغذية بالبدائل في الأسبوع الأول (فالاقتصار على الإرضاع من الثدي لدى 78%، والتغذية بالبدائل لدى 42% وقيمة الاحتمال تقل عن 0.001). ومن بين 1238 من غير المصابـات بالعـدوى بفـيروس الإيدز كان لدى 1021 منەن (82%) نية الاقتصار على الرضاعة من الثدي، ولدى 21 منەن (2%) نية التغذية بالبدائل، فيما لم يكن لدى 193 منەن (16%) أي نية مقرَّرة. وقد التـزم 75% ممن بَيَّتْن نية الاقتصار على الرضاعة من الثدي نياتەنّ بعد ولادتەنّ، فيما لم يزد عدد الرضّع ممن لم يتذوقوا حليب الثدي على 11 رضيعاً (أقل من 1%). وقد أثر عدد الزيارات المنزلية قبل الولادة بوضوح على الالتـزام بنوايا التغذية.
الاستنتاج: لم يكن لدى معظم المصابات بعدوى فيروس الإيدز المصادر للتغذية بالبدائل المأمونة، فاختاروا الاقتصار على الإرضاع من الثدي بشكل ملائم. وقد كان الالتـزام بالنية حول التغذية أعلى لدى المصابات بالعدوى بفيروس الإيدز اللاتي اخترن الاقتصار على الإرضاع من الثدي أكثر مما لدى من اختـرن التغذية بالبدائل. وبالتوعية والدعم الملائم تصبح الممارسات غير المثلى لدى النساء السلبيات بفيروس الإيدز في حدودەا الدنيا.
Introduction
United Nations (WHO/UNICEF/UNAIDS/UNFPA) recommendations on infant feeding to prevent postnatal mother-to-child transmission (MTCT) of HIV state that when replacement feeding is not acceptable, feasible, affordable, sustainable and safe, then exclusive breastfeeding is recommended.1 The recommendations promote fully-informed and free choice for HIV-infected women, who should receive the best available information on the benefits and risks of exclusive breastfeeding or replacement feeding to select the most suitable option for their situation. Furthermore, full support needs to be given to protecting, promoting and supporting breastfeeding for mothers who are HIV-negative or do not know their serostatus.2
Putting these recommendations into practice is challenging. Individual women find it difficult to balance risks and benefits in settings where access to safe replacement feeding and support is limited.3,4 For counsellors, the task of presenting information so that women can reach feasible, informed decisions requires effective counselling skills. Training staff to understand the complexities of feeding practices takes time and dedicated supervision.5
The decision to replacement feed is critically important for an HIV-infected woman, as it may either potentially save her child’s life or expose the newborn infant to unacceptably high risks of diarrhoea and malnutrition.6 The decisions of such women, and the way counselling is conducted, may also affect the feeding practices of HIV-uninfected mothers. Experience from MTCT programmes in southern Africa confirm that counsellors do not always present clear, impartial messages,7,8 that HIV-uninfected mothers at MTCT sites are inadvertently influenced to give commercial infant formula more often than at non-MTCT sites9 and that longitudinal follow-up of mothers and children in programmes is frequently inadequate.10
While there is increasing literature on the feeding practices of HIV-infected women postnatally,11–13 there have been few reports on the choices women make antenatally, and on whether these choices are consistent with the UN recommendations. Furthermore, little is known about processes of counselling on infant feeding, and whether they are achieving their goal of helping women to make the most appropriate decisions for their circumstances. Anecdotally, it has been reported that HIV-negative women increasingly avoid breast milk because of the spillover effect of infant formula introduced into areas of high HIV prevalence. However, to our knowledge there is no research that documents the feeding choices of HIV-negative women in areas where there is high HIV prevalence.
This paper examines the infant feeding intentions of HIV-infected and uninfected mothers in an area with one of the highest HIV prevalences in the world. It also examines the appropriateness of these choices given the resources available; and additionally, the women’s adherence to these choices in the first postnatal week.
