Abstract
Objective
We examined the prevalence, patterns, and correlates of adolescents' abuse, subthreshold dependence ("diagnostic orphans"), and dependence on prescription pain relievers (PPRs) such as opioids in a representative national sample (N = 36,992).
Method
Data were from the 2005–2006 National Surveys of Drug Use and Health. DSM-IV criteria for abuse and dependence were examined.
Results
Of all adolescents aged 12–17, 7% (n = 2,675) reported non-prescribed PPR use in the past year, and 1% (n = 400) met criteria for past-year PPR abuse or dependence. Among the 2,675 adolescents who reported non-prescribed PPR use, more than one in three reported symptoms of abuse or dependence: 7% abuse, 20% subthreshold dependence, and 9% dependence. Regular PPR use, major depressive episodes, and alcohol use disorders were associated with each diagnostic category. Compared with asymptomatic non-prescribed PPR users, increased odds of abuse were noted among non-students (AOR=2.6), users of mental health services (AOR=1.8), and those reporting poor or fair health (AOR=2.4); and increased odds of dependence were observed among females (AOR=1.6), those who were involved in selling illicit drugs (AOR=1.7), and users of multiple drugs (AOR=2.9). Subthreshold dependent users resembled dependent users in major depressive episodes (AOR=1.5), alcohol use disorders (AOR=1.8), and use of multiple drugs (AOR=1.7).
Conclusions
Dependence on PPRs can occur without abuse, and subthreshold dependence deserves to be investigated further for consideration in major diagnostic classification systems.
Keywords: opioids, prescription drug abuse, prescription drug dependence, prescription pain medications
Surveys of the general population and of adolescents in particular have shown that the non-prescribed use of prescription pain relievers (PPRs) such as opioids has emerged as a major health issue in the United States.1,2 Hydrocodone products (e.g., Vicodin®, Lortab®, Lorcet®, Lorcet Plus®, and generic hydrocodone) are reported to be the most commonly used PPRs by new non-prescribed PPR users.3 The annual Monitoring the Future survey found that lifetime non-prescribed PPR use among 12th graders doubled from about 6% in the early 1990s to 13% in 2005.4 The National Survey of Drug Use and Health (NSDUH) estimated that, in 2006, 3.2 million adolescents aged 12–17 were lifetime non-prescribed users of psychotherapeutics, and 84% of these users had used PPRs.5 In 2006, there were an estimated 2.2 million first-time non-prescribed users of PPRs in the previous 12 months (i.e., past-year new users), a figure rivalling the 2.1 million new users of marijuana, the most commonly used drug in the United States.2 Adolescents aged 12–17 years represented more than one third (37%) of all past-year new non-prescribed PPR users.5
Indicators of PPR-related morbidity and mortality also have risen.6 Data from both the Drug Abuse Warning Network (DAWN) and the Treatment Episode Data Set (TEDS) reveal a significant upward trend in PPR-related admissions to emergency departments and publicly funded substance abuse treatment facilities.7,8 The rate of drug-overdose deaths associated with PPR misuse has increased and now exceeds the rate associated with use of heroin or cocaine.9 While these data are good indicators of PPR-related morbidity among treatment-seeking PPR misusers or polysubstance users, they do not provide adequate information concerning the problems resulting from non-prescribe PPR use among adolescents.
Among adolescents aged 12–17 who reported a history of non-prescribed PPR use, recent research has demonstrated that 52% had used hydrocodone products, 50% had used propoxyphene (Darvocet® or Darvon®) or codeine (Tylenol® with codeine), and 24% had used oxycodone products (Percocet®, Percodan®, Tylox®, or OxyContin®).10 In particular, girls tend to be more likely than boys to report use of non-prescribed PPRs in the past year,3 although there are no gender differences in this age group in the types of PPRs used and age of first non-prescribed use.10
Studies also have revealed that non-prescribed PPR use in adolescence is associated with substance use and health problems, a finding that warrants investigation because the magnitude of this problem is unknown. Data from the 2005 NSDUH showed that approximately three-quarters of lifetime adolescent users of non-prescribed PPRs report a history of using other drugs.10 Specifically, adolescent users of non-prescribed PPRs initiate non-prescribed PPR use at a mean age of 13.3 years, which is younger than the mean age of first use of almost all the other drugs, and occurs as early as the mean age of first use of alcohol (13.1 years) and marijuana (13.6 years).10 Compared with non-users, adolescent non-prescribed users have increased odds of using alcohol and other drugs, engaging in criminal behaviors (e.g., being arrested for criminal activities or engaging in selling illicit drugs in the past year), using health care (e.g., receiving treatment in the emergency department or as an inpatient), receiving treatment services for mental health problems, and reporting poorer health.10–13
However, despite the increased use of non-prescribed PPRs, there is limited information concerning adolescents who use PPRs without a prescription and who then meet the criteria for abuse or dependence as specified by the Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV,14 or who perceive symptoms of dependence but do not meet the criteria for a diagnosis (i.e., “subthreshold dependence”). The latter group is also termed “diagnostic orphans” and includes drug users who exhibit one or two criterion symptoms of dependence but do not meet criteria for abuse and dependence.15–17 Studies of alcohol 16,17 and marijuana users15 have suggested that diagnostic orphans are prevalent and tend to resemble those with abuse in substance use profile. However, we have not found any analogous study examining adolescent non-prescribed PPR users.
Further, a key item on the research agenda for the coming DSM-V is the categorical nature of substance diagnoses.18 The categorical classification in the current DSM-IV may miss substance users who experience substance use-related problems but do not meet the full criteria for a diagnosis. Such a subthreshold dependence condition may benefit from being included in the major diagnostic system given its prevalence and association with other substance abuse.15 Thus, findings from this investigation not only are likely to shed new light on the magnitude of diagnoses associated with non-prescribed PPR use, but may also provide timely estimates for diagnostic orphans of adolescent PPR users.
