Abstract
Problem
In many countries, the tuberculosis (TB) annual case detection rate is below the target of 70%. In the Lao People’s Democratic Republic in 2005, it did not exceed 55%.
Approach
The DOTS strategy promotes passive case detection of TB. In order to increase the detection rate, we validated a questionnaire targeting lay informants at village level to notify patients with chronic cough and assessed the relevance for TB case-finding. A three-item questionnaire was sent through the district health departments to all villages in six districts in six provinces. The village headmen were asked to notify chronic cough patients. Answers were validated in a door-to-door survey (20 villages/district). In a sub-sample (four villages/district) all confirmed patients were screened for TB and paragonimiasis.
Local setting
Attapeu, Luang Namtha, Luang Prabang, Saravane, Savanakhet and Vientiane provinces in the Lao People’s Democratic Republic.
Relevant changes
Lay informant questionnaires sent from district health offices to villages are cost-effective and foster interaction between the health services and remote and underserved communities. Although the correct detection of patients is highly dependent on direct respondents, a substantial number of new TB and paragonimiasis cases were consistently diagnosed in chronic cough patients.
Lessons learned
Out of 456 questionnaires, 295 were returned (65%). Return rates were highly variable between districts (48–87%), questionnaires’ sensitivity (56–98%), positive predictive value (34–88%) and correlation between number of notified and confirmed patients (r: 0.26–0.78). In sub-sampled villages (13 541 population) 19 (5.1%) TB and 26 (7.0%) paragonimiasis cases were detected in 374 chronic cough patients. This quick questionnaire approach proved motivating for district authorities and village key informants, although no incentives were provided. The highly operator-dependent approach yielded a consistent detection rate of TB and paragonimiasis cases. This approach brings health services and populations in need in close contact, which is particularly crucial in remote and underserved areas.
Résumé
Problématique
Dans de nombreux pays, le taux de détection annuel des cas de tuberculose (TB) est inférieur à la valeur visée de 70%. En République démocratique populaire lao, ce taux n’a pas dépassé 55% pour l’année 2005.
Démarche
La stratégie DOTS encourage la détection passive des cas de TB. En vue d’accroître le taux de détection des cas, nous avons validé un questionnaire destiné à la notification par des informateurs non spécialistes dans les villages des cas de toux chronique et évalué l’intérêt de ce questionnaire pour le dépistage des cas de TB. Un questionnaire en trois points a été envoyé par l’intermédiaire des services sanitaires de district à tous les villages de six districts de six provinces. Il était demandé aux chefs de village de notifier les cas de toux chronique. Les réponses obtenues ont été validées par une enquête de porte à porte (20 villages/district). Dans un sous-échantillon (quatre villages/district), un dépistage de la tuberculose et de la paragonimiase a été pratiqué chez les cas confirmés de toux chronique.
Contexte local
Provinces d’Attapeu, de Luang Namtha, de Luang Prabang, de Saravane, de Savanakhet et de Vientiane, en République démocratique populaire lao.
Modifications pertinentes
L’envoi de questionnaires destinés à des informateurs non spécialistes par les services sanitaires de district aux villages constitue une solution peu onéreuse et favorise les contacts entre ces services et des communautés éloignées et non desservies. Bien que le dépistage correct des malades dépende fortement de la personne qui répond au questionnaire, la notification des cas de toux chronique a permis systématiquement de diagnostiquer un nombre supplémentaire de nouveaux cas de TB et de paragonimiase.
Enseignements tirés
Parmi les 456 questionnaires, 295 (65%) ont été retournés. D’un district à l’autre, on relevait une forte variation du taux de retour (48 à 87%), de la sensibilité du questionnaire (56 à 98%), de la valeur prédictive positive (34 à 88%) et du taux de corrélation entre le nombre des cas notifiés et celui des cas confirmés (r : 0,26 à 0,78). Dans les villages faisant partie du sous-échantillon (13 541 habitants), 19 cas de TB (5,1%) et 26 cas de paragonimiase (7,0%) ont été détectés chez 374 individus atteints de toux chronique. Cette démarche par questionnaire rapide s’est avérée motivante pour les autorités de district et les principaux informateurs des villages, malgré l’absence d’incitations. Bien que fortement dépendante de la personne remplissant le questionnaire, elle a permis d’obtenir un taux homogène de détection des cas de TB et de paragonimiase. Elle permet aussi d’établir un contact étroit entre les services sanitaires et les populations nécessitant des soins, ce qui est particulièrement important pour les zones reculées et non desservies.
