Abstract
The cardiac and skeletal muscle sarcoplasmic reticulum ryanodine receptor Ca2+ release channels contain thiols that are potential targets of endogenously produced reactive oxygen and nitrogen intermediates. Previously, we showed that the skeletal muscle ryanodine receptor (RyR1) has O2-sensitive thiols; only when these thiols are in the reduced state (pO2 ~ 10 mmHg) can physiological concentrations of NO (nanomolar) activate RyR1. Here, we report that cardiac muscle ryanodine receptor (RyR2) activity also depends on pO2, but unlike RyR1, RyR2 was not activated or S-nitrosylated directly by NO. Rather, activation and S-nitrosylation of RyR2 required S-nitrosoglutathione. The effects of peroxynitrite were indiscriminate on RyR1 and RyR2. Our results indicate that both RyR1 and RyR2 are pO2-responsive yet point to different mechanisms by which NO and S-nitrosoglutathione influence cardiac and skeletal muscle sarcoplasmic reticulum Ca2+ release.
Active muscle produces reactive nitrogen and oxygen species that modulate its contraction and relaxation (1–3). The massive skeletal muscle (RyR1)1 and cardiac muscle (RyR2) ryanodine receptors (4, 5) are among the major targets of NO and related molecules in muscle (3, 6–8). NO and/or NO-related species also modulate RyR1 and RyR2 channel activity in vitro [as measured by SR vesicle Ca2+ efflux, activity in lipid bilayers, and [3H]ryanodine binding to RyRs (an indirect assay of RyR channel activity)]. NO and NO donors activate and inhibit the RyRs depending on their concentrations and experimental conditions (9–13). Moreover, the effect of submicromolar NO on RyR1 is dependent on oxygen tension (pO2) (14), requiring low physiological O2 tension to activate the channel. In contrast, drugs such as N-ethyl-2-(1-ethyl-2-hydroxy-2-nitrosohydrazino)ethamine (NOC-12), which generates NO, or 3-morpholinosydnonimine (SIN-1) and S-nitrosoglutathione (GSNO), which generate a variety of reactive nitrogen species, including peroxynitrite, nitrosonium cation (NO+), or NO itself, can chemically modify and activate RyR1 at ambient pO2 (pO2 ~ 150 mmHg) (15–17).
We have reported previously that, in single-channel studies, GSNO and SIN-1 activated the purified RyR2 at ambient pO2 (18), but whether NO can directly modulate RyR2 remains unknown. Further, whether RyR2 contains pO2-sensitive thiols that might alter responsiveness to NO or GSNO remains unknown. In the study presented here, we examine the effects of NO, GSNO, NOC-12, and SIN-1 on RyR2 in SR vesicles at pO2 values of ~150 and ~10 mmHg. We report that RyR2 activity, like RyR1 activity, is dependent on pO2. But in contrast to RyR1, NO and NOC-12 neither effectively S-nitrosylated RyR2 nor activated the channel. RyR2 was nonetheless readily activated by GSNO and SIN-1.
EXPERIMENTAL PROCEDURES
Materials
[3H]Ryanodine was from DuPont NEN (Boston, MA). GSNO, NOC-12, monobromobimane, and myosin light chain kinase-derived CaM binding peptide were from Calbiochem (La Jolla, CA), and SIN-1 was from Molecular Probes (Eugene, OR). NO gas (purity of >99%, National Welders) was scrubbed to remove O2 and nitrite by passage through an argon-purged column filled with KOH pellets and a solution of NaOH. The concentration of NO was determined by a hemoglobin titration assay and NO electrode (WPI Instruments, Sarasota, FL) as described previously (14). Other chemicals were analytical grade.
SR Vesicle Preparations
SR vesicles were prepared from canine heart in the presence of protease inhibitors (100 nM aprotinin, 1 μM leupeptin, 1 μM pepstatin, 1 mM benzamidine, and 0.2 mM phenylmethanesulfonyl fluoride) (19). Recombinant rabbit RyR2s were expressed in human embryonic kidney 293 cells, and crude membrane fractions were prepared as described previously (20).
Determination of Free Thiol and S-Nitrosothiol Content, and pO2 Responsiveness of RyR2
The free thiols in RyR2 gradient fractions were assessed in situ (in cardiac SR vesicles) by the monobromobimane fluorescence method (14). Briefly, cardiac SR vesicles were exposed to 1 mM monobromobimane in the dark at 24 °C for 1 h at a pO2 of ~10 or ~150 mmHg. After solubilization in CHAPS, samples were loaded onto the top of a 7 to 20% continuous sucrose gradient, centrifuged overnight at 4 °C, and fractionated. RyR2 peak fractions, determined in parallel gradients using the RyR-specific ligand [3H]ryanodine (21), were assayed for monobromobimane fluorescence, protein content, and protein composition by SDS-PAGE. The S-nitrosothiol (SNO) content of RyR2 peak fractions was determined by a mercury-coupled photolysis/chemiluminescence method (14).
[3H]Ryanodine Binding
Ryanodine binds with high specificity to the RyRs and is widely used as a probe of channel activity because of its preferential binding to the open channel states (21). Unless otherwise indicated, [3H]ryanodine binding to SR vesicles (0.2 mg of protein/mL) or microsomal membrane fractions containing the recombinant RyR2s (0.4 mg/mL) was assessed at a pO2 of ~10 or ~150 mmHg by incubating samples for 4–5 h at 24 °C with 5 nM [3H]ryanodine in medium containing 0.125 M KCl, 20 mM imidazole (pH 7.0), 0.1 mM EGTA, and Ca2+ concentrations to yield ~5 μM free Ca2+, 0.3 mM Pefabloc, 30 μM leupeptin, and additions given in the figure legends. The level of nonspecific binding was determined using a 1000-fold excess of unlabeled ryanodine. Aliquots of the samples were diluted with 5 volumes of ice-cold water and placed on Whatman GF/B filters soaked with 2% (w/w) polyethyleneimine. Filters were washed with three 5 mL volumes of ice-cold 0.1 M KCl, 1 mM KPipes buffer (pH 7.0), and the radioactivity remaining on the filters was determined by liquid scintillation counting, yielding bound [3H]ryanodine.
