Abstract
Objective
To assess whether the strategy of “a midwife in every village” in Indonesia achieved its aim of increasing professional delivery care for the poorest women.
Methods
Using pooled Demographic and Health Surveys (DHS) data from 1986–2002, we examined trends in the percentage of births attended by a health professional and deliveries via caesarean section. We tested for effects of the economic crisis of 1997, which had a negative impact on Indonesia’s health system. We used logistic regression, allowing for time-trend interactions with wealth quintile and urban/rural residence.
Findings
There was no change in rates of professional attendance or caesarean section before the programme’s full implementation (1986–1991). After 1991, the greatest increases in professional attendance occurred among the poorest two quintiles – 11% per year compared with 6% per year for women in the middle quintile (P = 0.02). These patterns persisted after the economic crisis had ended. In contrast, most of the increase in rates of caesarean section occurred among women in the wealthiest quintile. Rates of caesarean deliveries remained at less than 1% for the poorest two-fifths of the population, but rose to 10% for the wealthiest fifth.
Conclusion
The Indonesian village midwife programme dramatically reduced socioeconomic inequalities in professional attendance at birth, but the gap in access to potentially life-saving emergency obstetric care widened. This underscores the importance of understanding the barriers to accessing emergency obstetric care and of the ways to overcome them, especially among the poor.
Résumé
Objectif
Evaluer si la stratégie « Une sage-femme dans chaque village » mise en œuvre en Indonésie a atteint son objectif qui était de développer l’assistance de l’accouchement par des professionnels de la santé pour les femmes les plus pauvres.
Méthodes
A partir d’un ensemble de données d’enquêtes démographiques et sanitaires (EDS) réalisées entre 1986 et 2002, nous avons étudié l’évolution des pourcentages de naissances assistées par des professionnels de santé et de naissances obtenues par césarienne. Nous avons évalué l’impact négatif de la crise économique de 1997 sur le système de santé indonésien. Nous avons fait appel à la régression logistique en tenant compte des interactions entre les tendances temporelles d’une part et le quintile de richesse et le lieu de résidence (urbain ou rural) d’autre part.
Résultats
Aucune variation de la fréquence de l’assistance des accouchements par un professionnel de santé ou des taux de césarienne n’a été relevée avant la pleine mise en œuvre du programme (1986-1991). Après 1991, c’est parmi les deux quintiles les plus pauvres qu’on a observé le plus fort accroissement de fréquence de l’assistance des accouchements par un professionnel de santé, à savoir 11% par an par rapport à 6% par an pour les femmes appartenant au quintile moyen (p = 0,02). Ces schémas se sont maintenus après la fin de la crise économique. A l’inverse, les augmentations de taux de césarienne se sont produites principalement chez les femmes appartenant au quintile le plus riche. Les taux d’accouchement par césarienne sont restés inférieurs à 1% pour les deux quintiles les plus pauvres de la population, en revanche ce taux est passé à 10% pour le quintile le plus riche.
Conclusion
Le programme « Une sage-femme dans chaque village pour l’Indonésie » a permis de réduire considérablement les inégalités socioéconomiques en matière d’assistance des naissances par des professionnels de santé, mais les disparités dans l’accès à des soins obstétricaux susceptibles de sauver des vies se sont accrues. Cette constatation souligne à quel point il est important de comprendre les obstacles à l’évaluation des soins obstétricaux d’urgence et de trouver des moyens de les surmonter, notamment parmi les pauvres.
Resumen
Objetivo
Determinar si la estrategia de «una partera en cada aldea» aplicada en Indonesia logró su objetivo de aumentar la asistencia profesional en el parto entre las mujeres más pobres.
Métodos
A partir de un conjunto de datos combinados de las Encuestas de Demografía y Salud (DHS) de 1986–2002, examinamos la tendencia seguida por el porcentaje de nacimientos atendidos por un profesional sanitario y los partos por cesárea. Analizamos los efectos de la crisis económica de 1997, que perjudicó al sistema de salud de Indonesia. Empleamos métodos de regresión logística, teniendo en cuenta la influencia de los quintiles de riqueza y de la zona urbana/rural de residencia en las tendencias temporales.
Resultados
No se observó ningún cambio en las tasas de asistencia profesional o de práctica de cesáreas antes de la plena aplicación del programa (1986–1991). A partir de 1991, los mayores aumentos de la asistencia profesional se registraron entre los dos quintiles más pobres: 11% anual, frente al 6% entre las mujeres del quintil medio (P = 0,02). Esta tendencia se mantuvo después de la crisis económica. En cambio, la mayoría del aumento de las tasas de cesárea se dio entre las mujeres del quintil más rico. Las tasas de parto por cesárea siguieron siendo inferiores al 1% entre los dos quintiles más pobres de la población, mientras que aumentaron al 10% en el quintil más rico.
Conclusión
El programa de parteras de aldea llevado a cabo en Indonesia redujo extraordinariamente las desigualdades socioeconómicas en lo que respecta a la asistencia profesional en el parto, pero la brecha en el acceso a medidas de atención obstétrica de urgencia que salvan vidas se amplió. Ello subraya la necesidad de comprender mejor las barreras al acceso a ese tipo de atención y las alternativas para superarlas, sobre todo en la población pobre.
ملخص
الغرض
استەدفت ەذە الدراسة معرفة ما إذا كانت استراتيجية (( قابلة في كل قرية )) قد حققت ەدفەا في تحسين خدمات الإشراف على الولادة المقدمة لأفقر السيدات في إندونيسيا.
