Abstract
Objective. We sought to determine whether lack of state Medicaid coverage for infant male circumcision correlates with lower circumcision rates.
Methods. We used data from the Nationwide Inpatient Sample on 417 282 male newborns to calculate hospital-level circumcision rates. We used weighted multiple regression to correlate hospital circumcision rates with hospital-level predictors and state Medicaid coverage of circumcision.
Results. The mean neonatal male circumcision rate was 55.9%. When we controlled for other factors, hospitals in states in which Medicaid covers routine male circumcision had circumcision rates that were 24 percentage points higher than did hospitals in states without such coverage (P < .001). Hospitals serving greater proportions of Hispanic patients had lower circumcision rates; this was not true of hospitals serving more African Americans. Medicaid coverage had a smaller effect on circumcision rates when a hospital had a greater percentage of Hispanic births.
Conclusions. Lack of Medicaid coverage for neonatal male circumcision correlated with lower rates of circumcision. Because uncircumcised males face greater risk of HIV and other sexually transmitted infections, lack of Medicaid coverage for circumcision may translate into future health disparities for children born to poor families covered by Medicaid.
Three recent randomized clinical trials in South Africa, Kenya, and Uganda found that male circumcision reduces a man's risk of becoming infected with HIV through contact with a female partner by 55% to 76%.1–3 These results are consistent with meta-analyses based on observational studies in Africa4,5 and the United States.6,7
The recent randomized clinical trial findings prompted the American Academy of Pediatrics (AAP) to form a committee in June 2007 to review its position on male circumcision.8 In 1999 the AAP had adopted a neutral stance, stating that the medical benefits were not compelling enough to recommend routine neonatal circumcision. In the wake of the AAP statement, several states withdrew Medicaid coverage for routine, nontherapeutic circumcision. Currently, 16 state Medicaid plans do not cover the procedure. In 2006, legislators in Hawaii and Vermont introduced resolutions challenging the need for state funding of routine male circumcision.9
In view of the striking results from the African clinical trials, it is timely to examine the impact of US hospital- and state-level policies on domestic rates of male circumcision. In particular, we hypothesized that male circumcision rates would be higher in states in which the Medicaid program pays for routine circumcision.
METHODS
Sample and Measures
Data for this study came from the 2004 Nationwide Inpatient Sample (NIS), from the Healthcare Cost and Utilization Project of the Agency for Health Care Research and Quality. The NIS is the largest all-payer inpatient-care database in the United States and consists of a random sample of hospitals in 37 states. It contains information included in a typical discharge abstract: hospital characteristics and patient demographics, expected payment source, diagnoses, procedures, length of stay, and discharge status. The 2004 NIS contains data from more than 8 million discharges from 1004 hospitals,10 reflecting roughly 20% of inpatient visits to US community hospitals. We used data from NIS records on newborn males who had a routine discharge from the hospital. Because many facilities reported no births, our analysis incorporated data from 683 hospitals, which reported 417 282 routine discharges of newborn males.
The outcome of interest was circumcision status, measured by the presence of an International Classification of Diseases, Ninth Revision (ICD-9),11 procedure code indicating circumcision among any of up to 15 procedures performed during the hospital stay. The unit of analysis was the hospital, so rates of circumcision for each hospital were calculated by dividing the number of circumcised newborn male infants by the total number of newborn boys in the hospital.
The main explanatory measure was a state policy variable reflecting whether Medicaid covered routine circumcisions for newborn males in the hospital's state in 2004.12 Other explanatory variables were those that had been found in previous analyses to predict male circumcision and that were also available in the NIS.13 Individual-level variables were aggregated to a hospital-level summary. Table 1 presents definitions and mean circumcision rates by each of the variables.
TABLE 1.