Single-Channel Recordings
Single-channel measurements were performed using Mueller-Rudin type planar lipid bilayers containing a 5:3:2 mixture of bovine brain phosphatidylethanolamine, phosphatidylserine, and phosphatidylcholine (25 mg of total phospholipid/mL of n-decane) (22). SR vesicles were added to the cis (SR cytosolic side) chamber of a bilayer apparatus and fused in the presence of an osmotic gradient [250 mM cis CsCH3SO3/20 mM trans CsCH3SO3 in 10 mM CsHepes (pH 7.0)]. After channel activity had appeared, the trans (SR lumenal) CsCH3SO3 concentration was increased to 250 mM to prevent further fusion of membranes. Proteoliposomes containing the purified recombinant RyR2s were recorded in a symmetrical 0.25 M KCl, 20 mM KHepes solution (pH 7.0). The trans side of the bilayer was defined as ground. The large cytosolic regulatory region of the channels faced the cis chamber in a majority (>98%) of the recordings (22). Channel activities were recorded before the addition and 1 min following the subsequent addition of GSNO. Electrical signals were filtered at 2 kHz, digitized at 10 kHz, and analyzed as described previously (22).
Other Biochemical Assays
Free Ca2+ concentrations were obtained by including in the solutions the appropriate amounts of Ca2+ and EGTA using the stability constants and computer program published by Schoenmakers et al. (23). Free Ca2+ concentrations were verified with the use of a Ca2+ selective electrode. The protein concentrations were determined using the Amido Black method (24).
Data Analysis
Results are given as means ± the standard error (SE). Significance of differences was analyzed with a Student’s t test. Differences were regarded to be significant at p < 0.05.
RESULTS
Oxygen Tension-Sensitive RyR2 Thiols
As we have reported previously, S-nitrosylation and activation of RyR1 by NO are linked to the redox state of pO2-sensitive thiols within the channel (25). We asked whether RyR2 also contains pO2-sensitive thiols and, if so, whether the redox state of these thiols is also linked to the modulation of RyR2 channel activity by NO. We first determined the activity of RyR2 at low (pO2 ~ 10 mmHg) and ambient (pO2 ~ 150 mmHg) oxygen tensions, using a ligand binding assay. With or without exogenously added GSH or GSSG, [3H]ryanodine binding was modestly (0.87 ± 0.06 and 0.96 ± 0.04 in the presence of 5 mM GSSG, 0.73 ± 0.05 and 0.84 ± 0.05 in the absence of glutathione, and 0.72 ± 0.06 and 0.81 ± 0.07 in the presence of 5 mM GSH, all in picomoles per milligram of protein) increased in the more oxidized forms of RyR2 (at pO2 ~ 150 mmHg) (Figure 1). Thus, RyR2 activity is pO2-regulated.
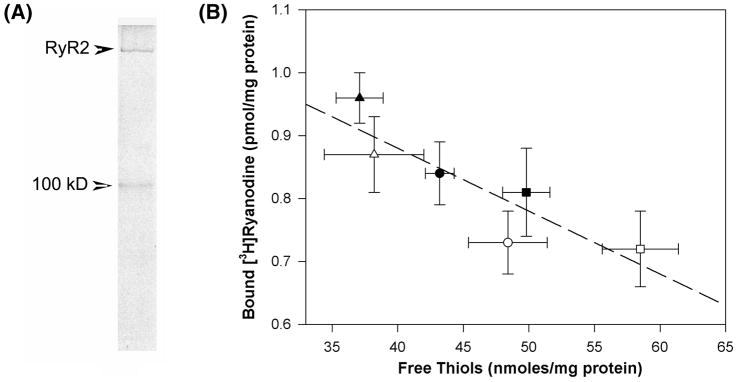
Figure 1.
Control of the redox state of RyR2-enriched gradient fractions and RyR2 activity by pO2 (oxygen tension) and glutathione redox potential. (A) Coomassie-stained gel of a RyR2-enriched sucrose gradient fraction electrophoresed through a 3 to 12% SDS-polyacrylamide gel. (B) [3H]Ryanodine binding and free thiol content determined as described in Experimental Procedures either in the absence (○ and ●) or in the presence of 5 mM GSH (□ and ■) or 5 mM GSSG (△ and ▲ ) at a pO2 of ~10 mmHg (empty symbols) or 150 mmHg (filled symbols). Data are means ± SE of three or four experiments. A linear correlation coefficient of 0.88 (n = 22) suggests a highly significant correlation between the free thiol content of RyR2-enriched gradient fractions and RyR2 activity (---).
The number of free thiols in RyR2-enriched sucrose gradient fractions was determined using the thiol-specific probe monobromobimane. SDS-PAGE showed that RyR2-enriched gradient fractions contained two protein bands with an apparent molecular mass corresponding to RyR2 and a second band with an apparent molecular mass of 100 kDa (Figure 1A). Quantitative analysis of Coomassie-stained gels indicated that RyR2 amounted to 59 ± 5% (n = 4) of the protein content in RyR2-enriched fractions. Under ambient oxygen tension in the absence of glutathione, RyR2 gradient fractions contained 43.1 ± 1.8 nmol free thiols/mg of protein (Figure 1B). The number increased to 48.5 ± 1.4 nmol free thiols/mg of protein at a pO2 of ~10 mmHg. Furthermore, RyR2-enriched gradient fractions contained pO2-sensitive thiols even in the presence of high concentrations of reducing equivalents comparable to those found in intact cells [5 mM glutathione (GSH)]. The number of free thiols in the presence of 5 mM GSH was 49.6 ± 1.8 and 58.5 ± 2.9 nmol thiols/mg of protein at pO2 values of ~150 and ~10 mmHg, respectively. The effects of oxidizing conditions produced by oxidized glutathione (GSSG) were also probed. In the presence of 5 mM GSSG, a decrease in oxygen tension from ~150 to ~10 mmHg had a modest effect, increasing the number of free thiols from 37.5 ± 1.8 to 38.5 ± 3.8 nmol thiols/mg of protein. Thus, a good correlation between RyR2 activity and free thiol content exists in RyR2 gradient fractions; however, because RyR2 was purified only by 60%, the exact number of pO2-sensitive thiols in native RyR2 remains to be determined.
