Abstract
Objective
In the past ten years effective treatments for pre-eclampsia and eclampsia have been evaluated and identified following large trials and systematic reviews. We investigated the extent of those effective interventions’ implementation.
Methods
Descriptive analysis of data collected as part of a cluster randomized trial. The trial was assigned the International Standardised Randomized Controlled Trial Number ISRCTN 14055385. Hospitals with more than 1000 deliveries per year not directly associated with an academic institution in Mexico City municipal area in Mexico (n = 22) and the north-east region of Thailand (n = 18) were included. All women delivering at the participating hospitals at two time periods in 2000 and 2002 contributed data on practice rates. The use of magnesium sulfate for pre-eclampsia and eclampsia were the outcomes.
Findings
Eight out of 22 hospitals in Mexico (range 0.8% to 8.5%) and all 18 hospitals in Thailand (range 18.6% to 63.6%) used magnesium sulfate for women with pre-eclampsia. In Mexico, 11 of 22 hospitals used magnesium sulfate for eclampsia (range 9.1% to 60.0%). In Thailand, all 17 hospitals having eclampsia cases used magnesium sulfate (range 25% to 100%).
Conclusion
Despite compelling evidence, magnesium sulfate use is below desired levels. Clinical practices should be audited and implementation of this effective intervention should be taken up as a priority where universal implementation is not in place.
Résumé
Objectif
Au cours de la dernière décennie, des essais de grande ampleur et des revues systématiques de la littérature ont permis d’évaluer et d’identifier des traitements efficaces contre la prééclampsie et l’éclampsie. Nous avons examiné dans quelle mesure ces interventions efficaces étaient appliquées.
Méthodes
Analyse descriptive des données recueillies dans le cadre d’un essai randomisé par grappes, ayant reçu le numéro d’essai contrôlé randomisé reconnu au plan international ISRCTN 14055385. Ont participé à l’étude les hôpitaux pratiquant plus de 1000 accouchements par an et non-associés directement à un établissement d’enseignement supérieur de la municipalité de Mexico (Mexique) (n = 22) et de la région nord-est de la Thaïlande (n = 18). Des données sur les fréquences de certaines pratiques ont été recueillies pour toutes les femmes ayant accouché dans les hôpitaux participant à l’étude pendant l’une des deux périodes étudiées, 2000 et 2002. L’étude visait à déterminer les taux d’utilisation du sulfate de magnésium contre la prééclampsie et l’éclampsie.
Résultats
Huit des vingt-deux hôpitaux de Mexico (taux d’utilisation : 0,8 - 8,5%) et la totalité des 18 hôpitaux thaïlandais (taux d’utilisation : 18,6 - 63,6%) utilisaient du sulfate de magnésium pour traiter les femmes dans un état prééclamptique. Dans la municipalité de Mexico, 11 des 22 hôpitaux faisaient appel à ce produit contre l’éclampsie (taux d’utilisation : 9,1 - 60,0%). En Thaïlande, la totalité des 17 hôpitaux accueillant des cas d’éclampsie ont utilisé du sulfate de magnésium (taux d’utilisation : 25 -100%).
Conclusion
Malgré les preuves éloquentes de son utilité, la fréquence d’administration du sulfate de magnésium est encore inférieure au niveau souhaitable. Une inspection des pratiques cliniques devrait être réalisée et la mise en œuvre de cette intervention efficace devrait être considérée comme une priorité partout où elle n’est pas universelle.
Resumen
Objetivo
En los últimos diez años se han evaluado e identificado los tratamientos más eficaces para la preeclampsia y la eclampsia mediante grandes ensayos y revisiones sistemáticas. Decidimos investigar el grado de aplicación de esas intervenciones eficaces.
Métodos
Se llevó a cabo un análisis descriptivo de datos recopilados como parte de un ensayo aleatorizado por conglomerados. Se incluyeron en el ensayo -código ISRCTN (International Standardised Randomized Controlled Trial Number) 14055385- hospitales con más de 1000 partos al año no vinculados directamente a instituciones académicas situados en el término municipal de Ciudad de México (n = 22) y en el noreste de Tailandia (n = 18). Todas las mujeres que dieron a luz en los hospitales participantes en dos periodos de 2000 y 2002 aportaron datos sobre la atención recibida. Los resultados considerados fueron el uso de sulfato de magnesio contra la preeclampsia y contra la eclampsia.
