ABSTRACT
Objective: To study the long-term outcome of endonasal endoscopic skull base reconstruction with nasal turbinate tissue free graft. Patients and Methods: This study included 55 consecutive patients who underwent endonasal endoscopic skull base reconstruction with nasal turbinate graft and were available for follow-up. They were 30 patients with pituitary adenomas, 20 with cerebrospinal fluid (CSF) rhinorrhea of different etiologies, three with meningoencephalocele, and two with skull base meningiomas. Autologous nasal turbinate tissue materials were used in reconstructing the skull base defect. Clinical follow-up with endoscopic nasal examination was done routinely 1, 3, 6, and 12 months after surgery. Computed tomography and magnetic resonance imaging were performed when indicated. The follow-up period ranged from 6 months to 8 years. Results: There were no major operative or postoperative complications. Nasal turbinate graft was effective in sealing of intraoperative CSF leak, obliteration of dead space, and anatomic reconstruction of the skull base. There was no evidence of graft migration or inflammatory changes. Starting from 3 months after surgery to the rest of the follow-up period, endonasal endoscopic view of the site of duraplasty showed that: with small skull base defect (less than 5 mm), there was neither dural pulsation nor prolapse; with moderate-sized defect (5 to 10 mm), there was dural pulsation without prolapse; with larger defect (> 10 mm), there was dural pulsation and prolapse. These finding were constant regardless of the etiology of the lesion and the reconstruction material used. Conclusions: This long-term study demonstrated the efficacy of nasal turbinate graft in sealing of CSF leak without any delayed complications. Other rigid materials may be considered in reconstruction of large skull base defect (more than 10 mm) to prevent dural prolapse and herniation. For any future endonasal procedure for those patients, who had previous endonasal endoscopic duraplasty, the surgeons should be fully aware of the state of duraplasty (e.g., dural prolapse) to avoid any intraoperative complication (e.g., penetration of the prolapsed dura during nasal packing).
Keywords: Endonasal, endoscopic, skull base, nasal turbinate
Endoscopic endonasal reconstruction of skull base defect for sealing of cerebrospinal fluid (CSF) rhinorrhea or following tumor resection is essential to: (1) form a watertight dural seal; (2) provide a barrier between the contaminated sinonasal space and the sterile subdural compartment; (3) prevent airflow into the intracranial space; (4) maintain a functional sinonasal system; and (5) provide a good cosmesis. It avoids serious and life-threatening complications (e.g., meningitis, encephalitis, or a cerebral abscess).1,2
In a previous report,2 we described the utilization and short-term follow-up of nasal turbinate tissue graft for repair of skull base defect. In that report, it was demonstrated that nasal turbinate tissue was a good source of donor material for successful endonasal reconstruction of skull base defects. It is costless, safe, soft, malleable, and easy to obtain in the same field of surgery with suitable size without inducing side effects or complications.
This work was performed to study the long-term outcome of endonasal endoscopic skull base reconstruction with nasal turbinate free graft.
PATIENTS AND METHODS
Between June 1997 and March 2006, 55 consecutive patients underwent endonasal endoscopic skull base reconstruction with nasal turbinate graft and were available for follow-up. They were managed at ENT and Neurosurgery Departments in El-Menoufyia University Hospital, El-Menoufyia, El-Hikma Hospital for Neurosurgery, El-Mansoura International Hospital, Dakahlia, Egypt and Riyadh Medical complex, Riyadh, Kingdom of Saudi Arabia.
All patients had clinical assessment and preoperative nasal endoscopy prior to surgery. Ophthalmic, endocrine, and radiological evaluations (plain X-ray, computed tomography [CT] scans, CT cisternogram, magnetic resonance imaging [MRI] with contrast enhancement) were done when indicated prior to surgery. Patients of this study group were classified as follows.
Patients with Pituitary Adenomas
This group consisted of 30 patients (17 men and 13 women) between 20 and 67 years of age (Table 1). There were 20 patients with macroadenomas (including three patients with pituitary apoplexy) and 10 with microadenomas. Four patients had recurrent pituitary adenomas. The histological diagnoses of pituitary adenomas were hormone-secreting pituitary adenomas in 18 patients (15 prolactinomas and three acromegalic), and 12 were nonsecreting adenomas. Patients with prolactinomas had received a fair trial with bromocriptine therapy previously with little improvement. The nonsecreting pituitary adenomas occurred in nine patients who presented with a visual disorder and three with symptoms of pituitary apoplexy.
Table 1.