Resumen
Problema
En muchos países la tasa anual de detección de casos de tuberculosis (TB) es inferior a la meta propuesta del 70%. En la República Democrática Popular Lao no superó el 55% en 2005.
Método
La estrategia DOTS fomenta la detección pasiva de casos de TB. Con el fin de aumentar la tasa de detección, hemos validado un cuestionario dirigido a informantes legos de los pueblos para que notifiquen los casos de tos crónica, y hemos analizado su importancia en la identificación de casos de TB. A través de los departamentos de salud distritales, se envió un cuestionario de tres preguntas a todos los pueblos de seis distritos de seis provincias. Se les pidió a los jefes de los pueblos que notificaran los casos de tos crónica. Las respuestas fueron validadas mediante una encuesta puerta a puerta en 20 pueblos/distrito. En una submuestra de cuatro pueblos/distrito se realizaron pruebas de detección de la TB y la paragonimiasis en todos los casos confirmados de tos crónica.
Lugares estudiados
Provincias de Attapeu, Luang Namtha, Luang Prabang, Saravane, Savanakhet y Vientiane de la República Democrática Popular Lao.
Cambios pertinentes
Los cuestionarios enviados por los departamentos de salud distritales a informantes legos de los pueblos son costoeficaces y fomentan la interacción entre los servicios de salud y las comunidades remotas subatendidas. Aunque la detección correcta de los pacientes depende mucho de quienes respondan, se diagnosticó un número considerable de nuevos casos de TB y paragonimiasis en pacientes con tos crónica.
Enseñanzas extraídas
De los 456 cuestionarios enviados, se completaron 295 (65%). Estas cifras fueron muy variables según los distritos, (48–87%), al igual que la sensibilidad (56–98%) y el valor predictivo positivo (34–88%) de los cuestionarios o la correlación entre el número de casos notificados y confirmados (r: 0,26–0,78). En los pueblos de la submuestra (13 541 habitantes) se detectaron 19 casos (5,1%) de TB y 26 (7,0%) de paragonimiasis entre 374 pacientes con tos crónica. Este cuestionario rápido motivó tanto a las autoridades distritales como a los informantes clave de los pueblos, pese a que no se ofrecieron incentivos. Este método muy dependiente del operador proporcionó una tasa homogénea de detección de casos de TB y paragonimiasis, y pone a los servicios de salud en contacto con las poblaciones necesitadas, lo cual es especialmente importante en zonas remotas y subatendidas.
ملخص
مشكلة البحث
تعاني بلدان عديدة من انخفاض المعدل السنوي لاكتشاف حالات السل عن المستوى المستەدف، وەو 70%. وفي جمەورية لاو الديمقراطية الشعبية، لم يزد ەذا المعدل على 55% في عام 2005.
الطريقة
تعزز استـراتيجية DOTS اكتشاف الحالات غير النشطة للسل. وبغية رفع معدل اكتشاف الحالات، أعددنا استبيانا للمرشدين غير المتخصصين لإخطار المرضى الذين يعانون من سعال مزمن، وقمنا بتقييم مدى صلة ذلك باكتشاف حالات السل. وتم إرسال استبيان من ثلاثة بنود إلى جميع القرى في ست مناطق تقع في ست مقاطعات، وذلك من خلال الإدارات الصحية في المناطق. وطُلب من شيوخ القرى إخطار المرضى الذين يعانون من سعال مزمن. وتم التحقق من الإجابات بإجراء مسح من منزل إلى منزل (20 قرية/منطقة). كما تم تحري السل وداء جانبية المناسل لدى جميع المرضى المؤكدة حالتەم في عينة فرعية (أربع قرى/منطقة).