الطريقة
استخدمنا البيانات الناتجة عن المسوحات الديمغرافية والصحية للفترة 1986 – 2002 في دراسة الاتجاەات في النسبة المئوية للولادات التي تتم تحت إشراف مەني صحي، والولادات التي تتم بالجراحة القيصرية. وقمنا بتقصي التأثيرات السلبية للأزمة الاقتصادية التي شەدتەا إندونيسيا في عام 1997 على نظامەا الصحي. وقد استخدمنا طريقة التحوف اللوجستي، مع إتاحة التفاعل بين الزمن والاتجاە في ما يتعلق بأحوال الشرائح الخُمُسية لمستوى الثراء، والإقامة في الريف والحضر.
الموجودات
لم يلاحظ أي تغير في معدلات الإشراف المەني على الولادة أو في معدلات الولادة القيصرية قبل التنفيذ الكامل للبرنامج (1986 – 1991). وبعد عام 1991، حدثت أعلى زيادات في معدل الإشراف المەني بين أفقر شريحتين، بلغت 11% في العام بالمقارنة مع 6% في العام بالنسبة للسيدات في الشريحة المتوسطة (P = 0.02). واستمرت ەذە الأنماط بعد انتەاء الأزمة الاقتصادية. وعلى عكس ذلك، حدثت معظم الزيادة في معدلات الولادة القيصرية بين السيدات اللاتي ەن في الشريحة الأكثر ثراءً. وظلت معدلات الولادة القيصرية أقل من 1% بين الشريحتين الخُمُسيتين الأشد فقراً من السكان، ولكنەا ارتفعت إلى 10% بين الشريحة الخُمُسية الأكثر ثراءً.
الاستنتاج
أدى تنفيذ برنامج قابلة في كل قرية في إندونيسيا إلى خفض جذري في مظاەر التفاوت الاجتماعي والاقتصادي في تلقي خدمات الإشراف المەني على الولادات، غير أن الفجوة في الحصول على خدمات الرعاية التوليدية الطارئة المنقذة للحياة ازدادت اتساعاً. ويؤكد ذلك على أەمية فەم العقبات أمام الحصول على الرعاية التوليدية الطارئة وأەمية فەم طرق التغلب عليەا، ولاسيما بين الفقراء.
Introduction
Concerns about inequalities in maternal health and use of health services have attracted renewed attention in recent years.1 There are substantial socioeconomic disparities in access to professional delivery care in low- and middle-income countries.2 Not surprisingly, maternal mortality has a clear poverty gradient, both between and within countries.3,4 The task now is to develop effective and affordable programmes that make skilled delivery care, including emergency obstetric care, accessible to all women.
There are few examples of successful maternal health interventions aimed at the poor,5 and calls have been made for monitoring national programmes so that more can be learned about how to reduce inequalities effectively.6 The Indonesian village midwife programme, launched by the Indonesian Government in 1989, offers a unique opportunity to do so. The aim of the programme was to reduce maternal mortality by increasing the proportion of deliveries managed by trained professionals, particularly among poor rural populations. Every village in the country was to have a trained midwife who would operate as a multipurpose health-care provider, but with specific responsibility for pregnancy, delivery and postpartum care.7–9 By 1996, more than 50 000 midwives (96% of those needed) had been trained and posted.10 The percentage of births attended by a professional increased dramatically, even in rural areas, but whether the programme reached poorer groups is not known.11
The aim of this paper was to assess the extent to which the village midwife programme improved access to professional delivery care for the poorest people in Indonesia. We examined trends in two indicators: the percentage of births attended by a health professional and the percentage of deliveries via caesarean section. The goal of the programme was to reduce maternal mortality by increasing skilled attendance at birth – the proportion of deliveries managed by trained professionals – particularly among poor, rural populations. The rate of caesarean sections indicates whether the presence of village midwives improved access to emergency obstetric care. We provide context for these trends by testing for observable effects of the economic crisis of 1997, which had a negative impact on the Indonesian health system.12–14 By focusing our analysis on issues of equity in access to basic as well as emergency obstetric care and on the effects of the economic crisis, we provide novel insights into the ways the skilled attendance strategy in Indonesia may have served the poor.
Methods
Data
We used data from the Indonesian Demographic and Health Surveys (DHS) for the years 1991, 1994, 1997 and 2002.15 The 1987 survey was not included because it lacked information about caesarean sections. We analysed live births occurring during the 5 years before each survey, pooling data from the four surveys and thus covering births between 1986 and 2002. There were 66 727 deliveries resulting in live births in this sample; only one live birth per delivery was analysed.
Variables
Our analysis focused on whether a professional attendant was present at delivery, and whether the delivery was via caesarean section. Throughout the paper we refer to “professional attendants” rather than “skilled attendants” because the surveys did not assess the technical skills of birth attendants; only their professional category was identified. Doctors, nurses and midwives were classified as professional birth attendants. We could not separate village midwives from other professional midwives because a village midwife category was only included in the 2002 survey. For the data from 1991, 1994 and 1997, we excluded 493 implausible caesarean sections reported by women who stated that they delivered at home (0.97% of births in these surveys). This improved comparability to the 2002 survey, in which the “skip” pattern of the questionnaire automatically excluded women who delivered at home from being asked about caesarean sections.
