Abstract
Objective
To obtain an estimate of the prevalence of new cases of smear-positive tuberculosis in Eritrea using a new low-cost approach.
Methods
The study was designed to include a sample of 35 000 people divided between 40 clusters. The clusters were selected by sampling proportional to population size. In each cluster, census data were obtained from eligible individuals. Individuals aged 15 years or more were questioned about cough and its duration and smoking and were asked to provide two samples of sputum (spot and morning) for examination by fluorescence microscopy.
Findings
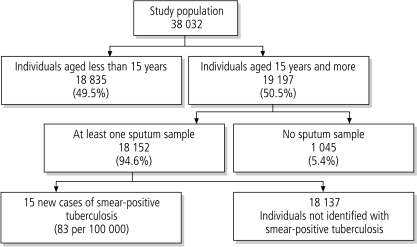
A total of 38 032 individuals were included in the study. Of the 19 197 individuals aged 15 years or more, 18 152 (94.6%) provided at least one sample of sputum. Fifteen individuals fulfilled the case definition, providing a prevalence of new cases of smear-positive tuberculosis of 90 per 100 000 (95% confidence interval, CI, 35–145 per 100 000) individuals aged 15 years or more and 50 per 100 000 (95% CI, 19–80 per 100 000) in the total population.
Conclusion
The estimated prevalence of new cases of smear-positive tuberculosis obtained from our study is considerably lower than the estimate published by the World Health Organization. The new methodology for surveys to determine the prevalence of tuberculosis that we used is feasible in the field. This methodology should be validated in other countries and compared with other methods for measuring prevalence.
Résumé
Objectif
Obtenir une estimation de la prévalence des nouveaux cas de tuberculose à frottis positif en Erythrée par une démarche nouvelle et économique.
Méthodes
L’étude a été conçue pour porter sur un échantillon de 35 000 personnes, réparties en 40 groupes. Les groupes ont été constitués par tirage proportionnel à la taille de la population. Dans chaque groupe, on a obtenu des données de recensement pour les personnes répondant aux critères d’inclusion. On a demandé aux sujets de 15 ans et plus s’ils toussaient et depuis combien de temps et d’autre part s’ils fumaient. On leur a également demandé de fournir deux échantillons d’expectoration pour examen par microscopie de fluorescence.
Résultats
Au total, 38 032 personnes ont été incluses dans l’étude. Parmi les 19 197 sujets de 15 ans ou plus, 18 152 (94,6%) ont fourni au moins un échantillon d’expectoration. Quinze personnes remplissaient les critères de la définition de cas, d’où une prévalence des nouveaux cas de tuberculose à frottis positif de 90 pour 100 000 [intervalle de confiance à 95% (IC) : 35 -145 pour 100 000] parmi les personnes de 15 ans ou plus et de 50 pour 100 000 [intervalle de confiance à 95% (IC) : 19-80 pour 100 000] parmi la population totale.
Conclusion
L’estimation de la prévalence des nouveaux cas de tuberculose à frottis positif obtenue par notre étude est considérablement inférieure à celle publiée par l’Organisation mondiale de la Santé. La nouvelle méthodologie d’enquête utilisée pour déterminer la prévalence de la tuberculose est applicable sur le terrain. Cette méthodologie doit être validée dans d’autres pays et comparée à d’autres techniques de mesure de la prévalence.
Resumen
Objetivo
Obtener una estimación de la prevalencia de nuevos casos de tuberculosis con baciloscopia positiva en Eritrea empleando un nuevo método de bajo costo.
Métodos
El estudio se diseñó de manera que abarcara una muestra de unas 35 000 personas repartidas entre 40 conglomerados. Éstos fueron seleccionados mediante la técnica de muestreo proporcional al tamaño de la población. En cada conglomerado se obtuvieron datos censales sobre las personas que reunían las condiciones. Se encuestó a los individuos de 15 o más años acerca de la tos y su duración y sobre su consumo de tabaco, pidiéndoseles que proporcionaran dos muestras de esputo (in situ y por la mañana) para someterlas a microscopía de fluorescencia.
Resultados
En total participaron en el estudio 38 032 personas. De los 19 197 individuos de 15 o más años que había entre ellas, 18 152 (94,6%) proporcionaron al menos una muestra de esputo. Quince cumplían la definición de caso, lo que arroja una prevalencia de nuevos casos bacilíferos de tuberculosis de 90 por 100 000 (intervalo de confianza [IC] del 95%: 35-145 por 100 000) personas de 15 años o más, y de 50 por 100 000 (IC95%: 19-80 por 100 000) en la población total.