In this study, we use the newly released data from the 2006 NSDUH, augmented by data from the previous year, to study the nature and extent of diagnostic patterns and correlates of DSM-IV abuse, subthreshold dependence, and dependence on PPRs. Understanding the full extent of diagnostic patterns of PPR use is essential and timely, given increasing rates of non-prescribed PPR use, early onset of such use, and the dearth of research on DSM-IV diagnoses for adolescent PPR users.1–9 We address the following questions: What is the prevalence of abuse, subthreshold dependence, and dependence among past-year adolescent users of non-prescribed PPRs? What symptoms of abuse and dependence are commonly reported by adolescent users? Are diagnoses of non-prescribed PPR use associated with demographics, access to PPRs, physical health, and risk-related factors?
METHOD
Data Source
This study is based on data from the public use file of the 2005 and 2006 NSDUH.2,19 NSDUH is designed to provide estimates of substance use and related disorders for the U.S. general population. It utilizes multistage area probability sampling methods to select a representative sample of the U.S. civilian, noninstitutionalized population aged 12 years or older in all 50 states. Participants include household residents; residents of shelters, rooming or boarding houses, halfway houses, college dormitories, and group homes; and civilians residing on military bases. To improve the precision of drug use estimates for key subgroups, adolescents aged 12–17 years and young adults aged 18–25 years are oversampled.
Prospective NSDUH participants were assured that their names would not be recorded and that their responses would be kept strictly confidential. All study procedures and protections were carefully explained to them. For adolescents aged 12–17 years, the field interviewer first sought verbal consent from their parents or guardians. Once parental permission was granted, field interviewers then approached the adolescents and obtained their agreement to participate in the study. Parents were then asked to leave the interview setting to ensure the confidentiality of their children’s responses.
The interview utilizes computer-assisted interviewing (CAI) to increase the likelihood of valid respondent reports of drug use behaviors.20 CAI methodology combines computer-assisted personal interviewing and audio computer-assisted self-interviewing (ACASI). ACASI is designed to provide the respondent with a highly private and confidential means of responding to questions, and is used for questions of a sensitive nature (e.g., substance use). Respondents read questions on the computer screen or questions were read to respondents through headphones, and they entered their responses directly into a laptop computer provided by the interviewer.
A total of 68,308 and 67,802 respondents aged 12 years or older completed the interview in 2005 and 2006, respectively. Weighted response rates for household screening and interviewing in 2005 were 91.3% and 76.2%, respectively; the corresponding rates in 2006 were 90.6% and 74.2%, respectively. Each independent, cross-sectional NSDUH sample is considered representative of the U.S. general population aged 12 years or older. NSDUH designs are reported in detail elsewhere.19
Study Variables
Non-prescribed PPR use was defined as any self-reported use of prescription pain relievers that were not prescribed for the respondent, or that the respondent took only for the experience or feeling they caused.10,13 Respondents were read the following statement: "These questions are about PPR use. We are not interested in your use of ‘over-the-counter’ pain relievers such as aspirin, Tylenol®, or Advil® that can be bought in drug stores or grocery stores without a doctor’s prescription." Interviewers also showed a pill card to the respondents and read the following: “Card A shows pictures of some different kinds of PPRs and lists the names of some others. These pictures show only pills, but we are interested in your use of any form of PPRs that were not prescribed for you or that you took only for the experience or feeling they caused.”
The following 21 categories of PPRs were listed on Pill Card A: Darvocet®, Darvon®, or Tylenol® with codeine; Percocet®, Percodan®, or Tylox®; Vicodin®, Lortab®, Lorcet®, or Lorcet Plus®; codeine; Demerol®; Dilaudid®; Fioricet®; Fiorinal®; hydrocodone; methadone; morphine; OxyContin®; Phenaphen® with codeine; propoxyphene; SK-65®; Stadol®; Talacen®; Talwin®; Talwin NX®; tramadol; and Ultram®. A series of separate questions was presented to respondents to assess their use. For example, respondents were asked “Have you ever, even once, used Darvocet®, Darvon®, or Tylenol® with codeine that was not prescribed for you, or that you took only for the experience or feeling it caused?”
The survey also assessed respondents’ age at first non-prescribed use (i.e., onset) of any PPR and the number of days of using PPRs in the past 12 months. Number of days of using PPRs was originally categorized into four groups: 1–5 days (experimental use), 6–11 days (infrequent), 12–51 (approximately monthly), and 52 or more days (approximately weekly). However, due to unstable estimates in the logistic regression analysis caused by small cell sizes, and to the finding that only the category of use on 52 or more days was significantly associated with diagnostic categories of PPR use, we condensed the four categories into two groups: less than weekly versus weekly or more (i.e., use on ≥ 52 days). Use of multiple PPRs was defined by counting the number of the 21 categories of PPRs specified above that the respondents had ever used without a prescription.
Past-year abuse of and dependence on PPRs were specified by DSM-IV criteria.14 For each criterion of abuse and dependence, the survey explicitly specified “During the past 12 months, did using PPRs ….” The four abuse criteria were assessed by the following questions: (A1) During the past 12 months, did using PPRs cause you to have serious problems like this either at home, work, or school (e.g., neglecting their children, missing work or school, doing a poor job at work or school, losing a job or dropping out of school)? (A2) Did you regularly use PPRs and then do something where using PPRs might have put you in physical danger? (A3) Did using PPRs cause you to do things that repeatedly got you in trouble with the law? (A4) Did you have any problems with family or friends that were probably caused by your use of PPRs? Did you continue to use PPRs even though you thought this caused problems with family or friends?
Likewise, the seven dependence criteria were assessed by the following questions: (D1) During the past 12 months, did you need to use more PPRs than you used to in order to get the effect you wanted? Did you notice that using the same amount of PPRs had less effect on you than it used to? (D2) Did you have three or more of symptoms after you cut back or stopped using PPRs (e.g., feeling kind of blue or down; vomiting or feeling nauseous; having cramps or muscle aches; having teary eyes or a runny nose; feeling sweaty, having enlarged eye pupils, or having body hair standing up on your skin; having diarrhea; yawning; having a fever; or having trouble sleeping)? Did you have 3 or more of these symptoms at the same time that lasted for longer than a day after you cut back or stopped using PPRs? (D3) Did you try to set limits on how often or how much PPRs you would use? Were you able to keep to the limits you set, or did you often use PPRs more than you intended to? (D4) Did you want to or try to cut down or stop using PPRs? Were you able to cut down or stop using PPRs every time you wanted to or tried to? (D5) Was there a month or more when you spent a lot of your time getting or using PPRs? Was there a month or more when you spent a lot of your time getting over the effects of the PPRs you used? (D6) Did using PPRs cause you to give up or spend less time doing important activities such as working, going to school, taking care of children, doing fun things such as hobbies and sports, and spending time with friends and family? (D7) Did you have any problems with your emotions, nerves, or mental health that were probably caused or made worse by your use of PPRs? Did you continue to use PPRs even you thought that this was causing you to have problems with your emotions, nerves, or mental health? Did you have any physical health problems that were probably caused or made worse by your use of PPRs? Did you continue to use PPRs even you thought that this was causing you to have physical problems?