Data of Patients with Pituitary Adenomas Included in This Study
| Patient No. | Age | Gender | Type of Lesion | Size (mm) | Follow-up Period (mo) | Pulsation | Prolapse |
|---|---|---|---|---|---|---|---|
| Follow-up ranged from 6 to 96 months (median 28 and mean 34). | |||||||
| 1 | 45 | Male | Nonsecreting macroadenoma | 18 | 96 | + | + |
| 2 | 55 | Male | Microadenoma, growth hormone secreting | 10 | 20 | + | + |
| 3 | 38 | Male | Microadenoma, prolactinoma | 18 | 32 | + | + |
| 4 | 24 | Female | Microadenoma, prolactinoma | 16 | 28 | + | + |
| 5 | 26 | Male | Nonsecreting macroadenoma | 15 | 24 | + | + |
| 6 | 27 | Female | Macroadenoma, growth hormone adenoma | 16 | 36 | + | + |
| 7 | 45 | Female | Macroadenoma, prolactinoma | 17 | 36 | + | + |
| 8 | 67 | Female | Macroadenoma, prolactinoma | 10 | 18 | + | + |
| 9 | 36 | Female | Microadenoma, prolactinoma | 12 | 48 | + | + |
| 10 | 30 | Male | Macroadenoma, prolactinoma | 16 | 24 | + | + |
| 11 | 53 | Male | Nonsecreting macroadenoma | 14 | 28 | + | + |
| 12 | 20 | Female | Microadenoma, prolactinoma | 11 | 24 | + | + |
| 13 | 46 | Male | Nonsecreting macroadenoma | 12 | 26 | + | + |
| 14 | 36 | Female | Microadenoma, prolactinoma | 15 | 28 | + | + |
| 15 | 27 | Male | Nonsecreting macroadenoma | 16 | 34 | + | + |
| 16 | 43 | Male | Pituitary apoplexy | 15 | 24 | + | + |
| 17 | 40 | Female | Microadenoma, prolactinoma | 10 | 60 | + | + |
| 18 | 56 | Female | Macroadenoma, prolactinoma | 18 | 18 | + | + |
| 19 | 27 | Female | Microadenoma, prolactinoma | 13 | 24 | + | + |
| 20 | 26 | Female | Microadenoma, prolactinoma | 17 | 72 | + | + |
| 21 | 37 | Male | Nonsecreting macroadenoma | 15 | 28 | + | + |
| 22 | 38 | Male | Pituitary apoplexy | 16 | 64 | + | + |
| 23 | 67 | Male | Nonsecreting macroadenoma | 15 | 32 | + | + |
| 24 | 39 | Male | Nonsecreting macroadenoma | 11 | 32 | + | + |
| 25 | 24 | Female | Microadenoma prolactinoma | 18 | 18 | + | + |
| 26 | 42 | Male | Macroadenoma, growth hormone secreting | 14 | 50 | + | + |
| 27 | 36 | Female | Nonsecreting macroadenoma | 17 | 19 | + | + |
| 28 | 52 | Male | Macroadenoma, prolactinoma | 11 | 48 | + | + |
| 29 | 42 | Male | Pituitary apoplexy | 13 | 6 | + | + |
| 30 | 53 | Male | Macroadenoma, prolactinoma | 13 | 24 | + | + |
Patients with CSF Rhinorrhea
There were 10 patients with iatrogenic, six with spontaneous, and four with traumatic CSF rhinorrhea (Table 2). Patients with iatrogenic CSF rhinorrhea included three that occurred during functional endoscopic sinus surgery (FESS) for recurrent chronic ethmoidal sinusitis, three that occurred during FESS for recurrent sinonasal polyposis, three patients who developed CSF leak postoperatively after endonasal pituitary surgery (6 to 8 days), and one case that occurred during excision of stage IIIb juvenile angiofibroma (based on Fisch classification3) by endoscopic-assisted midfacial degloving approach.4
Table 2.