Conclusión
La prevalencia de casos nuevos de tuberculosis con baciloscopia positiva estimada a partir de nuestro estudio es considerablemente inferior a la estimación publicada por la Organización Mundial de la Salud. La nueva metodología que empleamos en las encuestas para determinar la prevalencia de la tuberculosis es viable sobre el terreno, pero debería ser validada en otros países y comparada con otros métodos de medición de la prevalencia.
ملخص
الغرض
استەدفت ەذە الدراسة تقدير معدل انتشار حالات السل الإيجابية اللطاخة الجديدة في إريتريا، باستخدام أسلوب جديد منخفض التكلفة.
الطريقة
صُمِّمت الدراسة بحيث تضم عيِّنة قوامەا 35 000 شخص مقسَّمين على 40 مجموعة. وتم انتقاء المجموعات بأخذ عيِّنات متناسبة مع حجم السكان. وأُخذت بيانات التعداد، في كل مجموعة، من أفراد مستوفين للشروط. وسُئل أفراد البحث الذين ەم في عمر 15 عاماً أو أكبر عن معاناتەم من السعال ومدى حدَّتە، وعن التدخين، وطلب منەم تقديم عيِّنتَيْن من البلغم (عيِّنة فورية عند الحضور وعيِّنة في الصباح) لاختبارەما بطريقة الفحص المجەري التألُّقي.
الموجودات
شملت الدراسة 38 032 فرداً. ومن بين 19 197 فرداً يبلغ عمرەم 15 عاماً أو أكبر، قدَّم 18 152 فرداً (نسبة 94.6%) عيِّنة بلغم واحدة على الأقل. وقد انطبق تعريف الحالات على 15 فرداً، وبذلك يكون معدل انتشار الحالات الجديدة للسل الإيجابي اللطاخة 90 لكل 100 000 فرد في عمر 15 عاماً أو أكبر (بفاصلة ثقة 95%، إذ تراوح العدد من 35 إلى 145 لكل 100 000)، و50 لكل100 000 في عيِّنة الدراسة الكلية (بفاصلة ثقة 95%، إذ تراوح العدد من 19 إلى 80 لكل 100 000).
الاستنتاج
تبيِّن نتائج الدراسة أن معدل الانتشار المقدَّر لحالات السل الجديدة الإيجابية اللطاخة يقل بدرجة كبيرة عن التقديرات المنشورة لمنظمة الصحة العالمية. كما أثبتت الدراسة جدوى المنەجية الجديدة التي استُخدمت في المسوحات لتحديد معدل انتشار السل. وتوصي الدراسة بالاستيثاق من ەذە المنەجية في بلدان أخرى، والمقارنة بينەا وبين أساليب أخرى مستخدمة لقياس معدل الانتشار.
Introduction
In 2004, 84% of the population of Eritrea was covered by the directly-observed treatment, short-course (DOTS) programme for the management of tuberculosis (TB) and WHO was notified of 720 new cases of smear-positive TB, giving a case detection rate of 17%, which is far from the target of 70%.1 The cure rate for the 2003 cohort of new smear-positive cases was 78%, which approaches the target of 85% set by the World Health Assembly in 1991. The case detection rate is calculated by dividing the number of notified cases of TB by the expected number of cases of TB, i.e. incidence. The estimate for the incidence of TB in Eritrea was based on TB notification data only, which were ranked as being of low quality.2 Thus the estimate of the case detection rate in Eritrea is very uncertain. To obtain a solid estimate of the case detection rate, the National AIDS and Tuberculosis Control Division (NATCoD) of Eritrea decided to implement a TB prevalence survey.
In recently published surveys of TB prevalence,3,4 the survey population was screened to identify individuals with a high likelihood of having TB. TB-specific diagnostic methods were then used to detect individuals with a positive smear or culture.5 In these surveys, chest X-rays and symptom interviews were used to identify suspected cases. One disadvantage of using screening is that it requires a subjective judgment (from the investigator or the patient) about who has suspected TB. Furthermore, using interviews to identify individuals with TB-specific symptoms has been shown to have variable sensitivity and cannot be used in isolation.6–9 Using chest X-ray for the identification of suspected cases requires mobile chest X-ray equipment, which is expensive. Moreover, human capacity demands are high because experienced radiologists who can read chest X-rays must be part of the field teams. As the budget for the survey of TB prevalence in Eritrea was limited and there are very few radiologists available in the country, an alternative approach was applied. Instead of first screening the population for suspected cases, we requested two samples of sputum from all individuals aged 15 years and over. The samples were examined by fluorescence microscopy, which has a high sensitivity and specificity for the identification of Mycobacterium tuberculosis, the causative agent of TB.10–12
In this paper we describe the results of our survey and discuss the applicability of the new approach.