Consistent with the DSM-IV,14 respondents who met at least one abuse criterion but did not meet criteria for dependence in the past year were classified as exhibiting PPR abuse, while dependence included respondents who met criteria for at least three dependence symptoms in the past year, regardless of abuse. Subthreshold dependence included respondents who met 1–2 dependence criteria but did not manifest abuse.
Demographic variables examined included respondents’ age, sex, race/ethnicity, and school status.10,13 Factors related to access to PPRs included annual family income and health insurance status. For adolescents who were unable to respond to income and insurance questions, proxy responses were accepted from a household member who was better able to give the correct information.
Based on previous findings of non-prescribed PPR use,10–13 we examined alcohol use disorders (AUDs), use of multiple drugs, criminal activities, perceived health status, health care use, and mental health-related variables as potential correlates of PPR use disorders. Past-year AUDs (abuse or dependence) was also assessed per DSM-IV criteria.2,14 Use of multiple drugs was estimated by summing the number of eight drug classes (inhalants, marijuana, cocaine/crack, heroin, hallucinogens, and non-prescribed use of prescription sedatives, tranquilizers, and stimulants) that respondents used in the past year. Use of these drugs was assessed by eight separate subsections, within each of which the survey explicitly listed the names of drugs belonging to each drug class.
Past-year criminal activity was defined as adolescents’ self-reported past-year experiences of arrests or bookings for breaking the law, not counting minor traffic violations.21 Past-year illicit drug selling was defined as having sold illicit drugs in the past 12 months.13 Adolescents’ perceived overall health was dichotomized (excellent/good vs. fair/poor). Past-year emergency department (ED) visits were defined as treatment in an ED during the past 12 months.10 Past-year inpatient hospitalization was defined as self-reported inpatient hospitalization (staying overnight or longer in a hospital) during the past 12 months.10 Past-year use of mental health treatment services was defined as any use of treatment or counseling at any service location in the prior year for emotional or behavioral problems that were not caused by alcohol or drug use (e.g., hospital, residential treatment facility, day treatment facility, mental health clinic, family doctor, and school counselor).10,22
Assessments of major depressive episodes (MDEs) were based on DSM-IV criteria and adapted from the National Comorbidity Survey-Adolescents.2 The NSDUH assessed nine criterion symptoms of MDEs: depressed mood most of the day, markedly diminished interest or pleasure in all or almost all activities most of the day, changes in appetite or weight, sleep problems, psychomotor agitation or retardation, fatigue or loss of energy, feelings of worthlessness, diminished ability to concentrate or make decisions, and thoughts or plans for suicide. Adolescents who had ≥ 5 criterion symptoms were classified as having a lifetime MDE, and those who also reported that they had a period of depression lasting two weeks or longer while also having some of the symptoms mentioned during the past 12 months were classified as having a past-year MDE. In NSDUH, no exclusions were made for MDE caused by medical illness, bereavement, or substance use disorders.
Data Analysis
We first examined demographic distributions and prevalence rates of use, abuse, and dependence on PPRs among all respondents. We found no significant variations in each of these characteristics across the two survey years. We then combined the data from the two survey years (N = 36,992). Among the combined subsample of past-year non-prescribed PPR users (n = 2,675), we determined the prevalence of abuse, subthreshold dependence, and dependence, as well as their relation with patterns of PPR use. We then examined the pattern of symptoms of abuse and dependence. Bivariate associations were examined with χ2 tests for categorical variables and with t tests for continuous variables. Finally, we conducted multinomial logistic regression analyses to identify characteristics associated with respondents’ category of diagnoses. Due to the complex design of the survey, all analyses were conducted with the SUDAAN software.23 All results reported here are weighted estimates; only sample sizes are unweighted.
RESULTS
Demographics
A total of 18,678 and 18,314 adolescents aged 12–17 years were identified from the public use data file of 2005 and 2006 NSDUH, respectively. There were no significant yearly variations in the demographics examined (Table 1).
TABLE 1.
Selected Demographic Characteristics of the study sample and the Prevalence of Past-Year Non-prescribed Use of Prescription Pain relievers among the Total Adolescent Sample Aged 12–17 Years (N = 36,992)
| Characteristics, % | Total study sample | Past-year prevalence of non-prescribed use |
|---|---|---|
| % (N) | % (SE) | |
| Overall | 100 (36,992) | 7.0 (0.17) |
| Sex | ||
| Male | 51.1 (18,780) | 6.5 (0.24)* |
| Female | 48.9 (18,212) | 7.5 (0.25) |
| Age group in years | ||
| 12–13 | 32.0 (11,865) | 3.4 (0.26)* |
| 14–15 | 34.6 (12,682) | 6.3 (0.23) |
| 16–17 | 33.5 (12,445) | 11.2 (0.36) |
| Race/ethnicity | ||
| White | 60.4 (2,2701) | 7.7 (0.18)* |
| African American | 15.3 (5,172) | 5.9 (0.44) |
| American Indian/Alaska Native | 0.6 (534) | 9.8 (1.57) |
| Asian/Native Hawaiian | 4.6 (1,223) | 4.3 (0.72) |
| Multiple race | 1.5 (1,320) | 10.8 (1.53) |
| Hispanic | 17.6 (6,042) | 5.9 (0.53) |
| Student status | ||
| Yes | 98.6 (36,396) | 6.8 (0.17)* |
| No | 1.5 (596) | 18.9 (2.35) |
| Family income | ||
| $0–$19,999 | 17.4 (6,500) | 7.8 (0.43) |
| $20,000–$39,999 | 22.1 (8,528) | 7.1 (0.38) |
| $40,000–$74,999 | 29.4 (11,381) | 7.3 (0.25) |
| $75,000 or more | 31.2 (10,583) | 6.2 (0.29) |
| Health insurance coverage | ||
| Yes | 91.4 (34,366) | 7.0 (0.19) |
| No | 8.6 (2,626) | 6.8 (0.57) |
| Survey | ||
| 2005 | 50.0 (18,678) | 6.9 (0.23) |
| 2006 | 50.0 (18,314) | 7.1 (0.23) |
SE: standard error.