To measure socioeconomic status, we developed a principal components wealth index.16 The principal components analysis used the pooled household-level DHS data files, which are representative of the entire Indonesian population between 1991 and 2002. We used all asset and housing variables that were available in all four surveys, including ownership of a radio or tape recorder, television set, bicycle or boat, motorized vehicle, and gas, electric or kerosene stove. Housing characteristics included source of water, time to nearest water source, availability of electricity, type of floor and type of toilet. Principal components’ scores are available from the authors upon request. Since our goal was to control for improvements in the overall economic status of the population over time, we used the wealth index to rank all households from the four pooled surveys and divided them into quintiles across the pooled data, rather than calculating survey-specific quintiles. The first quintile thus indicates the poorest 20% and the fifth quintile indicates the wealthiest 20% of the pooled population for the period 1991–2002; in the earlier surveys, more of the sample was concentrated in the lower quintiles, while in the later surveys more of the sample was concentrated in the higher economic quintiles because the wealth of the population was increasing over time.
Other dimensions of socioeconomic status were represented by the mother’s educational attainment and that of her husband, by region, by urban or rural residence and by the woman’s religion. Finally, we included the woman’s parity, her age at delivery and whether she delivered twins.
Analysis
All statistical analyses were conducted using Stata version 8. We first examined changes in the sociodemographic profile of the population over time, comparing proportions using a χ² test adjusted for survey clustering. In the descriptive analyses of trends in professional attendance and caesarean section, we used 3- and 4-year groupings of the year of birth, combining 1998 and 1999 into one group to represent the 2 years during which the economic crisis was most severe.17 For our adjusted regressions, we modelled time as a linear variable (assuming a constant change per year), allowing for changes in the trend at 1991, when the village midwife programme was fully under way, and at 1997, when the economic crisis began.
We used logistic regression to estimate crude and adjusted multivariate models for each outcome, using Wald tests to assess statistical significance and adjusting for survey clustering at the primary sampling unit level via the Huber-White robust variance estimator.18 We explored time trend interactions with wealth quintile, education and urban/rural residence to determine whether the odds of delivery by caesarean section and with a professional attendant were changing at the same rate in all socioeconomic groups and in urban and rural areas. Because more than half of all caesarean sections occurred among women in the wealthiest quintile, we modelled this interaction in two strata only, comparing trends in the wealthiest quintile with trends in the four poorer quintiles. To assist with interpretation of these interactions, we generated predicted probabilities from the final adjusted models, calculated average predicted probabilities by year of delivery and quintile, and plotted these against observed rates of professional attendance and caesarean section.
Results
Sociodemographic profile of the population
The Indonesian population underwent major sociodemographic changes during the four survey periods (Table 1). In the 1991 survey, 29% of the sample lived in urban areas, compared with 47% in the 2002 survey (P < 0.001). In 1991, 22% of the sample’s mothers and 30% of their husbands had some secondary or higher education, compared with 47% and 51% respectively in 2002. The proportion of the population falling within the poorest pooled quintile was 35% in 1991 compared with 9% in 2002.
Table 1. Distribution of sample by key social and demographic indicators.
| Indicator | Distribution (%)a according to year of survey |
P-valueb | ||||
|---|---|---|---|---|---|---|
| 1991 |
1994 |
1997 |
2002 |
|||
| (n = 15 594) | (n = 18 059) | (n = 17 302) | (n = 15 772) | |||
| Residence | ||||||
| Rural | 71 | 73 | 73 | 53 | ||
| Urban | 29 | 27 | 27 | 47 | 0.0000 | |
| Woman’s education | ||||||
| No education | 15 | 12 | 9 | 5 | ||
| Some primary education | 64 | 60 | 57 | 48 | ||
| Some secondary education | 20 | 25 | 30 | 41 | ||
| Some higher education | 2 | 3 | 4 | 6 | 0.0000 | |
| Husband’s education | ||||||
| No education | 9 | 8 | 5 | 3 | ||
| Some primary education | 61 | 57 | 53 | 45 | ||
| Some secondary education | 26 | 30 | 36 | 44 | ||
| Some higher education | 4 | 5 | 5 | 7 | 0.0000 | |
| Pooled wealth quintile | ||||||
| Quintile 1 (lowest SES) | 35 | 27 | 17 | 9 | ||
| Quintile 2 | 24 | 22 | 20 | 15 | ||
| Quintile 3 | 17 | 17 | 24 | 18 | ||
| Quintile 4 | 13 | 18 | 24 | 24 | ||
| Quintile 5 (highest SES) | 10 | 15 | 15 | 33 | 0.0000 | |
| Woman’s age at delivery (years) | ||||||
| < 20 | 15 | 14 | 14 | 12 | ||
| 20–29 | 58 | 56 | 55 | 56 | ||
| 30–39 | 24 | 27 | 28 | 28 | ||
| ≥ 40 | 2 | 3 | 3 | 3 | 0.0000 | |
| Parity at delivery | ||||||
| 1 | 29 | 29 | 33 | 35 | ||
| 2–5 | 59 | 57 | 57 | 57 | ||
| ≥ 6 | 13 | 14 | 10 | 8 | 0.0000 | |
| Total | 100 | 100 | 100 | 100 | ||
SES, socioeconomic status. a All percentages were calculated using sample weights. The unit of analysis was live births in the past 5 years. b P-values are from χ² tests for differences by survey, adjusted for survey clustering.