Circumcision Rates as a Function of Hospital and State Predictors (Hospitals Weighted by Number of Male Births): Nationwide Inpatient Sample, 2004
| Mean Circumcision Rate (SD) | ANOVA F | ANOVA P | |
| All hospitals (N = 683) | 55.9 (29.9) | ||
| State Medicaid program coverage of routine male circumcision | 412.5 | <.001 | |
| Not covered | 31.2 (29.6) | ||
| Covered | 69.6 (20.8) | ||
| Hospital sizea | 1.5 | .216 | |
| Small | 61.0 (21.9) | ||
| Medium | 55.8 (29.5) | ||
| Large | 54.9 (34.1) | ||
| Hospital location | 5.3 | .021 | |
| Rural | 63.7 (14.9) | ||
| Urban | 55.1 (36.3) | ||
| Hospital teaching status | 12.0 | <.001 | |
| Nonteaching | 52.3 (26.6) | ||
| Teaching | 60.2 (39.1) | ||
| Region | 132.4 | <.001 | |
| Northeast | 68.7 (15.7) | ||
| Midwest | 77.2 (16.7) | ||
| South | 59.7 (28.2) | ||
| West | 27.1 (29.0) | ||
| Proportion of male births with LOS of ≤ 1 dayb | 65.9 | <.001 | |
| Low | 64.8 (26.4) | ||
| Medium | 61.4 (28.5) | ||
| High | 36.0 (27.4) | ||
| Proportion of male births with LOS of 2 to 5 daysb | 77.6 | <.001 | |
| Low | 37.5 (29.3) | ||
| Medium | 61.2 (30.4) | ||
| High | 68.4 (20.2) | ||
| Proportion of male births with LOS of ≥ 6 daysb | 1.1 | .345 | |
| Low | 55.1 (18.2) | ||
| Medium | 58.9 (27.0) | ||
| High | 55.0 (40.4) | ||
| Proportion of male births with Medicaid as primary payerb | 63.4 | <.001 | |
| Low | 65.1 (27.0) | ||
| Medium | 59.9 (25.9) | ||
| High | 36.8 (29.6) | ||
| Proportion of male births with no insuranceb | 11.9 | <.001 | |
| Low | 57.1 (28.2) | ||
| Medium | 60.8 (31.8) | ||
| High | 47.3 (28.2) | ||
| Proportion of male births with private insuranceb | 61.4 | <.001 | |
| Low | 36.3 (28.8) | ||
| Medium | 59.9 (25.7) | ||
| High | 64.5 (28.2) | ||
| Proportion of male births living in a lower income area (lowest quartile)bc | 17.5 | <.001 | |
| Low | 62.5 (24.2) | ||
| Medium | 56.7 (34.6) | ||
| High | 44.4 (27.9) | ||
| Proportion of male births living in a medium-low income area (second quartile)bc | 1.0 | .380 | |
| Low | 57.6 (29.0) | ||
| Medium | 56.0 (34.4) | ||
| High | 53.1 (25.8) | ||
| Proportion of male births living in a medium-high income area (third quartile)bc | 8.2 | <.001 | |
| Low | 44.6 (22.0) | ||
| Medium | 56.7 (32.4) | ||
| High | 58.7 (33.2) | ||
| Proportion of male births living in a higher income area (highest quartile)bc | 11.3 | <.001 | |
| Low | 55.4 (18.3) | ||
| Medium | 48.1 (36.2) | ||
| High | 60.1 (33.2) | ||
| Proportion of male births who are Whiteb | 67.5 | <.001 | |
| Low | 43.8 (37.0) | ||
| Medium | 65.0 (23.4) | ||
| High | 72.3 (18.1) | ||
| Proportion of male births who are African Americanb | 18.4 | <.001 | |
| Low | 45.6 (30.3) | ||
| Medium | 55.2 (29.1) | ||
| High | 62.7 (28.1) | ||
| Proportion of male births who are Hispanicb | 142.5 | <.001 | |
| Low | 75.5 (16.9) | ||
| Medium | 66.6 (22.6) | ||
| High | 39.0 (33.2) | ||
| Proportion of male births who are another race/ethnicitybd | 8.3 | <.001 | |
| Low | 47.9 (30.4) | ||
| Medium | 58.8 (30.0) | ||
| High | 58.4 (28.4) |
Note. ANOVA = analysis of variance; LOS = length of hospital stay.
Determined based on the number of beds. Classifications were relative to a hospital's region, urban or rural location, and teaching status.
For characteristics measured on a continuous scale, neonatal male circumcision rates were calculated for hospitals that fell into the lowest third of the distribution of the characteristic across hospitals (low), the middle third (medium), and the highest third (high).
Proportion of newborns in each hospital who resided in zip codes with median income of $1 to $35 999 (lowest quartile), $36 000 to $44 999 (second quartile), $45 000 to $58 999 (third quartile), and $59 000 or higher (highest quartile). This was calculated from Nationwide Inpatient Sample data on median household income quartile for each patient's zip code.10
Other ethnicity includes non-White, non–African American, non-Hispanic (e.g., Asian/Pacific Islander, American Indian).
Missing Data
Complete data were available for all hospital and policy variables. However, there were missing data for some patient characteristics. All hospitals reported primary payer data for at least 75% of admissions, and all but 8 hospitals had income data for at least 80% of patients. We based the hospital-level insurance and income variables on those cases with complete data.
Race/ethnicity information was missing at higher rates. Patients' racial/ethnic group was not provided at all in hospital records from 10 states, accounting for 178 of the 683 hospitals analyzed. An additional 36 hospitals in other states provided race/ethnicity data for fewer than half of their patients.
Appending county-level and state-level population data on the proportions of infant males falling into each category,14,15 we performed a 2-step multiple imputation procedure for the proportion of newborn boys in the hospital who were White, African American, Hispanic, or other race/ethnicity.16,17 State-level data were appended for hospitals in all states; county-level data was appended only for hospitals in states in which county code was provided in the NIS. In the first step of the procedure, we imputed racial/ethnic proportions for 140 hospitals that had available county-level racial/ethnic data as well as the measures presented in Table 1. For the second imputation step we used state-level, rather than county-level, racial/ethnic percentages, and imputed values for 74 hospitals for which we did not have county-level data. We performed multiple imputation procedures with the SAS version 9.1 PROC MI (SAS Institute Inc, Cary, NC), by using the Markov Chain Monte Carlo method. Time-series plots for the worst linear function remained stable across iterations. Five imputed data sets were produced.