χ2 tests with variables in the first column, two-tailed: p-values < .010.
Use, Abuse, and Dependence among All Adolescents
Of the combined sample (N = 36,992), 7% (n = 2,675) reported non-prescribed PPR use in the past year. As shown in Table 1, use of non-prescribed PPRs was associated with sex, age group, race/ethnicity, and student status (χ2 test, p < .010). A comparatively high prevalence of non-prescribed PPR use was observed among females (8%), adolescents aged 16–17 (11%), whites (8%), adolescents of multiple race (11%), and non-students (19%). Prevalence rates of use of each category of PPRs from the NSDUH are reported elsewhere.10
There was no significant yearly variation in the prevalence of past-year PPR abuse or dependence (data not shown). Approximately 1.1% (n = 400) of all adolescents met criteria for past-year PPR abuse (0.5%) or dependence (0.6%).
Abuse, Subthreshold Dependence, and Dependence among Users
Overall, more than one-third (35%, n = 911) of all non-prescribed users reported one or more symptoms of abuse or dependence: abuse, 6.7%; subthreshold dependence, 19.6%; and dependence regardless of abuse, 9.1%.
As shown in Table 2, respondents with dependence reported on average more cumulative days of non-prescribed PPR use (86.7 days) than did those with abuse (55.6 days) or subthreshold dependence (39.6 days) (t test, p < .05). They on average also reported more categories of PPRs used (3.9 categories) than the abuse (2.7 categories) and subthreshold dependence (2.1 categories) groups (t test, p < .05). There were no significant differences in these characteristics between the abuse and the subthreshold groups.
TABLE 2.
Prevalence of Abuse of and Dependence on Prescription Pain relievers among Non-prescribed Users of Prescription Pain relievers Aged 12–17 Years (N = 2,675)
| Past-year diagnostic status | Weighted prevalence | Age of first use of non-prescribed pain relievers | Number of days of using pain relievers in the past year | Categories of pain relievers ever used |
|---|---|---|---|---|
| % | Mean | Mean | Mean | |
| (n) | (95% CI) | (95% CI) | (95% CI) | |
| Overall | 100 | 13.5 | 38.2 | 2.0 |
| (2,675) | (13.33–13.62) | (35.11–41.23) | (1.94–2.13) | |
| Use without DSM-IV symptom | 64.7 | 13.6 | 29.0 | 1.7 |
| (1,764) | (13.44–13.76) | (25.55–32.49) | (1.59–1.75) | |
| Abuse | 6.7 | 13.1a | 55.6b | 2.7b |
| (186) | (12.74–13.43) | (39.50–71.75) | (2.15–3.26) | |
| Subthreshold dependence | 19.6 | 13.3 | 39.6b | 2.1b |
| (511) | (12.98–13.65) | (33.04–46.07) | (1.91–2.37) | |
| Dependence regardless of abuse | 9.0 | 13.3 | 86.7c | 3.9c |
| (214) | (12.75–13.76) | (73.45–101.89) | (3.49–4.32) | |
CI = confidence interval.
Bold: Significant differences between diagnostic groups by t-tests, two-tailed, p < .05.
Abuse < Use without DSM-IV symptom.
Abuse, Subthreshold dependence > Use without DSM-IV symptom.
Dependence regardless of abuse > Use without DSM-IV symptom, Abuse, Subthreshold dependence.
Symptoms of Abuse and Dependence among Users
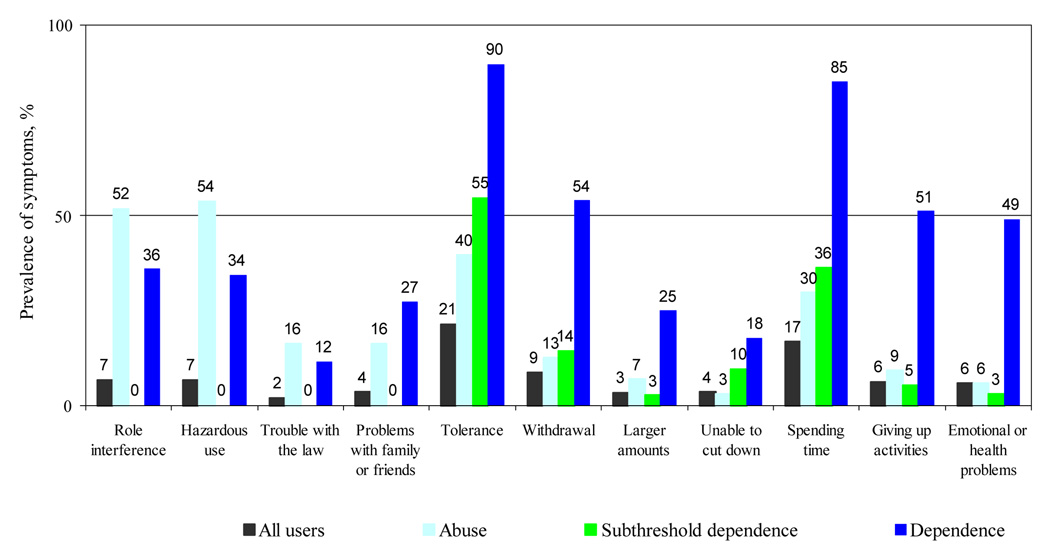
As shown in Fig. 1, irrespective of diagnostic category, “tolerance” (using the same amount of PPRs with decreasing effects) and “salience” (spending a lot of time using or getting over the effects of PPRs) constituted the most commonly presented symptoms of dependence by users. Both were prevalent in the dependence group (90% and 85%, respectively). “Withdrawal (54%),” “giving up activities (51%),” and “continued use despite having physical/psychological problems (49%)” also were common in the dependence group.