Methods
Study area
Eritrea is located in the Horn of Africa. It became independent from Ethiopia in 1991 after 30 years of armed struggle. The country had a population of 3 158 590 in 2004. Eighty percent of the population works in the agricultural sector. Eritrea is divided into six zobas, which are split into 57 sub-zobas and 699 administrative areas. Each administrative area comprises several villages.
Study design
The study was designed to include a sample of 35 000 individuals divided between 40 clusters, providing an average cluster size of 875 individuals. The institutionalized population was excluded from the sampling frame. We selected 40 villages by probability proportional to population size sampling. The population estimates for 2000 from local government reports were used. In each village, the direction in which inclusion of individuals in the survey should start was determined by spinning a pen on the ground and choosing the direction indicated by the tip of the pen (a method used by the Expanded Programme on Immunization13). All persons in the first house in this direction were included in the survey. After visiting the first household, the fieldworkers moved to the next household, which was defined as the one whose front door was closest to the one just visited. When the village border was reached but the number of individuals included was less than 875, the survey team continued to include households in the study by moving onwards in a clockwise direction. If the village had less than 500 individuals aged 15 years or more, the village closest to the east side of the selected village was included.
Study methods
The methods of the survey were tested in a one-week pilot study. Each selected cluster was visited by one of the three field teams between February and May 2005. The field teams collected census data (name, age, and sex) from all individuals, either by interviewing the person him/herself or by interviewing a household member. A person was eligible for inclusion in the survey if he/she had slept in the household the night before the census. For individuals aged 15 years or more, information about cough and its duration and smoking was also recorded on the census form. Supervision was provided by the project manager, who visited the field teams regularly.
Each individual aged 15 years or more was asked to provide a spot sample (provided ‘on the spot’) and a morning sample (produced immediately after waking up) of sputum. The field teams actively traced persons that did not provide two samples. Reasons for not providing a sample were recorded on the census form (not able to produce sputum, not willing to produce sputum, not present, other). The samples were stored in a moist place away from direct sunlight and then transported to one of the three microscopy centres at least once per week. Sputum samples were not collected from individuals aged less than 15 years because smear-positive TB is rarely diagnosed in children. Furthermore, it is difficult to collect sputum from children, especially the very young.
In the laboratory, the macroscopic appearance of the sample (sputum or saliva) was first recorded by the microscopist. Smears were then prepared from all samples, and the slides were stained with auramine O and examined under the fluorescence microscope. If a slide gave a positive result by fluorescence microscopy, it was re-stained with Ziehl-Neelsen stain and re-examined for confirmation. Samples that gave a positive result with both staining methods were sent to the National Health Laboratory where they were re-examined. A randomly selected sample of 5% of the slides that gave a negative result by fluorescence microscopy was also re-examined by the National Health Laboratory. The microscopist who performed the re-examination at the National Health Laboratory was not informed of the initial result. For smears that were initially reported to be positive for M. tuberculosis, when the results reported by the microscopy centre and by the National Health Laboratory did not agree, they were checked by the laboratory supervisor. The outcome of this, the third examination, by the laboratory supervisor was considered to be final. As culture facilities are not available in Eritrea, culture could not be used for quality control. The National Health Laboratory supervised the three microscopy centres.
All clusters containing individuals with a positive smear result were visited by staff of the national TB programme. Individuals with two positive sputum samples were informed about the test result and were sent to a nearby health-care facility for clinical evaluation and treatment. Individuals with one positive sputum sample were referred to a nearby health-care facility for repeat smear examination (three sputum samples) and clinical evaluation. If smear examination was negative, i.e. all three sputum samples gave a negative result, a chest X-ray was made. Chest X-rays were evaluated by two experienced radiologists.
We used the Ministry of Health classification (i.e. the WHO definition1) to define cases. A sputum smear-positive patient is a patient with at least two sputum specimens that give a positive result for acid-fast M. tuberculosis bacilli by Ziehl-Neelsen microscopy or with at least one sputum specimen that is positive for acid-fast bacilli, and radiographic abnormalities consistent with active pulmonary TB. All identified cases were interviewed to assess whether they were new cases, relapsed cases or defaulters.
Patients who had a sputum smear that gave a positive result when tested for TB were asked to provide informed consent for anonymous unlinked testing for human immunodeficiency virus (HIV). Collected blood samples were tested for HIV antibodies by enzyme-linked immunosorbent assay (ELISA) using the Genscreen HIV1/2 test from Bio-Rad, according to the protocol provided by the manufacturer. Samples giving a positive result with the first ELISA were re-tested (confirmation test) with the Murex HIV Ag/Ab combination, from Abbott.