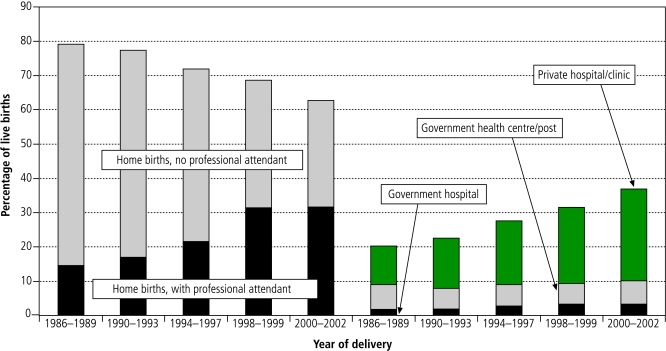
Crude trends by place of birth
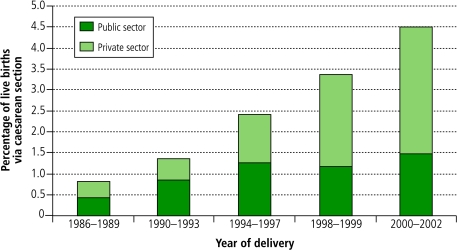
The percent of live births attended by a health professional nearly doubled over the 16-year period, from 35% (1986–1989) to 69% (2000–2002) of live births. Home births attended by a health professional increased from 14% in 1986–1989 to 32% in 2000–2002, while health facility births increased from 20% to 37% over the same period (Fig. 1). The entire increase in facility births occurred in private facilities. Similarly, caesarean section rates rose steadily over time (from 0.8% in 1986–1989 to 4.5% in 2000–2002), with an increasing share taking place in the private sector (Fig. 2). There was no apparent decrease in rates of professional attendance at birth or caesarean section during the economic crisis in 1998–1999.
Fig. 1.
Trends in location of births in Indonesia 1986–2002, by type of provider and presence of skilled attendant
Source: Demographic and Health Surveys, Indonesia, Reference 15.
Fig. 2.
Trends in rates of caesarean section in Indonesia 1986–2002, by public or private sector
Source: Demographic and Health Surveys, Indonesia, Reference 15.
Adjusted time trends
Table 2 (available at: http://www.who.int/bulletin volumes/85/10/06-033472) summarizes regression results for professional attendance and caesarean sections. There was no annual change in professional attendance at birth before the village midwife programme (1986–1991) (adjusted odds ratio, OR, 0.98 per year; P = 0.143). From 1991 to 1997, professional attendance at birth increased dramatically by 12% per year in the unadjusted analysis (a significant change compared with the trend in the previous period, P < 0.001). The trend was somewhat attenuated after adjusting for sociodemographic variables (adjusted odds increased by 7% per year; P < 0.001), suggesting that changes in the population’s economic and demographic profile did explain part of the observed increase in professional birth attendance over time. After the onset of the economic crisis in 1997, the rise in the odds of professional attendance at birth was sustained at 14% per year, though part of this increase was accounted for by sociodemographic change (adjusted trend, 5% per year). There was no significant change in the trend between 1991–1997 and 1997–2002 (P = 0.298).
Table 2. Determinants of professional attendance at birth and caesarean section, Indonesia 1986–2002.
| Variable | Births with professional attendance |
Births via caesarean section |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| % of live births | Crude OR | 95% CI | Adjusted ORa | 95% CI | % of live births | Crude OR | 95% CI | Adjusted ORa | 95% CI | ||
| Linear trends per yearb | |||||||||||
| 1986–1991 | 1.01 | (0.98–1.04) | 0.98 | (0.95–1.01) | 1.03 | (0.95–1.12) | 1.01 | (0.93–1.09) | |||
| 1991–1997 | – | 1.12 | (1.11–1.14) | 1.07 | (1.06–1.09) | – | 1.15 | (1.11–1.20) | 1.08 | (1.04–1.12) | |
| 1997–2002 | 1.14 | (1.10–1.17) | 1.05 | (1.02–1.08) | 1.06 | (1.02–1.11) | 0.99 | (0.94–1.03) | |||
| Wealth quintiles | |||||||||||
| Quintile 1 (lowest SES) | 16 | 1.00 | – | 1.00 | – | 0.4 | 1.00 | – | 1.00 | – | |
| Quintile 2 | 28 | 2.32 | (2.13–2.53) | 1.77 | (1.63–1.92) | 0.7 | 1.85 | (1.31–2.62) | 1.39 | (0.97–1.99) | |
| Quintile 3 | 45 | 5.47 | (4.97–6.02) | 3.14 | (2.86–3.45) | 1.0 | 4.64 | (3.36–6.40) | 2.44 | (1.74–3.42) | |
| Quintile 4 | 66 | 14.60 | (13.12–16.25) | 5.61 | (5.06–6.23) | 2.4 | 9.91 | (7.29–13.47) | 3.26 | (2.30–4.61) | |
| Quintile 5 (highest SES) | 89 | 54.11 | (47.57–61.54) | 11.40 | (9.99–13.01) | 6.9 | 24.61 | (18.21–33.25) | 4.34 | (3.02–6.22) | |
| Woman’s education | |||||||||||
| No education | 16 | 1.00 | – | 1.00 | – | 0.3 | 1.00 | – | 1.00 | – | |
| Some primary education | 35 | 3.14 | (2.89–3.50) | 1.67 | (1.51–1.84) | 0.9 | 3.74 | (2.39–5.85) | 2.17 | (1.36–3.47) | |
| Some secondary education | 78 | 15.95 | (14.15–17.99) | 3.14 | (2.80–3.53) | 3.9 | 15.02 | (9.54–23.64) | 3.28 | (1.99–5.39) | |
| Some higher education | 97 | 149.49 | (114.54–195.11) | 6.61 | (5.01–8.74) | 13.5 | 52.17 | (32.80–82.97) | 4.30 | (2.57–7.18) | |
| Husband’s education | |||||||||||
| No education | 14 | 1.00 | – | 1.00 | – | 0.2 | 1.00 | – | 1.00 | – | |
| Some primary education | 32 | 3.23 | (2.84–3.68) | 1.36 | (1.21–1.54) | 0.9 | 3.46 | (1.98–6.04) | 1.56 | (0.87–2.80) | |
| Some secondary education | 71 | 13.07 | (11.43–14.95) | 2.12 | (1.86–2.41) | 3.2 | 12.30 | (7.07–21.39) | 1.93 | (1.07–3.49) | |
| Some higher education | 94 | 75.93 | (61.86–93.20) | 3.59 | (2.94–4.38) | 11.0 | 40.86 | (23.29–71.69) | 2.66 | (1.45–4.87) | |
| Residence | |||||||||||
| Rural | 34 | 1.00 | – | 1.00 | – | 1.0 | 1.00 | – | 1.00 | – | |
| Urban | 76 | 7.63 | (6.86–8.48) | 2.68 | (2.43–2.95) | 4.7 | 5.59 | (4.81–6.49) | 1.82 | (1.53–2.16) | |
a CI, confidence interval; OR, odds ratio; SES, socioeconomic status. a These models were also adjusted for a woman’s age at delivery, parity, twin births, region, and religion (results not shown). b The confidence intervals for the linear time trends indicate that we are 95% confident that a given annual odds ratio falls within this range.