Population and methods
Design
Pregnant women attending seven rural clinics, one semi-urban clinic and one urban clinic in KwaZulu Natal, South Africa, were offered confidential HIV counselling and testing as part of a cohort study investigating breastfeeding and MTCT. From August 2001 to June 2003 all HIV-infected, and a subsample of uninfected, women were offered enrolment in the study. From July 2003 all women attending antenatal clinics were offered enrolment before HIV testing. After post-test counselling, HIV-infected women were offered a further infant feeding counselling session one to two weeks later. HIV and infant feeding counselling were provided by lay staff who had completed 12 years of schooling and were selected after assessment of literacy, numeracy and basic counselling skills. Their initial training included an HIV counselling course (two weeks), a WHO/UNICEF breastfeeding counselling course (five days),14 and a WHO/UNICEF HIV and infant feeding counselling course (three days).5 Free commercial infant formula for HIV-infected women was not available initially, but was provided by the KwaZulu Natal provincial prevention of mother-to-child transmission (PMTCT) programme starting in December 2002.
Personal details including age, past pregnancies, education, water supply, sanitation, access to a refrigerator and income were recorded antenatally. Feeding intentions were compared against four resources considered necessary for safe replacement feeding: access to clean water, a refrigerator, fuel for boiling water (electricity, gas or paraffin) and a regular maternal income. The latter was used as a proxy for a woman’s ability to control financial resources in the household, particularly important in this area where few couples cohabit because of high levels of migration.15,16 Pregnancy outcomes and feeding practices in the first week of life were collected during home visits.
Data were captured using optical imaging recognition software (Teleform V7.1, Cardiff Inc., San Diego, CA, USA) in a Microsoft SQL server database. Analyses were carried out using SPSS version 12 (SPSS Inc., Chicago, IL, USA). Univariable and multivariable logistic regression analyses were used to obtain unadjusted and adjusted odds ratios (AOR) and 95% confidence intervals (CIs).
The study was approved by the ethics committee of the University of KwaZulu Natal, Durban, South Africa.
HIV and infant feeding counselling approach
Pregnant women who were HIV uninfected, or of unknown serostatus, were given information about exclusive breastfeeding for the first six months of the infant’s life, with sustained breastfeeding thereafter. HIV-infected women were counselled on different feeding options available to them.
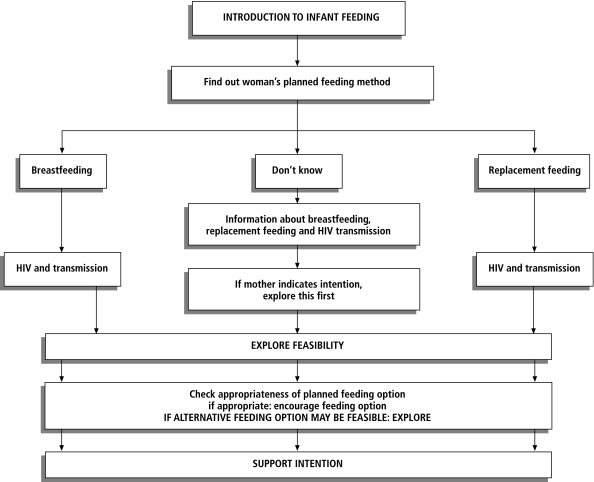
We developed an algorithm for the counsellors to use when presenting infant feeding choices to an HIV-infected woman (Fig. 1). The approach considers the woman’s feeding intention and explores the appropriateness of this based on her home circumstances. Her choice is discussed to understand what she means by breastfeeding and replacement feeding, i.e. whether her choice is based on previous experience or family preferences, whether breastfeeding would be mixed or exclusive, and how long she planned to use this feeding method. Finally, the feasibility of the woman’s intention is explored, focusing on home circumstances, past experiences, family expectations and likelihood of disclosure of HIV status at home. If the woman’s intention seems consistent with her circumstances, the counsellor affirms the woman’s intention, but also mentions that there are options that other women may choose. If the woman’s circumstances do not favour her intention, or a better practice may be feasible, e.g. the woman has the conditions for giving replacement feeding safely, then the counsellor discusses these options in more detail.
Fig. 1.