مواقع الدراسة
أجريت الدراسة في ست مقاطعات في جمەورية لاو الديمغرافية الشعبية، ەي: أتابو، ولوانغ نامثا، ولوانغ برابانغ، وسارافان، وسافاناكت، وفينتيان.
التغييرات ذات الصلة
لوحظ أن الاستبيانات المعدة للمرشدين غير المتخصصين، المرسلة من المكاتب الصحية للمناطق إلى القرى، عالية المردود، وأنەا تعزز التفاعل بين المرافق الصحية والمجتمعات النائية والمحرومة من الخدمات. وبرغم أن الاكتشاف الصحيح للمرضى يعتمد إلى حد كبير على المستجيبين المباشرين، إلا أن عدداً كبيراً من الحالات الجديدة للسل ولداء جانبية المناسل تم تشخيصەا في المرضى الذين يعانون من السعال المزمن.
الدروس المستفادة
تم تلقي 295 استبياناً من جملة 456 استبياناً تم إرسالەا (أي نسبة 65%). ولوحظ تفاوت كبير في نسبة الاستبيانات التي تم تلقيەا من المناطق (48 إلى 87%)، وفي حساسية الاستبيانات (56 إلى 98%)، وفي القيمة التنبؤية الإيجابية (34 إلى 88%)، وفي الارتباط بين عدد المرضى المبلَّغين وعدد المرضى المؤكديــن (معامــل الارتبـاط (( r )) = 0.26 إلى 0.78). وفي القرى التي أُخذت منەا عينات فرعية (البالغ عدد سكانەا 541 13 نسمة) تم اكتشاف 19 حالة سل (5.1%) و26 حالة لداء جانبية المناسل من بين 374 مريضاً يعانون من سعال مزمن. وقد أثبت أسلوب الاستبيان السريع ەذا فعالية في تحفيز سلطات المناطق والمرشدين الرئيسيين في القرى، برغم عدم تقديم أي حوافز لەم. وأسفر ەذا الأسلوب، المعتمد أساساً على المرشدين، عن ثبات معدل اكتشاف حالات السل وداء جانبية المناسل. ويعزز ەذا الأسلوب الاتصال المباشر بين المرافق الصحية والسكان المحتاجين للخدمات، وەو عنصر بالغ الأەمية في المناطق النائية والمناطق المحرومة من الخدمات.
Background
Tuberculosis accounts for almost 2 million deaths per year worldwide.1,2 The DOTS strategy is implemented to curb the burden of disease. The target for 2005 included 100% DOTS coverage, 70% annual case detection and 85% cure rates. In WHO’s Western Pacific Region, substantial progress has been achieved in the last 10 years.3
The Lao People’s Democratic Republic is a landlocked country in south-east Asia. Its multiethnic and rural (87%) population (5.6 million) is young (50% below 20 years of age) and scattered (population density 24 persons/km²) in mountainous areas (National Census 2005). The Lao People’s Democratic Republic ranks 133rd among 177 countries in the Human Development 2006 index (available at: http://hdr.undp.org/hdr2006/statistics/). The provision of health services is challenging due to the scattered population, lack of resources and difficult access to remote areas.
The national TB control programme started in 1995.4 The DOTS coverage and cure rates in 2000 reached 98% and 80%, respectively.3 The prevalence of TB estimated by WHO was 318 per 100 000 population in 2004.3 The low case detection rate of 55% is a major challenge for TB control, as is low access to health facilities.
The DOTS strategy relies on self-presentation of patients with chronic cough (> 3 weeks) at the health facility and on sputum smear examination for acid-fast bacilli. Actively identifying patients with chronic cough in the community has the potential to improve case-detection rates. Hence, rapid, low-cost and easily applicable approaches are demanded. Chronic cough is an easily recognizable symptom for laypersons.
The objective of our study was to validate a rapid and low-cost questionnaire to identify patients with chronic cough and assess its relevance in TB case detection.
Population and procedures
Study area
We selected six provinces representative of the Lao People’s Democratic Republic’s geographical and sociocultural diversity (Attapeu, Luang Namtha, Luang Prabang, Saravane, Savanakhet and Vientiane). One district was randomly selected in each province.