Resultados
Ocho de los 22 hospitales de México (intervalo: 0,8% - 8,5%) y los 18 hospitales de Tailandia (intervalo: 18,6% - 63,6%) trataron con sulfato de magnesio a las mujeres con preeclampsia. En México, 11 de los 22 hospitales utilizaron sulfato de magnesio contra la eclampsia (intervalo: 9,1% - 60,0%). En Tailandia, la totalidad de los 17 hospitales con casos de eclampsia administraron sulfato de magnesio (intervalo: 25% - 100%).
Conclusión
Pese a lo contundente de la evidencia, el uso de sulfato de magnesio es inferior a lo deseable. Es necesario revisar la práctica clínica, y la aplicación de esta intervención eficaz debería considerarse una prioridad en los casos en que no se ha implantado de forma universal.
ملخص
الغرض
تم في السنوات العشر الماضية تحديد وتقيـيم عمليات المعالجة الفعَّالة لمقدِّمات الارتعاج والارتعاج، بعد تجارب ودراسات منەجية موسَّعة. وقد استەدفت ەذە الدراسة تقصِّي مدى تنفيذ تلك التدخلات الفعَّالة.
الطريقة
استُخدم في الدراسة التحليل الوصفي للبيانات التي جُمعت في إطار تجربة عنقودية معشاة. وقد أُعطي لەذە التجربة رقم 14055385 ISRCTN، وەو يمثِّل الرقم الدولي المعياري للتجارب المعشاة المضبطة بالشواەد. وقد شملت التجربة المستشفيات التي يزيد عدد الولادات التي تُجرى بەا في كل عام على 1000 ولادة، والتي لا ترتبط مباشرةً بأي مؤسسة أكاديمية، وذلك في كلٍ من المنطقة البلدية لمدينة مكسيكوسيتي بالمكسيك (وعددەا 22 مستشفى)، ومنطقة شمال شرقي تايلاند (وعددەا 18 مستشفى). وقد قدَّمت جميع السيدات اللاتي ولدن في المستشفيات المشاركة في الدراسة في فتـرتَيْن زمنيَّتَيْن، ەما عاما 2000 و2004، بيانات عن معدلات إعطاء سلفات المغنيزيوم. وكان معدل استخدام سلفات المغنيزيوم لمعالجة الارتعاج ومقدِّمات الارتعاج ەو حصيلة البيانات.
الموجودات
تبيَّن أن 8 مستشفيات من جملة 22 مستشفى في المكسيك (بمجال يتـراوح من %0.8 إلى %8.5)، وأن جميع مستشفيات تايلاند البالغ عددەا 18 مستشفى (بمجال يتـراوح من %18.6 إلى %63.6) قد أعطت سلفات المغنيزيوم للسيدات اللاتي عانين من مقدِّمات الارتعاج. وفي المكسيك، أعطى 11 مستشفى من جملة 22 مستشفى سلفات المغنيزيوم لمعالجة الارتعاج (بمجال يتـراوح من %9.1 إلى %60). وأما في تايلاند، فقد أعطت جميع المستشفيات التي واجەت حالات ارتعاج، والبالغ عددەا 17 مستشفى، سلفات المغنيزيوم (بمجال يتـراوح من %25 إلى %100).
الاستنتاج
برغم البيِّنات القاطعة، لايزال استخدام سلفات المغنيزيوم دون المستويات المنشودة. وينبغي مراجعة الممارسات السريرية في ەذا الشأن، وإعطاء أولوية لتنفيذ ەذە الممارسة الفعَّالة في المناطق التي لا تنفَّذ فيەا بشكل شامل.