Counselling algorithm on infant feeding choices for use by lay HIV counsellors
After counselling at the clinic, all women received one antenatal home visit by a breastfeeding counsellor (blinded to HIV status) to discuss study logistics and to support the woman in her feeding option. Those choosing replacement feeding were referred to the project infant feeding specialist for a home visit to demonstrate safe replacement feeding preparation. Women who chose to breastfeed received up to three further antenatal home visits (up to four sessions) by the lay breastfeeding counsellor. If a woman changed her mind about her feeding choice antenatally, her intention nearest to the time of delivery was used for analysis.
Strict WHO feeding definitions were applied throughout this study.5 Exclusive breastfeeding means an infant receives only breast milk and no other liquids or solids, not even water, with the exception of drops or syrups consisting of vitamins, mineral supplements or medicines.
Results
Between August 2001 and September 2004, 3465 pregnant women were enrolled, of whom 535 withdrew, 71 did not fulfil the follow-up criteria, nine had indeterminate HIV status, six died in the antenatal period, 17 had spontaneous abortions and 104 had stillbirths. Thus, 2723 women of known HIV status who delivered a live infant remained. Of these 2723 women, 111 were not located antenatally for a home visit, and there were no feeding data for the first antenatal week for 121 women. Thus, 2491 women remained (1253 HIV-infected and 1238 HIV-uninfected) for whom there is information about antenatal feeding intention and postnatal feeding practices. There were no significant differences between those included in, and those excluded from, the analysis across all the measured sociodemographic characteristics. The median age (and range) at delivery of HIV-infected and HIV-uninfected women was 25 (15–45) and 21 (14–53) years, respectively; the median parity (and range) was 1 (0–8) and 0 (0–11), respectively.
HIV-infected women
After counselling and before delivery, 73% (911/1253) of HIV-infected women stated that they intended to exclusively breastfeed, 9% (113/1253) planned to replacement feed, 18% (228/1253) were undecided and one woman intended to mix feeding methods.
Table 1 presents the women’s feeding intentions and their access to the four resources considered necessary for safe replacement feeding. Those women who intended to replacement feed were more likely than the rest to have a clean water supply and to be the main income provider in both univariable and multivariable logistic regression analyses (adjusted odds ratio (AOR) 1.94, 95% confidence interval (CI) 1.2–3.2; AOR 2.1, 95% CI: 1.2–3.5; respectively). Table 1 also presents the cumulative number of resources available to women in each feeding group. Of the 39 women with all four resources, 49% (19) intended to exclusively breastfeed. Of those intending to replacement feed, 8% (9/113) had access to all four resources. As free formula was introduced in December 2002, making access to income less important, we looked at the cumulative number of resources omitting maternal income – leaving water, fuel and a refrigerator. Only 32.1% of all women (402/1253) had access to these three resources, of whom 72% (290/402) intended to exclusively breastfeed. Counsellors reported that these women were concerned with the stigma and practicalities of avoiding breastfeeding altogether.
Table 1. Access to individual and cumulative resources necessary for safe replacement feeding versus antenatal feeding intention.
| Maternal HIV status | Antenatal feeding intention | N | Resources available |
Cumulative number of resources availablea |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Safe water |
Fridge |
Electricity, gas or paraffin |
Mother is main source of income |
None |
1 |
2 |
3 |
4 |
||||
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | ||||
| HIV positive (n = 1253) | Exclusive breastfeeding | 911 | 621b (68%) | 390 (42.8%) | 646 (70.9%) | 83a (9.1%) | 109 (12%) | 199 (22%) | 277 (30%) | 307 (34%) | 19c (2%) | |
| Replacement feeding | 113 | 92 (81%) | 59 (52.2%) | 90 (79.6%) | 23 (20.3%) | 3 (2%) | 18 (16%) | 39 (35%) | 44 (39%) | 9 (8%) | ||
| Mixed feed | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | ||
| Undecided | 228 | 149 (65%) | 105 (46%) | 158 (69%) | 34 (15%) | 26 (11%) | 49 (21%) | 71 (31%) | 71 (31%) | 11 (4%) | ||
| HIV negatived (n = 1238) | Exclusive breastfeeding | 1021 | 719 (70.4%) | 573 (56%) | 669 (65.5%) | 55 (5.3%) | 130 (12%) | 232 (23%) | 338 (33%) | 303 (30%) | 18 (2%) | |
| Replacement feeding | 21 | 15 (71.4%) | 13 (61.9%) | 14 (66.6%) | 3 (14.2%) | 1 (5%) | 6 (28%) | 9 (43%) | 4 (19%) | 1 (5%) | ||
| Mixed feed | 3 | 2 | 0 | 3 | 0 | 0 | 0 | 1 | 2 | 0 | ||
| Undecided | 193 | 120 (62%) | 99 (51%) | 129 (67%) | 16 (8%) | 18 (9%) | 53 (27%) | 62 (32%) | 58 (30%) | 2 (1%) | ||
a Any combination of safe water, access to fridge/freezer, fuel other than wood and mother has regular income. b P-value < 0.01 when comparing antenatal feeding intentions of exclusively breastfeeding, replacement feeding and undecided for resources available among HIV-positive women. c P-value < 0.01 when comparing antenatal feeding intentions of exclusively breastfeeding, replacement feeding and undecided for cumulative resources available among HIV-positive women. d All P-values > 0.5 when comparing antenatal feeding intentions of exclusive breastfeeding, replacement feeding and undecided for each individual resource and cumulative resources available among HIV-negative women.