Rapid identification of patients
Village headmen were targeted as key informants in a three-item questionnaire. First, they were asked to state three main health problems among the villagers, then they were asked whether chronic cough patients (>3 weeks) were present and to identify them by name. It was explained to them in writing that their information would help to clarify the village’s health priorities. We deliberately did not give more information to avoid introducing bias. Furthermore, the village headmen were asked to consult other village key informants, i.e. health volunteers, elders, monks and schoolteachers, during the study. Finally, they were requested to return the questionnaires to the district health offices.
Questionnaire distribution and collection
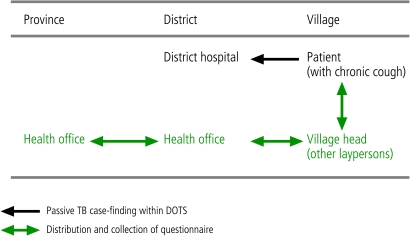
Questionnaires were sent to all villages in the districts. A member of the National Institute of Public Health in Vientiane dispatched the letters and questionnaires, in collaboration with the provincial health office (Fig. 1), to the district health offices which forwarded them to the villages using normal information channels. No financial incentive was offered at any level. The village informants received no preliminary information about the study.
Fig. 1.
Utilization of rapid and low-cost questionnaire targeted at village key informants to detect patients with chronic cough (schematic representation)
Validation surveys
Based on the number of reported patients, villages were classified in four quartiles. From each quartile, five villages were randomly selected for the validation survey. A house-to-house investigation was conducted in each village by a two-member study team. Any villager reported as having a chronic cough was examined. At the same time, additional chronic cough patients were identified.
Etiology of chronic cough
In each district, the four villages with the highest number of people with confirmed chronic coughs were re-visited. Three sputum samples per patient were collected over two days and microscopically examined on-site for Paragonimus ova (unstained specimens) and Mycobacterium tuberculosis (Ziehl-Neelsen stain). All patients diagnosed with TB were referred to the national TB programme. Paragonimiasis cases were treated with praziquantel (3 x 25mg/kg/day for 3 days).
Data analysis
All data were entered in EpiInfo version 6.04 and cross-checked with original data sheets. Analyses were performed with STATA version 8. The questionnaire return rate (number returned/number distributed), correlation coefficients (number notified/number confirmed chronic cough cases) and the questionnaires’ sensitivity and positive predictive value were calculated for each district.
Ethical clearance was obtained from the Council of Medical Science in Vientiane. Approval was obtained from provincial and district health authorities and oral informed consent was obtained from the villagers involved. The study was carried out from May 2002 to June 2003.
Findings
Out of 456 questionnaires sent to village headmen, 295 were returned (65%). The rates varied widely between districts (range 48–87%).
In the validation surveys, 1071 and 1002 chronic cough patients were found by village headmen and the team, respectively. In identifying chronic cough patients, a large variability was found between districts in the sensitivity (range 56–98%) and positive predictive values (range 34–88%). For example, in Sanamxay district almost all cases of chronic cough (98%) were reported, but over-reporting resulted in low positive predictive value (34%). By contrast, in Namback and Hinheub districts chronic cough was under-reported (60% and 56%, respectively; positive predictive value 85% and 88%, respectively). The correlation between the number of reported and confirmed people with cough was also highly variable between districts, from weak to moderate correlation (0.26< r <0.78).
Between 35 and 119 patients were screened for TB and Paragonimus per district (Table 1). Both infections were diagnosed in all districts except Hinheub (no TB) and Muang Sing (no paragonimiasis). In 374 patients with chronic cough notified in a population of 13 541 persons, 19 new TB cases and 26 new paragonimiasis cases were identified. An overall case detection rate of 5.1% (range 0–26%) and 7.0% (range 0–10.1%) was found for TB and paragonimiasis, respectively. In four out of six districts, the rate of infection paragonimiasis was higher than TB.