Physiological Concentrations of NO neither Modulate nor S-Nitrosylates RyR2 at either Physiological or Ambient O2 Tension
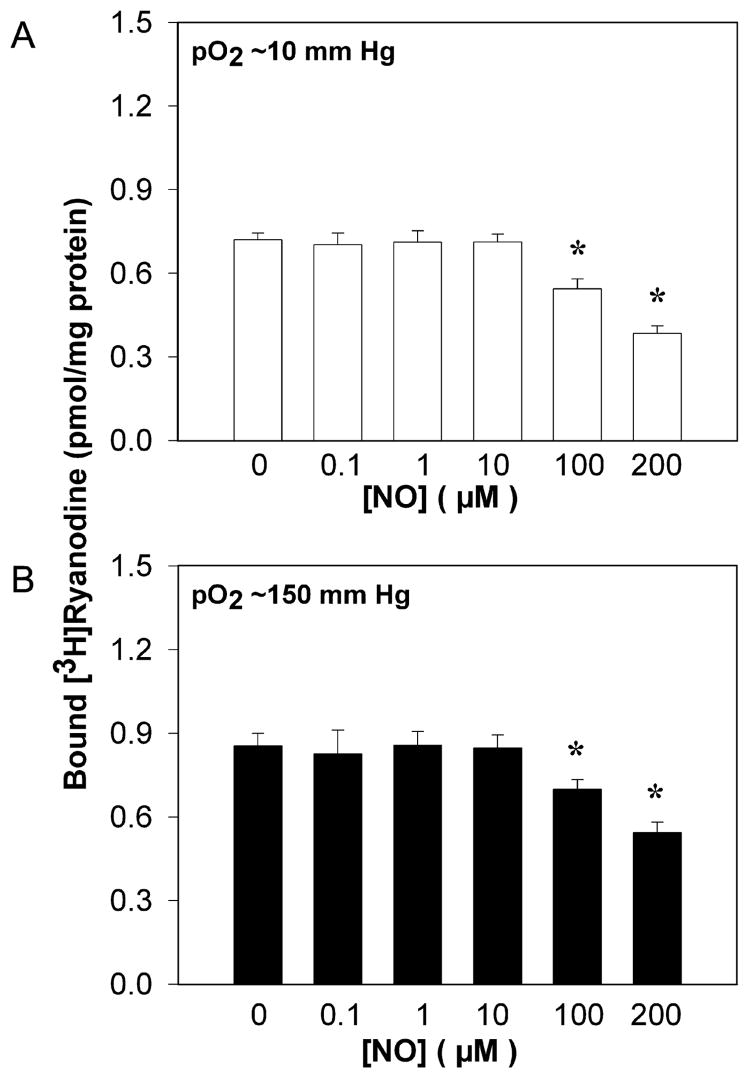
We treated cardiac SR vesicles with a range of NO concentrations at pO2 values of ~10 and ~150 mmHg. We determined the activity of NO-treated RyR2 using [3H]ryanodine binding, and the extent of S-nitrosylation in RyR2-enriched gradient fractions using a photolysis/chemiluminescence assay (14). Unlike RyR1 (14), RyR2 was not activated or S-nitrosylated by 1 μM NO at a pO2 of ~10 mmHg (Figure 2A and Table 1). At an ambient oxygen tension of ~150 mmHg, physiological concentrations of NO were also without effect (Figure 2B and Table 1). Supraphysiological amounts of NO (≥100 μM) inhibited RyR2 at both high and low O2 tensions.
Figure 2.
Effect of gaseous NO on [3H]ryanodine binding of cardiac muscle SR at pO2 values of ~10 and ~150 mmHg. The level of specific [3H]ryanodine binding to cardiac SR vesicles was determined by incubating samples at ~10 (A) and ~150 mmHg (B) at the indicated initial NO concentration for 4–5 h at 24 °C as described in Experimental Procedures. Data are means ± SE of three or four experiments. An asterisk denotes p < 0.05, compared with each control (−NO).
Table 1.
Free Thiol (SH) and S-Nitrosothiol (SNO) Contents of RyR2-Enriched Gradient Fractions and [3H]Ryanodine Binding Levels in the Absence and Presence of NO and Related Moleculesa
| addition | free thiol content (nmol/mg of protein) | S-nitrosothiol content (nmol/mg of protein) | [3H]ryanodine binding level (pmol/mg of protein) |
|---|---|---|---|
| pO2 ~ 10 mmHg | |||
| none | 48.5 ± 1.4 | 0.41 ± 0.27 | 0.72 ± 0.02 |
| NO (1 μM) | NDb | 0.39 ± 0.14 | 0.71 ± 0.02 |
| NOC-12 (0.1 mM) | NDb | 0.13 ± 0.13 | 0.73 ± 0.02 |
| GSNO (0.2 mM) | 45.6 ± 1.1 | 3.56 ± 0.36c | 1.12 ± 0.03c |
| SIN-1 (0.2 mM) | 39.1 ± 0.7c | NDb | 0.95 ± 0.06c |
| pO2 ~ 150 mmHg | |||
| none | 43.2 ± 1.8 | 0.45 ± 0.27 | 0.85 ± 0.03 |
| NO (1 μM) | NDb | 0.59 ± 0.32 | 0.83 ± 0.04 |
| NOC-12 (0.1 mM) | NDb | 0.23 ± 0.16 | 0.83 ± 0.02 |
| GSNO (0.2 mM) | 40.2 ± 1.8 | 4.80 ± 0.30c | 1.29 ± 0.03c |
| SIN-1 (0.2 mM) | 35.7 ± 0.7c | NDb | 0.96 ± 0.03c |
The amount of free thiols (SH) and the amount of S-nitrosylation (SNO) of RyR2-enriched gradient fractions were determined as described in Experimental Procedures. The [3H]ryanodine binding level was determined as described in the legend of Figure 1 with a pO2 of ~10 or ~150 mmHg in the presence of the indicated additions. Data are means ± SE of three to five experiments.
Not determined.
p < 0.05 compared with control (no addition).
