ABSTRACT
Objectives: 1. Case report of foreign body and associated orbitoethmoid and skull base mucocele following orbital blowout fracture repair. 2. Literature review of orbital fracture repair complications and endoscopic removal of paranasal sinus and anterior skull base foreign body. Design: Case report and literature review. Setting: Tertiary-care academic otolaryngology practice. Results: Foreign body involvement of the orbit, paranasal sinuses, and skull base are relatively rare entities. In contrast, orbital blowout fractures are relatively common facial fractures. We report skull base involvement of a previously placed orbital floor implant complicated by mucocele formation and exophthalmos. Successful endoscopic removal and decompression of foreign body and associated mucocele were accomplished. Review of orbital floor fracture repair complications and paranasal sinus and skull base foreign body endoscopic removal were also performed. Conclusions: Transnasal endoscopic removal of complicated foreign bodies involving the orbit, paranasal sinuses, and anterior skull base can be successfully accomplished given appropriate patient selection and careful technique.
Keywords: Orbital fractures, skull base, paranasal sinus, foreign body
Orbital blowout fractures are relatively common sequelae of midfacial trauma. Considerable variation exists in the literature regarding the indications for operative exploration, reduction, and fixation as well as the optimal techniques and implant materials used for these fractures. Multiple studies have reported complications with enophthalmos, with infection and visual disturbance among the more commonly reported complications. Plate migration and cyst and mucocele formation have also previously been reported.1,2,3,4,5,6,7,8
Foreign bodies involving the paranasal sinuses and skull base are rare, with the majority of these being posttraumatic in nature.9 We report the first case of migration of a previously placed orbital floor plate resulting in an anterior skull base and orbital mucocele. We also review orbital blowout fracture repair complications and previous reports of paranasal sinus and anterior skull base foreign bodies.
METHODS
Our case report is followed by a literature review using PubMed with a combination of the terms: “orbit blowout fracture, complications, Silastic (Dow Corning, Midland, MI), removal, transnasal,” “orbit foreign body, transnasal, anterior cranial fossa, skull base, cribriform” with limits to English language. A total of 34 articles were identified for further review.
CASE REPORT
A 40-year-old male with a history of previous right orbital fracture repaired at an outside facility 10 years prior to his presentation complained of recent onset of episodic severe pain, swelling and erythema of his right eye, and periorbital area with concurrent diplopia with each episode. Additionally, he reported decreased right cheek sensation with each episode. Previous oral and intravenous antibiotic treatment yielded a good response for a presumed diagnosis of ethmoid sinusitis and periorbital cellulitis. His past medical history was significant for a stable asymptomatic pituitary adenoma being managed medically and a previous endoscopic sinus surgery performed 6 years prior.
On physical examination he was noted to have diplopia worst in the superior and right lateral visual fields, along with minimal (1 to 2 mm) proptosis of the right eye. His extraocular movements superior and laterally were mildly restricted on the right. Visual acuity was 20/20 in both eyes, and the remainder of his physical exam was significant only for minimal hypesthesia in the distribution of the right infraorbital nerve. Flexible nasopharyngeal endoscopy was performed, which revealed only fullness in the right middle meatus and lateral nasal wall without any mucosal disease or evidence of sinusitis.
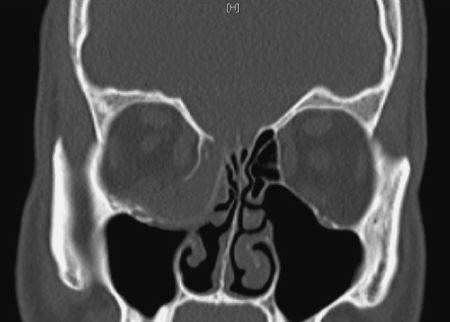
Magnetic resonance imaging (MRI) and computed tomography (CT) scans of the head and sinuses (Figs. 1 and 2) were obtained, which revealed significant accumulation of a hypodense material in the right anterior ethmoid sinus and orbit to the root of the middle turbinate. A linear foreign body was noted to be impinging upon the cribriform plate without evidence of intracranial involvement and appeared to be causing the obstruction in this area. Due to concern for the risk of continued expansion and possible spread of infection intraorbitally and intracranially, the decision was made to take the patient for a transnasal endoscopic decompression of the mucocele with removal of the foreign body. The patient also consented for the endoscopic repair of any skull base defect if deemed necessary intraoperatively.
Figure 1.