Figure 1.
Prevalence of past-year symptoms of abuse and dependence on prescription pain relievers among past-year non-prescribed users of prescription pain relievers aged 12–17 years: by diagnostic categories (N = 2,675)
Of all abuse symptoms, “hazardous use” and “role interference” were most frequently endorsed by the abuse group (54% and 52%, respectively) and the dependence group (34% and 36%, respectively). More than one-fourth of adolescents with dependence also reported “problems with family or friends” (27%).
It should be noted that 66% (4.4% out of 6.7%) of adolescents in the abuse group also reported symptoms of subthreshold dependence (one or two dependence symptoms) and that 58% (5.3% out of 9.1%) of adolescents in the dependence group also reported symptoms of abuse.
Correlates of Abuse, Subthreshold Dependence, and Dependence
Table 3 summarizes results from multinomial logistic regression of correlates of abuse (without a dependence diagnosis), subthreshold dependence (without abuse), and dependence (irrespective of any abuse). The odds of being in each category of diagnoses were each compared to users without any criterion symptom. Family income, health insurance, inpatient treatment, criminal activities, and age of first non-prescribed PPR use were unassociated with each diagnostic category and were thus excluded from the adjusted model.
TABLE 3.
Adjusted Odds Ratios (AOR) and 95% Confidence Intervals (95% CI) of Abuse of or Dependence on Prescription Pain relievers among Past-year Non-prescribed Users of Prescription Pain relievers Aged 12–17 Years (N = 2,675)
| AOR and 95% CIa | Abuseb | Subthreshold dependenceb |
Dependence regardless of abuseb |
|---|---|---|---|
| Sex (vs. male) | |||
| Female | 0.85 (0.49–1.48) | 1.02 (0.77–1.34) | 1.60 (1.08–2.39) |
| Age group (vs. 16–17 years) | |||
| 12–13 | 2.30 (1.31–4.02) | 1.44 (0.92–2.24) | 0.99 (0.52–1.86) |
| 14–15 | 2.20 (1.36–3.58) | 0.98 (0.74–1.29) | 1.20 (0.76–1.91) |
| Race/ethnicity (vs. white) | |||
| Hispanic | 1.04 (0.47–2.28) | 0.70 (0.45–1.09) | 0.98 (0.56–1.71) |
| African American | 1.53 (0.78–3.00) | 1.88 (1.25–2.83) | 1.37 (0.70–2.67) |
| American Indian/Alaska Native/Multiple race | 1.40 (0.59–3.32) | 1.26 (0.78–2.02) | 1.23 (0.52–2.93) |
| Asian/Native Hawaiian | 1.18 (0.21–6.82) | 2.54 (1.02–6.33) | 0.13 (0.05–0.34) |
| Student status (vs. students) | |||
| Non-students | 2.62 (1.27–5.39) | 1.02 (0.48–2.17) | 0.52 (0.22–1.25) |
| Number of days of using pain relievers (vs. less than weekly) | |||
| ≥ Weekly | 1.72 (1.00–2.94) | 1.39 (1.02–1.88) | 5.45 (3.97–7.49) |
| Perceived overall health(vs. excellent/good) | |||
| Fair/poor | 2.37 (1.28–4.37) | 0.95 (0.51–1.76) | 1.44 (0.68–3.05) |
| Emergency depart. treatment (vs. no) | |||
| Yes | 1.91 (1.18–3.08) | 1.36 (1.01–1.83) | 1.46 (0.99–2.16)† |
| Mental health service use (vs. no) | |||
| Yes | 1.78 (1.20–2.62) | 0.74 (0.51–1.06) | 1.42 (0.91–2.22) |
| Major depressive episodes (vs. no) | |||
| Episode in the last year | 1.31 (0.73–2.33) | 1.46 (1.01–2.11) | 1.77 (1.04–3.01) |
| Prior to last year | 2.42 (1.16–5.06) | 1.90 (1.10–3.27) | 1.45 (0.74–2.87) |
| Sold illicit drugs (vs. no) | |||
| Yes | 1.66 (0.94–2.95) | 1.07 (0.77–1.49) | 1.74 (1.13–2.69) |
| Alcohol use disorder (vs. no) | |||
| Yes | 3.44 (2.23–5.30) | 1.81 (1.28–2.56) | 2.12 (1.31–3.43) |
| Number of the other 8 drug classes used, not counting pain relievers (vs. none) | |||
| One | 0.83 (0.45–1.53) | 0.87 (0.61–1.24) | 1.21 (0.58–2.51) |
| Two | 0.74 (0.43–1.28) | 1.03 (0.71–1.51) | 1.81 (0.82–3.97) |
| Three or more | 1.29 (0.64–2.57) | 1.73 (1.10–2.71) | 2.90 (1.43–5.89) |
The adjusted logistic regression model included variables listed in the first column. Total family income, health insurance status, inpatient treatment, past-year arrests for criminal activities, and age at onset of non-prescribed PPR use were tested, but they not significant and were not included in the adjusted model.
The comparison group included non-prescribed PPR users who did not report any criterion symptom of abuse and dependence.
Bold: p ≤ .05.
p = 0.059.
Weekly non-prescribed PPR use (AOR = 1.4 to 5.5), MDEs (AOR = 1.5 to 2.4), and past-year AUDs (AOR = 1.8 to 3.4) were all associated with each diagnostic category. The association with weekly non-prescribed PPR use was significantly stronger in the dependence group (AOR = 5.5) than in the other groups (AOR = 1.4 to 1.7). Additionally, past-year MDEs were associated with the two dependence groups (AOR = 1.5 to 1.8). Former MDEs (AOR = 1.9 to 2.4) and pastyear ED visits (AOR = 1.4 to 1.9) were associated with abuse and with subthreshold dependence.
Several characteristics were associated with the abuse group only, including being age 12–15 (AOR = 2.2 to 2.3), non-student status (AOR = 2.6), self-reported fair or poor health (AOR = 2.4), and use of mental health services for psychological problems (AOR = 1.8). For example, relative to non-users, past-year users of mental health services were 1.8 times more likely to be classified in the abuse group. On the other hand, African Americans (AOR = 1.9) and Asians/Native Hawaiians (AOR = 2.5) had increased odds of being in the subthreshold dependence group, whereas Asians/Native Hawaiians (AOR = 0.1) had reduced odds of being in the dependence group. Females (AOR = 1.6) and those who sold illicit drugs in the past year (AOR = 1.7) had increased odds of being in the dependence group. Finally, past-year use of three or more drug classes was a significant correlate of the two dependence groups only (AOR = 1.7, subthreshold dependence; AOR = 2.9, dependence).