Results from sensitivity analyses that tested the inclusion of hospitals from the 3 states (Georgia, Nebraska, and Ohio) that accounted for 73 of the 74 hospitals that did not report race or county data did not differ meaningfully. Therefore, we present estimates based on all 37 available states.
Statistical Analysis
We used simple analysis of variance to compare average hospital circumcision rates by state and hospital characteristics. For characteristics measured on a continuous scale (such as proportion of patients with a hospital length of stay of 1 day), neonatal male circumcision rates were calculated for hospitals that fell into the lowest third of the distribution of the characteristic across hospitals (low), the middle third (medium), and the highest third (high).
Many of the factors that correlated with hospital male circumcision rates were correlated with each other (e.g., region and percentage Hispanic). To isolate the effect of each variable, we performed ordinary least squares regression with circumcision rate as our dependent variable and with state policy and hospital characteristics as predictors. Regressions were weighted by the normalized number of male births reported in each hospital. We included all stratification variables used to develop the sample as regressors. Because the circumcision rate variable was bounded below by 0 and above by 1, we used a logistic (logit) transformation of the measure as follows to conform with regression model assumptions:
 |
where pi is the circumcision rate for hospital (i).
To avoid extreme values of yi, values of pi that were less than 0.01 were recoded to 0.01, and values of pi that were greater than 0.99 were recoded to 0.99. To assess the sensitivity of findings to this transformation, we also tested an arcsine transformation, which allows values of 0 or 1 for pi:
 |
Results from analyses with the arcsine transformation did not differ meaningfully from analyses with the logit transformation; we present only the logit-transformation results.
In fitting the regression model, we examined quadratic and interaction terms. Only significant terms were retained in the final model. We performed model fitting on 1 of the 5 imputed data sets produced by SAS PROC MI in an initial run. We then reran the imputation with a new random seed, and we performed final analyses on all 5 imputation data sets; we combined results by using SAS PROC MIANALYZE.
We used the regression results to predict circumcision rates as a function of state Medicaid policy, proportion of patient stays covered by Medicaid, and proportion of Hispanic newborns, in each case maintaining all other predictors at their observed values. In the “Discussion” section, we present predicted values of male circumcision rates under different Medicaid policy scenarios.
RESULTS
Across the 683 hospitals in the sample, the average weighted circumcision rate was 55.9%. Table 1 summarizes observed male circumcision rates. When we did not control for correlated factors, routine circumcision was less common in hospitals with higher proportions of births paid for by Medicaid (36.8%), in hospitals with greater proportions of uninsured deliveries (47.3%), and in hospitals that serve a greater share of patients in the lowest quartile of the income distribution (44.4%; P < .001). Male circumcision rates were higher (72.3%) in the one third of the hospitals with the largest proportion of infants who are White (P < .001) and lower (39.0%) in the one third of the hospitals with the largest proportions of infants who are Hispanic (P < .001). Male circumcision rates were lower (36.0%) in hospitals with the largest proportions of newborns with 1-day stays (P < .001).
Neonatal male circumcision rates differed significantly across regions of the country (P < .001). Male circumcision rates averaged 77.2% in the Midwest, 68.7% in the Northeast, 59.7% in the South, and just 27.1% in the West. Bivariate analyses showed that neonatal male circumcision rates were higher in teaching hospitals (P < .001) and in hospitals located in rural areas (P = .021). However, a hospital's circumcision rate was not significantly related to the number of beds (P = .216).
Our public policy measure also showed a significant relationship with neonatal male circumcision rates. In states whose Medicaid program covers neonatal male circumcision, rates were more than twice as high (69.6%) as in states whose Medicaid program does not pay for male circumcision (31.2%).
Regression results, presented in Table 2, show effects of each factor with control for all other predictors. The set of primary payer variables significantly predicted neonatal male circumcision rates (F = 22.96; P < .001). Hospitals with higher proportions of Medicaid-covered births (P < .001) and uninsured births (P < .004) had lower circumcision rates than did hospitals with more patients covered by private insurance. However, in states in which Medicaid paid for routine neonatal circumcision, rates were significantly higher than in states in which this was not the case (P < .001). As expected, the greater the share of Medicaid-covered births in the hospital, the greater the effect of state coverage for neonatal male circumcision on the hospital's circumcision rate.
TABLE 2.