Data of Patients with CSF Rhinorrhea Included in This Study
| Patient No. | CSF Rhinorrhea Patients | Site of Skull Base Defect | Size (mm) | Technique of Duraplasty | FU Period (mo) | Pulsation | Prolapse |
|---|---|---|---|---|---|---|---|
| CP, cribriform plate; FE, fovea ethmoidalis; OF, olfactory fossa; FU, follow-up; lat., lateral; Bilat., bilateral; MT, middle turbinate; PE, posterior ethmoids; ST, superior turbinate; RCES, recurrent chronic ethmoidal sinusitis; RSNP, recurrent sinonasal polyps. | |||||||
| Follow-up ranged from 6 to 94 months (median 24 and mean 28.45). | |||||||
| 1 | Spontaneous | CP defects in FE | 3 | Overlay | 26 | − | − |
| 2 | Traumatic | OF lat. wall | 3 | Overlay | 20 | − | − |
| 3 | Traumatic | Bilat. FE defects | 4/6 | Overlay/combined overlay and underlay | 24 | −/+ | −/− |
| 4 | Perioperative during FESS for RCES | Junction between MT and FE | 5 | Overlay | 17 | − | − |
| 5 | Perioperative during FESS for RCES | Junction between MT and FE | 4 | Overlay | 42 | − | − |
| 6 | Postoperative after PS | Sellar floor | 16 | Combined overlay and underlay | 18 | + | + |
| 7 | Excision of stage IIIb JAF | PE adjacent to junction of ST and FE | 13 | Combined overlay and underlay | 94 | + | + |
| 8 | Postoperative after PS | Sellar floor | 18 | Combined overlay and underlay | 28 | + | + |
| 9 | Perioperative during FESS for RSNP | Junction between MT and FE | 3 | Overlay | 26 | − | − |
| 10 | Spontaneous | CP defects in FE | 4 | Overlay | 34 | − | − |
| 11 | Spontaneous | Roof of the sphenoid | 5 | Overlay | 48 | − | − |
| 12 | Traumatic | OF lat. wall | 4 | Overlay | 6 | − | − |
| 13 | Perioperative during FESS for RCES | Junction between MT and FE | 3 | Overlay | 18 | − | − |
| 14 | Postoperative after PS | Sellar floor | 15 | Combined overlay and underlay | 24 | + | + |
| 15 | Perioperative during FESS for RSNP | Junction between MT and FE | 7 | Combined overlay and underlay | 14 | + | − |
| 16 | Spontaneous | CP defects in FE | 3 | Overlay | 18 | − | − |
| 17 | Spontaneous | CP defects in FE | 5 | Overlay | 16 | − | − |
| 18 | Perioperative during FESS for RSNP | Junction between MT and FE | 4 | Overlay | 18 | − | − |
| 19 | Traumatic | OF lat. wall | 3 | Overlay | 42 | − | − |
| 20 | Spontaneous | CP defects in FE | 4 | Overlay | 36 | − | − |
There were six patients with spontaneous CSF rhinorrhea. They presented with symptoms of spontaneous intermittent CSF rhinorrhea (unilateral in five patients and bilateral in one), which failed to respond to conservative medical treatments. The leak persisted for a period ranging from 5 to 10 months. Preoperative CT cisternogram and MRI showed evidence of the leak in all cases.
There were four patients with traumatic CSF rhinorrhea. CSF leak was unilateral in three cases, and it was due to minor head injury with fracture lines at the floor of the anterior cranial fossa as demonstrated by high-resolution computed tomography and MRI. None of these patients required other operative intervention. The last case was a 38-year-old man who had a road traffic accident with multiple skull bone fractures and persistent bilateral CSF leak. He was operated in another hospital for fixation of the fractured skull bone and transcranial skull base reconstruction for bilateral defects in fovea ethmoidalis. One month after surgery, he developed meningitis after recurrence of CSF leak. He received successful medical treatment for meningitis and underwent a lumboperitoneal shunt as a treatment for recurrent CSF leak. Six months later, the shunt was obstructed and it was replaced by ventriculoperitoneal shunt, which also was obstructed. He came to our hospital with another attack of meningitis following recurrent CSF leak from the same previously reported sites.
Patients with Meningoencephaloceles
The group consisted of three patients (two men and one woman), aged between 8 and 34 years (Table 3). The presenting symptoms were spontaneous intermittent CSF rhinorrhea and/or nasal obstruction due to intranasal cavity mass. CT scans and MRI showed the lesions in all cases.
Table 3.
Data of Patients with Meningoceles and Meningiomas Included in This Study
| Pat. No. | Etiology of Defect | Gender | Age (y) | Size (mm) | Site of Skull Base Defect | Technique of Duraplasty | Follow-up Period (mo) | Pulsation | Prolapse |
|---|---|---|---|---|---|---|---|---|---|
| Follow-up ranged from 18 to 28 months (median 18 and mean 21.6). | |||||||||
| 1 | Meningoencephalocele | Male | 8 | 4 | Ethmoid | Overlay | 18 | − | − |
| 2 | Meningoencephalocele | Male | 25 | 5 | Ethmoid | Overlay | 12 | − | − |
| 3 | Meningoencephalocele | Female | 34 | 15 | Junction between nasal septum and cribriform plate | Combined overlay and underlay | 18 | + | + |
| 4 | Greater wing meningioma | Male | 40 | 18 | Sphenoid and posterior ethmoid area | Combined overlay and underlay | 32 | + | + |
| 5 | Recurrent olfactory groove meningioma | Male | 45 | 10 | Olfactory groove | Combined overlay and underlay | 28 | + | + |
Patients with Skull Base Meningiomas
They were two male patients aged 40 and 45 years old (Table 3). The first case was an extensive greater wing meningioma reaching the nasal cavity. It was treated by combined approach (trans-cranial pterional approach for the cranial part and endonasal endoscopic approach for the transnasal part). Surgery was followed by radiotherapy to the residual tumor in the lateral sellar compartment. The second case was recurrent olfactory grove meningioma, which was treated also by combined approach (oblique subfrontal approach for the cranial part and endonasal endoscopic removal for the transnasal part).