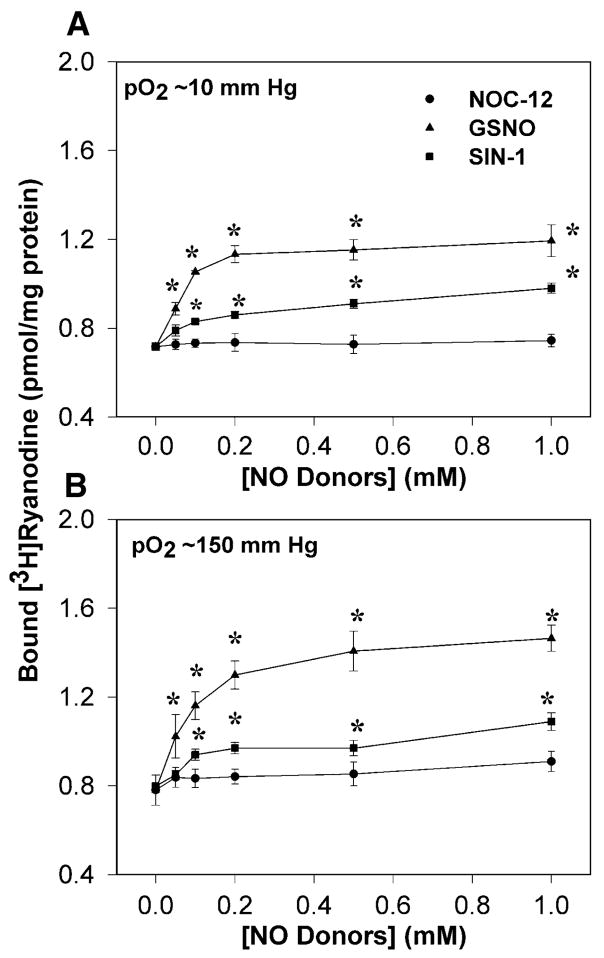
Effects of NO Donors, S-Nitrosothiols, and Peroxynitrite
Compounds capable of donating NO and/or NO+ are widely used to mimic the effects of NO synthases in cellular studies (26). We tested the effects of NOC-12 which releases NO with a half-time of ~6 h (27) and GSNO which releases NO with a half-time of ~3 h under our conditions (27) [but can also modulate protein function by S-transnitros(yl)ation (28, 29)]. As shown in Figure 3, at 0.1 mM NOC-12 did not affect the binding of [3H]ryanodine to cardiac SR vesicles at a pO2 of ~10 or ~150 mmHg or S-nitrosylated RyR2 (Table 1). In contrast, GSNO, from 50 μM to 1 mM, activated RyR2 at either O2 tension. The activating effect of GSNO reached a near-maximal level at 0.2 mM (Figure 3). At that concentration, the S-nitrosothiol content in RyR2-enriched gradient fractions was increased from ~0.4 to ~4 nmol/mg of protein (Table 1). In reasonable agreement, the free thiol content per RyR2 subunit decreased by ~3 nmol/mg of protein in the presence of GSNO.
Figure 3.
Effects of NOC-12, GSNO, and SIN-1 on [3H]ryanodine binding of cardiac muscle SR. The level of specific [3H]ryanodine binding to cardiac SR vesicles was determined by incubating samples at pO2 values of ~10 (A) and ~150 mmHg (B) in the presence of the indicated initial concentrations of NOC-12 (●), GSNO (▲), or SIN-1 (■) for 4–5 h at 24 °C as described in Experimental Procedures. Data are means ± SE of three or four experiments. An asterisk indicates p < 0.05, compared with each control.
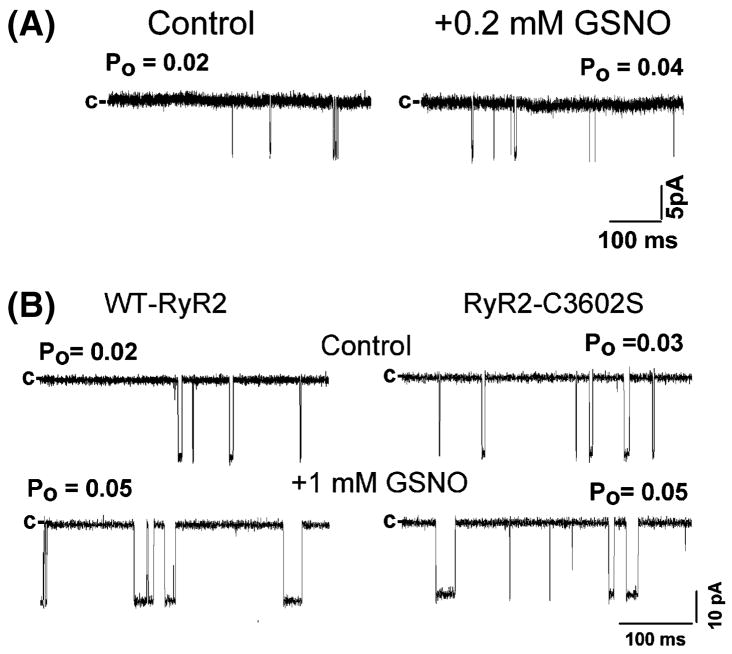
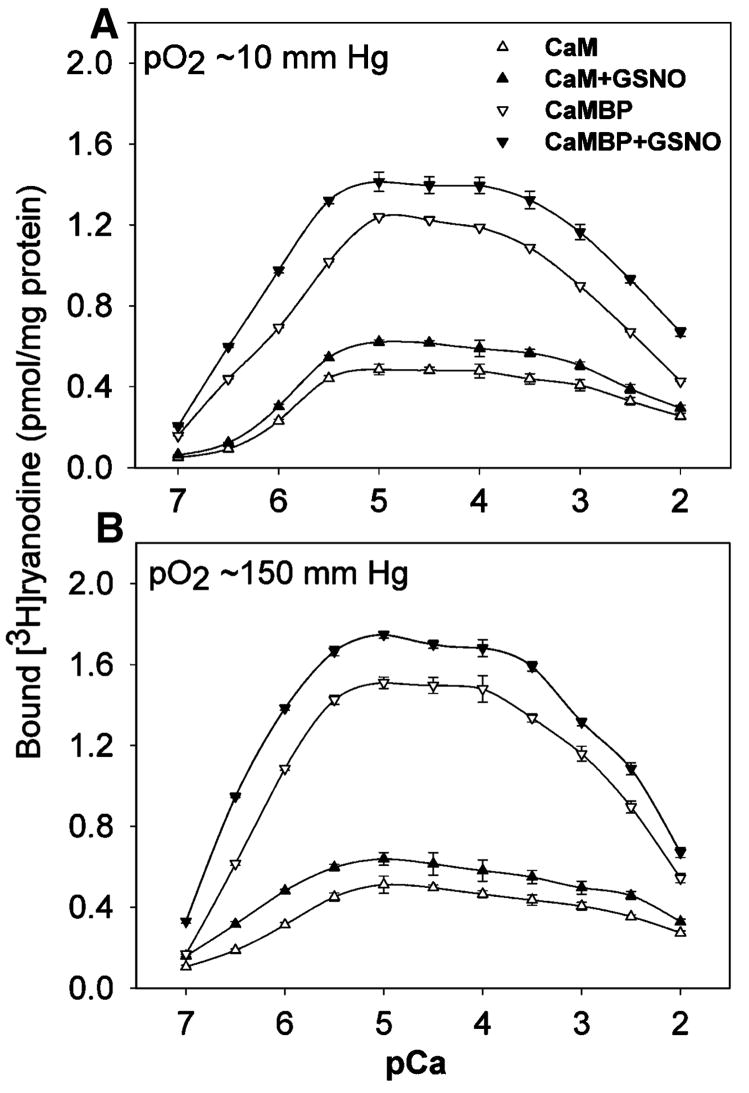
The effects of GSNO on RyR2 were further examined in single-channel measurements. Figure 4A shows the current fluctuations of a single RyR2 ion channel. In the left trace, the channel was partially activated by ~0.7 μM free cis (cytosolic) Ca2+. Addition of 0.2 mM GSNO increased the single-channel open probability (Po) ~2-fold (Figure 4A, right trace). Kinetic analysis indicated that GSNO increased Po by increasing the number of single-channel events [270 ± 54 vs 657 ± 57 events/min (n = 4)] without significantly changing the mean open times. Previously, we found that NO and NOC-12 activated RyR1 via S-nitrosylation of Cys3635 which is contained within the calmodulin (CaM) binding domain of RyR1 (14, 16). S-Nitrosylation of Cys3635 reversed the inhibitory effect of CaM on RyR1. In contrast, activation of RyR1 by GSNO was independent of Cys3635 and CaM. Likewise, we find that the corresponding RyR2 cysteine (Cys3602) was not required for RyR2 activation by GSNO in single-channel measurements (Figure 4B). In [3H]ryanodine binding measurements, across the range of Ca2+ concentrations tested (from 0.1 μM to 10 mM), GSNO activated the native RyR2 as it did the native RyR1, both with exogenous CaM (1 μM CaM) added to the medium or following removal of endogenous CaM using 0.1 μM myosin light chain kinase-derived CaM binding peptide (30) (Figure 5).
Figure 4.