Multiple Regression Results With Multiply Imputed Data Sets For Predictors of Male Infant Circumcision: Nationwide Inpatient Sample, 2004
| ba (95% CI) | P | |
| Intercept | 1.276 (0.629, 1.923) | <.001 |
| State Medicaid program covers routine male circumcision | 0.866 (0.375, 1.357) | <.001 |
| Hospital sizeb (Ref = large) | .866 | |
| Small | 0.068 (–0.186, 0.323) | .599 |
| Medium | 0.021 (–0.168, 0.210) | .827 |
| Rural hospital location | 0.213 (–0.182, 0.607) | .290 |
| Teaching hospital | −0.162 (–0.447, 0.124) | .267 |
| Region (Ref = South) | <.001 | |
| Northeast | −0.549 (−0.859, −0.239) | <.001 |
| Midwest | 0.210 (–0.085, 0.504) | .164 |
| West | −0.813 (−1.189, −0.436) | <.001 |
| Hospital ownershipc | .122 | |
| Income quartile of patient's zip coded (Ref = lowest) | .373 | |
| Proportion in second quartile | 0.341 (–0.176, 0.857) | .196 |
| Proportion in third quartile | 0.038 (–0.560, 0.637) | .900 |
| Proportion in highest quartile | −0.107 (–0.634, 0.421) | .692 |
| Length of stay (LOS; Ref = 2 to 5 d) | <.001 | |
| Proportion with LOS = 1 d, centered | −1.487 (−2.343, −0.632) | <.001 |
| Proportion with LOS = 1 d, squared | −4.601 (−8.497, −0.706) | .021 |
| Proportion with LOS ≥ 6 d, centered | −5.267 (−8.009, −2.525) | <.001 |
| Proportion with LOS ≥ 6 d, squared | 4.303 (–0.824, 9.431) | .1 |
| Primary payer (Ref = private insurance) | <.001 | |
| Proportion with Medicaid as primary payer | −2.986 (−3.758, −2.215) | <.001 |
| Medicaid coverage × Medicaid proportion | 2.080 (1.165, 2.996) | <.001 |
| Proportion with no insurance | −1.561 (−2.625, −0.496) | .004 |
| Race/ethnicity (Ref = non-Hispanic White) | <.001 | |
| Proportion African American | 1.324 (–0.258, 2.905) | .099 |
| Medicaid coverage × African American proportion | −1.029 (–2.814, 0.756) | .251 |
| Proportion Hispanic | −2.095 (−2.846, −1.344) | <.001 |
| Medicaid coverage × Hispanic proportion | −0.961 (−1.834, −0.087) | .031 |
| Proportion other race/ethnicity | 0.550 (–0.994, 2.095) | .445 |
| Medicaid coverage × other race proportion | −0.428 (–2.111, 1.255) | .615 |
Note. CI = confidence interval.
Logit-transformed scale.
Determined based on the number of beds. Classifications were relative to a hospital's region, urban or rural location, and teaching status.10
In sampling, hospitals were first assigned to strata on the basis of their region, location, and teaching status and then broken down further by hospital ownership. Number of categories used to define ownership depended on the size of these initial strata. Because of these context-specific aggregation levels, this variable is difficult to interpret, but was included in the multivariate analyses as a means of control for stratification. Hospital size was also used in stratification.
This was based on zip codes with median income of $1 to $35 999 (lowest quartile), $36 000 to $44 999 (second quartile), $45 000 to $58 999 (third quartile), and $59 000 or higher (highest quartile). This was calculated from Nationwide Inpatient Sample data on median household income quartile for each patient's zip code.10
Circumcision rates varied significantly by region in the regression analysis (F = 16.13; P < .001). Relative to hospitals in the South, and with control for other factors, neonatal male circumcision rates were significantly lower in the West (P < .001) and the Northeast (P < .001), but not significantly different in the Midwest (P = .164). Even net of region effects, the race/ethnicity variables remained highly significant predictors of male circumcision (F = 29.35; P < .001). Hospitals that had a greater proportion of Hispanic newborns relative to Whites showed significantly lower circumcision rates (P < .001), although hospitals in which African Americans accounted for a larger share of the births relative to Whites did not differ significantly.
The length-of-stay variables were also significantly related to male circumcision rates in the regression analysis (F = 12.20; P < .001). Hospitals with greater proportions of very short maternity stays (P < .001) had lower circumcision rates. Hospitals with larger shares of very long stays also had lower circumcision rates (P < .001) compared with hospitals in which a greater share of the maternity stays were between 2 and 5 days.
Although they had significant bivariate relationships with neonatal male circumcision rates, rural status, hospital teaching status, and median income in the zip code of the child's residence were not significantly associated with circumcision rates once we controlled for region and other patient characteristics. Neither hospital size (F = 0.14; P = .866) nor hospital ownership (F = 1.82; P = .122) was significantly associated with male circumcision rates.
Retransforming the parameter estimates in Table 2 to the original scale, we can predict differences in hospital circumcision rates when varying a single factor. For example, other factors being equal, we estimated that a hospital in the Northeast would have a circumcision rate 10 percentage points lower than would a comparable hospital in the South; a comparable hospital in the West would have a male circumcision rate 15 percentage points lower than would a hospital in the South.