Table 2 shows women’s feeding practices in week one postnatally compared with their intention. Significantly, more of those intending to exclusively breastfeed than replacement feed adhered to their intention postnatally (exclusive breastfeeding 78%, replacement feeding 42%, P < 0.001). Maternal age at delivery, parity, education, water, refrigerator and maternal income were not significantly associated with adherence. In all 1253 HIV-infected women, the number of antenatal feeding counselling visits was significantly associated with an intention to exclusively breastfeed or replacement feed and the ability to adhere to this decision postnatally. Compared to the maximum of four visits, those visited once (AOR 10.4, 95% CI: 7.73–14.03), twice (AOR 2.04, 95% CI: 1.35–3.09) or three times (AOR 1.74, 95% CI: 1.11–2.74) were more likely to change their feeding option postnatally.
Table 2. Antenatal feeding intention versus actual practice in the first week of life.
| HIV status | Antenatal feeding intentiona | Exclusive breastfeeding |
Replacement feeding |
Mixed feed |
Some missing data |
Switched from breastfeeding to replacement feeding |
Switched from replacement feeding to breastfeeding |
|---|---|---|---|---|---|---|---|
| N (%)b | N (%) | N (%) | N (%) | N (%) | N (%) | ||
| HIV positive (n = 1253) | Exclusive breastfeeding (n = 911) | 707 (78%) | 33 (3.6%) | 98 (10.7%) | 59 (6.5%) | 11 (1%) | 3 |
| Replacement feeding (n = 113) | 35 (3%) | 47 (41%) | 14 (12%) | 12c (10%) | 4 | 1 | |
| Mixed feed (n = 1) | 0 | 0 | 0 | 1 | 0 | 0 | |
| Undecided (n = 228) | 121 (53%) | 21 (9%) | 57 (25%) | 25 (11%) | 2 | 2 | |
| HIV negative (n = 1238) | Exclusive breastfeeding (n = 1021) | 765 (75%) | 5 (0.5%) | 142 (4%) | 106 (10%) | 1 | 2 |
| Replacement feeding (n = 21) | 8 (38%) | 1 (5%) | 5 (24%) | 4 (19%) | 2 (9%) | 1 (5%) | |
| Mixed feed (n = 3) | 1 | 0 | 2 | 0 | 0 | 0 | |
| Undecided (n = 193) | 128 (66%) | 5 (2.5%) | 34 (18%) | 24 (12.5%) | 2 (1%) | 0 |
a P = 0.001 comparing antenatal feeding intentions of HIV-positive and HIV-negative women. b P = 0.001 comparing women who intended to exclusively breastfeed and adhered to this postnatally between HIV-positive and HIV-negative women. c Including 1 baby on intravenous fluids.
When only those who intended to exclusively breastfeed or replacement feed were analysed separately, those intending to exclusively breastfeed were less likely to adhere if they had electricity, gas or paraffin (AOR 1.69, 95% CI: 1.16–2.46) and if they had one antenatal counselling visit compared to four (AOR 1.69, 95% CI: 1.04–2.76). Those intending to replacement feed were less likely to adhere if they had inadequate fuel (i.e. wood or no fuel; AOR 3.52, 95% CI: 1.15–10.77), and if they had one compared to four antenatal visits (AOR 4.08, 95% CI: 1.45–14.56).