DISCUSSION
Among this representative national sample of adolescents aged 12–17 years, about 7% reported PPR use without a prescription in the previous 12 months, and approximately 1% met criteria for past-year PPR abuse or dependence. Among the subset of past-year non-prescribed users, we found that 16% of users met criteria for abuse (7%) or dependence (9%), and an additional 20% exhibited subthreshold dependence. Individuals in the latter group have typically not been recognized (“diagnostic orphans”). Thus, if we had relied exclusively on the formal DSM-IV classification, we would have overlooked one-fifth of past-year non-prescribed PPR users who reported symptoms of dependence.
The most salient finding of this study is the high prevalence of clinical features of abuse or dependence among adolescent users of non-prescribed PPRs: more than one in three users reported one or more DSM-IV criterion symptoms, and close to one in six met criteria for abuse or dependence. This observation is in agreement with the pattern of non-prescribed PPR use reported by all users in this sample: they reported, on average, using PPRs for 38 days in the past year and using two categories of PPRs. This finding is also is consistent with recent studies that have revealed substantially increased rates of PPR-related admissions to emergency departments and publicly funded substance abuse treatment facilities.6–8,24
However, the lack of research on PPR use disorders among adolescents has constrained our ability to compare our findings with those of others. We have found one study that reported the prevalence of PPR abuse and dependence among youth. In their sample of youth aged 14–24 in Germany,25 investigators reported that about 8% of lifetime non-prescribed PPR users (N = 114) met criteria for DSM-IV PPR abuse (4.3%) or dependence (3.5%) and an additional 21% met criteria for subthreshold dependence. Although past-year PPR abuse and dependence was not reported by Perkonigg et al.,25 our findings clearly show that use of non-prescribed PPRs among domicile American adolescents is noteworthy and deserves further research and attention.
Results from this study also suggest that the DSM-IV classification may be insufficient to capture the heterogeneity of symptoms presented by adolescent PPR users. Although the DSM-IV,14 defines a hierarchical distinction between abuse and dependence and implies that abuse occurs before dependence, we found a much higher prevalence of dependence than abuse symptoms. All adolescents with subthreshold dependence (20% of non-prescribed users), as well as 42% of those with a dependence diagnosis (3.8% of non-prescribed users), reported no abuse symptom, as compared to 12% of non-prescribed users who reported at least one abuse symptom (i.e., 6.7% with an abuse diagnosis and 5.3% with a dependence diagnosis plus concomitant abuse symptoms). Considering the young age of this sample, our findings support the conclusion that dependence can occur in the absence of abuse, and that an exclusive reliance on the presence of abuse symptoms as a screener to identify cases of dependence is likely to miss cases where dependent individuals report no abuse symptoms.26
Consistent with the study of dependence symptoms from non-prescribed PPR use,27 we found that “tolerance” and “salience” were the most common symptoms experienced by users. Our results revealed further that both symptoms were endorsed by the great majority of the dependence group, and that “role interference” and “hazardous use” were cited as the most frequently exhibited symptoms of abuse. The latter two abuse symptoms were each reported by more than one-third of the dependence group and by more than one-half of the abuse group. Overall, adolescents classified as having dependence suffered the most clinical features from PPR use, including symptoms of physiological dependence (tolerance and withdrawal), compulsive PPR use behaviors (spending a great deal of using PPRs, giving up important activities, and continued use despite having psychological or physical problems), as well as consequences from PPR use (role interference and use in hazardous conditions). This higher rate of symptoms in the dependence group is likely related to the greater numbers of days that these adolescents reported using PPRs, as well as additional types of PPRs used.
Results from this study further suggest that a subgroup of vulnerable adolescents with depression or alcohol problems are at risk for using non-prescribed PPRs regularly, and that the odds of escalating to a diagnosis are closely associated with additional days of PPR use. We found that having MDEs or AUDs each increased adolescents’ odds of being classified in all three diagnostic categories. Past-year ED treatment also increased odds of PPR abuse and subthreshold dependence, and was marginally associated with dependence (AOR = 1.5, p =0.059). Because “relieving pain” is much more likely than “getting high” to be endorsed by adolescent users of non-prescribed PPRs as the primary reason for their use,11 it seems likely that PPRs are taken to reduce the discomfort associated with physical or mental health problems,28 and that the risk of developing abuse or dependence may be exacerbated by existing physical and mental health conditions.
Compared with PPR users who reported no DSM-IV symptoms, abusers were generally younger, likely to be non-students, had already received services for psychological problems, reported fair/poor health, and had a history of MDEs. Because the abuse group was unassociated with engagement in criminal activities and use of multiple drugs, it seems likely that they had suffered internalizing problems and might have used PPRs for self-medication to alleviate mental health-related conditions.28 Given the young age of this group, longitudinal studies are needed to determine whether the subset of young abusers progresses to dependence as suggested by the DSM-IV (i.e., abuse occurs before dependence).
In contrast, adolescents categorized as dependent, as compared to PPR users who reported no DSM-IV symptoms, were likely to report past-year MDEs, to sell illicit drugs, and to use multiple drugs in the past year, suggesting co-occurrences of internalizing and externalizing problems. In this group, PPR use may be a manifestation of self-medication for mental health problems,28 delinquency, and polydrug use.29
Further, dependence on PPRs among girls deserves attention. Girls are more likely than boys to report a history of both prescribed (37% vs. 23%) and non-prescribed (22% vs. 10%) PPR use.11 They also are more likely than boys to give or loan their PPRs to others (e.g., female friends),30 but appear less likely to use them for getting high.31 Given that prescribed PPR use is associated with non-prescribed use and that girls may take PPRs to alleviate menstrual cramps,11 girls’ risk for dependence may be related to their greater access to PPRs11 and to their need to self-medicate to reduce discomfort or psychological distress. Additionally, non-prescribed PPR users typically obtain their PPRs from peers.32 Affiliation with PPR-using friends may thus pose a risk for non-prescribed use.