Surgical Procedures
The procedures were performed by otolaryngologist or by a team of an otolaryngologist and a neurosurgeon. The operative procedures were planned according to the nature of the lesions. Endoscopic endonasal approach with partial middle turbinectomy, as described by El-Banhawy et al,5 was used in most surgeries. Patients with pituitary adenomas were dealt with according to the method described by Jho et al.6 Patients with meningoencephalocele and CSF rhinorrhea were dealt with according to the method described by Mattox and Kennedy.7 Meningiomas were dealt with by the method reported by Jho and Ha.8
Methods of Reconstruction
Bolger and McLaughlin9 found that the average size of skull base bone defect in cases with CSF leak and encephalocele repair was ~0.92 × 0.7 cm. Accordingly, intraoperative skull base bone defect was measured and recorded using the diameter of the utilized endoscope (4 mm). If the bone defect was less than the endoscope diameter, it was considered as small, less than double of the diameter was designated as a moderate defect, and if larger than that was considered as a large defect.
The nasal turbinate was the grafting materials for all patients. It was obtained from middle turbinate when a partial middle turbinectomy approach was used for surgery. In patients where partial middle turbinectomy was not done, nasal turbinate graft was obtained from ipsilateral posterior two-thirds of inferior turbinate. The harvested nasal turbinate graft was incised longitudinally at its lateral border and opened in such a manner that the bone and mucoperiosteum lay superiorly and the covering nasal mucosa inferiorly. A turbinate graft was fashioned with scissors and cut to a size 50% larger than that of skull base defect. Turbinate graft is flexible and can be inserted by one side, then spread easily in the chosen site because of its elasticity and reasonable stiffness. The maneuver is easy to perform with achieving a watertight seal without restriction related to the working space, which is usually limited.
The technique of repair was chosen according to the site and size of the defects. For small defects (< 5 mm), an overlay technique was utilized, where the graft was fixed over the bone (extracranial); nasal mucosa around the defect was removed to allow the perfect adhesion of the graft extracranial to the bone.
For moderate-sized (5 to 10 mm) and large defects (> 10 mm), an overlay and underlay technique,2 was performed, which uses two grafts, one inserted under the bone defect between bone and dura and the other as an overlay graft. Combination of nasal turbinate tissue and other different simple grafts materials (e.g., abdominal free fat, pedicled mucopericondrial graft from the ipsilateral nasal septum) were used in some cases.
After obtaining a watertight seal, duraplasty multiple layers of Gelfoam soaked with autogenous local laboratory-prepared fibrin glue were inserted under the grafts. A layer of packing ribbon gauze soaked in gentamicin cream was placed beneath them and kept in place for 2 days. Patients were kept in the hospital to apply systemic intravenous antibiotic, to observe them for the onset of diabetes insipidus, and to exclude CSF leak or other complications. The nasal pack was removed 48 hours after surgery.
Follow-up with endoscopic nasal examination was done routinely 1 month after surgery to exclude synechia formation, to remove crustation, and to document the state of the nasal cavity. Endonasal endoscopic morphological appearances of successful duraplasties were documented from the third month to the end of the follow-up period using an integrated imaging system with a digitally enhanced video camera enabled still and video images. Digital pictures were reproduced by coupling the video images with a computer video capture system. CT and MRI were performed when indicated. The follow-up period ranged from 6 months to 8 years.
RESULTS
Patients with Pituitary Adenomas
There was neither neural nor vascular injury. Intraoperative CSF leak was encountered in 14 patients (12 macroadenomas and two microadenomas). The size of bone defects that occurred during tumor removal ranged from 10 mm to 18 mm at sella floor (Table 1). The mean operative time was 2.1 ( ± 0.7), hours and the average intraoperative blood loss was 130 mL.
Postoperative CSF leaks were recorded in three patients. They were repaired successfully by endonasal endoscopic approach. Postoperative intranasal synechia were found in five patients in the first 2 weeks of surgery. They were divided under local anesthesia. No other complications related to the surgery or the closure technique occurred in this series during the follow-up period.