Introduction
Pre-eclampsia is a multiple organ disorder of unknown etiology usually associated with raised blood pressure and proteinuria. Eclampsia, the occurrence of one or more convulsions (fits), is a rare but serious complication in patients with pre-eclampsia. Pre-eclampsia/eclampsia remains one of the leading problems that threaten safe motherhood, particularly in developing countries. It was estimated that hypertension complicates approximately 5% of all pregnancies and 11% of all first pregnancies.1 Based on these estimations and case fatality rates, up to 40 000 women could die from pre-eclampsia and eclampsia each year.1
In a systematic review involving six trials (11 444 women) magnesium sulfate significantly reduced the risk of eclampsia (relative risk, RR 0.41; 95% confidence interval, CI: 0.29–0.58) and the risk of maternal death (RR 0.54; 95% CI: 0.26–1.10) among patients with pre-eclampsia although the latter was not statistically significant.2,3 Magnesium sulfate was more effective than phenytoin for reducing the risk of eclampsia among patients with pre-eclampsia (two trials, 2241 women; RR 0.05; 95% CI: 0.00–0.84).2
Magnesium sulfate appears to be substantially more effective than phenytoin (six trials, 897 women)4 or diazepam (seven trials, 1441 women)5 for the treatment of eclampsia. Magnesium sulfate is therefore the anticonvulsant of choice for both prevention and treatment of eclampsia.1
Implementing magnesium sulfate for the prevention and treatment of eclampsia in low- and middle-income countries could potentially benefit hundreds of thousands of women.6 This study aims to evaluate the use of magnesium sulfate for women with pre-eclampsia and eclampsia in Mexico and Thailand, where a cluster randomized trial to evaluate an educational strategy to change obstetric practices was conducted. The study methodology was published in detail elsewhere.7 The main results related to the effects of the intervention was published separately.8
Methods
The study was conducted in two countries: the Mexico City municipal area, Mexico, and the north-east region of Thailand. Maternity units of hospitals with > 1000 deliveries/year that were not associated directly with a university or other academic/research department were eligible to participate. In Mexico, all state and social security hospitals in the Mexico City municipal area were approached. Twenty-two out of 34 hospitals approached were eligible and agreed to participate in the trial. In Thailand, 18 hospitals out of 19 in the north-east region agreed to participate. There were therefore 40 hospitals in this study. The objective of the main trial was to evaluate the improvement in obstetric practices using an active dissemination strategy to promote uptake of recommendations contained in the WHO Reproductive Health Library (RHL).9
A multifaceted intervention addressing potential barriers to evidence-based practice was conducted over a period of six months following baseline data collection on clinical practices. Three interactive workshops focusing on principles of evidence-based medicine, the RHL and how to implement change formed the core intervention. The use of magnesium sulfate and other effective practices were not specifically addressed during the workshops.
The data on the occurrences of pre-eclampsia and eclampsia and the use of anticonvulsants were collected as part of measuring the rate of evidence-based practices in the main trial. The data were collected at baseline (September 2000) and 10 to 12 months after implementation of the intervention (September 2002). We collected data from 1000 women or for six months, whichever was reached first in each unit. Field workers not involved in the implementation of the trial collected the data. The data collection forms were completed in the postnatal wards mostly from hospital records. The mothers were consulted if information was missing from the records.
We report crude prevalence rates of pre-eclampsia and eclampsia. The rates of magnesium sulfate use and their 95% confidence intervals were considered at cluster (hospital) level.
The study was approved by the Scientific and Ethical Review Group of the UNDP/UNFPA/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP) and the ethics review committees of the participating institutions.
Results
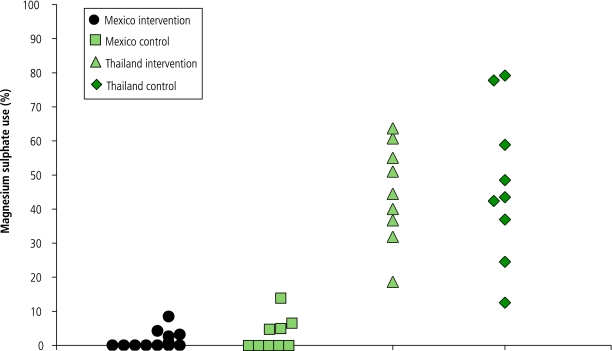
The overall prevalence of pre-eclampsia in Mexico and Thailand was 5.5% (2320/41 828) and 1.9% (699/35 923), respectively. There was no statistically and clinically significant difference between the rate of magnesium sulfate use for women with pre-eclampsia (and eclampsia) at baseline and at the end of the study, in both intervention and control hospitals. We therefore combined the data collected during these two periods for each hospital. Only eight out of 22 hospitals in Mexico used magnesium sulfate for pre-eclampsia, and for those using magnesium sulfate the rate of use ranged from 0.8% (95% CI: 0–4.5) to 8.5% (95% CI: 4.8–13.6) among women with pre-eclampsia (Fig. 1). In Thailand, all 18 hospitals used magnesium sulfate for pre-eclampsia; the rates of use ranged from 18.6% (95% CI: 8.4–33.9) to 63.6% (95% CI: 50.9–75.1) in the intervention group and 12.5% (95% CI: 1.6–38.3) to 79.2% (95% CI: 65.0–89.5) in the control group (Fig. 1). In Mexico, phenytoin was more commonly used than magnesium sulfate but it was not used at all in Thailand. Diazepam was not used in either country for women with pre-eclampsia.