Training of data collectors
All the individuals involved in data collection were trained in the techniques for data collection and quality assurance described in the survey protocol, and they participated in the one-week pilot study.
Before the start of data collection in a cluster, a local assistant was selected to help the field team with its work, for example, identifying individuals and introducing them to the survey team members. The local assistant received a briefing by the team leader about the purpose and procedures of the study.
Data management and analysis
Data were entered in duplicate using the Census and Survey Processing System (CSPro) from the United States Census Bureau, Population Division, International Programs Center (IPC). Data analysis was performed using Excel 2002 and SPSS 12.0.1 for Windows. The prevalence of new cases of smear-positive TB was estimated by: (a) assuming that the data comprised a self-weighting sample (crude estimate); (b) taking into account the cluster design effect14 by estimating the prevalence in each cluster and thereafter calculating the average estimated prevalence per cluster, together with the corresponding standard error and 95% confidence interval (CI); and (c) using the complex sampling module of SPSS, taking into account the under-sampling of males. To calculate the prevalence rate for the total population, we assumed that there were no cases of smear-positive TB in people aged less than 15 years.
Results
Census information for the study population
Census information was collected for 38 047 eligible individuals in 40 clusters (range per cluster, 764–1223). Fifteen individuals of unknown age were excluded from the analysis, giving a total of 38 032 (Fig. 1). Of all individuals included, 56.2% were female and 43.8% were male (Table 1). The mean age of males was 20.4 (± 21.4) years and of females was 23.4 (± 19.2) years (t-test, P < 0.001). Approximately half the population was aged less than 15 years and of these individuals, 47.6% were female and 52.4% were male. In those aged 15 years or more, 64.6% were female and 35.4% were male (chi-squared test, P < 0.001). Compared with the total population of Eritrea, males aged between 20 and 49 years were under-represented in our survey.15
Fig. 1.
Flowchart summarizing the results of the survey of tuberculosis prevalence in Eritrea
Table 1. Census information for the study population.
| Variable | Males (%) | Females (%) | Total (%) |
|---|---|---|---|
| Total | 16 661 (43.8) | 21 371 (56.2) | 38 032 (100.0) |
| Age | |||
| < 15 year | 9 867 (59.2) | 8 968 (41.9) | 18 835 (49.5) |
| ≥ 15 years | 6 794 (40.8) | 12 403 (58.0) | 19 197 (50.5) |
| Reported cougha | |||
| Yes | 882 (13.0) | 1 264 (10.2) | 2 146 (11.2) |
| No | 5 904 (86.9) | 11 135 (89.8) | 17 039 (88.8) |
| Unknown/missing | 8 (0.1) | 4 (0.0) | 12 (0.1) |
| Smokinga | |||
| Yes | 326 (4.8) | 18 (0.1) | 344 (1.8) |
| No | 6 178 (90.9) | 12 329 (99.4) | 18 507 (96.4) |
| Quit smoking | 115 (1.7) | 6 (0.0) | 121 (0.6) |
| Unknown | 175 (2.6) | 50 (0.4) | 225 (1.2) |
a In individuals aged 15 years or more.
Of the 6786 males aged 15 years or older, 882 (13.0%) reported cough, while of the 12 399 females 1264 (10.2%) reported cough (chi-squared test, P < 0.001; Table 1). The percentage of individuals reporting cough increased with age from 6.4% in those aged 15–19 years to 25.7% in those aged 80 years or more (Mantel-Haenszel chi-squared test for trend, P < 0.001). The median duration of cough was 4.0 weeks in males and 2.0 weeks in females (Mann–Whitney U test, P < 0.001). Of the 2145 individuals (11.2%) reporting duration of cough, 1528 individuals (71.2%) reported a duration of at least 2 weeks.
Of all individuals aged 15 years or more, 344 (1.8%) reported smoking, 121 (0.6%) that they had quit smoking and for 225 (1.2%) no information was available (Table 1). Males more frequently reported smoking (4.8%) than females (0.1%) (chi-squared test, P < 0.001). Of those who reported smoking 62 (18.0%) reported coughing, while of the 18 626 not reporting smoking and for whom information about coughing was available 2073 (11.1%) reported coughing (odds ratio, OR, 1.76; 95% CI, 1.33–2.32).
Sputum examination
Of all individuals aged 15 years or more, 18 152 (94.6%) provided at least one sputum sample and 16 087 (83.8%) provided two sputum samples (Table 2). In total, 34 249 sputum samples were examined by fluorescence microscopy in the laboratory. Females more frequently provided two samples (87.4%) than did males (77.2%) (chi-squared test, P < 0.001). The oldest age group more frequently provided two samples than did the younger age groups, respectively 85.5% and 83.5%. Two samples were more frequently provided by those reporting cough (86.9%) than by those not reporting cough (83.4%) (OR, 1.32; 95% CI, 1.16–1.50).