Lastly, the subthreshold dependence group is also characterized by past-year ED treatment, AUDs, use of multiple drugs, and MDEs. This group differs from the dependence group in a lack of association with delinquency variables examined. However, this group appears to be represented by African Americans and Asians/Native Hawaiians. Given its high prevalence, an exclusive use of the DSM-IV to find cases in need of clinical attention or research will likely miss minority adolescents who perceived adverse effects from PPR use.
Taken together, adolescents in the dependence group use more PPRs and exhibit more DSM-IV symptoms than adolescents in the other groups. They also appear to be more likely than abusers to use multiple drugs, be involved in criminal activities, and experience MDEs recently. In this regard, dependence tends to be more severe than abuse as indicated by the DSM-IV.14 Additionally, subthreshold dependence (20%) is more common than the combined prevalence for abuse and dependence (16%), and this group resembles the dependence group in past-year MDEs, AUDs, and use of multiple drugs. Given the young age of this sample, prospective studies are needed to study the course and treatment needs of adolescents with subthreshold dependence. Adding a symptom count in addition to relying on the DSM’s formal classification criteria may help identify “diagnostic orphans of drug users” who otherwise could be missed by clinicians or researchers.
These findings should be interpreted within the context of the following limitations. First, due to the cross-sectional nature of the survey, no causal pathways among the variables examined can be inferred. Self-reports on which this study relies are influenced by various biases, including memory errors and under-reporting due to social desirability biases. In addition, a small (less than 2%) subgroup of adolescents, including incarcerated, institutionalized, and homeless adolescents, was not included in the NSDUH. These findings do not apply to them. Further, while the diagnoses of abuse and dependence were assessed by standardized questions administered by trained interviewers, they were not validated by clinicians.
Moreover, non-prescribed PPR use is defined broadly.10, 33 This definition may have led to the inclusion of users who had a legitimate medical condition but lacked a prescription for various reasons.10,33 The wording of the survey questions might have served to include PPR users who received medication from friends or family members to alleviate their health-related conditions.10, 33 Nevertheless, our findings are generally in agreement with research on students indicating an association of substance use with non-prescribed PPR use.11 Last, although the NSDUH explicitly listed more categories of PPRs used than the other population-based surveys,4,26 it should be noted that the 21 categories of PPRs specified in the survey are not entirely inclusive. There are a few PPRs that are not listed by the survey.
In conclusion, more than one-third of adolescent users of non-prescribed PPRs report DSM-IV symptoms of abuse or dependence. Unsupervised use of prescription PPRs places users at risk for adverse interactions with other central nervous system depressants, for overdose, and for addiction.9,34,35 Considering that family members and friends constitute sources of PPRs for adolescents,30 issues concerning the health risk of unsupervised use of prescription PPRs should be included in adolescent drug prevention education efforts among families and in the community.
Acknowledgments
This work was supported by research grants from the U.S. National Institute on Drug Abuse of the National Institutes of Health to Li-Tzy Wu (DA019901 and DA019623). The Substance Abuse and Mental Health Data Archive and the Inter-university Consortium for Political and Social Research provided the public use data files for NSDUH, which was sponsored by SAMHSA’s Office of Applied Studies. The opinions expressed in this paper are solely those of the authors and not of any sponsoring agency. The authors thank Amanda McMillan for proofreading the manuscript.
Footnotes
Disclosure Dr. Patkar has received grant support from Pfizer, Forest Laboratories, Cephalon, and Titan Pharmaceuticals and is on the speaker’s bureaus of Cephalon and Reckitt-Benckiser. Dr. Mannelli has received research funding from AstraZeneca, Bristol-Myers Squibb, Forest, GlaxoSmithKline, Janssen, McNeil Consumer and Specialty, Organon, Orphan Medical, Pfizer, Reckitt Benckiser, and Jazz Pharmaceuticals. The other authors report no conflicts of interest.
REFERENCES
- 1.Compton WM, Volkow ND. Abuse of prescription drugs and the risk of addiction. Drug Alcohol Depend. 2006;83 suppl 1:S4–S7. doi: 10.1016/j.drugalcdep.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 2.Office of Applied Studies. Rockville, MD: Substance Abuse and Mental Health Services Administration; Results from the 2006 National Survey on Drug Use and Health: National Findings. 2007 (DHHS Publication No. SMA 07-4293, NSDUH Series H-32)
- 3.Office of Applied Studies. Rockville, MD: Substance Abuse and Mental Health Services Administration; The NSDUH Report: Patterns and Trends in Nonmedical Prescription Pain Reliever Use: 2002 to 2005. 2007
- 4.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Bethesda, MD: National Institute on Drug Abuse; Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings, 2005. 2006 (NIH Publication No. 06-5882)
- 5.Office of Applied Studies. [Accessed February 5, 2008];Rockville, MD: Substance Abuse and Mental Health Services Administration; 2006 National Survey on Drug Use & Health: Detailed Tables. 2007b Available at: http://www.oas.samhsa.gov/NSDUH/2k6NSDUH/tabs/Sect4peTabs1to16.htm#Tab4.1B.
- 6.Zacny J, Bigelow G, Compton P, Foley K, Iguchi M, Sannerud C. College on Problems of Drug Dependence taskforce on prescription opioid nonmedical use and abuse: position statement. Drug Alcohol Depend. 2003;69:215–232. doi: 10.1016/s0376-8716(03)00003-6. [DOI] [PubMed] [Google Scholar]
- 7.Gilson AM, Ryan KM, Joranson DE, Dahl JL. A reassessment of trends in the medical use and abuse of opioid analgesics and implications for diversion control: 1997–2002. J Pain Symptom Manage. 2004;28:176–188. doi: 10.1016/j.jpainsymman.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 8.Office of Applied Studies. [Accessed March 15, 2007];Rockville, MD: Office of Applied Studies, Substance Abuse and Mental Health Services Administration; The DASIS Report: Treatment Admissions Involving Narcotic Painkillers, 2002 Update. 2004 Available at: http://www.oas.samhsa.gov/2k4/PainTX/PainTX.htm.