HIV-uninfected women
Of the 1238 uninfected women, 82% (1021) intended to exclusively breastfeed, 2% (21) to replacement feed only, 16% (193) were undecided and three women intended to mix feeding methods. Of those who intended to replacement feed (and were not part of the PMTCT programme, thus not eligible for free infant formula), few had the necessary resources to prepare infant formula safely.
Of those intending to exclusively breastfeed, 74% (766/1042) adhered to their intention. Of those who were undecided before delivery, 66% (128/193) exclusively breastfed after delivery. Less than 1% of infants received no breast milk at all in the first week of life (11/1238). Of the women who intended to exclusively breastfeed antenatally, the only significant factors associated with non-adherence postnatally, in both univariable and multivariable logistic regression analyses were access to a refrigerator (AOR 1.44, 95% CI: 1.1–1.88) and the number of antenatal counselling visits compared to a maximum of four (one visit AOR 15.26, 95% CI: 10.6–21.97; two visits AOR 1.54, 95% CI: 1.04–2.28).
Discussion
To our knowledge this is the first study to examine the antenatal feeding choices of women in an area of high HIV prevalence, and to discuss whether these choices are appropriate to the women’s socioeconomic situation. The results demonstrate some of the complexities of counselling women on making the difficult decision to exclusively breastfeed or to replacement feed. Our counselling approach was effective, in most cases, in matching the intention of HIV-infected women with their physical resources. Most women in this largely rural population do not have the resources to prepare replacement feeds in an acceptable, feasible, affordable, sustainable and safe manner.1 Of the HIV-infected women, 63% (792/1253) had access to only two or fewer of the four resources we considered necessary; most (73%; 585/792) chose, appropriately, exclusive breastfeeding, even when free formula milk was introduced in the area. Three percent of all HIV-infected women had access to all four resources required to facilitate safe replacement feeding; of these, only 23% stated they intended to replacement feed. This suggests that qualitative considerations (such as family acceptability, the practicalities of preparing replacement feeds or the fear of inadvertent disclosure of HIV status by avoiding breastfeeding altogether) were probably more important.13,17,18
Only 32.1% of HIV-infected women had access to safe water, a fridge and adequate fuel for heating water. Most of these women (72%) still intended to exclusively breastfeed, suggesting that even access to regular finances or free infant formula for six months were not the main influences in their feeding decision. HIV counsellors discussed finances with the women, emphasizing costs for travel to clinics, strategies for purchasing milk if supplies ran out17 and the need to provide milk for their children until they were at least two years of age.19
Those intending to replacement feed were more likely to have access to clean water and to be the main income provider. Studies have suggested that working women generally have more decision-making autonomy,20 either because they have control over the household finances or because they are more assertive and able to gain employment.
While most women (78%) who intended to exclusively breastfeed did so for the first week postnatally, only 42% (47/113) of those intending to replacement feed did so exclusively. Those with inadequate fuel were less likely to adhere to replacement feeding, suggesting there were practical difficulties in preparing formula with wood or no fuel. Conversely, those intending to exclusively breastfeed were less likely to practise this postnatally if they had adequate fuel, suggesting that it was easier for them to prepare safe replacement feeds.
This study demonstrates that, with appropriate counselling and community support for HIV-uninfected women, spillover of suboptimal feeding practices is minimal despite the provision of free infant formula in the district. The majority (82%) of HIV-uninfected women intended to exclusively breastfeed. The 2% of women who intended to replacement feed were women who were going to work or school in another town. Most women who intended to exclusively breastfeed adhered to this in week one after delivery. Only 11 infants of HIV-negative women received no breast milk at all in the first week of life (< 1%). While this paper reports only on feeding practices in the first week of life, it is encouraging that most HIV-negative women opted for exclusive breastfeeding and managed to sustain this during the first few days. There is much evidence that early feeding practices predict longer-term practices, with early initiation of exclusive breastfeeding (i.e. avoidance of prelacteal feeds and early mixed feeding) impacting on long-term lactation success.21–23 Infants born in hospitals with early breastfeeding interventions based on the baby-friendly hospital initiative are more likely to practise exclusive breastfeeding at three months postpartum.24–27 Women who have avoided breastfeeding for the first week of the infant’s life are unlikely to commence breastfeeding without active support to encourage lactation, as their prolactin levels will be low because of lack of nipple stimulation.