Table 2. Number of samples provided, by sex, age group and by individuals reporting cough or not.
| Variable | Number of samples |
||
|---|---|---|---|
| Two (%) | One (%) | None (%) | |
| Sex | |||
| Males | 5 243 (77.2) | 944 (13.9) | 607 (8.9) |
| Females | 10 844 (87.4) | 1 121 (9.0) | 438 (3.5) |
| Age | |||
| 15–29 years | 6 601 (82.6) | 862 (10.9) | 533 (6.7) |
| 30–59 years | 6 747 (84.4) | 881 (11.0) | 369 (4.6) |
| ≥ 60 years | 2 739 (85.5) | 322 (10.0) | 143 (4.5) |
| Reported cougha | |||
| Yes | 1 865 (86.9) | 208 (9.7) | 73 (3.4) |
| No | 1 4213 (83.4) | 1 865 (10.9) | 970 (5.7) |
a For 12 individuals, information about cough was missing.
There was no recorded reason for not providing sputum samples or a laboratory result for 1616 (4.7%) samples. Registered reasons for the other 2539 times a sample was not provided were ‘Not able to provide sample’ (17.6%), ‘Not willing to provide sample’ (19.4%), ‘Not present’ (62.9%), and ‘Other’ (0.1%). Only 212 individuals (1.1% of those aged 15 years or more) were not willing to produce any sputum sample.
Of the 16 410 morning samples, 3443 (21.0%) appeared to be sputum on macroscopic examination, while of 16 262 spot samples only 1582 (9.7%) appeared to be sputum. The percentage of samples that appeared to be sputum was not associated with age, sex, or reported cough (Table 3).
Table 3. Macroscopic appearance of sample, by sex, age group and by individuals reporting cough or not.
| Variable | Macroscopic appearance of sample |
||||
|---|---|---|---|---|---|
| Morning sample |
Spot sample |
||||
| Sputum | Saliva | Sputum | Saliva | ||
| Sex | |||||
| Males | 1 130 (32.8) | 4 373 (33.7) | 555 (35.1) | 4 815 (32.8) | |
| Females | 2 313 (67.2) | 8 594 (66.3) | 1 027 (64.9) | 9 865 (67.2) | |
| Age | |||||
| 15–29 years | 1 448 (42.1) | 5 288 (40.8) | 633 (40.0) | 6 018 (41.0) | |
| 30–59 years | 1 412 (41.0) | 5 491 (42.3) | 650 (41.1) | 6 178 (42.1) | |
| ≥ 60 years | 583 (16.9) | 2 188 (16.9) | 299 (18.9) | 2 484 (16.9) | |
| Reported cougha | |||||
| Yes | 377 (11.0) | 1 498 (11.6) | 164 (10.4) | 1 734 (11.8) | |
| No | 3 065 (89.0) | 11 461 (88.4) | 1 417 (89.6) | 12 937 (88.2) | |
a For 19 samples, information about reported cough in the patient was missing.
There were 0 (95% CI, 0–0.0025) false negative smears identified among the 1712 negative smears that were re-examined at the National Health Laboratory.
Prevalence of smear-positive TB
In the initial examination, 28 individuals had at least one positive smear. One man aged 56 years was a relapse case. Of the remaining 27 individuals, 9 (33.3%) provided two samples that were both positive, 15 (55.6%) individuals provided two samples of which one was positive and 3 (11.1%) individuals provided only one sample that was positive. All 18 individuals with one positive sample were traced and referred to a health-care facility for examination of three new sputum samples. Five had two or more samples that gave a positive result by Ziehl-Neelsen staining at the health-care facility. One did not have a positive smear in the follow-up examination, but a chest X-ray evaluated by two experienced radiologists was suggestive of TB. Twelve had negative smears in the follow-up and chest X-ray that was not suggestive of TB. Thus according to our case definition, fifteen individuals were diagnosed as being new patients with smear-positive TB in the survey; seven (46.7%) were men and eight (53.3%) were women. The mean age was 41 years (range, 15–78 years). Blood samples for HIV testing were provided by 12 out of 15 (80%) of the identified patients with TB. None tested positive for HIV. Smear-positive individuals were diagnosed in ten clusters; six clusters had one smear-positive individual, three had two smear-positive individuals and one cluster had three. Positive results were more frequently reported in samples that appeared to be sputum. Of the spot samples, 0.25% of the samples that appeared to be sputum and 0.05% of the samples that appeared to be saliva were positive; for the morning samples this was 0.15% and 0.04% respectively (Mantel-Haenszel OR, 4.4; 95% CI, 1.8–10.6). Three individuals (20.0%) diagnosed with smear-positive TB reported cough during the census, while of those not diagnosed with TB 11.2% reported cough (chi-squared test, P = 0.23).