Fig. 1.
The rate of magnesium sulfate use for women with pre-eclampsia in Mexico and Thailand (some hospitals did not have any cases)
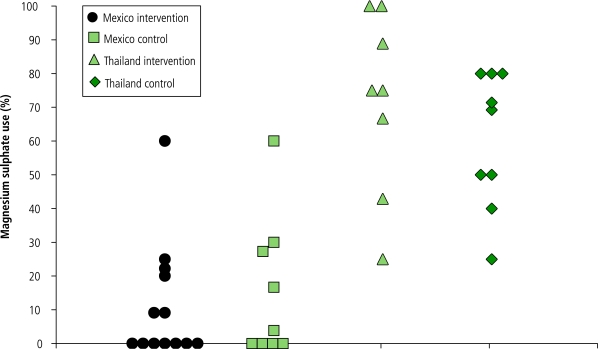
The overall prevalence of eclampsia was 0.6% (232/41 828) and 0.3% (122/35 923) in Mexico and Thailand, respectively. Only 11 out of 22 hospitals in Mexico used magnesium sulfate for eclampsia; for those using it the rates of use ranged from 9.1% (95% CI: 0.2–41.3) to 60.0% (95% CI: 14.7–94.7) in the intervention group and 3.8% (95% CI: 0.5–13.2) to 60.0% (95% CI: 14.7–94.7) in the control group (Fig. 2). In Thailand, there was one hospital that did not have patients with eclampsia at both baseline and at the end of the study; it was excluded from the analysis. The remaining 17 hospitals used magnesium sulfate for eclampsia. The rates of use ranged from 25.0% (95% CI: 0.6–80.6) to 100% (95% CI: 29.2–100) in the intervention group, and 25.0% (95% CI: 0.6–80.6) to 80.0% (95% CI: 44.4–97.5) in the control group (Fig. 2). Phenytoin was more commonly used than magnesium sulfate in Mexico but was not used at all in Thailand for eclampsia. Diazepam was rarely used in both countries.
Fig. 2.
The rate of magnesium sulfate use for women with eclampsia in Mexico and Thailand (some hospitals did not have any cases)
Discussion
The prevalence of pre-eclampsia and eclampsia in Mexico was 5.5% and 0.6% respectively, which is quite similar to the overall global picture.1 However, the corresponding rates in Thailand were 1.8% and 0.3%, which are lower. The uses of magnesium sulfate for pre-eclampsia and eclampsia were surprisingly low in Mexico. In Thailand, magnesium sulfate was used more frequently for both pre-eclampsia and eclampsia.
A report on the management of eclampsia from Sweden shows the remarkably increased use of magnesium sulfate: from 8% during 1980–1989 to 83% during 1990–1999.10 A questionnaire survey of obstetricians in the United Kingdom and Ireland in 1996 indicated that 40% and 60% of respondents would use magnesium sulfate for pre-eclampsia and eclampsia, respectively.11
The very low rate of magnesium use particularly in Mexico is alarming. Magnesium sulfate is reasonably cheap and its effectiveness when used in pre-eclampsia and eclampsia has been clearly shown by evidence from randomized controlled trials and systematic reviews.2,12,13 Although magnesium sulfate use for pre-eclampsia and eclampsia in Thailand is much higher than in Mexico, there is still room for improvement. Magnesium sulfate has been in the National Essential Drug List of Thailand since 1999. As of 2002, there were only 45 countries that had magnesium sulfate in their essential drug list (WHO unpublished data). As of 16 October 2006, the Mexican National Essential Drug List did not include magnesium sulfate (Edición 2005 del Cuadro Básico y Catálogo de Medicamentos, available at: http://www.salud.gob.mx). Responsible persons and organizations in these two countries should take immediate actions to ensure wider use of this effective and inexpensive drug for these conditions. Researchers and responsible persons in other low- to middle-income countries should also evaluate the situation regarding this issue and take appropriate actions.