Axial computed tomography without contrast showing intraorbital fluid collection lateral to foreign body.
Figure 2.
Coronal computed tomography without contrast showing foreign body involvement of anterior skull base with ethmoid and orbital mucocele.
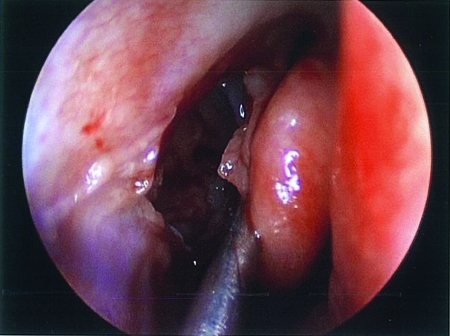
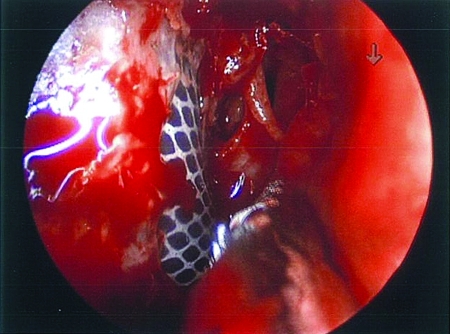
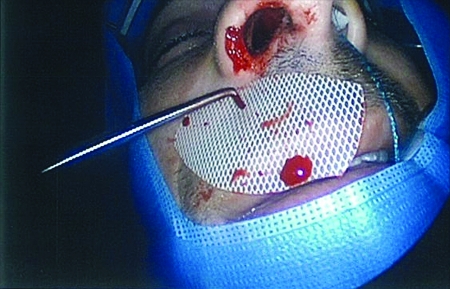
We performed a stereotactic navigation-assisted transnasal endoscopic approach and noted the patient to have a distinct erythematous bulge centered on the middle meatus and lateral nasal wall (Fig. 3). Upon incising the area of the ethmoid bulla, we encountered immediate copious mucopurulent secretions surrounding a thin membrane bluish-gray in color in which was embedded a Silastic implant (Fig. 4). Careful dissection of the implant was carried medially into the orbit and toward the skull base. There was apparent erosion of the root of the middle turbinate with impingement upon the cribriform plate noted, and the implant was carefully dissected free. There was no sign of cerebrospinal fluid leak. A dissecting hook and straight Blakesly forceps were used to deliver the implant from the orbit and cranial base through the nasal cavity (Fig. 5). It measured 3 × 4 cm. A considerable amount of fluid the color of motor oil was mixed with the previously seen mucopurulent material in this area. This was suctioned free from behind the implant and the diseased mucosa of the medial orbital wall and floor were then removed to the point of healthy appearing bone. Thorough external evaluation revealed no significant enophthalmos despite the concern due to unopposed orbital prolapse medially. Due to no apparent cosmetically significant enophthalmos or significant dystopia, the decision was made not to reconstruct the medial orbital wall. Copious irrigation of the cavity with antibiotic impregnated saline was then performed followed by a complete ethmoidectomy and revision of his maxillary antrostomy to aid future irrigations of the area.
Figure 3.
Endoscopic transethmoid approach to orbit; middle turbinate is to right of figure.
Figure 4.
Foreign body (Silastic) revealed in ethmoid sinus.
Figure 5.
Implant removed.
Postoperatively, the patient has done well with restoration of globe symmetry without enophthalmos. His visual acuity remains consistent with his preoperative levels, and he has had no further infectious complications through the first 6 months postoperatively.