Effects of GSNO on single-RyR2 channel activities. (A) Single-channel currents (downward deflections from closed levels, c-) of native RyR2 were recorded at −35 mV as described in Experimental Procedures in 0.25 M CsCH3SO3 buffer in the presence of ~0.7 μM free Ca2+ cis without (left trace) and 1 min after the subsequent addition of 0.2 mM GSNO (right trace) to the cis (cytosolic) chamber of the bilayer setup. Averaged channel parameters were as follows in the absence and presence of GSNO: Po = 0.016 ± 0.004 and 0.037 ± 0.008, 270 ± 54 and 657 ± 57 events/min, To (open mean times) = 2.12 ± 0.33 and 3.66 ± 1.47 ms, and Tc (closed mean times) = 242 ± 41 and 109 ± 19 ms, respectively. Channel parameters were calculated from four recordings that contained a single channel activity. The differences of Po, the number of channel events, and Tc between control and those with GSNO are significant (p < 0.05). (B) Single recombinant WT and C3602S mutant channels were recorded as for panel A in 0.25 M KCl buffer without (top trace) and after the subsequent addition of 1 mM GSNO (bottom trace) to the cis (cytosolic) chamber of the bilayer setup. Averaged channel parameters were as follows in the absence and presence of GSNO: for wild-type RyR2, Po = 0.03 ± 0.02 and 0.10 ± 0.08 (n = 5), respectively; for RyR2-C3602S, Po = 0.04 ± 0.02 and 0.07 ± 0.03 (n = 6), respectively. The normalized Po is significant compared to each control (−GSNO) (p < 0.05).
Figure 5.
Effect of GSNO on the Ca2+ dependence of [3H]ryanodine binding in the presence of calmodulin or calmodulin binding peptide. The level of specific [3H]ryanodine binding to cardiac SR vesicles was determined by incubating samples at pO2 values of ~10 (A) and ~150 mmHg (B) in the presence of the indicated concentrations of free Ca2+, in the absence or presence of 0.2 mM GSNO, and in the presence of either 1 μM CaM or 0.1 μM CaM binding peptide (CaMBP). Data are means ± SE of four experiments.
We also probed the effect on RyR2 of 3-morpholinosydnomine (SIN-1), which releases both NO and superoxide (O2−) at a 1:1 ratio, thus generating peroxynitrite (ONOO−) (31). We previously showed that SIN-1 oxidized and thereby activated the purified RyR2 at ambient oxygen tension (18). To determine the effects of SIN-1 on native RyR2, cardiac SR vesicles were treated with 0–1 mM SIN-1 at pO2 values of ~10 and ~150 mmHg. SIN-1 increased the level of [3H]ryanodine binding to cardiac SR vesicles in a concentration-dependent manner at both O2 tensions (Figure 3). At a concentration of 0.2 mM, SIN-1 activation was associated with the loss of ~7–9 nmol of free cysteine residues/mg of protein in RyR2-enriched gradient fractions (Table 1).
DISCUSSION
Cardiac contractility in the healthy heart is enhanced by nNOS through S-nitrosylation of RyR2 (7). By contrast, oxidation of the RyR2 by xanthine oxidase, which coprecipitates with nNOS and RyR2, has been assigned a role in pathophysiological states such as heart failure (7, 32): cardiac contractility may thus be enhanced or impaired through nitrosative and oxidative effects of NO and SNO or peroxynitrite on RyR2. The exact molecular mechanisms by which NO and SNO modulate contractility in healthy versus diseased hearts are still unclear. A major goal of this study was therefore to characterize regulation of RyR2 activity by endogenous reactive nitrogen species (NO, GSNO, and peroxynitrite). In addition, since cardiac tissue is low in pO2 and frequently subjected to oxidative insults, we sought to understand the influence of pO2 on cardiac channel activity.