The annual trend in caesarean section rates was also flat before 1991 (crude annual OR, 1.03), but increased dramatically after 1991 (crude annual OR for 1991–1997, 1.15; adjusted OR, 1.08). The change in the trend after 1991 is significant in the crude (P = 0.045) but not in the adjusted analysis (P = 0.234). There was a significant downward shift in the trend for rates of caesarean section after the onset of the economic crisis. In the crude analysis, rates of caesarean section still increased after 1997 (OR = 1.06, P-value for the change in trend from 1991–1997 to 1997–2002, 0.019), but socioeconomic factors played a massive role since the adjusted trend was flat (OR = 0.99; P = 0.016).
Demographic and socioeconomic determinants
The socioeconomic status of the mother was a major determinant of professional attendance at birth and caesarean section delivery. Nearly 90% of women in the wealthiest quintile gave birth with a health professional in attendance, compared with only 16% in the poorest quintile (adjusted OR, 11.40). The disparities were even greater according to mothers’ and husbands’ educational achievement, although these differences were strongly reduced after adjustment (crude OR for mother’s education, 149.49; adjusted OR, 6.61). Inequities in rates of caesarean section were substantial, with only 1% or fewer of women in the poorest three quintiles having a caesarean section, compared with 7% in the wealthiest quintile (adjusted OR, 4.34). Caesarean section among women with higher education reached rates of 13.5%, compared with only 0.3% for those without education (adjusted OR, 4.30).
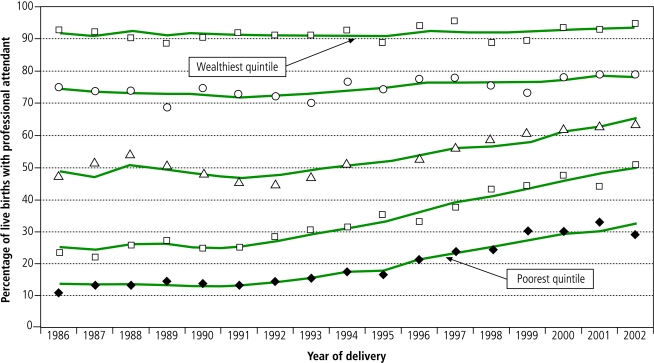
Trends by wealth, mother’s education and urban/rural residence
After 1991, increases in professional attendance occurred at significantly different rates in different wealth strata (Table 3, Fig. 3). Notably, the greatest increases in rates of professional attendance occurred among the two quintiles with the lowest socioeconomic status. From 1991 to 1997, professional attendance in the latter increased on average by 11% per year, compared with only 6% per year for women in the middle quintile (P-value for the difference = 0.02) and 4% per year for the fourth quintile (P < 0.001). There was no change over time in rates of professional attendance at delivery for the richest quintile during this period (P < 0.001). From 1997 to 2002, these differences by wealth strata persisted, with rates increasing significantly more quickly among poorer than wealthier women. In essence, the gap in access to professional attendance between rich and poor narrowed during this time (Fig. 3).
Table 3. Trends in determinants of professional attendance at birth and caesarean section according to wealth quintile or urban/rural residence, Indonesia 1986–2002.