A hospital with 35% of newborn males having only a 1-day length of stay (which is 1 SD above the mean of 19%) would be expected to have a circumcision rate that is 6 percentage points lower than would a comparable hospital with the percentage of newborns having a 1-day length of stay at the mean. Other factors being equal, a hospital whose percentage of newborn males staying 6 days or more is 12% (mean + 1 SD), is predicted to have a circumcision rate 7 percentage points lower than is a hospital with the average proportion of length of stay of 6 days or more (4%).
The estimated impact of Medicaid coverage for routine circumcisions is substantial: given the proportions of patients with Medicaid as primary payer across observed hospitals, the model predicted that hospitals in states that cover routine circumcisions have circumcision rates averaging 24 percentage points higher than comparable hospitals in states in which Medicaid does not cover neonatal male circumcision. This overall effect is complicated by the significant interaction effects of state Medicaid coverage with the percentage of births that are Hispanic.
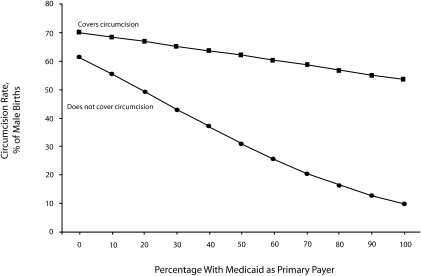
Figure 1 shows that even in states in which Medicaid pays for neonatal male circumcision, the rates of circumcision fall with increasing shares of births that are paid for by Medicaid. However, the decline in circumcision associated with a higher proportion of patients with Medicaid insurance is much steeper when Medicaid does not cover the procedure.
FIGURE 1.
Predicted neonatal male circumcision rates as a function of Medicaid coverage of circumcision and the percentage of male newborns in hospital for whom Medicaid is their primary payer: Nationwide Inpatient Sample, 2004.
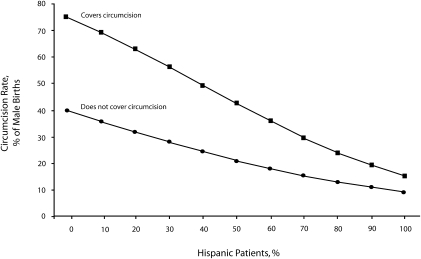
Further, the greater the share of Hispanic births at a hospital, the smaller the difference in male circumcision rates between states with and without Medicaid coverage of routine circumcision (P = .031), as illustrated in Figure 2. These predictions, based on the regression, show that although when the proportion of Hispanic births is low there is a large differential between male circumcision rates in states with and without Medicaid coverage of neonatal male circumcision, this differential narrows when the proportion of Hispanic births is very high.
FIGURE 2.
Predicted neonatal male circumcision rates as a function of Medicaid coverage of circumcision and percentage of births that are Hispanic: Nationwide Inpatient Sample, 2004.
DISCUSSION
How relevant to the United States are recent findings from randomized clinical trials in Africa that strongly support the positive effects of male circumcision in reducing female-to-male HIV transmission? Major differences in the HIV epidemic in Africa and the United States signal a need to be cautious about applying the clinical trial results in the US context. The African results relate to transmission from female sexual partners to uninfected men. However, in the United States, only 16% of all AIDS cases among men are linked to heterosexual transmission, whereas 18% are linked exclusively to injection drug use and 65% are linked to male-to-male sexual contact.18 Male circumcision may have only a limited role in protecting men who have sex with men (MSM) from HIV infection because the receptive partner in anal intercourse is at the greater risk of becoming infected, yet the African clinical trials relate to transmission to the male insertive partner of an HIV-infected woman.19–21
Nonetheless, observational data support a protective effect for male circumcision among both MSM and heterosexual men. Kreiss and Hopkins6 found that HIV was twice as prevalent among uncircumcised MSM as among those who were circumcised, but Millett et al.22 found no such effect. In a prospective study of MSM, Buchbinder et al.7 found that HIV seroconversion was twice as likely among uncircumcised men as among those who were circumcised.7 Among heterosexual men with a known HIV-positive female sexual partner, those who were circumcised had a significantly lower rate of HIV infection.23
Meta-analyses document other health benefits for circumcised men, including lower rates of urinary tract infections,24 lower rates of penile human papillomavirus,25 lower rates of penile cancer,26,27 and lower risk of chancroid and syphilis.4 Moses et al. reported that medical complications from the circumcision procedure occur at the rate of 0.2% to 0.6%, and that most are minor. They did not find evidence for long-term adverse psychological or physical effects.26
Observational data suggest health benefits, as well, for women partners of circumcised men in terms of a reduced risk of cervical cancer.25,26 However, a randomized clinical trial in Rakai, Uganda, in which the effect of male circumcision on transmission by HIV-positive men to their female partners was examined found no protective effect for women within the first 6 months after the surgery and was terminated early.28 A statistically insignificant trend toward increased HIV transmission by newly circumcised HIV-positive men relative to uncircumcised men was attributed to resumption of sexual activity before complete wound healing. However, this adverse consequence of circumcising adult men would not be a relevant issue for infant circumcision. Indeed, observational data from Rakai documented lower HIV transmission rates by HIV-positive men circumcised at a prior date. Reductions in female-to-male transmission that lower the population prevalence rates of HIV will also result in fewer male-to-female transmissions.29
Despite likely positive effects of circumcision on health, male circumcision rates in the United States have been falling since the 1980s.30 If trends continue toward having shorter hospital stays, fewer states offering Medicaid coverage for neonatal male circumcision, and a larger share of the US population being of Hispanic origin, it is reasonable to expect male circumcision rates to continue to fall.