Our studies suggest that GSNO may serve as a major effector of NO bioactivity in the heart. We report that RyR2 channel function is regulated by GSNO (not NO) and sensitive to both oxygen tension and GSH:GSSG ratio, albeit to a lesser extent than RyR1. The redox responsiveness of RyRs correlated directly with free thiol content in RyR2-enriched gradient fractions, indicating that RyR2 thiols are modified. These data strongly suggest a cause and effect relationship between redox-based modification of RyR2 and channel activation. We are not, however, able to dispositively assign the modified thiols to RyR2 because of the presence of another contaminating protein with a molecular mass of ~100 kDa. In addition, we report that RyR2 activation by peroxynitrite correlated with oxidation of free thiols in RyR2-enriched gradient fractions. Overall, these data support the idea that RyR activity is regulated under (patho)physiological conditions by GSNO and oxidation.
RyR oxidation in vivo is likely to involve different effectors under physiological and pathophysiological conditions. Peroxynitrite formation, for example, is favored when NO and superoxide (O2−) concentrations increase, as in the postischemic heart. Peroxynitrite is an indiscriminant oxidant, readily oxidizing thiols to higher S-oxides and thus predisposing the heart to cellular injury (33). Oxidation of RyR2 by peroxynitrite is likely to adversely impact contractile function.
Mammalian tissues express three nitric oxide synthase isoforms: endothelial (eNOS), neuronal (nNOS), and inducible (iNOS) nitric oxide synthases. In normal cardiac and skeletal muscle, the predominant constitutive isoforms eNOS and nNOS are targeted to different subcellular compartments with nNOS colocalizing with RyR1 and RyR2 (34). In mice with a malignant hyperthermia mutation (RyR1-Y522S), an increased RyR1 activity increased the level of formation of reactive nitrogen species which by S-nitrosylating the mutant channels increased the rate of temperature-sensitive SR Ca2+ release (35). Repeated exercise in mice resulted in an increased level of RyR1 S-nitrosylation, which may have contributed to the formation of “leaky” channels and decreased exercise capacity (36). Functional studies with nNOS−/− and eNOS−/− mice showed that the two isoforms have divergent effects on cardiac SR Ca2+ cycling and thus contractility (37, 38). nNOS is found by immunoelectron microscopy in cardiac muscle SR (39), and a selective association of nNOS with RyR2 has been reported (37). Elimination of nNOS in cardiomyocytes led to RyR2 hyponitrosylation, increased diastolic Ca2+ levels, and a proarrhthmic phenotype (32). It has been suggested that under physiological conditions, nNOS may primarily generate GSNO, which can either release NO or transfer NO+ to acceptor thiols (40). The results of this study suggest that nNOS exerts its physiological effects on cardiac SR Ca2+ release via the transnitrosylative action of GSNO.
We showed previously that a submicromolar NO level activates RyR1 at a pO2 of ~10 mmHg but not at a pO2 of ~150 mmHg (14). In contrast, NOC-12 activated RyR1 in a manner independent of pO2 (16), a behavior that may result from its direct interaction with the channel. Nonetheless, modulation of RyR1 activity by both NO and NOC-12 depends on CaM and is mediated by S-nitrosylation of Cys3635. The same conserved cysteine in RyR2 (RyR2-C3602 vs RyR1-C3635) is part of a putative hydrophobic motif for S-nitrosylation (41). However, neither 1 μM NO nor 0.1 mM NOC-12 [which releases NO with a peak concentration of 2.6 μM under our conditions (16)] nitrosylated RyR2 or altered RyR2 activity. RyR2 activity was not activated by NO or NOC-12 regardless of whether CaM was present.
Under physiological conditions, GSNO can modulate protein function by release of NO or by S-transnitros(yl)ation, the direct transfer of NO+ to cysteine thiols [S-glutathiolation by GSNO, a minor side reaction mediated by byproducts accumulated during GSNO decomposition (42), is unlikely to be relevant]. It is difficult to rationalize the involvement of released NO, as neither NO itself nor NOC-12, which releases NO, can activate RyR2. We also note that the number of thiols nitrosylated by GSNO correlated well with the total number of free thiols lost. Taken together, our data indicate that S-nitrosylation, through NO group transfer chemistry, is the most straightforward explanation in this case.
In conclusion, we show that RyR2, like RyR1, is an oxygen-responsive ion channel suggestive of a class effect for RyRs and, more broadly, for a subset of thiol-regulatory channels (43). However, whereas pO2 serves to modulate the NO responsiveness of RyR1, enhancing channel activity at physiological pO2, RyR2 does not respond to NO. Differences in pO2 regulation thus reflect, in part, the nature of the nitrosylating species: NO in skeletal muscle and GSNO in the heart. Our data point to GSNO serving as a major effector of NO bioactivity in the heart.
Acknowledgments
We thank Daniel Pasek for his assistance with the studies.
Footnotes
The work was supported by National Institutes of Health Grants HL073051 and AR016867 (to G.M.), HL081285 (to J.P.E.), and HL059130 (to J.S.S.).
Abbreviations: SR, sarcoplasmic reticulum; RyR, ryanodine receptor; RyR1, skeletal muscle isoform of RyR; RyR2, cardiac muscle isoform of RyR; NO, nitric oxide; GSNO, S-nitrosoglutathione; NOC-12, N-ethyl-2-(1-ethyl-2-hydroxy-2-nitrosohydrazino)ethamine; SIN-1, 3-morpholinosydnonimine; CaM, calmodulin; pO2, partial pressure of oxygen.