| Period | Strata of interaction | Professional attendance |
Caesarean section |
|||
|---|---|---|---|---|---|---|
| OR | 95% CIa | OR | 95% CIa | |||
| Annual trends by wealth quintileb | ||||||
| 1986–1991 | All quintiles | 0.98 | (0.95–1.00) | 1.01 | (0.93–1.10) | |
| 1991–1997 | Lowest four quintiles combined | – | – | 1.05 | (1.00–1.11) | |
| Quintile 1 (lowest SES) | 1.11 | (1.08–1.15) | – | – | ||
| Quintile 2 | 1.11 | (1.08–1.14) | – | – | ||
| Quintile 3 | 1.06 | (1.04–1.09) | – | – | ||
| Quintile 4 | 1.04 | (1.01–1.06) | – | – | ||
| Quintile 5 (highest SES) | 0.99 | (0.95–1.04) | 1.10 | (1.05–1.15) | ||
| 1997–2002 | Poorest four quintiles combined | – | – | 0.94 | (0.88–1.01) | |
| Quintile 1 (lowest SES) | 1.09 | (1.02–1.16) | – | – | ||
| Quintile 2 | 1.08 | (1.04–1.14) | – | – | ||
| Quintile 3 | 1.06 | (1.02–1.11) | – | – | ||
| Quintile 4 | 1.00 | (0.96–1.05) | – | – | ||
| Quintile 5 (highest SES) | 1.04 | (0.98–1.11) | 1.01 | (0.95–1.07) | ||
| Annual trends by urban/rural residenceb | ||||||
| 1986–1991 | All areas | 0.98 | (0.96–1.01) | 1.01 | (0.93–1.09) | |
| 1991–1997 | Rural areas | 1.09 | (1.07–1.11) | 1.09 | (1.03–1.15) | |
| Urban areas | 1.03 | (0.99–1.06) | 1.07 | (1.03–1.12) | ||
| 1997–2002 | Rural areas | 1.08 | (1.05–1.12) | 0.98 | (0.90–1.05) | |
| Urban areas | 0.98 | (0.93–1.03) | 0.99 | (0.94–1.05) | ||
OR, odds ratio; SES, socioeconomic status. a 95% confidence intervals (CI) are meant to help the reader gauge whether a particular annual trend is statistically different from 1.0. For P-values that measure whether the trend in one period is different from the trend in another period, or whether the trends are significantly different by strata, please see text. b Both models were also adjusted for the respondent’s education, partner’s education, woman’s age at delivery, parity, twin births, region, and religion (results not shown). The first model was also adjusted for urban/rural residence, and the second was also adjusted for wealth quintile.
Fig. 3.
Trends in ratesa of professional attendance in Indonesia 1986–2002, by wealth quintile
a Predicted rates were calculated from the adjusted logistic regression model and overlaid on observed rates, by quintile and year.
Source: Demographic and Health Surveys, Indonesia, Reference 15.
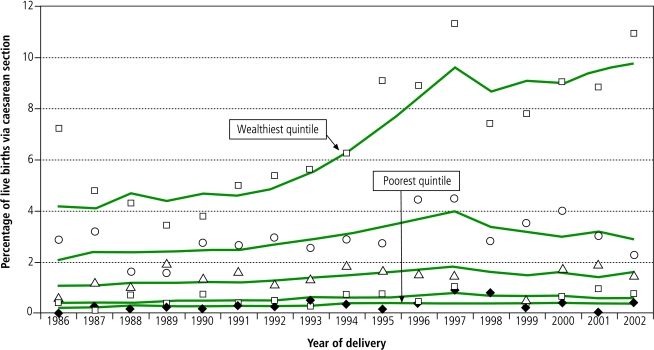
In contrast, most of the increase in rates of caesarean section occurred among women in the wealthiest fifth of the population (Table 3, Fig. 4). Before the crisis (1991–1997), the likelihood of a caesarean section increased by about 5% per year for women in the bottom four-fifths of the population, while this likelihood increased by about 10% per year for women in the top fifth (P-value for difference in trends = 0.19). After 1997, the trend was decreasing for those in the bottom four quintiles (OR, 0.94) and stable for women in the wealthiest quintile (OR, 1.01; P-value for difference in trends = 0.008). Rates of caesarean section remained at less than 1% for the bottom two-fifths of the population, while the richest fifth sustained caesarean section rates of 10% (Fig. 4). Trends within strata of mother’s level of education echo findings for wealth quintiles (data not shown).
Fig. 4.
Trends in ratesa of caesarean section in Indonesia 1986–2002, by wealth quintile
a Predicted rates were calculated from adjusted logistic regression model and overlaid on observed rates, by quintile and year.
Source: Demographic and Health Surveys, Indonesia, Reference 15.
Finally, because the village midwife programme was primarily a rural programme, we also tested interactions between time trends and area of residence. As expected, from 1991 to 1997, the odds of professional attendance increased significantly more rapidly in rural areas (adjusted annual OR, 1.09) than urban areas (adjusted annual OR, 1.03; P-value for difference in trends = 0.001). This disparity persisted after 1997, with continuing increases in rural areas (adjusted annual OR, 1.08) and no growth in urban areas (adjusted annual OR, 0.98; P-value for difference in trends < 0.001). By contrast, for caesarean sections there were no statistically significant differences between urban and rural trends in either time period (P-value for difference in trends = 0.688 (1991–1997) and 0.915 (1997–2002).
Discussion
The national strategy to increase skilled attendance at birth was successful in reaching the poor in Indonesia. Use of a professional attendant at birth increased dramatically among the poorest 40% of the population and those living in rural areas, considerably narrowing the gap between poor and rich in this regard. However, these trends obscure the huge unmet need for access to emergency obstetric care among the large majority of the population, as the increase in rates of caesarean section was almost solely concentrated among the richest segments of the population.
The dramatic effect on professional attendance at birth is not surprising given the huge investment in the training and deployment of midwives in rural areas. There were some 15 000 community midwives in villages in 1991, increasing to 54 000 by 1997.10,19 With a total rural population of 129 million, this represents a ratio of one village midwife per 2389 population, or roughly one per 54 births per year. This is far in excess of the international recommendation of one midwife per 175 births.20 Compounded by the recent decline in the total number of births,21 this density of providers no doubt contributed to their increased use. The wealthier segments of society, on the other hand, had already achieved such high rates of professional attendance in the late 1980s that further improvements were barely attainable.