Early hospital discharge (within 24 hours), which our analyses showed correlates with lower neonatal male circumcision rates, is becoming more common.31 Ongoing emphasis on reducing inpatient costs will continue to accelerate hospital discharge following delivery, thereby making it difficult to schedule a circumcision.
Demographic changes may also put downward pressure on neonatal male circumcision rates because Hispanics, whom we found to have low circumcision rates, account for an increasing share of all US births. In 2004, 23% of all US births were to Hispanic or Latino mothers, up from 17.4% in 1995.32 Low male circumcision rates among Hispanics appear to depend more on personal preferences and cultural factors than on the cost of the procedure; we found that, in hospitals with large proportions of Hispanic births, male circumcision rates seemed less responsive to Medicaid coverage for circumcision (i.e., male circumcision rates were low among Hispanics regardless of whether the state Medicaid program pays for circumcision).
Further, Medicaid pays for a large and increasing share (now more than 41%) of all births in the United States,33 and male children whose delivery is paid for by Medicaid are less likely to receive circumcision. This finding appears to reflect the preferences of Medicaid clients and not solely their low income, because the negative relationship between Medicaid and male circumcision persists even when the state Medicaid plan pays for the procedure and ability to pay should not be an issue. Nevertheless, the choices of Medicaid clients can be somewhat affected by the context. As shown in Figure 1, neonatal male circumcision rates were higher in states that cover the cost of the procedure. We conclude that the lack of reimbursement for neonatal male circumcision may act as an additional deterrent to circumcision among low-income non-Hispanic families. This finding is consistent with the evidence from Great Britain, whose declining rates of male circumcision have been attributed to a lack of coverage by the British National Health Service.34
We found pronounced differences in neonatal male circumcision rates across regions of the United States. High variability in the rates of elective surgery has been documented for other discretionary procedures, especially in cases in which the scientific evidence of benefits is still being debated.35 In these instances, physician attitudes or patient preferences may lead to persistent differences across regions, which have been termed “surgical signatures.”36 The AAP's neutral stance on neonatal male circumcision may, therefore, contribute to variation in circumcision rates across regions by allowing a greater role for the exercise of patient and physician preferences.
Male circumcision is likely to have its greatest effects among poor and minority populations, among whom the prevalence of HIV and other sexually transmitted infections is highest.18,37 Medicaid coverage of childbirth may be a more accurate indicator of poverty status than a zip code income average, a measure that did not significantly predict neonatal male circumcision rates in the regression analysis. It is therefore of concern that low-income families who receive Medicaid coverage for childbirth seem less likely to opt for infant circumcision in states that do not include circumcision among covered Medicaid benefits. This lack of coverage deprives the most disadvantaged children of an array of apparent health benefits, including fewer urinary tract infections and lower rates of human papillomavirus and HIV infection in the future. In this manner, current efforts to reduce Medicaid costs may generate future health disparities and greater medical costs as a consequence.
Limitations
A limitation of this study was its use of cross-sectional data, which allowed us to detect relationships between predictors and neonatal male circumcision rates but did not provide any proof of causality. A further limitation was that circumcision rates were measured by the presence of ICD-9 procedure codes on hospital discharge records, which a 1985 to 1986 study showed may underreport circumcision.38 We believe that hospital recordkeeping has become more accurate since that time. Further, underreporting of male circumcision would affect our results only in the unlikely event that the underreporting were correlated with the explanatory factors in our model. Some circumcisions are performed outside the hospital, as is the custom among Jewish people and Muslims. Although our hospital-based data did not account for these circumcisions, this omission is unlikely to affect our results, because circumcision is almost universal for Jewish and Muslim boys, who, in any case, account for a minor proportion of all US births. Adult male circumcision is also extremely rare (approximately 50 000 surgeries among nearly 100 million men in 1995, a rate of 0.05%).39
Conclusions
Although religion and culture are strong determinants of the male circumcision decision, we have demonstrated the importance of financing and insurance coverage for some parents. We have shown that the lack of Medicaid coverage for neonatal male circumcision is associated with lower rates of the procedure, with expected long-term differential effects on the health of low-income newborns. Using the regression presented in Table 2, we predicted the effect of the Medicaid policy variable on the circumcision rate under different state policies. If all states whose Medicaid plans did not cover routine, infant male circumcision altered their policy to cover male circumcision, and all other variables remained as they currently are, one would expect the national circumcision rate to increase from the current 55.9% to 62.6%. Alternatively, if all states dropped male circumcision coverage from their Medicaid plans, one would expect only 38.5% of all male infants to be circumcised.