The most significant factor in adherence to choice in both HIV-infected and HIV-uninfected women was the number of antenatal home visits a woman received. Of HIV-infected women, when we compared those who intended to exclusively breastfeed or replacement feed and who adhered to their intention postnatally with those who did not, the number of visits was highly significant. Although all women received a separate clinic-based infant feeding counselling session two weeks after receiving their HIV results, our data suggest that this is not enough, and that women need at least two further antenatal visits. These visits help women to further explore the feasibility and implications of their choice. Mixed feeding was the norm in this area28 and women choosing exclusive breastfeeding or replacement feeding may be making a feeding choice that is uncommon in their environment. Furthermore, opportunities were provided to have discussions with other household members if the woman so wished.
After making their infant feeding decision, the women who chose to replacement feed were visited only once antenatally by the lay breastfeeding counsellors, and were supported postnatally by clinic-based study nurses and an infant feeding specialist. Our data suggest that those who choose replacement feeding, even when this is provided freely by the health services, require the same level of home support as those who choose exclusive breastfeeding. It is possible that women who chose replacement feeding realized how impractical this was in their home situations after delivery and changed to breastfeeding.
Studies have documented that infant feeding counselling is often of poor quality or unavailable for many women.7,29 Our study demonstrates that well-trained and well-supported lay HIV counsellors with no health background are able to provide quality infant feeding counselling according to international guidelines and to help women make appropriate choices for their socioeconomic situations. Our method enabled counsellors to explore in a systematic way the options available and the feasibility of each woman’s choice. The set of counselling tools recently produced by WHO30 include an algorithm similar to the one used in this study and a card designed to help counsellors explore the woman’s home and family situation; this is based on a table we used during training. Experience shows that where superficial training has been given on HIV and infant feeding, counsellors are unable to provide adequate support to HIV-positive mothers to carry out their feeding choice.31 There is an urgent need to train all those involved in infant feeding counselling so they have both the knowledge and the skills to help women make appropriate choices, and so they can support women in their choice after delivery. ■
Acknowledgements
We are grateful to all women and children in the study, and for the continued dedication of the study’s field, clinic and data staff, in particular the managers and trainers: Thembi Blose, Zanele Fakude, Cookie Govender, Dumo Mkwanazi, Nqobile Mkhwanazi, Londiwe Mthethwa and Samukelisiwe Mtshali. We thank Jane Lucas, Felicity Savage and Heidi Van Rooyen for their valuable insights in designing our feeding strategy and their encouragement, and Zandile Myeni and Ayanda Ngidi for their initial support and supervision of the HIV counsellors. We also are grateful to: Jan van den Broeck and Colin Newell, who assisted with data management during the study and analyses; Dave Perlman and Kobus Herbst for their assistance in the design of the database; and Geoff Solarsh, Shuaib Kauchali and Ameena Goga for assistance in the initial formative pilot work and training. We wish to thank the Community Liaison Office at the Africa Centre and the Community Advisory Board for their guidance and feedback throughout the study, and also the local government clinics that allowed us to work in their facilities.
We are grateful to the independent members of the Study Steering Committee and the Data Monitoring and Safety Committees. These include Janet Darbyshire (MRC, the United Kingdom), None Simelela (South Africa National Department of Health), Victoria Sithole (Community Advisory Board). Data Monitoring and Safety Committee: Cathy Wilfert (Paediatric AIDS Foundation), Carl Lombard (MRC, SA), Ames Dhai (Department of Obstetrics and Gynaecology and the Biomedical Ethics Unit, the United Kingdom) and Francis Crawley (Free University of Brussels).
Footnotes
Funding: This study was supported by grants from the Wellcome Trust UK.
Competing interests: None declared.