That the trends in professional attendance at birth among the poorest quintiles were sustained during the economic crisis is remarkable. After the crisis hit the country in 1997, incomes fell, prices of basic goods increased and the government’s expenditure on health and education declined.12,17 The purported effects of the crisis on health-care use have been contradictory, but there were reports of declining use of government-run health centres and village health posts.17 However, some strategies to mitigate the effects of the crisis on the health of the poor may have protected the midwife programme. For example, the resources allocated to essential health services such as the village midwife were maintained, and funds were made available so that poor and vulnerable members of the population could be exempt from user fees. The extent to which this social safety net has been effective is not known, but it almost certainly contributed to increased access for poorer groups.12,22
In contrast, there is little evidence that the village midwife programme has increased access to emergency obstetric care among the poor. Although not all caesarean sections are necessarily life-saving, caesarean section rates of less than 1% indicate an unmet need for potentially life-saving care.4,23 Where caesareans are uncommon, the majority are done to save the woman’s life.24 In Indonesia, the poorest two-fifths of the population sustained these low caesarean section rates for 16 years, and the economic crisis may have worsened the situation. With the programme’s emphasis on outreach services at the woman’s home, access to emergency obstetric care in hospitals has remained relatively neglected. Furthermore, public hospitals in Indonesia have increasingly gained autonomous status since 1991, and are as a result required to raise more revenue in the form of user fees.25 Higher user fees may have increased the costs of emergency obstetric care23 with potentially serious consequences for equity in access to caesarean sections. Although emergency obstetric care was covered by the social safety net after the economic crisis in 1997, our results do not suggest that such care was assured by this programme.
Interestingly, about half the increase in professional attendance occurred in health facilities, challenging the assumption that women prefer to give birth at home.9 Sustained economic growth since the 1970s, substantially declining rates of poverty26,27 and strong increases in female literacy may all have contributed to changing cultural preferences. Shifts from home- to facility-based births may be difficult to reverse once they occur.28
Our study has some limitations. First, women may have misclassified their birth attendant since they may not be able to distinguish professionals from other providers. Such errors are probably uncommon, however, since there is no intermediate cadre of obstetric care-providers in Indonesia, and women are not likely to misreport the presence of a traditional birth attendant. Second, the exclusion from the survey of women who died during pregnancy or delivery may have biased the results, particularly if these women were more likely to give birth with a skilled attendant or by caesarean. However, their numbers would be extremely small and the bias negligible. Third, the number of home-based caesarean sections in the early surveys points to some problems with the validity of reporting of caesarean sections; excluding them from our analysis was essential to improve the consistency of the data.
In addition, while the programme has been successful in increasing the use of trained professionals for birth, not all trained professionals are sufficiently skilled,29,30 and they may lack the supportive environment essential for the provision of skilled care.31 Great caution is required in inferring that health outcomes improved as a result of the programme. The construction of a pooled asset score over a 16-year period, ignoring the possibly changing value of assets over time, may have led to misclassification of socioeconomic status. Some authors have suggested that the ranking of households is robust to the asset items included,16 while others have suggested the opposite.32 However, the changes in the distribution of wealth groups over time is consistent with the rapid economic growth in Indonesia during this time.26,27
The strategy of a midwife in every village has dramatically reduced socioeconomic inequalities in professional attendance at births, but the gap in access to potentially life-saving emergency obstetric care may have nonetheless widened. This underlies the importance of monitoring rates of caesarean section as well as professional attendance, particularly among those living in poverty. Future research should examine the barriers to accessing emergency obstetric care in Indonesia and ways to overcome them. The effectiveness of the village midwife programme in achieving its ultimate goals – reducing maternal and perinatal morbidity and mortality – also remains to be measured. ■
Footnotes
Competing interests: None declared.
References
- 1.Gwatkin DR, Bhuiya A, Victora C. Making health systems more equitable. Lancet. 2004;364:1273–80. doi: 10.1016/S0140-6736(04)17145-6. [DOI] [PubMed] [Google Scholar]
- 2.Gwatkin DR, Johnson K. A, Rutstein S, Pande R. Socioeconomic differences in health, nutrition, and population. Washington: World Bank; 2000. [Google Scholar]
- 3.Graham WJ, Fitzmaurice AE, Bell JS, Cairns JA. The familial technique for linking maternal death with poverty. Lancet. 2004;363:23–7. doi: 10.1016/S0140-6736(03)15165-3. [DOI] [PubMed] [Google Scholar]
- 4.DeBrouwere V, Van Lerberghe W. [Unmet obstetric needs]. Paris: L’Harmattan; 1998. [Google Scholar]
- 5.Manandhar DS, Osrin D, Shrestha BP, Mesko N, Morrison J, Tumbahangphe KM, et al. Effect of a participatory intervention with women’s groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet. 2004;364:970–9. doi: 10.1016/S0140-6736(04)17021-9. [DOI] [PubMed] [Google Scholar]
- 6.Yazbeck A, Gwatkin D, Wagstaff A, Qamruddin J. Why were the reaching the poor studies undertaken? In: Gwatkin D, Wagstaff A, Yazbeck A, eds. Reaching the poor with health, nutrition and population services: what works, what doesn’t, and why. Washington: World Bank; 2005. [Google Scholar]
- 7.Shiffman J. Generating political will for safe motherhood in Indonesia. Soc Sci Med. 2003;56:1197–207. doi: 10.1016/S0277-9536(02)00119-3. [DOI] [PubMed] [Google Scholar]
- 8.Hull T, Widayatun, Raharto A, Setiawan B. Neither dukun nor doctor: Some problems of the village midwife programme in eastern Indonesia. Australian Council for Overseas Aid Development Bulletin 1998;48.