The crude prevalence of smear-positive TB was 83 per 100 000 (95% CI, 41–124 per 100 000) individuals aged 15 years or more. Taking into account cluster sampling provided a prevalence estimate of 81 per 100 000 (95% CI, 33–130 per 100 000) individuals aged 15 years or more. The design effect derived from this calculation was 1.08. In 2005, the ratio of males to females in the population aged 15 or more was 0.98 in Eritrea,15 while the sex ratio found in our survey was 0.55. Thus, males were under-represented in the sample, especially in the age group 20–49 years. Taking this into account resulted in a prevalence of new cases of smear-positive TB of 90 per 100 000 (95% CI, 35–145 out of 100 000) individuals aged 15 years or more. In 2005, 44.7% of the Eritrean population was aged less than 15 years,16 resulting in an overall prevalence of new cases of smear-positive TB of 50 per 100 000 (95% CI, 19–80 out of 100 000) assuming that there are no cases of smear-positive TB in those aged less than 15 years.
Discussion
This survey of TB prevalence in Eritrea is the first national TB prevalence survey conducted in Africa in 45 years.17 The estimated prevalence of new smear-positive TB was 50 per 100 000 in the total population. This is considerably lower than the WHO provisional estimate for 2005 of 251 per 100 000 (Catherine Watt, personal communication). In our survey, the new approach that we tested (i.e. collecting samples from all individuals aged 15 years or more and examining the samples by fluorescence microscopy) proved to be feasible. The cost of the survey was approximately €200 000, (excluding costs of salaries for Eritrean staff, which were covered by the Ministry of Health); this is considerably lower than the cost of a survey using screening of individuals by chest X-ray. The cost of one mobile chest X-ray machine alone would be at least €100 000.
To be able to assess progress towards the Millennium Development Goals18 for TB and especially Indicator 23, which concerns prevalence and death rates associated with TB, reliable information about the prevalence of TB is required. The prevalence of TB can be estimated from notification data in countries where routine surveillance is accurate. However, in most countries with a high burden of TB, routine surveillance is weak and incomplete, or even nonexistent. In 2004, it was estimated by WHO that it was notified of only 53% of cases of TB globally.1 Therefore, until surveillance systems provide complete and accurate data, additional epidemiological information from surveys is required. The approach tested in this national survey in Eritrea could facilitate the performance of surveys of TB prevalence in countries where limited resources are available.
The currently used estimate of 251 per 100 000 population is based on TB notification data only, which were ranked as being of low quality2 and the estimate is therefore very uncertain. This may explain the large difference between this estimate and that obtained from our survey. In the survey not all individuals provided samples (5% did not provide a sample) and macroscopic examination showed that many samples appeared to be saliva. Furthermore, the institutionalized population (prisons, military barracks, mental institutions and hospitals) with potentially high rates of TB was excluded from the sampling frame of this survey, which may have resulted in an underestimation of the prevalence of TB. However, it is unlikely that this underestimation would attain a factor of 5.
We show that it is feasible to collect samples from almost all individuals aged 15 years or more. Thus initial screening of the study population by chest X-ray or symptoms is not necessary to motivate individuals to provide samples. On macroscopic examination, only a small proportion of the samples appeared to be sputum. Data from TB prevalence surveys conducted in Africa between 1955 and 1960 also showed that a high percentage (93%) of samples contain saliva if they are collected from an unselected study population.17 Other TB prevalence surveys did not publish information about the proportion of samples that appear to be saliva. The effect of the high number of samples that appear to be saliva on the prevalence estimate and how this relates to the results of other surveys remains to be determined. It is possible that individuals who provided a saliva sample may not be able to produce a sputum sample although they have smear-positive TB, or because they do not have pulmonary pathology.