References
- 1.New data on the prevention of mother-to-child transmission of HIV and their policy implications: conclusions and recommendations. WHO Technical Consultation on behalf of the UNFPA/UNICEF/WHO/UNAIDS Inter-Agency Task Team on Mother-to-Child Transmission of HIV, Geneva, 11-13 October 2000. Geneva: WHO; 2001. WHO document WHO/RHR/01.28. Available from: http://whqlibdoc.who.int/hq/2001/WHO_RHR_01.28.pdf
- 2.Global strategy on infant and young child feeding. Geneva: WHO; 2003. Available from: http://whqlibdoc.who.int/publications/2003/9241562218.pdf [PubMed]
- 3.Piwoz EG, Bentley ME. Women’s voices, women’s choices: the challenge of nutrition and HIV/AIDS. J Nutr. 2005;135:933–7. doi: 10.1093/jn/135.4.933. [DOI] [PubMed] [Google Scholar]
- 4.Piwoz EG, Ross JS. Use of population-specific infant mortality rates to inform policy decisions regarding HIV and infant feeding. J Nutr. 2005;135:1113–9. doi: 10.1093/jn/135.5.1113. [DOI] [PubMed] [Google Scholar]
- 5.HIV and infant feeding counselling: a training course. Division of Child and Adolescent Health. WHO/SCH/CAH/00.4; UNICEF/PD/NUT/(J)00-3; UNAIDS/99.57E. Geneva: WHO; 2000.
- 6.Coutsoudis A, Goga AE, Rollins N, Coovadia HM. Free formula milk for infants of HIV-infected women: blessing or curse? Health Policy Plan. 2002;17:154–60. doi: 10.1093/heapol/17.2.154. [DOI] [PubMed] [Google Scholar]
- 7.Chopra M, Piwoz E, Sengwana J, Schaay N, Dunnett L, Sanders D. Effect of a mother-to-child HIV prevention programme on infant feeding and caring practices in South Africa. S Afr Med J. 2002;92:298–302. [PubMed] [Google Scholar]
- 8.Chopra M, Doherty T, Jackson D, Ashworth A. Preventing HIV transmission to children: quality of counselling of mothers in South Africa. Acta Paediatr. 2005;94:263–5. doi: 10.1080/08035250510029479. [DOI] [PubMed] [Google Scholar]
- 9.Botswana PMTCT Advisory Group. An evaluation of infant feeding practices by mothers at PMTCT and non-PMTCT sites in Botswana. Botswana Food and Nutrition Unit, Ministry of Health, Botswana and UNICEF Botswana; November 2001.
- 10.Koniz-Booher P, Burkhalter B, Iliff P, Willumsen J, de Wagt A, Labbok M, editors. HIV and infant feeding: a compilation of programmatic evidence. UNICEF; 2003. [Google Scholar]
- 11.Rollins NC, Meda N, Becquet R. Preventing postnatal transmission of HIV-1 through breastfeeding: modifying infant feeding practices. J Acquir Immune Defic Syndr. 2004;35:188–95. doi: 10.1097/00126334-200402010-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Poggensee G, Schulze K, Moneta I, Mbezi P, Baryomunsi C, Harms G. Infant feeding practices in western Tanzania and Uganda: implications for infant feeding recommendations for HIV-infected mothers. Trop Med Int Health. 2004;9:477–85. doi: 10.1111/j.1365-3156.2004.01214.x. [DOI] [PubMed] [Google Scholar]
- 13.Suryavanshi N, Jonnalagadda S, Erande A, Sastry J, Pisal H, Bharucha KE, et al. Infant feeding practices of HIV-positive mothers in India. J Nutr. 2003;133:1326–31. doi: 10.1093/jn/133.5.1326. [DOI] [PubMed] [Google Scholar]
- 14.Breastfeeding counselling: a training course. Trainers guide. Division of diarrhoeal and acute respiratory disease control, WHO/CDR/93.3-6 and UNICEF/NUT/93. Geneva: WHO; 1993.