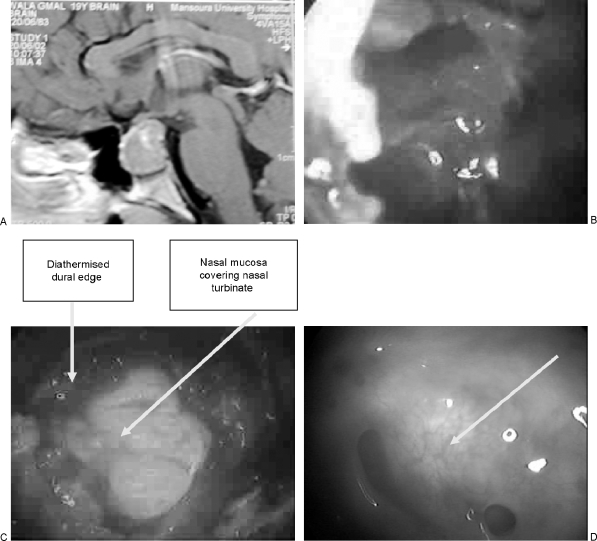
Endonasal endoscopic view at the site of duraplasty after 3 months of surgery and throughout the follow-up period showed dural pulsation and prolapse at the site of duraplasty. The dural prolapse was mild, ~2 to 3 mm from the level of skull base (Fig. 1).
Figure 1.
(A) Preoperative magnetic resonance imaging of pituitary macroadenoma. (B) Intraoperative endoscopic view, 0 degrees, of the sellar cavity after removal of macroadenoma visualizing cerebrospinal fluid leak. (C) Intraoperative image at the completion of surgery showing the middle turbinate tissue fitted and fashioned inside the sella. A watertight seal was achieved. (D) Postoperative image (3 years) of the same case showing vascularized dura with mild prolapse at the site of duraplasty (arrows).
Patients with CSF Rhinorrhea
There were no major operative or postoperative complications. In patients with iatrogenic CSF rhinorrhea, the size of the bone defects varied from 3 to 13 mm. The largest bony defect, which occurred during excision of stage IIIb juvenile angiofibroma, was adjacent to the junction of left superior turbinate and fovea ethmoidalis. In patients with spontaneous (normal pressure leak) CSF rhinorrhea, the size of the bone defects varied from 3 to 5 mm. In patients with unilateral traumatic CSF rhinorrhea, the size of the bone defects varied from 3 to 4 mm. The patient with bilateral CSF leak had bilateral bone defects in fovea ethmoidalis (4 mm in left site and 6 mm in the right side).
Postoperative intranasal synechiae were found in three patients in the first 2 weeks after surgery. They were divided under local anesthesia. Complete closure of the leaks was achieved in all patients. In one case of spontaneous CSF leak that was operated endoscopically, the leak recurred 6 months postoperatively and ceased spontaneously after a month with conservative medical treatment.
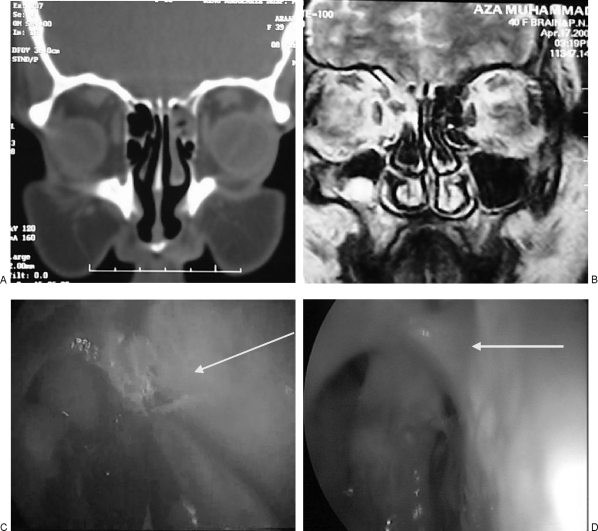
Starting from 3 months after surgery to the rest of the follow-up period, endonasal endoscopic view of the site of duraplasty showed that with small skull base defects (less than 5 mm), there was neither dural pulsation nor prolapse (Fig. 2). With moderate-sized defects (5 to 10 mm), there was dural pulsation without prolapse, and with larger defects (> 10 mm), dural pulsation and prolapse were apparent.
Figure 2.
A case of spontaneous cerebrospinal fluid. (A) Computed tomography cisternogram showing contrast accumulation at the level of the bony dehiscence in the right cribriform plate and fovea ethmoidalis. (B) Magnetic resonance imaging for the same patient showing accumulation at the same site. (C) Intraoperative endoscopic (0 degrees) view of the same case showing cribriform plate defects in fovea ethmoidalis adjacent to anterior ethmoidal artery. (D) Postoperative (4 years) of the same case showing vascularized dura without prolapse at the site of duraplasty (arrows).