DISCUSSION
Orbital floor “blowout” fractures are relatively common sequelae of midfacial trauma. There is considerable debate regarding the indications, technique, and optimal implant material employed to best manage these injuries. Most authors agree upon the repair of any injury resulting in significant enophthalmos, persistent diplopia, herniation, or entrapment of the extraocular musculature.10 The repair methods commonly employ autologous or alloplastic materials with each choice having relative benefits over the others. Choices of implant materials have included autogenous bone (including calvarium, iliac crest, rib cartilage), titanium, porous polyethylene (Medpor, Porex Technologies, Fairburn, GA), silicone (Silastic, Dow Corning, Midland, MI), polyamide mesh (Supramid, S. Jackson, Inc., Alexandria, VA), gelatin film (Gelfilm, Pfizer, New York, NY), Marlex mesh (Marlex mesh, Chevron Phillips Chemical, The Woodlands, TX) hydroxyapatite, polyglactin910/polydiaxanone (Ethisorb, Codman, Raynham, MA), and Teflon, (DuPont, Wilmington, DE) among others.1,8,11 Repair using autogenous materials carries the disadvantages of donor site morbidity, prolonged operative time, and poorly predictable resorption rates.1 Recently, alloplastic implants have been widely accepted as the treatment of choice for repair. Improved pliability, porous architecture allowing fibrous ingrowth, ready availability of implant material, and low complication rates are cited by proponents of various materials. Rates of postoperative sequelae vary widely among reports, from 3 to 83%, with considerable difficulty noted in accurately establishing their true incidence. Determination of complication rates is difficult due to the fact that some reported “complications” could be attributed to the injury itself, and many late complications are not reported due to patients being lost to follow-up.1,4,5,6,11,12,13 Generally accepted complication rates range from 7 to 17% with variability noted among various materials used.5,13,14 Infection rates range from 0.4 to 7%.10,14
Reported complications from orbital fracture repair include enophthalmos, visual disturbance, numbness, ectropion, dystopia, extrusion or migration of implant, hemorrhage, cyst and mucocele formation, orbital infection, dacryocystitis, fistula formation, proptosis, cold intolerance, pain, and palpable hardware requiring removal.1,2,3,4,7,14,15 Several of these complications, including extrusion, migration, cyst, and hemorrhage, have been attributed directly to the implant itself.2,3,5,10,16 The majority of complications occur within weeks to months, although delayed infection, extrusion, and cyst or mucocele formation have been well documented. Jordan et al reported on the largest series of complications related to alloplastic implants in orbital fracture repair. Fistula formation, implant migration, infection, motility restriction, globe elevation (hyperophthalmia), cyst formation, hemorrhage with sudden proptosis, and optic nerve trauma were found in their series of 17 patients.8 Timing of complications postoperatively ranged from 2 weeks to 10 years. Failure to fixate the implant and fracture mobility have been noted to be contributory to the likelihood of complication occurrence.4,8
Mucocele and cyst formation following midface fracture and alloplastic implantation have been previously reported, although they are not commonly found in many of the larger series.2,3,7,16,17,18,19 Cyst formation with respiratory and squamous epithelium have both been described. Respiratory epithelial-lined cysts have been described following orbital fracture repair and are thought to arise from the traumatic implantation of respiratory epithelium into the orbit. These are most commonly described in combination with mucocele formation. When isolated, they have been described to be filled with an oily-brown fluid, as seen in our patient's case.2,3 Cyst formation following Gelfilm resorption has also been reported.8,17 Migration of the implant has also been well described. Involvement of the anterior skull base with cerebrospinal fluid leak following migration of a silicone implant was previously described only once in our review of the literature.20
Foreign body involvement of the orbit, paranasal sinuses, and skull base is a relatively rare entity, with up to 70% of cases being posttraumatic in nature.9,21 The indications and techniques for removal must be individualized and are dictated by the mechanism of injury and location of the object.9,21,22,23 The endoscopic transnasal approach to the orbit has been supported for multiple indications, including removal of an orbital foreign body.9,12,23,24,25,26 Initial open or combined approaches are typically reserved for completely intracranial foreign bodies or those complicated by risk of severe hemorrhage.26 Dodson et al have previously described the endoscopic retrieval of a completely intracranial foreign body.27
Our case represents a previously unreported complication of orbital fracture repair resulting in implant migration with mucocele involvement of the anterior skull base and orbit. Notably, there was no evidence of fixation of the implant noted during surgical removal, a factor thought to contribute to implant complication rates. Complications related to silicone itself are well documented in the literature. Increased rates of infection, migration, and rejection leading to extrusion have been documented.5,16 Fibrous capsule formation around the implant is thought to stabilize the implant in place without true integration into the surrounding tissues. The presence of the bluish-gray membrane seen in our patient is suggestive of capsule formation consistent with previous reports. Specific histological examination was not performed in this case, so this is a presumptive finding only. Cyst formation around the implant has been theorized to occur secondary to hemorrhage into the capsule.3,19 These silicone-specific reactions typically occur late, as much as 25 years postoperatively.28 The avascular plane surrounding the implant is also thought to contribute to greater risk of bacterial infection.14,17 Previous studies have shown Staphylococcus aureus and Escherichia coli to have a preferential ability to bind to the silicone polymer as well.16 Additionally, the chronic exposure to a contaminated field is thought to contribute to the potential for future infection when used to bridge a defect from the orbit to the exposed maxillary sinus.10 The removal rate for complications after the use of silicone orbital implants was 13.2% in a large series by Morrison et al.5 They questioned the routine use of silicone as an orbital implant given this complication rate but acknowledged further comparison studies with other alloplastic and autogenous materials were required to better define its role.
