Abstract
Objective
To describe mental health services utilization for adolescents after attempted suicide, explore factors related to treatment compliance, and determine the relationship between compliance and suicidality.
Method
Eighty-five adolescents (ages 13–18) who had attempted suicide and their families were recruited from four psychiatric hospitals and were evaluated for symptoms of psychopathology. Subsequent assessments were conducted every six months for two years to determine treatment utilization, treatment compliance (non-adherence to medication regimes or non-attendance of psychosocial treatments against provider advice), attitudes towards treatments utilized, and further suicide attempts and ideation.
Results
Adolescents with a disruptive behavior disorder diagnosis were less compliant with individual psychotherapy, as were those with a substance dependence other than alcohol or marijuana. Those with an affective/anxiety disorder diagnosis were less compliant with psychopharmacological interventions (6 months post attempt). Parental perception of treatment as helpful was predictive of greater compliance, while adolescents' attitudes towards treatment were not predictive of compliance. Finally, compliance with treatment was not generally predictive of future suicidality.
Conclusion
Interventions focused on increasing compliance with mental health treatment for adolescent suicide attempters should focus on specific child psychopathology, as well as parental attitudes towards treatment.
Keywords: adolescent, suicide, treatment, compliance
The problem of recurrent adolescent attempted suicide is a major one and has been the focus of increasing attention.1–2 Adolescents have been shown to reattempt suicide at rates ranging from 6% to 50%,2–3 depending on the time lapse at follow-up, with up to 11% of those who initially attempt suicide eventually dying by suicide.4 Recurrent suicidal ideation is also of significance, with a range between 38.5% and 45% of adolescent suicide attempters reporting suicidal ideation at follow-up three to six months after the attempt.3,5 Although a number of treatments have shown promise in improving outcomes among suicidal youth, including individual, family, and pharmacotherapies,6–8 there is some evidence that treatment compliance is generally poor.
Treatment Compliance among suicidal youth
Compliance with mental health treatments among adolescents is recognized to be poor,9 and adolescents who attempt suicide comprise a very difficult group to engage in even initial treatment follow-through after hospitilization.10–12 Trautman, Stewart, and Morishima13 found that 77% of their sample of 112 suicide attempters (ages 10–18 years old) either did not attend or failed to complete recommended treatment, and that suicide attempters missed more appointments and dropped out more quickly from treatment than non-attempters (mean of 3 visits versus 11 visits). Similarly, Granboulan and colleagues14 reported that only 32% of adolescent attempters (13–18 year-olds) attended all scheduled appointments, 31% attended some scheduled appointment, 11% attended only one session post-hopitilization, and 25% never attended any follow-up appointment. Reported rates of non-compliance with first appointments (i.e. post-hopitilization) for this population range from 17.5% to 41.6%.11,14–16
Compliance and Suicidality Outcomes
The few studies investigating the hypothesis that treatment compliance has positive implications for adjustment outcome and course have yielded some empirical support for it. Pillay and Wassenaar17 found significantly lower rates of psychiatric symptoms and hopelessness in those who had complied with treatment as compared to those who were non-compliant. Furthermore, Rotheram-Borus and colleagues18 found that for participants in their psychosocial intervention (140 female adolescent suicide attempters, ages 12–18 years) who had low to moderate symptomatology at baseline, attending at least 7 sessions was protective vis-à-vis suicidal ideation. Finally, Callor et al.,19 found through autopsy reports that among youths (ages 21 and under) who completed suicide, 82% did not have the therapeutic level of prescribed psychotropic medication at the time of death.
Factors shown to relate to noncompliance
Since treatment compliance may have important implications for outcomes in this population, it is important to focus on factors related to noncompliance. Researchers have found poorer rates of treatment compliance among suicidal adolescents with comorbid diagnoses of substance abuse, conduct disorders,15 and depressive disorders,20 in terms of number of therapy appointments scheduled and kept, refusal of recommended treatment, and non-compliance with medication regimes.20 A number of family factors have been identified as having a positive influence on treatment compliance among adolescent suicide attempters, including parental involvement in treatment and family cohesion, which are associated with increased attendance at psychotherapy sessions, and positive parental attitudes toward mental health treatment, associated with initial treatment follow-through.12,21 King and colleagues10 assessed treatment compliance (none/minimal contact with recommended provider, some contact, or complete treatment) in the initial 6 months after hospitalization for suicidal symptoms. They found that mothers’ depressive and paranoid symptoms were associated with lower rates of individual and family treatment compliance, while mothers’ hostility was linked with poorer medication follow-through.