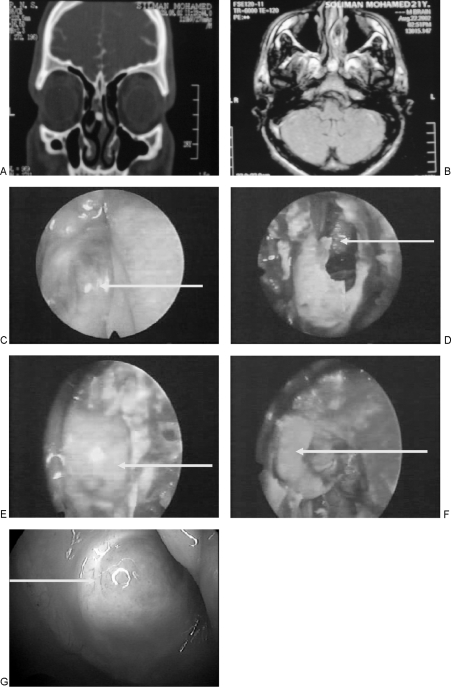
Patients with Meningoencephaloceles
Meningoencephalocele originated from the ethmoid complex in two patients, and the sizes of the bone defects after excision were 4 to 5 mm; the third case was from the junction between nasal septum and cribriform plate where the size of the bone defects was 15 mm (Fig. 3). Complete excision of the herniated part and closure of the defect were achieved in all patients. No complications were seen and no patients developed meningitis or postoperative anosmia.
Figure 3.
A case of a meningeo-encephalocele (A) Preoperative plain CT (coronal view) showing herniated intranasal meningeo-encephalocele in the left nasal cavity. (B) Preoperative non contrast MRI (axial T2 WI) of the same case. (C) Intraoperative endoscopic (30°) view of the same case showing the meningeo-encephalocele protruding between left middle turbinate and lateral nasal wall (arrow). (D) Intraoperative endoscopic (0°) view of the same case showing brain tissue through the skull base defect after excision of the meningeo-encephalocele (arrow). (E, F) Intraoperative endoscopic (0°) view showing underlay (E) and overlay (F) skull base grafting by mucoperiostium layer combined with bone taken from the harvested middle (arrows). (G) Postoperative (turbinate 5 years) of the same case showing vascularized dura with mild prolapse at the site of duraplasty (arrows).
Endonasal endoscopic view at the site of duraplasty 3 months after surgery and throughout the follow-up period did not show dural pulsation or prolapse at the site of duraplasty in the first two cases and dural pulsation with mild prolapse in the third case (Table 3).
Patients with Skull Base Meningiomas
Endoscopic exposure for the meningiomas was not adequate without excision of the lower half of the middle turbinate, which also facilitated the endonasal endoscopic removal of the tumor. The sizes of the bone defects were 18 and 10 mm, respectively (Table 3). No major operative or postoperative complications were seen, and skull reconstruction was successful with no CSF leak.
Endonasal endoscopic view at the site of duraplasty 3 months after surgery and throughout the follow-up period showed dural pulsation and prolapse occurred at the site of duraplasty (Table 3).
DISCUSSION
Skull base surgery has undergone an evolution as advanced endoscopic endonasal techniques and modern neuroimaging allow for safe and sometimes radical resection for different skull base lesions. In most cases, surgical management is best optimized using a multidisciplinary team consisting of neurosurgeons and otolaryngologists.1,2,3,4,5
Endoscopic endonasal reconstruction of skull base defects for sealing of CSF rhinorrhea or following tumor resection is of paramount importance in avoiding serious and life-threatening complications (e.g., meningitis, encephalitis, or a cerebral abscess).2,3,4,5
In the current study, we used the endoscopic endonasal partial middle turbinectomy approach5 in most of the surgeries; besides the wider surgical field created by this approach, the harvested piece of turbinate obtained was used in repairing the skull base defect. It was used either as an overlay, underlay, or combined technique of repair.1,2,3,4,5,6,7,8 By utilizing that approach, there was no need to use any other reconstructive materials, either autologous materials like the cartilage or mucoperichondrium of the nasal septum, which in some occasions were unavailable,10,11 or artificial foreign materials like titanium plates11 or ceramic substances.12 These materials are limited by their rigidity, availability, compatibility with MRI, and its cost.