Table 1. Tuberculosis and paragonimiasis detection rates in patients with chronic cough in six provinces (24 villages) of the Lao People’s Democratic Republic, 2002–2003.
| Province | District | Population (4 villages/district) | Number of patients with chronic cough checked (%) | Number of TB patients (%)a | Number of TB patients 100 000 | Number of paragonimiasis (%)b |
|---|---|---|---|---|---|---|
| Luang Namtha | Muang Sing | 1 163 | 44 (3.8) | 1 (2.3) | 86 | 0 (0) |
| Luang Prabang | Namback | 1 933 | 81 (4.2) | 2 (2.5) | 103 | 5 (6.2) |
| Savannakhet | Atsaphanthong | 2 631 | 35 (1.3) | 9 (25.7) | 342 | 2 (5.7) |
| Attapeu | Sanamsay | 3 416 | 55 (1.6) | 4 (7.3) | 117 | 5 (9.1) |
| Vientiane | Hinheubc | 3 159 | 119 (3.8) | 0 | 0 | 12 (10.1) |
| Saravane | Toumlanec | 1 239 | 40 (3.2) | 3 (7.5) | 242 | 2 (5.0) |
| Total | 13 541 | 374 (2.8) | 19 (5.1) | 140 | 26 (7.0) |
a At least one of three sputum-positive for TB. b At least one of three sputum-positive for ova of Paragonimus sp. c Survey carried out in May and June 2003.
Discussion
The study showed that village headmen and their informants participated well in the questionnaire approach. The return rate was higher than expected, given that these groups received no specific preliminary information or incentives to collect the questionnaire at district health offices, to search for symptomatic villagers or to return the filled data sheets to the health offices. In extremely remote districts like Toumlane (Saravane province), the return rate reached 87% and the information provided was relevant; i.e., a strong correlation was found between the numbers of reported and confirmed chronic cough patients. However, the opposite was also found (e.g. Attapeu province) where the return rate was low (58%) with weak correlation, indicating that laypersons may have more difficulty assessing chronic cough than originally thought. In the context of the Lao People’s Democratic Republic, coughing may be very common given poor housing and daily indoor exposure to tobacco and fuel smoke.
Rapid and low-cost questionnaires to screen large areas for urinary schistosomiasis have shown to be a highly cost-effective community diagnosis tool.5 The questionnaire approach is based on an easily recognizable symptom, haematuria (blood in urine), reported by laypersons. The questionnaire is sent to primary schools through administrative channels from provincial to village level and back. Teachers question their pupils to identify patients with haematuria, which is subsequently treated. Areas with higher numbers of patients represent priority areas for interventions.
Chronic cough is a much less specific symptom or marker. Haematuria is highly specific for urinary schistosomiasis, while chronic cough can be found in various diseases involving upper and lower respiratory tract infections.
However, the moderate performance of the quick questionnaire has to be considered in the light of its extremely low cost and high feasibility. Indeed, it allowed the detection of several hitherto undiagnosed smear-positive TB cases. In Savannakhet province nine TB patients were newly diagnosed, yielding an incidence rate of 342/100 000, which is three times the national incidence rate. Furthermore, the questionnaire fosters contact between the community and health services, which in itself is extremely valuable in addressing access-related issues.
The DOTS strategy promotes a passive detection option. Mathematical models suggest that increasing TB detection and cure rates by a more proactive strategy would be the most effective way to reduce TB incidence and burden,6 and would avert millions of cases and deaths worldwide.7 A recent review listed these proactive strategies as including tuberculin surveys, mass radiography, house-to-house surveys and systematic outpatient screening.8 Our rapid questionnaire approach could be added to the list.