Purpose of the Present Study
The present study seeks to add to the limited research on treatment compliance in this population by providing: (a) Detailed description of treatment utilization and subsequent treatment compliance in a sample of hospitalized adolescents who made a recent suicide attempt; (b) A systematic examination of whether several factors are predictive of poorer treatment compliance, including particular types of adolescent psychopathology, parental psychopathology, and adolescent and parental perceptions of treatment helpfulness; (c) An exploration of the degree to which treatment compliance was predictive of future suicidal symptoms. For the purposes of this study non-compliance with psychosocial treatments was coded if the adolescent reported having dropped out of psychotherapy for reasons other than therapist recommendation or financial /insurance causes. Non-compliance with medication treatments was coded if the participant reported having taken the prescribed medicines rarely, only some of the time, or not at all.
METHOD
Participants
Data were gathered from 85 adolescent (62 females, 23 males) who were hospitalized immediately following a suicide attempt and at least one of their primary caregivers, as part of a larger prospective project examining risk factors associated with adolescent suicidal behavior. Families were recruited from among consecutive adolescent admissions to four private psychiatric hospitals in the mid-Atlantic region. While the number of adolescents recruited differed between hospitals (35, 22, 21, and 7 adolescents recruited from each of the four hospitals, respectively), participants did not differ in age (F [3, 80] = 1.595), gender (χ2 [3] = 2.75), or SES (F [3, 81] = 2.195) between the four hospitals. Moreover, adolescents did not significantly differ between hospitals in the presence of an externalizing (χ2 [3] = 3.609) or internalizing diagnosis (χ2 [3] = 5.292). Families were excluded if no parent or legal guardian resided in the extended metropolitan area or if the adolescent was mentally retarded, severely neurologically impaired, or psychotic and judged to be incapable of participating in the interview.
Participating adolescents and parents were assessed as soon as possible following the attempt (Time 1), and again at 6 months after the initial interview (Time 2), 12 months (Time 3), 18 months (Time 4), and 24 months (Time 5). The mean time between the index suicide attempt and Time 1 interview was 35.1 days (SD = 14.4). The mean times between interviews were: Time 1 to Time 2 = 6.4 months (SD = 2.0); Time 2 to Time 3 = 6.3 months (SD = 1.0); Time 3 to Time 4 = 6.2 months (SD = 1.6); and Time 4 to Time 5 = 6.4 months (SD = 1.8). At each time point (including Time 1), assessment focused on the preceding 6-month interval. At the time of the indexed suicide attempt, adolescents ranged in age from 13.3 to 18.7 years, with a mean age of 15.6 years (SD = 1.3). The adolescent sample was 89.4% Caucasian, 4.7% African-American, 3.5% Asian, and 2.4% Hispanic. Parents included 81 female caretakers and 51 male caretakers. Most (78.9%) were biological parents, but there were 11 stepfathers, 2 stepmothers, 8 adoptive fathers, 6 adoptive mothers, and 1 set of foster parents. Comparisons of non-biological versus biological parents revealed that only 2 of 24 tests were significant: non-biological fathers had more symptoms of alcohol abuse, and families with one or more non-biological caregivers were more satisfied with their children’s individual therapy at the 18-month follow-up. The socioeconomic levels, as measured by Hollingshead’s22 categories, for the highest scoring parent in each household were: professional (56.5%), technical (34.1%), craftsmen/clerical (3.5%), semiskilled (2.4%), and unskilled (3.5%).
Suicide attempts for this study were defined using O’Carroll and colleagues’ criteria23, i.e. self-injurious behavior for which there was at least minimal evidence—either implicit or explicit—of suicidal intent. Adolescents were qualified for participation in this study based on a rating of 2.0 on the 11-point Smith et al.24 Lethality of Attempt Scale, indicating that medical attention was at least warranted by the attempt, but might not have been necessary for survival (M=4.27, SD=2.07). The intraclass reliability coefficient for pairs of ratings was r=.88. Sixty-four participants (75%) attempted suicide by drug overdose, eight (9.4%) used a combination of an overdose and either self-cutting or alcohol poisoning, and thirteen (15.3%) utilized other methods including asphyxiation, jumping from a high place, gunshot, or stabbing.