CONCLUSIONS
Orbital fracture repair complications occurring as late sequelae are well documented throughout the literature. Proptosis and visual changes occurring in patients with previous orbital blowout repair must be carefully evaluated clinically and radiographically with suspicion for a late complication of previous repair. Further long-term studies are needed to delineate the relative risk-to-benefit ratio of each alloplastic implant given the occurrence of late complications. Paranasal sinus and anterior skull base foreign bodies are extremely rare in the absence of trauma. Their removal is dictated by the nature of injury and location of the object. We feel that in selected cases, the removal of orbital and anterior skull base foreign bodies can be successfully achieved via an endoscopic approach.
REFERENCES
- Ozturk S, Sengezer M, Isik S, Turegun M, Deveci M, Cil Y. Long-term outcomes of ultra-thin porous polyethylene implants used in orbital floor defects. J Craniofac Surg. 2005;16:973–977. doi: 10.1097/01.scs.0000179744.91165.3a. [DOI] [PubMed] [Google Scholar]
- Neves R B, Yeatts R P, Martin T J. Pneumo-orbital cyst after orbital fracture repair. Am J Ophthalmol. 1998;125:879–880. doi: 10.1016/s0002-9394(98)00050-6. [DOI] [PubMed] [Google Scholar]
- Schmidt B L, Lee C, Young D M, O'Brien J. Intraorbital squamous epithelial cyst: an unusual complication of Silastic. J Craniofac Surg. 1998;9:452–455. discussion 456–458. [PubMed] [Google Scholar]
- Nagase D Y, Courtemanche D J, Peters D A. Plate removal in traumatic facial fractures. Ann Plast Surg. 2005;55:608–611. doi: 10.1097/01.sap.0000189666.13860.c0. [DOI] [PubMed] [Google Scholar]
- Morrison A D, Sanderson R C, Moos K F. The use of silastic as an orbital implant for reconstruction of orbital wall defects: review of 311 cases treated over 20 years. J Oral Maxillofac Surg. 1995;53:412–417. doi: 10.1016/0278-2391(95)90714-9. [DOI] [PubMed] [Google Scholar]
- Folkestad L, Westin T. Long-term sequelae following surgery for orbital floor fractures. Otolaryngol Head Neck Surg. 1999;120:914–921. doi: 10.1016/S0194-5998(99)70336-0. [DOI] [PubMed] [Google Scholar]
- Reiter E R, August M, Varvares M A, Curtin H D. Mucocele of the infratemporal fossa as an unusual complication of midface fracture. Ann Otol Rhinol Laryngol. 2000;109:522–525. doi: 10.1177/000348940010900515. [DOI] [PubMed] [Google Scholar]
- Jordan D R, St Onge P, Anderson R L, Patrinely J R, Nerad A. Complications associated with alloplastic implants used in orbital fracture repair. Ophthalmology. 1992;99:1600–1608. doi: 10.1016/s0161-6420(92)31760-9. [DOI] [PubMed] [Google Scholar]
- Kwiatkowski T J, Magardino T M, Austin M. Management of orbital-sinus foreign bodies. J Craniomaxillofac Trauma. 1998;4:24–29. [PubMed] [Google Scholar]
- Brown A E, Banks P. Late extrusion of alloplastic orbital floor implants. Br J Oral Maxillofac Surg. 1993;31:154–157. doi: 10.1016/0266-4356(93)90114-c. [DOI] [PubMed] [Google Scholar]
- Nam S B, Bae Y C, Moon J S, Kang Y S. Analysis of the postoperative outcome in 405 cases of orbital fracture using 2 synthetic orbital implants. Ann Plast Surg. 2006;56:263–267. doi: 10.1097/01.sap.0000199173.73610.bc. [DOI] [PubMed] [Google Scholar]
- Kim K S, Kim E S, Hwang J H. Combined transcutaneous transethmoidal/transorbital approach for the treatment of medial orbital fractures. Plast Reconstr Surg. 2006;117:1947–1955. doi: 10.1097/01.prs.0000218330.55731.2d. [DOI] [PubMed] [Google Scholar]