The reevaluation by the AAP of its position on male circumcision is of more than academic interest. The historical record shows that in the wake of the 1999 AAP statement on male circumcision, which adopted a neutral stance, many states opted to remove the procedure from Medicaid coverage. In deciding whether to recommend routine neonatal male circumcision, we believe that the AAP should weigh the impact of their recommendation on the long-term health of both male and female children and the potentially disparate effects of their decisions on poor children.
Acknowledgments
Support for this work was provided by the University of California, Los Angeles, Center for HIV Identification, Prevention and Treatment Services (grant 2P30MH058107).
Human Participant Protection
This study was approved by the University of California, Los Angeles, institutional review board.
References
- 1.Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet 2007;369:657–666 [DOI] [PubMed] [Google Scholar]
- 2.Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet 2007;369:643–656 [DOI] [PubMed] [Google Scholar]
- 3.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 trial. PLoS Med 2005;2:e298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weiss HA, Thomas SL, Munabi SK, Hayes RJ. Male circumcision and risk of syphilis, chancroid, and genital herpes: a systematic review and meta-analysis. Sex Transm Infect 2006;82:101–110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Quinn TC. Viral load, circumcision and heterosexual transmission. Hopkins HIV Rep 2000;12:1,5,11 [PubMed] [Google Scholar]
- 6.Kreiss JK, Hopkins SG. The association between circumcision status and human immunodeficiency virus infection among homosexual men. J Infect Dis 1993;168:1404–1408 [DOI] [PubMed] [Google Scholar]
- 7.Buchbinder SP, Vittinghoff E, Heagerty PJ, et al. Sexual risk, nitrite inhalant use, and lack of circumcision associated with HIV seroconversion in men who have sex with men in the United States. J Acquir Immune Defic Syndr 2005;39:82–89 [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC) Atlanta, GA: CDC; 2008 [Google Scholar]
- 9.National Council for State Legislators. State Health Notes [Web page]. 2006;28(475). Available at: http://www.ncsl.org/print/health/shn/shn475.pdf. Accessed September 19, 2007.
- 10.Healthcare Cost and Utilization Project. Introduction to the HCUP Nationwide Inpatient Sample (NIS); 2004. Available at: http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2004.pdf. Accessed August 2, 2007.
- 11.Centers for Medicare and Medicaid Services, Department of Health and Human Services. Diagnosis and Procedure Codes and Their Abbreviated Titles. Available at: http://www.cms.hhs.gov/IDC9ProviderDiagnosticCodes/06_codes.asp. Accessed November 15, 2006.
- 12.International Coalition for Genital Integrity. Medicaid defunding of nontherapeutic infant circumcision. Available at: http://icgi.org/Medicaid_Project/index.htm. Accessed July 10, 2008.
- 13.Nelson CP, Dunn R, Wan J, Wei JT. The increasing incidence of newborn circumcision: data from the nationwide inpatient sample. J Urol 2005;173:978–981 [DOI] [PubMed] [Google Scholar]
- 14.US Bureau of the Census. Population estimates program. Available at: http://www.census.gov/popest/counties/asrh/files/cc-est2005-alldata-XX.csv [where XX indicates the state]. Accessed April 24, 2007.
- 15.US Bureau of the Census. Population estimates program. Available at: http://www.census.gov/popest/states/asrh/files/SC_EST2005_alldata6_AL_MO.csv and http://www.census.gov/popest/states/asrh/files/SC_EST2005_alldata6_MT_WY.csv. Accessed April 24, 2007.
- 16.Schenker N, Raghunathan TE, Chiu P-L, et al. Multiple imputation of missing income data in the National Health Interview Survey. J Am Stat Assoc 2006;101:924–933 [Google Scholar]
- 17.Snedecor GW, Cochran WG. Statistical Methods. 7th ed.Ames: Iowa State University Press; 1980 [Google Scholar]
- 18. HIV/AIDS Surveillance Report. Cases of HIV Infection and AIDS in the United States and Dependent Areas, 2005. Vol 17. Atlanta, GA: Centers for Disease Control and Prevention; 2006. Available at: http://www.cdc.gov/hiv/topics/surveillance/resources/reports/2005report/default.htm. Accessed March 8, 2007.