- 9.Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006;15:618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- 10.Wu LT, Pilowsky DJ, Patkar AA. Non-prescribed use of pain relievers among adolescents in the United States. Drug Alcohol Depend. 2008;94:1–11. doi: 10.1016/j.drugalcdep.2007.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boyd CJ, Esteban McCabe S, Teter CJ. Medical and nonmedical use of prescription pain medication by youth in a Detroit-area public school district. Drug Alcohol Depend. 2006;81:37–45. doi: 10.1016/j.drugalcdep.2005.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCabe SE, Boyd CJ, Young A. Medical and nonmedical use of prescription drugs among secondary school students. J Adolesc Health. 2007a;40:76–83. doi: 10.1016/j.jadohealth.2006.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sung HE, Richter L, Vaughan R, Johnson PB, Thom B. Nonmedical use of prescription opioids among teenagers in the United States: trends and correlates. J Adolesc Health. 2005;37:44–51. doi: 10.1016/j.jadohealth.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 14.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed., text rev. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 15.Degenhardt L, Lynskey M, Coffey C, Patton G. 'Diagnostic orphans' among young adult cannabis users: persons who report dependence symptoms but do not meet diagnostic criteria. Drug Alcohol Depend. 2002;67:205–212. doi: 10.1016/s0376-8716(02)00064-9. [DOI] [PubMed] [Google Scholar]
- 16.Sarr M, Bucholz K, Phelps D. Using cluster analysis of alcohol use disorders to investigate ‘diagnostic orphans’: subjects with alcohol dependence symptoms but no diagnosis. Drug Alcohol Depend. 2000;60:295–302. doi: 10.1016/s0376-8716(00)00118-6. [DOI] [PubMed] [Google Scholar]
- 17.Pollock NK, Martin CS. Diagnostic orphans: adolescent with alcohol symptoms who do not qualify for DSM-IV abuse or dependence diagnoses. Am J Psychiatry. 1999;156:897–901. doi: 10.1176/ajp.156.6.897. [DOI] [PubMed] [Google Scholar]
- 18.Helzer JE, van den Brink W, Guth SE. Should there be both categorical and dimensional criteria for the substance use disorders in DSM-V? Addiction. 2006 Sep;101 Suppl 1:17–22. doi: 10.1111/j.1360-0443.2006.01587.x. Review. [DOI] [PubMed] [Google Scholar]
- 19.Office of Applied Studies. [Accessed March 15, 2007];Rockville, MD: Office of Applied Studies, Substance Abuse and Mental Health Services; Results from the 2005 National Survey on Drug Use and Health: National Findings. 2006 Available at: http://www.oas.samhsa.gov/nsduh/2k5nsduh/2k5results.pdf.
- 20.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280:867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- 21.Wu LT, Schlenger WE, Galvin DM. Concurrent use of methamphetamine, MDMA, LSD, ketamine, GHB, and flunitrazepam among American youths. Drug Alcohol Depend. 2006;84:102–113. doi: 10.1016/j.drugalcdep.2006.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu LT, Pilowsky DJ, Schlenger WE. Inhalant abuse and dependence among adolescents in the United States. J Am Acad Child Adolesc Psychiatry. 2004;43:1206–1214. doi: 10.1097/01.chi.0000134491.42807.a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Research Triangle Institute. SUDAAN User’s Manual, Release 9.0. Research Triangle Park, NC: Research Triangle Institute; 2006. [Google Scholar]
- 24.Peindl KS, Mannelli P, Wu LT, Patkar AA. Trends in nonheroin opioid abuse admissions: 1992–2004. J Opioid Manag. 2007;3:215–223. doi: 10.5055/jom.2007.0007. [DOI] [PubMed] [Google Scholar]
- 25.Perkonigg A, Lieb R, Wittchen HU. Prevalence of use, abuse and dependence of illicit drugs among adolescents and young adults in a community sample. Eur Addict Res. 1998;4:58–66. doi: 10.1159/000018923. [DOI] [PubMed] [Google Scholar]
- 26.Hasin DS, Hatzenbueler M, Smith S, Grant BF. Co-occurring DSM-IV drug abuse in DSM-IV drug dependence: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2005;80:117–123. doi: 10.1016/j.drugalcdep.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 27.Martins SS, Ghandour LA, Chilcoat HD. Profile of dependence symptoms among extramedical opioid analgesic users. Addict Behav. 2007;32:2003–2019. doi: 10.1016/j.addbeh.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 28.Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv Rev Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- 29.Jessor R. Risk behavior in adolescence: a psychosocial framework for understanding and action. J Adolesc Health. 1991;12:597–605. doi: 10.1016/1054-139x(91)90007-k. [DOI] [PubMed] [Google Scholar]
- 30.Boyd CJ, McCabe SE, Cranford JA, Young A. Prescription drug abuse and diversion among adolescents in a southeast Michigan school district. Arch Pediatr Adolesc Med. 2007;161:276–281. doi: 10.1001/archpedi.161.3.276. [DOI] [PubMed] [Google Scholar]
- 31.McCabe SE, Cranford JA, Boyd CJ, Teter CJ. Motives, diversion, and routes of administration associated with nonmedical use of prescription opioids. Addict Behav. 2007b;32:562–575. doi: 10.1016/j.addbeh.2006.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McCabe SE, Boyd CJ. Sources of prescription drugs for illicit use. Addict Behav. 2005;30:1342–1350. doi: 10.1016/j.addbeh.2005.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Colliver JD, Kroutil LA, Dai L, Gfroerer JC. Rockville, MD: Office of Applied Studies, Substance Abuse and Mental Health Services Administration; Misuse of Prescription Drugs: Data from the 2002, 2003, and 2004 National Surveys on Drug Use and Health. 2006
- 34.National Institute on Drug Abuse. [Accessed August 10, 2007];Washington, DC: National Institute on Drug Abuse, the National Institutes of Health, U.S. Department of Health and Human Services; Prescription Pain and Other Medications. 2006 Available at: http://www.drugabuse.gov/infofacts/PainMed.html.
- 35.Schulteis G, Koob GF. Reinforcement processes in opiate addiction: a homeostatic model. Neurochem Res. 1996;21:1437–1454. doi: 10.1007/BF02532385. [DOI] [PubMed] [Google Scholar]