We detected paragonimiasis cases in all but one investigated district. This allowed the discovery of an endemic focus of this ill-known and underdiagnosed parasitic lung disease (Hinheub district).9,10,11
To our knowledge, this is the first attempt to examine the usefulness of administering low-cost, rapid questionnaires targeting village lay informants through the health system. In the 1970s in Kenya, direct questioning of community leaders yielded satisfactory results in detecting suspected TB in individuals with chronic cough, which consequently led to smear-positive rates of 1.5% to 2.3%.12
Although this rapid questionnaire approach is operator-dependent for the identification of chronic cough cases, it results in a consistent increase in TB case detection at an extremely low cost. Repeated application with preliminary additional information to village key informants is likely to increase its performance. The communities’ motivation to participate will increase with the subsequent successful management of chronic cough patients and TB treatment. ■
Acknowledgements
The authors appreciate the interest and contributions of health authorities at provincial, district and village levels, and the active participation of the village populations. Special thanks go to the postgraduate students of the Institut de la Francophonie pour la Medicine Tropicale (IFMT) who participated in the district field work. The support of Professor Boungong Boupha, director of the National Institute of Public Health in Vientiane, is highly appreciated. Our thanks also go to Dr Fréderique Bonnet of the Swiss Red Cross, who facilitated work in Namback district. Funding was granted by Agence Universitaire de la Francophonie via IFMT and the PAS/AUF 2002 project (Number 6301PS314).
Footnotes
Competing interests: None declared.
References
- 1.Corbett EL, Watt CJ, Walker N, Maher D, Williams BG, Raviglione MC, et al. The growing burden of tuberculosis: global trends and interactions with the HIV epidemic. Arch Intern Med. 2003;163:1009–21. doi: 10.1001/archinte.163.9.1009. [DOI] [PubMed] [Google Scholar]
- 2.Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. JAMA. 1999;282:677–86. doi: 10.1001/jama.282.7.677. [DOI] [PubMed] [Google Scholar]
- 3.Tuberculosis Control in the Western Pacific Region. Manila: WHO Regional Office for the Western Pacific; 2006. ISBN 92 9061 219 3. [Google Scholar]
- 4.Arnadottir TH, Soukaseum H, Vangvichit P, Bounmala S, Vos E. Prevalence and annual risk of tuberculosis infection in Laos. Int J Tuberc Lung Dis. 2001;5:391–9. [PubMed] [Google Scholar]
- 5.Lengeler C, Utzinger J, Tanner M. Questionnaires for rapid screening of schistosomiasis in sub-Saharan Africa. Bull World Health Organ. 2002;80:235–42. [PMC free article] [PubMed] [Google Scholar]
- 6.Currie CS, Williams BG, Cheng RC, Dye C. Tuberculosis epidemics driven by HIV: is prevention better than cure? AIDS. 2003;17:2501–8. doi: 10.1097/00002030-200311210-00013. [DOI] [PubMed] [Google Scholar]
- 7.Murray CJ, Salomon JA. Expanding the WHO tuberculosis control strategy: rethinking the role of active case-finding. Int J Tuberc Lung Dis. 1998;2:S9–15. [PubMed] [Google Scholar]
- 8.Golub JE, Mohan CI, Comstock GW, Chaisson RE. Active case finding of tuberculosis: historical perspective and future prospects. Int J Tuberc Lung Dis. 2005;9:1183–203. [PMC free article] [PubMed] [Google Scholar]
- 9.Strobel M, Veasna D, Saykham M, Wei Z, Tran DS, Valy K, et al. Pleuro-pulmonary paragonimiasis. Med Mal Infect. 2005;35:476–81. doi: 10.1016/j.medmal.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Tran DS, Nanthapone S, Odermatt P, Strobel M. A village cluster of paragonimiasis in Vientiane Province, Lao PDR. Southeast Asian J Trop Med Public Health. 2004;35(suppl 1):323–6. [Google Scholar]
- 11.Odermatt P, Habe S, Manichanh S, Tran DS, Duong V.Zwang Wie, et alParagonimiasis and its intermediate hosts in a transmission focus in Lao People’s Democratic Republic. Acta Trop 2007In press 10.1016/j.actatropica.2007.05.015 [DOI] [PubMed] [Google Scholar]
- 12.Nsanzumuhire H, Lukwago EW, Edwards EA. 11. Stott H, Fox W, Sutherland I. A study of the use of community leaders in case-finding for pulmonary tuberculosis in the Machakos district of Kenya. Tubercle. 1977;58:117–28. doi: 10.1016/0041-3879(77)90012-5. [DOI] [PubMed] [Google Scholar]