- 15.Lurie M, Williams BG, Zuma K, Mkaya-Mwamburi D, Garnett G, Sturm AW, et al. The impact of migration on HIV-1 transmission in South Africa: a study of migrant and nonmigrant men and their partners. Sex Transm Dis. 2003;30:149–56. doi: 10.1097/00007435-200302000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Hosegood V, McGrath N, Herbst K, Timaeus I. The impact of adult mortality on household dissolution and migration in rural South Africa. AIDS. 2004;18:1585–90. doi: 10.1097/01.aids.0000131360.37210.92. [DOI] [PubMed] [Google Scholar]
- 17.Doherty T, Chopra M, Nkonki L, Jackson D, Greiner T. Effect of the HIV epidemic on infant feeding in South Africa: “When they see me coming with the tins they laugh at me. Bull World Health Organ. 2006;84:90–5. doi: 10.2471/BLT.04.019448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Paoli M, Manongi R, Klepp KI. Are infant feeding options that are recommended for mothers with HIV acceptable, feasible, affordable, sustainable and safe? Pregnant women’s perspectives. Public Health Nutr. 2004;7:611–9. doi: 10.1079/PHN2003596. [DOI] [PubMed] [Google Scholar]
- 19.Guiding principles for feeding the non-breastfed child 6-24 months. Geneva: WHO; 2005.
- 20.Hindin MJ. Women’s power and anthropometric status in Zimbabwe. Soc Sci Med. 2000;51:1517–28. doi: 10.1016/S0277-9536(00)00051-4. [DOI] [PubMed] [Google Scholar]
- 21.de Chateau P, Wiberg B. Long-term effect on mother-infant behaviour of extra contact during the first hour post-partum II. A follow-up at three months. Acta Paediatr Scand. 1977;66:145–51. doi: 10.1111/j.1651-2227.1977.tb07826.x. [DOI] [PubMed] [Google Scholar]
- 22.Perez-Escamilla R, Segura-Millan S, Canahuati J, Allen H. Prelacteal feeds are negatively associated with breastfeeding outcomes in Honduras. J Nutr. 1996;126:2765–73. doi: 10.1093/jn/126.11.2765. [DOI] [PubMed] [Google Scholar]
- 23.Hruschka DJ, Sellen DW, Stein AD, Martorell R. Delayed onset of lactation and risk of ending full breast-feeding early in rural Guatemala. J Nutr. 2003;133:2592–9. doi: 10.1093/jn/133.8.2592. [DOI] [PubMed] [Google Scholar]
- 24.Lutter CK, Perez-Escamilla R, Segall A, Sanghvi T, Teniya K, Wickham C. The effectiveness of a hospital-based program to promote exclusive breastfeeding among low-income women in Brazil. Am J Public Health. 1997;87:659–63. doi: 10.2105/ajph.87.4.659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Merten S, Dratva J, Ackermann-Liebrich U. Do baby-friendly hospitals influence breastfeeding duration on a national level? Pediatrics. 2005;116:e702–8. doi: 10.1542/peds.2005-0537. [DOI] [PubMed] [Google Scholar]
- 26.Kramer MS, Chalmers B, Hodnett ED, Sevkovskaya Z, Dzikovich I, Shapiro S, et al. Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA. 2001;285:413–20. doi: 10.1001/jama.285.4.413. [DOI] [PubMed] [Google Scholar]
- 27.Evidence for the ten steps to successful breastfeeding. Geneva: WHO. WHO/CHD/98.9.
- 28.Bland RM, Rollins NC, Coutsoudis A, Coovadia HM. Breastfeeding practices in an area of high HIV prevalence in rural South Africa. Acta Paediatr. 2002;91:704–11. doi: 10.1080/080352502760069151. [DOI] [PubMed] [Google Scholar]
- 29.Shankar AV, Sastry J, Erande A, Joshi A, Suryawanshi N, Phadke MA, et al. Making the choice: the translation of global HIV and infant feeding policy to local practice among mothers in Pune, India. J Nutr. 2005;135:960–5. doi: 10.1093/jn/135.4.960. [DOI] [PubMed] [Google Scholar]
- 30.HIV and infant feeding: counselling tools. Geneva: WHO; 2005.
- 31.HIV and infant feeding: guide for health-care managers and supervisors. Geneva: WHO; 2003. WHO/UNICEF/UNFPA/UNAIDS document. Available from: http://www.who.int/child-adolescent-health/publications/NUTRITION/ISBN_92_4_159122_6.htm