- 19.Sullivan PS, Kilmarx PH, Peterman TA, et al. Male circumcision for prevention of HIV transmission: what the new data mean for HIV prevention in the United States. PLoS Med 2007;4:e223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sawires SR, Dworkin SL, Fiamma A, Peacock D, Szekeres G, Coates TJ. Male circumcision and HIV/AIDS: challenges and opportunities. Lancet 2007;369:708–713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zuckerman RA, Whittington WL, Celum CL, et al. Higher concentration of HIV RNA in rectal mucosa secretions than in blood and seminal plasma, among men who have sex with men, independent of antiretroviral therapy. J Infect Dis 2004;190:156–161 [DOI] [PubMed] [Google Scholar]
- 22.Millett G, Ding H, Lauby J, et al. Circumcision status and HIV infection among Black and Latino men who have sex with men in 3 US cities. J Acquir Immune Defic Syndr 2007;46:643–650 [DOI] [PubMed] [Google Scholar]
- 23.Warner L, Ghanem KG, Newman D, et al. Male circumcision and risk of HIV infection among heterosexual men attending Baltimore STD clinics: an evaluation of clinic-based data. Paper presented at: Society for Epidemiologic Research Meeting; June 21–24, 2006; Seattle, WA. Available at: http://cdc.confex.com/cdc/std2006/techprogram/P11223. Accessed September 18, 2007. [Google Scholar]
- 24.Singh-Grewal D, Macdessi J, Craig J. Circumcision for the prevention of urinary tract infection in boys: a systematic review of randomized trials and observational studies. Arch Dis Child 2005;90:853–858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Castellsagué X, Bosch FX, Muñoz N, et al. Male circumcision, penile human papillomavirus infection, and cervical cancer in female partners. N Engl J Med 2002;346:1105–1112 [DOI] [PubMed] [Google Scholar]
- 26.Moses S, Bailey RC, Ronald AR. Male circumcision: assessment of health benefits and risks. Sex Transm Inf 1998;74:368–373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fergusson DM, Boden JM, Horwood LJ. Circumcision status and risk of sexually transmitted infection in young adult males: an analysis of a longitudinal birth cohort. Pediatrics 2006;118:1971–1977 [DOI] [PubMed] [Google Scholar]
- 28. Study presents new information on male circumcision to prevent spread of HIV in Africa [press release]. Montreux, Switzerland: Rakai Health Sciences Program; March 6, 2007.
- 29.Williams BG, Lloyd-Smith JO, Gouws E, et al. The potential impact of male circumcision on HIV in Sub-Saharan Africa. PLoS Med 2006;3:e262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xu F, Markowitz LE, Sternberg MR, Aral SO. Prevalence of circumcision and herpes simplex virus type 2 infection in men in the United States: the National Health and Nutrition Examination Survey (NHANES), 1999–2004. Sex Transm Dis 2007;34:479–484 [DOI] [PubMed] [Google Scholar]
- 31.Health Services/Technology Assessment Committee, National Library of Medicine. Post-delivery care and stabilization of mother and newborn. Health Technology Advisory Committee Final Technology Evaluation Report. 1996. Available at: http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat6.section.2644. Accessed August 2, 2007.
- 32.Health, United States, 2006 With Chartbook on Trends in the Health of Americans. Hyattsville, MD: National Center for Health Statistics; 2006 [PubMed] [Google Scholar]
- 33. Kaiser Family Foundation. Statehealthfacts.org Web site. Births financed by Medicaid as percent of total births, 2002. Available at: http://www.statehealthfacts.org/comparemaptable.jsp?ind=223&cat=4&yr=12&typ=2&o=a&sort=n&print=1. Accessed August 3, 2007.
- 34.Weiss H, Polonsky J. Male Circumcision: Global Trends and Determinants of Prevalence, Safety and Acceptability. London, England: World Health Organization, London School of Hygiene and Tropical Medicine, and UNAIDS; 2007. [Google Scholar]
- 35.Weinstein JN, Bronner KK, Morgan TS, Wennberg JE. Trends and geographic variations in major surgery for degenerative diseases of the hip, knee, and spine. Health Aff (Millwood) 2004;(suppl Web exclusive):VAR81–VAR89 [DOI] [PubMed] [Google Scholar]
- 36.Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES. United States' trends and regional variations in lumbar spine surgery: 1992–2003. Spine 2006;31:2707–2714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Trends in reportable sexually transmitted diseases in the United States, 2005. STD Surveillance 2005. Atlanta, GA: Centers for Disease Control and Prevention; 2006. Available at: http://www.cdc.gov/std/stats/trends2005.htm. Accessed September 26, 2007.
- 38.O'Brien TR, Calle EE, Poole WK. Incidence of neonatal circumcision in Atlanta, 1985–1986. South Med J 1995;88:411–415 [DOI] [PubMed] [Google Scholar]
- 39.Owings MF, Kozak LJ. Ambulatory and inpatient procedures in the United States, 1996. Vital Health Stat 13. 1998;(139):1–119. Available at: http://www.cdc.gov/nchs/data/series/sr_13/sr13_139.pdf. Accessed March 26, 2008. [Google Scholar]