- Buchel P, Rahal A, Seto I, Iizuka T. Reconstruction of orbital floor fracture with polyglactin910/polydiaxanon patch: a retrospective study. J Oral Maxillofac Surg. 2005;63:646–650. doi: 10.1016/j.joms.2004.11.013. [DOI] [PubMed] [Google Scholar]
- Ng S G, Madill S A, Inkster C F, Maloof A J, Leatherbarrow B. Medpor porous polyethylene implants in orbital blowout fracture repair. Eye. 2001;15(Pt 5):578–582. doi: 10.1038/eye.2001.188. [DOI] [PubMed] [Google Scholar]
- Rosen C E. Late migration of an orbital implant causing orbital hemorrhage with sudden proptosis and diplopia. Ophthal Plast Reconstr Surg. 1996;12:260–262. doi: 10.1097/00002341-199612000-00007. [DOI] [PubMed] [Google Scholar]
- Gregory G F. Silicone-associated tissue reaction: a dilemma for oral and maxillofacial surgeons. Br J Oral Maxillofac Surg. 1995;33:180–184. doi: 10.1016/0266-4356(95)90294-5. [DOI] [PubMed] [Google Scholar]
- Stewart M G, Patrinely J R, Appling W D, Jordan D R. Late proptosis following orbital floor fracture repair. Arch Otolaryngol Head Neck Surg. 1995;121:649–652. doi: 10.1001/archotol.1995.01890060047009. [DOI] [PubMed] [Google Scholar]
- Yeakley J W, Ghorayeb B Y. Orbital blowout fractures as a cause of sinonasal obstructive disease. J Comput Assist Tomogr. 1992;16:774–778. doi: 10.1097/00004728-199209000-00019. [DOI] [PubMed] [Google Scholar]
- Mauriello J A, Jr, Flanagan J C, Peyster R G. An unusual late complication of orbital floor fracture repair. Ophthalmology. 1984;91:102–107. doi: 10.1016/s0161-6420(84)34335-4. [DOI] [PubMed] [Google Scholar]
- Schmidt B L, Lee C, Young D M, O'Brien S. Intraorbital squamous epithelial cyst: an unusual complication of Silastic implantation. J Craniofac Surg. 1998;9:452–455. discussion 456–458. [PubMed] [Google Scholar]
- Jin H R. Foreign body in the orbit associated with blowout fracture. Plast Reconstr Surg. 2006;117:1050–1051. doi: 10.1097/01.prs.0000201216.69887.09. [DOI] [PubMed] [Google Scholar]
- Roy D. The removal of foreign bodies from within the eyeball and orbit: report of cases. Trans Am Ophthalmol Soc. 1917;15:56–73. [PMC free article] [PubMed] [Google Scholar]
- Tsao Y H, Kao C H, Wang H W, Chin S C, Moe K S. Transorbital penetrating injury of paranasal sinuses and anterior skull base by a plastic chair glide: management options of a foreign body in multiple anatomic compartments. Otolaryngol Head Neck Surg. 2006;134:177–179. doi: 10.1016/j.otohns.2005.01.002. [DOI] [PubMed] [Google Scholar]
- Tsirbas A, Kazim M, Close L. Endoscopic approach to orbital apex lesions. Ophthal Plast Reconstr Surg. 2005;21:271–275. doi: 10.1097/01.iop.0000169254.44642.3d. [DOI] [PubMed] [Google Scholar]
- Khan-Lim D, Ellis J, Saleh H, Ram B. Endoscopic transnasal removal of orbital foreign body. Eye. 1999;13(Pt 5):667–668. doi: 10.1038/eye.1999.181. [DOI] [PubMed] [Google Scholar]
- Presutti L, Marchioni D, Trani M, Ghidini A. Endoscopic removal of ethmoido-sphenoidal foreign body with intracranial extension. Minim Invasive Neurosurg. 2006;49:244–246. doi: 10.1055/s-2006-948302. [DOI] [PubMed] [Google Scholar]
- Dodson K M, Bridges M A, Reiter E R. Endoscopic transnasal management of intracranial foreign bodies. Arch Otolaryngol Head Neck Surg. 2004;130:985–988. doi: 10.1001/archotol.130.8.985. [DOI] [PubMed] [Google Scholar]
- Dancey A L, Perry M J. Late presentation of alloplastic implant extrusion. Plast Reconstr Surg. 2004;113:1081–1082. doi: 10.1097/01.prs.0000107655.00920.fa. [DOI] [PubMed] [Google Scholar]