In a previous report,2 we described the utilization and short-term follow-up of nasal turbinate free graft for repair of skull base defect. In that report, it was shown that middle turbinate tissue has proven to be an excellent source of donor material for successful endonasal reconstruction of the skull base defect after transnasal endoscopic of skull base surgery. It was effective in sealing intraoperative CSF leak, obliteration of dead space, and anatomic reconstruction of the skull base. We highlighted the need for long-term follow-up before final assessment of this technique.
The current long-term study did not show any evidence of nasal turbinate graft migration or inflammatory changes, granuloma, or osteitis that may cause delayed brain abscess formation. One case of a granuloma and hematoma around the dimethylpolysiloxane (silicone) plate has been reported after transsphenoidal surgery by Matsumoto et al,13 in which a delayed immune response to a foreign body was considered to have played a major role.
The major advancement in skull base reconstruction is free tissue transfer, which is regarded by most authors as the best method to repair defects of the skull base.14,15,16 The choice of the graft is paramount to the location, size of the leak, and anatomy of each patient.17 The size of the graft has to exceed the dimensions of the prepared area.
The current work and that of Fliss et al19 and Tachibana et al18 confirmed that successful skull base reconstruction could be achieved by free nasal turbinate autologous grafts without requiring blood supply from an overlying regional flap. Moreover, the rapid healing process of this reconstruction provides a robust physiological barrier between the nasopharynx and the intracranial space within days following surgery.18,19 Bolger and McLaughlin9 used cranial bone grafts in CSF leak and encephalocele repair. They demonstrated that cranial bone graft is an excellent material for endoscopic reconstruction of skull base defects. It confers special advantages in large defects, in defects with complex three-dimensional characteristics, and in patients with CSF leaks associated with an elevated intracranial pressure.
Endonasal endoscopic follow-up of the patients of the current study to view the site of duraplasty showed that whenever the original size of the defect was less than 5 mm, there was neither dural pulsation nor prolapse regardless the etiology of the lesion and the reconstruction material used. The integration between the grafting material used and the vascularized fibrous tissue that occurred during the healing process of the dura was so tight that it did not allow dural pulsation nor prolapse through this small defect (less than 5 mm).
With moderate-sized skull base bone defect (5 to 10 mm), it is likely that the surrounding edges of skull base bone defect act as supportive shoulders to the successfully healed dura, which permitted pulsation and prevented its downward prolapse. In larger skull base bone defect (more than 10 mm), surrounding edges of this large skull base bone defect could not act as a supportive shoulder, resulting in dural pulsation and prolapse at the site of duraplasty.
In a trial to investigate the healing process of skull base grafts in patients who had undergone a second surgery, Fliss et al19 reported that histological examination of previously harvested human fascial flaps showed evidence of integration of a vascularized fibrous tissue into the fascial graft. They found that fascial flap was uniformly coated by fibrous tissue, and invasion of blood vessels was achieved without the presence of an overlying vascularized flap. In an animal model, Tachibana et al18 demonstrated a tight connection between the fascial graft and the dura within 1 week after surgery. They reported that the fascial graft had been completely replaced by durable fibrous tissue by 2 weeks following the surgical repair, and they speculated that fibroblast growth factor18 plays a significant role in the healing process of free fascial grafts.
CONCLUSIONS
This long-term study demonstrated that dural pulsation and prolapse at the site of the successful duraplasty is a function of the size of the bony defect and does not depend on the pathology of the lesion or the autologous material used for reconstruction. These grafts are eventually replaced by durable fibrous tissue. Other rigid materials may be considered in reconstruction of large skull base defect (more than 10 mm) to prevent dural prolapse and herniation. For any future endonasal procedure for patients who had previous endonasal endoscopic duraplasty, the surgeons should be fully aware of the state of duraplasty (e.g., dural prolapse) to avoid any intraoperative complication (e.g., penetration of the prolapsed dura during nasal packing).