The other approach used in TB prevalence surveys, i.e. screening of the population by chest X-ray and symptoms, will not detect all smear-positive individuals, as not all smear-positive patients have symptoms or show abnormalities on chest X-ray. In our survey, only 20% of the patients identified as having TB reported cough or were known to cough during census and would have been eligible for sputum examination if cough was used as the basis for screening. Thus a screening strategy using cough only would have resulted in a serious underestimation of the prevalence of smear-positive TB in Eritrea. Gothi et al. reported that 37% of culture-positive cases were missed by screening for symptoms compared with screening for symptoms and via chest X-ray.19 Also, using chest X-ray to identify individuals from whom sputum samples should be requested may miss 14–50% of smear-positive cases17 and 3–43% of culture-positive cases.9,20,21
In the survey, two samples (morning and spot) were collected and examined to limit the workload of the laboratory teams. If microscopy is used for diagnosing TB in patients suspected of having pulmonary TB, 0.8% to 7.9% of cases may be missed if only two slides are examined.22–26 However, the sensitivity of fluorescence microscopy for the diagnosis of smear-positive TB in cases of suspected TB is higher than the sensitivity of Ziehl-Neelsen microscopy.10,12 It has been shown that examination of two samples using fluorescence microscopy has a higher test sensitivity than examination of three samples with Ziehl-Neelsen microscopy.11 Had only spot specimens been examined in our survey, 13 out of 14 smear-positive patients would have been diagnosed.
The results of this, the first, national survey of the prevalence of TB in Eritrea showed an overall prevalence of new cases of smear-positive TB of 90 per 100 000 individuals aged 15 years or more. The new approach used in this survey is feasible and of low cost compared with an approach using a screening step. A comprehensive survey to compare the new approach and screening by symptoms and chest X-ray should be performed to determine the quality of the prevalence estimates provided by the different study designs. ■
Ethical considerations
The study protocol was approved by the Ministry of Health, R & HRD Health Research Coordinating Office (HRU) on 5 November 5 2004, Ref. No. 15.38/8506/04. Zoba, sub-zoba and administrative area authorities were informed about the aim and procedures of the survey. During the household survey, individuals were informed about the survey and were able to refuse to participate.
Risks to study participants were considered to be minimal, involving interview and sputum collection only. The survey provided a service to those included via the detection of cases of infectious tuberculosis.
Acknowledgements
We thank Christopher Gilpin for training the laboratory teams in fluorescence microscopy and quality assurance. We very much appreciated the help of Frank Cobelens, Frank van Leth, Nico Nagelkerke, and Suzanne Verver.
The survey was financially supported by the World Bank, the World Health Organization, the International Union Against Tuberculosis and Lung Disease, the Ministry of Health of Eritrea and the Ministry of Foreign Affairs, the Netherlands.
Footnotes
Funding: Funding was provided by the World Bank, the World Health Organization/Public Health and Rehabilitation Programme in Eritrea, the International Union Against Tuberculosis and Lung Disease, the Ministry of Health of Eritrea, and the Ministry of Foreign Affairs of the Netherlands.
Competing interests: None declared.
References
- 1.World Health Organization. Global tuberculosis control: surveillance, planning, financing: WHO report 2006. Geneva: World Health Organization;2006. WHO document WHO/HTM/TB/2006.362. [Google Scholar]
- 2.Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. JAMA. 1999;282:677–86. doi: 10.1001/jama.282.7.677. [DOI] [PubMed] [Google Scholar]
- 3.Hong YP, Kim SJ, Lew WJ, Lee EK, Han YC. The seventh nationwide tuberculosis prevalence survey in Korea, 1995. Int J Tuberc Lung Dis. 1998;2:27–36. [PubMed] [Google Scholar]
- 4.Tupasi TE, Radhakrishna S, Rivera AB, Pascual ML, Quelapio MI, Co VM, et al. The 1997 nationwide tuberculosis prevalence survey in the Philippines. Int J Tuberc Lung Dis. 1999;3:471–7. [PubMed] [Google Scholar]
- 5.Van der Werf MJ, Borgdorff MW. How to measure the prevalence of tuberculosis in a population. Trop Med Int Health. doi: 10.1111/j.1365-3156.2006.01799.x. In press. [DOI] [PubMed] [Google Scholar]