- 9.Geefhuysen C. Safe motherhood in Indonesia: a task for the next century. In: Berer M, Raminshan T, eds. Safe motherhood initiatives: critical issues. London: Blackwell Science; 1999. [Google Scholar]
- 10.Indonesia: health profile 1997. Jakarta: Centre for Health Data, Ministry of Health; 1997.
- 11.Bell J, Curtis S, Alayon S. Trends in delivery care in six countries (DHS Analytical Studies No. 7). Calverton: ORC Macro and International Research Partnership for Skilled Attendance for Everyone (SAFE); 2003. [Google Scholar]
- 12.Simms C, Rowson M. Reassessment of health effects of the Indonesian economic crisis: donors versus the data. Lancet. 2003;361:1382–5. doi: 10.1016/S0140-6736(03)13076-0. [DOI] [PubMed] [Google Scholar]
- 13.Indonesia health strategy in a post-crisis, decentralizing Indonesia (Report No. 21318-IND). Washington: World Bank; 2000.
- 14.Frankenberg E, Thomas D, Beegle K. The real cost of Indonesia’s economic crisis: preliminary findings from the Indonesia Family Life Surveys (Labor and Population Program Working Paper Series 99-04). Santa Monica: RAND; 1999.
- 15.Demographic and Health Surveys. Indonesia. Washington: Macro International; 2006. Available at: http://www.measuredhs.com/aboutsurveys/search/search_survey_main.cfm?SrvyTp=type&listtypes=1
- 16.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data — or tears: an application to educational enrolments in states of India. Demography. 2001;38:115–32. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 17.Waters H, Saadah F, Pradhan M. The impact of the 1997–98 East Asian economic crisis on health and health care in Indonesia. Health Policy Plan. 2003;18:172–81. doi: 10.1093/heapol/czg022. [DOI] [PubMed] [Google Scholar]
- 18.White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817–38. doi: 10.2307/1912934. [DOI] [Google Scholar]
- 19.Staff appraisal report Indonesia: fifth population project (family planning and safe motherhood). Washington: World Bank; 1991. [Google Scholar]
- 20.The world health report 2005: make every mother and child count. Geneva: WHO; 2005. [DOI] [PubMed]
- 21.World population prospects: the 2006 revision (database). New York: United Nations; 2007. Available at: http://esa.un.org/unpp
- 22.Pradhan M, Saadah F, Sparrow R. Did the healthcard program ensure access to medical care for the poor during Indonesia’s economic crisis? Tinbergen Institute Discussion Paper 03-016. Amsterdam: Tinbergen Institute; 2004.
- 23.Ronsmans C, Achadi E, Supratikto G, Zazri A, McDermott J, Koblinsky M, et al. Evaluation of a comprehensive home-based midwifery programme in South Kalimantan, Indonesia. Trop Med Int Health. 2001;6:799–810. doi: 10.1046/j.1365-3156.2001.00780.x. [DOI] [PubMed] [Google Scholar]
- 24.Dubourg D, Derveeuw M, Litt V, De Brouwere V, Van Lerberghe W. The UON network: tackling unmet need for major obstetric interventions (online). Available at: http://www.uonn.org
- 25.Hanson K, Archard L, McPake B. Creating markets in hospital care: the adoption of developed country health sector reforms by developing countries. Is it appropriate? Trop Med Int Health. 2001;6:747–8. doi: 10.1046/j.1365-3156.2001.00808.x. [DOI] [PubMed] [Google Scholar]
- 26.Hill H. The Indonesian economy since 1966: Southeast Asia’s emerging giant. Cambridge: Cambridge University Press; 1996. [Google Scholar]
- 27.Indonesia Human Development Report 2001: towards a new consensus. Democracy and human development in Indonesia. Jakarta: Central Ministry of Statistics, Ministry of National Development Planning, and United Nations Development Programme; 2001.
- 28.Koblinsky MA, Campbell O, Heichelheim J. Organizing delivery care: what works for safe motherhood? Bull World Health Organ. 1999;77:399–406. [PMC free article] [PubMed] [Google Scholar]
- 29.Setiarini A, Khusan H, Guarenti L, Batubara I. Needs assessment for obstetric and neonatal emergency care provision in Serang district. Jakarta: Ministry of Health/WHO; 2003. [Google Scholar]
- 30.Sadjimin D. Assessment of clinical skills of village midwives in ASUH program districts. Jakarta: Program for Appropriate Technology in Health; 2003. [Google Scholar]
- 31.Graham WJ, Bell JS, Bullough CHW. Can skilled attendance at delivery reduce maternal mortality in developing countries? In: De Brouwere V, Van Lerberghe W, eds. Safe motherhood strategies: a review of the evidence. Antwerp: ITG Press; 2001:97-130. [Google Scholar]
- 32.Houweling TA, Kunst AE, Mackenbach JP. Measuring health inequality among children in developing countries: does the choice of the indicator of economic status matter? Int J Equity Health. 2003;2:8. doi: 10.1186/1475-9276-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]