REFERENCES
- El-Banhawy O A, Halaka A N, El-Hafiz Shehab El-Dien A, Ayad H. Subcranial transnasal repair of cerebrospinal fluid rhinorrhea with free autologous grafts by the combined overlay and underlay techniques. Minim Invasive Neurosurg. 2004;47:197–202. doi: 10.1055/s-2004-818513. [DOI] [PubMed] [Google Scholar]
- El-Banhawy O A, Halaka A N, El-Dien A E, Ayad H. Sellar floor reconstruction with nasal turbinate tissue after endoscopic endonasal transsphenoidal surgery for pituitary adenomas. Minim Invasive Neurosurg. 2003;46:289–292. doi: 10.1055/s-2003-44453. [DOI] [PubMed] [Google Scholar]
- Andrews J C, Fisch U, Valavanis A, Aeppli U, Makek M S. The surgical management of extensive nasopharyngeal angiofibromas with the infratemporal fossa approach. Laryngoscope. 1989;99:429–437. doi: 10.1288/00005537-198904000-00013. [DOI] [PubMed] [Google Scholar]
- El-Banhawy O A, Shehab El-Dien A, Amer T. Endoscopic-assisted midfacial degloving approach for type III juvenile angiofibroma. Int J Pediatr Otorhinolaryngol. 2004;68:21–28. doi: 10.1016/j.ijporl.2003.09.013. [DOI] [PubMed] [Google Scholar]
- El-Banhawy O A, El-Dien A E, Zolfakar A S, Halaka A N, Ayad H. Endoscopic endonasal partial middle turbinectomy approach: adaptability of the procedure in a cadaveric study and in surgery for different sphenoid sinus and skull base lesions. Skull Base. 2006;16:1–13. doi: 10.1055/s-2005-922014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jho H D, Carrau R L, Ko Y. In: Rengachary SS, Wilkins RH, editor. Neurosurgical Operative Atlas. Vol. 5. Park Ridge, IL: American Association of Neurological Surgeons; 1996. Endoscopic pituitary surgery. p. 112.
- Mattox D E, Kennedy D W. Endoscopic management of cerebrospinal fluid leaks and cephalocele. Laryngoscope. 1990;100:857–862. doi: 10.1288/00005537-199008000-00012. [DOI] [PubMed] [Google Scholar]
- Jho H D, Ha H G. Endoscopic endonasal skull base surgery: part 1—the midline anterior fossa skull base. Minim Invasive Neurosurg. 2004;47:1–8. doi: 10.1055/s-2003-812538. [DOI] [PubMed] [Google Scholar]
- Bolger W E, McLaughlin K. Cranial bone grafts in cerebrospinal fluid leak and encephalocele repair: a preliminary report. Am J Rhinol. 2003;17:153–158. [PubMed] [Google Scholar]
- Jho H D, Carrau R L, Ko Y, Daly M A. Endoscopic pituitary surgery: an early experience. Surg Neurol. 1997;47:213–222. discussion 222–223. doi: 10.1016/s0090-3019(96)00452-1. [DOI] [PubMed] [Google Scholar]
- Arita K, Kurisu K, Tominaga A, et al. Size-adjustable titanium plate for reconstruction of the sella turcica: technical note. J Neurosurg. 1999;91:1055–1057. doi: 10.3171/jns.1999.91.6.1055. [DOI] [PubMed] [Google Scholar]
- Kobayashi S, Sugita K, Matsuo K, Inoue T. Reconstruction of the sellar floor during transsphenoidal operations using alumina ceramic. Surg Neurol. 1981;15:196–197. doi: 10.1016/0090-3019(81)90142-7. [DOI] [PubMed] [Google Scholar]
- Matsumoto M, Kohmura E, Tsuruzono K, Mori K, Kawano K, Tsujimura T. Silicone plate-induced granuloma presenting pituitary apoplexylike symptoms: case report. Surg Neurol. 1995;43:166–169. doi: 10.1016/0090-3019(95)80129-5. [DOI] [PubMed] [Google Scholar]
- Izquierdo R, Leonetti J P, Origitano T C, et al. Refinements using free-tissue transfer for complex cranial base reconstruction. Plast Reconstr Surg. 1993;92:567–575. [PubMed] [Google Scholar]
- Funk G F, Laurenzo J F, Valentino J, et al. Free-tissue transfer reconstruction of midfacial and cranio-orbito-facial defects. Arch Otolaryngol Head Neck Surg. 1995;121:293–303. doi: 10.1001/archotol.1995.01890030033006. [DOI] [PubMed] [Google Scholar]
- Urken M L, Catalano P J, Sen C, et al. Free tissue transfer for skull base reconstruction: analysis of complications and a classification scheme for defining skull base defects. Arch Otolaryngol Head Neck Surg. 1993;119:1318–1325. doi: 10.1001/archotol.1993.01880240054007. [DOI] [PubMed] [Google Scholar]
- Couldwell W T. Surgery of the anterior skull base. Otolaryngol Clin North Am. 1993;26:673–693. [PubMed] [Google Scholar]
- Tachibana E, Saito K, Fukuta K, et al. Evaluation of the healing process after dural reconstruction achieved using a free fascial graft. J Neurosurg. 2002;96:280–286. doi: 10.3171/jns.2002.96.2.0280. [DOI] [PubMed] [Google Scholar]
- Fliss D M, Gil Z, Spektor S, et al. Skull base reconstruction after anterior subcranial tumor resection. Neurosurg Focus. 2002;12:e10. doi: 10.3171/foc.2002.12.5.11. [DOI] [PubMed] [Google Scholar]