References
- 1.Reid MB. Reactive oxygen and nitric oxide in skeletal muscle. News Physiol Sci. 1996;11:114–121. [Google Scholar]
- 2.Ji LL. Exercise-induced oxidative stress in the heart. In: Sen CK, Packer L, Hanninen O, editors. Handbook of exercise and oxygen toxicity. Elsevier Science; Amsterdam: 2000. pp. 689–712. [Google Scholar]
- 3.Stamler JS, Meissner G. Physiology of nitric oxide in skeletal muscle. Physiol Rev. 2001;81:209–237. doi: 10.1152/physrev.2001.81.1.209. [DOI] [PubMed] [Google Scholar]
- 4.Fill M, Copello JA. Ryanodine receptor calcium release channels. Physiol Rev. 2002;82:893–922. doi: 10.1152/physrev.00013.2002. [DOI] [PubMed] [Google Scholar]
- 5.Meissner G. Regulation of mammalian ryanodine receptors. Front Biosci. 2002;7:2072–2080. doi: 10.2741/A899. [DOI] [PubMed] [Google Scholar]
- 6.Salama G, Menshikova EV, Abramson JJ. Molecular interaction between nitric oxide and ryanodine receptors of skeletal and cardiac sarcoplasmic reticulum. Antioxid Redox Signaling. 2000;2:5–16. doi: 10.1089/ars.2000.2.1-5. [DOI] [PubMed] [Google Scholar]
- 7.Hare JM, Stamler JS. NO/redox disequilibrium in the failing heart and cardiovascular system. J Clin Invest. 2005;115:509–517. doi: 10.1172/JCI200524459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hidalgo C, Donoso P. Crosstalk between calcium and redox signaling: From molecular mechanisms to health implications. Antioxid Redox Signaling. 2008;10:1275–1312. doi: 10.1089/ars.2007.1886. [DOI] [PubMed] [Google Scholar]
- 9.Aghdasi B, Reid MB, Hamilton SL. Nitric oxide protects the skeletal muscle Ca2+ release channel from oxidation induced activation. J Biol Chem. 1997;272:25462–25467. doi: 10.1074/jbc.272.41.25462. [DOI] [PubMed] [Google Scholar]
- 10.Hart JD, Dulhunty AF. Nitric oxide activates or inhibits skeletal muscle ryanodine receptors depending on its concentration, membrane potential and ligand binding. J Membr Biol. 2000;173:227–236. doi: 10.1007/s002320001022. [DOI] [PubMed] [Google Scholar]
- 11.Suko J, Drobny H, Hellmann G. Activation and inhibition of purified skeletal muscle calcium release channel by NO donors in single channel current recordings. Biochim Biophys Acta. 1999;1451:271–287. doi: 10.1016/s0167-4889(99)00098-1. [DOI] [PubMed] [Google Scholar]
- 12.Meszaros LG, Minarovic I, Zahradnikova A. Inhibition of the skeletal muscle ryanodine receptor calcium release channel by nitric oxide. FEBS Lett. 1996;380:49–52. doi: 10.1016/0014-5793(96)00003-8. [DOI] [PubMed] [Google Scholar]
- 13.Zahradnikova A, Minarovic I, Venema RC, Meszaros LG. Inactivation of the cardiac ryanodine receptor calcium release channel by nitric oxide. Cell Calcium. 1997;22:447–454. doi: 10.1016/s0143-4160(97)90072-5. [DOI] [PubMed] [Google Scholar]
- 14.Eu JP, Sun J, Xu L, Stamler JS, Meissner G. The skeletal muscle calcium release channel: Coupled O2 sensor and NO signaling functions. Cell. 2000;102:499–509. doi: 10.1016/s0092-8674(00)00054-4. [DOI] [PubMed] [Google Scholar]
- 15.Sun J, Xu L, Eu JP, Stamler JS, Meissner G. Classes of thiols that influence the activity of the skeletal muscle calcium release channel. J Biol Chem. 2001;276:15625–15630. doi: 10.1074/jbc.M100083200. [DOI] [PubMed] [Google Scholar]
- 16.Sun J, Xu L, Eu JP, Stamler JS, Meissner G. Nitric oxide, NOC-12 and S-nitrosoglutathione modulate the skeletal muscle calcium release channel/ryanodine receptor by different mechanisms: An allosteric function for O2 in S-nitrosylation of the channel. J Biol Chem. 2003;278:8184–8189. doi: 10.1074/jbc.M211940200. [DOI] [PubMed] [Google Scholar]
- 17.Aracena-Parks P, Goonasekera SA, Gilman CP, Dirksen RT, Hidalgo C, Hamilton SL. Identification of cysteines involved in S-nitrosylation, S-glutathionylation, and oxidation to disulfides in ryanodine receptor type 1. J Biol Chem. 2006;281:40354–40368. doi: 10.1074/jbc.M600876200. [DOI] [PubMed] [Google Scholar]
- 18.Xu L, Eu JP, Meissner G, Stamler JS. Activation of the cardiac calcium release channel (ryanodine receptor) by poly-S-nitrosylation. Science. 1998;279:234–237. doi: 10.1126/science.279.5348.234. [DOI] [PubMed] [Google Scholar]
- 19.Meissner G, Henderson JS. Rapid calcium release from cardiac sarcoplasmic reticulum vesicles is dependent on Ca2+ and is modulated by Mg2+, adenine nucleotide, and calmodulin. J Biol Chem. 1987;262:3065–3073. [PubMed] [Google Scholar]
- 20.Yamaguchi N, Xu L, Pasek DA, Evans KE, Meissner G. Molecular basis of calmodulin binding to cardiac muscle Ca2+ release channel (ryanodine receptor) J Biol Chem. 2003;278:23480–23486. doi: 10.1074/jbc.M301125200. [DOI] [PubMed] [Google Scholar]
- 21.Sutko JL, Airey JA, Welch W, Ruest L. The pharmacology of ryanodine and related compounds. Pharmacol Rev. 1997;49:53–98. [PubMed] [Google Scholar]
- 22.Xu L, Meissner G. Regulation of cardiac muscle Ca2+ release channel by sarcoplasmic reticulum lumenal Ca2+ Biophys J. 1998;75:2302–2312. doi: 10.1016/S0006-3495(98)77674-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schoenmakers TJ, Visser GJ, Flik G, Theuvenet AP. CHELATOR: An improved method for computing metal ion concentrations in physiological solutions. BioTechniques. 1992;12:870–879. [PubMed] [Google Scholar]