Why has magnesium sulfate not become the treatment of choice particularly for eclampsia throughout the world? There are two possible hypotheses. First, magnesium sulfate is too cheap to motivate mass manufacturing, licensing, production and distribution. Second, health-care providers and administrators may be reluctant to adopt a practice that requires intensive monitoring for a condition (eclampsia) that is relatively infrequent.14 Not having experience with magnesium sulfate administration has been proposed as a reason for not using it in the United Kingdom.15 International organizations have advocated the use of magnesium sulfate in the treatment and prevention of eclampsia.14 There are often systematic gaps between evidence of effectiveness and what is actually practiced. Failure in the registration, procurement and distribution mechanisms for magnesium sulfate contribute to its poor availability in Mozambique and Zimbabwe.16 A survey of WHO drug information officers, regulatory officials and obstetricians in 12 countries was undertaken to identify barriers and facilitators to knowledge translation on the use of magnesium sulfate to treat pre-eclampsia. The perceived barriers include drug licensing and availability, inadequate and poorly implemented clinical guidelines, and the lack of political support for policy change.17 There were significant regional and national differences in the importance of specific barriers.17
Our report is unique in that we measured actual practices of using magnesium sulfate in pre-eclampsia and eclampsia by extracting data from medical records of a large number of women from 22 hospitals in Mexico and 18 hospitals in Thailand. Based on anecdotal evidence before data collection, we had assumed that magnesium sulfate would be routinely used in both Mexico and Thailand. For pre-eclampsia we anticipated some variation because the evidence was not strong at the time. The Magpie trial was published in June 2002.18 However, the use of phenytoin for pre-eclampsia and eclampsia in Mexico was surprising. These data highlight the importance of collecting actual practice data rather than reported behaviour, which can often overestimate the quality of care.
Our data has the limitation of being retrospective. The quality of data might be somewhat limited to the standards of patient records in the two countries. However, both pre-eclampsia and eclampsia are serious conditions where women are hospitalized, and it is unlikely that magnesium sulfate would have been used but not recorded.
We conclude that magnesium sulfate is not as widely used for preventing and treating eclampsia as it should be, in spite of its inexpensiveness and the very clear evidence about its effectiveness. Immediate actions are necessary to promote its use in all countries around the world, including insertion in National Essential Drug Lists. Organizations, such as the International Federation of Gynecology and Obstetrics (FIGO) and the International Confederation of Midwives (ICM), their national counterparts and other professional organizations should advocate for the availability and use of magnesium sulfate, assist in the development of local treatment protocols to follow and training of health-care workers in the use of magnesium sulfate. Given the paucity of evidence to select appropriate strategies for implementation, research projects to evaluate innovative approaches to implement magnesium sulfate treatment are of high priority in low- and middle-income countries. ■
Acknowledgements
We thank Evelyn Jiguet for her assistance with the data preparation. Jeremy Grimshaw holds a Canada Research Chair in Health Knowledge Transfer and Uptake. We thank Paul FA Van Look for his valuable comments on the manuscript.
Footnotes
Funding: The study was funded by the UNDP/UNFPA/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction, Geneva, Switzerland.
Competing interests: None declared.