- 6.Datta M, Gopi PG, Appegowda BNA, Bhima Rao KR, Gopalan BN. Tuberculosis in north Arcot district of Tamil Nadu - a sample survey. Indian J Tuberc. 2000;47:147–54. [Google Scholar]
- 7.Gopi PG, Subramani R, Radhakrishna S, Kolappan C, Sadacharam K, Devi TS, et al. A baseline survey of the prevalence of tuberculosis in a community in south India at the commencement of a DOTS programme. Int J Tuberc Lung Dis. 2003;7:1154–62. [PubMed] [Google Scholar]
- 8.Gopi PG, Subramani R, Sadacharam K, Narayanan PR. Yield of pulmonary tuberculosis cases by employing two screening methods in a community survey. Int J Tuberc Lung Dis. 2006;10:343–5. [PubMed] [Google Scholar]
- 9.den Boon S, White NW, van Lill SW, Borgdorff MW, Verver S, Lombard CJ, et al. An evaluation of symptom and chest radiographic screening in tuberculosis prevalence surveys. Int J Tuberc Lung Dis. 2006;10:876–82. [PubMed] [Google Scholar]
- 10.Githui W, Kitui F, Juma ES, Obwana DO, Mwai J, Kwamanga D. A comparative study on the reliability of the fluorescence microscopy and Ziehl-Neelsen method in the diagnosis of pulmonary tuberculosis. East Afr Med J. 1993;70:263–6. [PubMed] [Google Scholar]
- 11.Kivihya-Ndugga LE, van Cleeff MR, Githui WA, Nganga LW, Kibuga DK, Odhiambo JA, et al. A comprehensive comparison of Ziehl-Neelsen and fluorescence microscopy for the diagnosis of tuberculosis in a resource-poor urban setting. Int J Tuberc Lung Dis. 2003;7:1163–71. [PubMed] [Google Scholar]
- 12.Steingart KR, Henry M, Ng V, Hopewell PC, Ramsay A, Cunningham J, et al. Fluorescence versus conventional sputum smear microscopy for tuberculosis: a systematic review. Lancet Infect Dis. 2006;6:570–81. doi: 10.1016/S1473-3099(06)70578-3. [DOI] [PubMed] [Google Scholar]
- 13.Lemeshow S, Robinson D. Surveys to measure programme coverage and impact: a review of the methodology used by the Expanded Programme on Immunization. World Health Stat Q. 1985;38:65–75. [PubMed] [Google Scholar]
- 14.Bennett S, Woods T, Liyanage WM, Smith DL. A simplified general method for cluster-sample surveys of health in developing countries. World Health Stat Q. 1991;44:98–106. [PubMed] [Google Scholar]
- 15.IDB population pyramids [database on the Internet]. Washington DC: United States Census Bureau; c2006. Available at: http://www.census.gov/ipc/www/idbpyr.html
- 16.World population prospects: the2004revision [database on the Internet]. New York: United Nations Population Division; c2005. Available at: http://esa.un.org/unpp/
- 17.Roelsgaard E, Iversen E, Blocher C. Tuberculosis in tropical Africa: an epidemiological study. Bull World Health Organ. 1964;30:459–518. [PMC free article] [PubMed] [Google Scholar]
- 18.United Nations. Millennium Development Goals Indicators. Available at: http://unstats.un.org/unsd/mi/mi_goals.asp, accessed on August 17, 2006.
- 19.Gothi GD, Narayan R, Nair SS, Chakraborty AK, Srikantaramu N. Estimation of prevalence of bacillary tuberculosis on the basis of chest X-ray and/or symptomatic screening. Indian J Med Res. 1976;64:1150–9. [PubMed] [Google Scholar]
- 20.Fourie PB, Austoker LH. Tuberculosis prevalence survey in the Daveyton (Benomi) urban black community. S Afr Med J. 1981;60:64–7. [PubMed] [Google Scholar]
- 21.Gatner EM, Burkhardt KR. Correlation of the results of X-ray and sputum culture in tuberculosis prevalence surveys. Tubercle. 1980;61:27–31. doi: 10.1016/0041-3879(80)90056-2. [DOI] [PubMed] [Google Scholar]
- 22.Ipuge YA, Rieder HL, Enarson DA. The yield of acid-fast bacilli from serial smears in routine microscopy laboratories in rural Tanzania. Trans R Soc Trop Med Hyg. 1996;90:258–61. doi: 10.1016/S0035-9203(96)90239-4. [DOI] [PubMed] [Google Scholar]
- 23.Walker D, McNerney R, Mwembo MK, Foster S, Tihon V, Godfrey-Faussett P. An incremental cost-effectiveness analysis of the first, second and third sputum examination in the diagnosis of pulmonary tuberculosis. Int J Tuberc Lung Dis. 2000;4:246–51. [PubMed] [Google Scholar]
- 24.Wu ZL, Wang AQ. Diagnostic yield of repeated smear microscopy examinations among patients suspected of pulmonary TB in Shandong province of China. Int J Tuberc Lung Dis. 2000;4:1086–7. [PubMed] [Google Scholar]
- 25.Van Deun A, Salim AH, Cooreman E, Hossain MA, Rema A, Chambugonj N, et al. Optimal tuberculosis case detection by direct sputum smear microscopy: how much better is more? Int J Tuberc Lung Dis. 2002;6:222–30. [PubMed] [Google Scholar]
- 26.Gopi PG, Subramani R, Selvakumar N, Santha T, Eusuff SI, Narayanan PR. Smear examination of two specimens for diagnosis of pulmonary tuberculosis in Tiruvallur District, south India. Int J Tuberc Lung Dis. 2004;8:824–8. [PubMed] [Google Scholar]