- 24.Kaplan RS, Pedersen PL. Determination of microgram quantities of proteins in the presence of milligram levels of lipid with amido black 10B. Anal Biochem. 1985;150:97–104. doi: 10.1016/0003-2697(85)90445-2. [DOI] [PubMed] [Google Scholar]
- 25.Sun J, Xin C, Eu JP, Stamler JS, Meissner G. Cysteine-3635 is responsible for skeletal muscle ryanodine receptor modulation by NO. Proc Natl Acad Sci USA. 2001;98:11158–11162. doi: 10.1073/pnas.201289098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feelish M. The use of nitric oxide donors in pharmacological studies. Naunyn-Schmiedeberg’s Arch Pharmakol. 1998;358:113–122. doi: 10.1007/pl00005231. [DOI] [PubMed] [Google Scholar]
- 27.Fitzhugh AL, Keefer LK. Diazeniumdiolates: Pro-and antioxidant applications of the “NONOates”. Free Radical Biol Med. 2000;28:1463–1469. doi: 10.1016/s0891-5849(00)00251-3. [DOI] [PubMed] [Google Scholar]
- 28.Feelish M, Kubitzek D, Werringloer J. The oxyhemoglobin assay. In: Feelish M, Stamler JS, editors. Methods in Nitric Oxide Research. John Wiley and Sons; Chichester, U.K: 1996. pp. 455–478. [Google Scholar]
- 29.Hogg N. The biochemistry and physiology of S-nitrosothiols. Annu Rev Pharmacol Toxicol. 2002;42:585–600. doi: 10.1146/annurev.pharmtox.42.092501.104328. [DOI] [PubMed] [Google Scholar]
- 30.Balshaw DM, Xu L, Yamaguchi N, Pasek DA, Meissner G. Calmodulin binding and inhibition of cardiac muscle calcium release channel (ryanodine receptor) J Biol Chem. 2001;276:20144–20153. doi: 10.1074/jbc.M010771200. [DOI] [PubMed] [Google Scholar]
- 31.Feelish M, Stamler JS. Methods in Nitric Oxide Research. John Wiley and Sons; Chichester, U.K: 1996. Donors of nitrogen oxdes; pp. 71–117. [Google Scholar]
- 32.Gonzalez DR, Beigi F, Treuer AV, Hare JM. Deficient ryanodine receptor S-nitrosylation increases sarcoplasmic reticulum calcium leak and arrhythmogenesis in cardiomyocytes. Proc Natl Acad Sci USA. 2007;104:20612–20617. doi: 10.1073/pnas.0706796104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang P, Zweier JL. Measurement of nitric oxide and peroxynitrite generation in the postischemic heart. J Biol Chem. 1996;271:29223–29230. doi: 10.1074/jbc.271.46.29223. [DOI] [PubMed] [Google Scholar]
- 34.Salanova M, Schiffl G, Rittweger J, Felsenberg D, Blottner D. Ryanodine receptor type-1 (RyR1) expression and protein S-nitrosylation pattern in human soleus myofibres following bed rest and exercise countermeasure. Histochem Cell Biol. 2008;130:105–118. doi: 10.1007/s00418-008-0399-6. [DOI] [PubMed] [Google Scholar]
- 35.Durham WJ, Aracena-Parks P, Long C, Rossi AE, Goonasekera SA, Boncompagni S, Galvan DL, Gilman CP, Baker MR, Shirokova N, Protasi F, Dirksen R, Hamilton SL. RyR1 S-nitrosylation underlies environmental heat stroke and sudden death in Y522S RyR1 knockin mice. Cell. 2008;133:53–65. doi: 10.1016/j.cell.2008.02.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bellinger AM, Reiken S, Dura M, Murphy PW, Deng SX, Landry DW, Nieman D, Lehnart SE, Samaru M, LaCampagne A, Marks AR. Remodeling of ryanodine receptor complex causes “leaky” channels: A molecular mechanism for decreased exercise capacity. Proc Natl Acad Sci USA. 2008;105:2198–2202. doi: 10.1073/pnas.0711074105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barouch LA, Harrison RW, Skaf MW, Rosas GO, Cappola TP, Kobeissi ZA, Hobai IA, Lemmon CA, Burnett AL, O’Rourke B, Rodriguez ER, Huang PL, Lima JAC, Berkowitz DE, Hare JM. Nitric oxide regulates the heart by spatial confinement of nitric oxide synthase isoforms. Nature. 2002;416:337–340. doi: 10.1038/416337a. [DOI] [PubMed] [Google Scholar]
- 38.Khan SA, Hare JM. The role of nitric oxide in the physiological regulation of Ca2+ cycling. Curr Opin Drug Discovery Dev. 2003;6:658–666. [PubMed] [Google Scholar]
- 39.Xu KY, Huso DL, Dawson TM, Bredt DS, Becker LC. Nitric oxide synthase in cardiac sarcoplasmic reticulum. Proc Natl Acad Sci USA. 1999;96:657–662. doi: 10.1073/pnas.96.2.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mayer B, Pfeiffer S, Schrammel A, Koesling D, Schmidt K, Brunner F. A new pathway of nitric oxide/cyclic GMP signaling involving S-nitrosoglutathione. J Biol Chem. 1998;273:3264–3270. doi: 10.1074/jbc.273.6.3264. [DOI] [PubMed] [Google Scholar]
- 41.Stamler JS, Lamas S, Fang FC. Nitrosylation: The prototypic redox-based signaling mechanism. Cell. 2001;106:675–683. doi: 10.1016/s0092-8674(01)00495-0. [DOI] [PubMed] [Google Scholar]
- 42.Tao L, English AM. Protein S-glutathiolation triggered by decomposed S-nitrosoglutathione. Biochemistry. 2004;43:4028–4038. doi: 10.1021/bi035924o. [DOI] [PubMed] [Google Scholar]
- 43.Takahashi H, Shin Y, Cho SJ, Zago WM, Nakamura T, Gu Z, Ma Y, Furukawa H, Liddington R, Zhang D, Tong G, Chen HS, Lipton SA. Hypoxia enhances S-nitrosylation-mediated NMDA receptor inhibition via a thiol oxygen sensor motif. Neuron. 2007;53:53–64. doi: 10.1016/j.neuron.2006.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]