References
- 1.Villar J, Say L, Shennan A, Lindheimer M, Duley L, Conde-Agudelo A, et al. Methodological and technical issues related to the diagnosis, screening, prevention, and treatment of pre-eclampsia and eclampsia. Int J Gynaecol Obstet. 2004;85:S28–41. doi: 10.1016/j.ijgo.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 2.Duley L, Gulmezoglu AM, Henderson-Smart DJ. Magnesium sulfate and other anticonvulsants for women with pre-eclampsia. Cochrane Database Syst Rev. 2003:CD000025. doi: 10.1002/14651858.CD000025. [DOI] [PubMed] [Google Scholar]
- 3.Duley L. Pre-eclampsia and the hypertensive disorders of pregnancy. Br Med Bull. 2003;67:161–76. doi: 10.1093/bmb/ldg005. [DOI] [PubMed] [Google Scholar]
- 4.Duley L, Henderson-Smart D. Magnesium sulfate versus phenytoin for eclampsia. Cochrane Database Syst Rev. 2003:CD000128. doi: 10.1002/14651858.CD000128. [DOI] [PubMed] [Google Scholar]
- 5.Duley L, Henderson-Smart D. Magnesium sulfate versus diazepam for eclampsia. Cochrane Database Syst Rev. 2003:CD000127. doi: 10.1002/14651858.CD000127. [DOI] [PubMed] [Google Scholar]
- 6.Sheth SS, Chalmers I. Magnesium for preventing and treating eclampsia: time for international action. Lancet. 2002;359:1872–3. doi: 10.1016/S0140-6736(02)08783-4. [DOI] [PubMed] [Google Scholar]
- 7.Gülmezoglu AM, Villar J, Grimshaw J, Piaggio G, Lumbiganon P, Langer A. Cluster randomized trial of an active, multifaceted information dissemination intervention based on the WHO Reproductive Health Library to change obstetric practices: methods and design issues. BMC Med Res Methodol. 2004;4:2. doi: 10.1186/1471-2288-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gülmezoglu A, Langer A, Piaggio G, Lumbiganon P, Villar J, Grimshaw J. Cluster randomised trial of an active, multifaceted educational intervention based on the WHO Reproductive Health Library to improve obstetric practices. BJOG 2006; article published online 27-Sep-2006. [DOI] [PubMed]
- 9.The WHO Reproductive Health Library. Geneva: WHO. http://www.rhlibrary.com
- 10.Rugarn O, Carling Moen S, Berg G. Eclampsia at a tertiary hospital 1973-99. Acta Obstet Gynecol Scand. 2004;83:240–5. doi: 10.1111/j.0001-6349.2004.0173.x. [DOI] [PubMed] [Google Scholar]
- 11.Gülmezoglu AM, Duley L. Use of anticonvulsants in eclampsia and pre-eclampsia: survey of obstetricians in the United Kingdom and Republic of Ireland. BMJ. 1998;316:975–6. doi: 10.1136/bmj.316.7136.975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duley L. Magnesium sulfate in eclampsia. Eclampsia Trial Collaborative Group. Lancet. 1998;352:67–8. doi: 10.1016/S0140-6736(05)79550-7. [DOI] [PubMed] [Google Scholar]
- 13.Eclampsia Trial Collaborative Group Which anticonvulsant for women with eclampsia? Evidence from the Collaborative Eclampsia Trial. Lancet. 1995;345:1455–63. [PubMed] [Google Scholar]
- 14.Roberts JM, Villar J, Arulkumaran S. Preventing and treating eclamptic seizures. Magnesium sulfate is effective and recommended for use. BMJ. 2002;325:609–10. doi: 10.1136/bmj.325.7365.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fox R, Draycott T. Prefer diazepam for initial control of pre-eclamptic fit. BMJ. 1995;311:1433. doi: 10.1136/bmj.311.7017.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sevene E, Lewin S, Mariano A, Woelk G, Oxman A, Matinhure S, et al. System and market failures: the unavailability of magnesium sulphate for the treatment of eclampsia and pre-eclampsia in Mozambique and Zimbabwe. BMJ. 2005;331:765–9. doi: 10.1136/bmj.331.7519.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aaserud M, Lewin S, Innvaer S, Paulsen E, Dahlgren AT, Trommald M, et al. Translating research into policy and practice in developing countries: a case study of magnesium sulphate for pre-eclampsia. BMC Health Serv Res. 2005;5:68. doi: 10.1186/1472-6963-5-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duley L and the Magpie Trial Collaborative Group Do women with pre- eclampsia, and their babies, benefit from magnesium sulfate? The Magpie Trial: a randomized placebo-controlled trial. Lancet. 2002;359:1877–90. doi: 10.1016/S0140-6736(02)08778-0. [DOI] [PubMed] [Google Scholar]