Measures
Child and Adolescent Services Assessment.25
At each time point, adolescents were asked to report on each of 19 categories of mental health related services potentially received at any point in the previous 6 month period. They were further asked about the dates and duration of service and reasons for terminating each of the psychosocial treatments. Non-compliance for psychosocial treatment was assessed by responses of having terminated treatment for any reason other than “therapist recommended termination” (including mutual terminations) or “insurance/financial concerns;” the most common reasons were (a) decided not to go anymore (without elaborating on the decision), (b) did not find the treatment helpful, (c) did not like the therapist, and (d) logistical reasons such as the office being “too far out of the way.” Non-compliance with medication treatments was coded if the participant reported having taken the prescribed medicines rarely, only some of the time, or not at all.
Helpfulness of services received
in the previous 6-month period was assessed by asking adolescents and parents two open-ended questions: “Which services were helpful?” and “Which services weren’t all that helpful?” For purposes of analyses, those services rated as “helpful” were compared against all others (i.e., against services not specified as helpful).
Family History Interview.26
Parents’ current psychopathology was assessed with Cohen’s structured Family History Interview with both parents (when available). The measure yielded DSM-III-R27 symptom counts in parents for major depressive disorder, mania, generalized anxiety disorder, antisocial personality, as well as alcohol abuse and drug abuse. A variable indicating whether mothers or fathers met or exceeded the symptom threshold for one or more diagnoses was used in the analyses.
Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3), Youth and Parent Forms.28
At Time 1, Time 3, and Time 5, adolescents and their parents were interviewed separately with the DISC-2.3. Portions of the affective disorders (major depressive disorder, dysthymia, mania, hypomania, and bipolar disorder), anxiety disorders (generalized anxiety disorder), and disruptive behavior disorders (attention-deficit/hyperactivity disorder, oppositional defiant disorder, and conduct disorder) modules, as well as the module for alcohol, marijuana, and other substance abuse and dependence, were administered. These disorders were selected as they have been repeatedly linked to adolescent suicidal behavior.29 Parental reports of disruptive behavior disorders and adolescent reports of the other disorders were utilized as adolescents with disruptive behavior disorders are less likely to accurately report their symptoms.30
Suicidal ideation and suicide attempts
Adolescents’ level of suicidal ideation was evaluated at baseline and follow-ups with three items from the DISC-131 and three items from the DISC-2.328 assessing ideation over the past six months, which were summed to reach an ideation score. Wagner and Cohen32 used a similar measure which they found had acceptable reliability (alpha = .94) and validity. Adolescent reports of suicide attempts were assessed with the question, “In the past six months, have you tried to kill yourself?” Affirmative responses were followed by interviewer probes for the methods, the extent of injury, the circumstances, and the frequency. Self-mutilative behavior and behavior resulting in only superficial injury were excluded.
Design and Procedures
Hospital staff screened all new admissions to adolescent units and obtained written permission for telephone contact. The Primary Investigator telephoned eligible parents to describe the study and to schedule interviews. Parents’ written informed consent and adolescents’ assent were obtained for the protocol, which was approved by the Institutional Review Boards at the authors’ university and at each hospital site. Of the families contacted, 57% agreed to participate in the study. The demographics of those who refused to participate were roughly comparable to those who participated on mean age (participants = 15.6 years, refusals =15.2), gender (participants = 73% females, refusals = 67% female), and race (participants = 89% Caucasian, refusals = 80% Caucasian). At 6 months follow-up, 76.5% of the original adolescents and 86.4% of the parents were interviewed, while 70.6% of the adolescents and 78.8% of the parents were retained at 12 months. At 18 months, 68.2% of the adolescents and 72.7% of the parents were interviewed, and at 2 years, 56.5% of the adolescents and 53.8% of the parents were retained. These rates are comparable to those reported by other investigators of prospective studies of adolescent suicide attempters.33–35 T-tests were run comparing dropouts versus non-dropouts at each time point on the baseline family observation variables; only 1 of 24 comparisons was significant, indicating that the retained sample was not biased on the central variables of interest.
Data Analysis
Discrete-time survival analyses36 were run to test for the relationship between adolescent and parent psychopathology, as well as helpfulness ratings, on the probability of non-compliance with a given treatment across the full follow-up period. For psychotherapy, the dates of treatment were used to create data points at each 3-month interval, yielding 7 data points (data from 21 months after the attempt were not used since no adolescents were noncompliant with individual psychotherapy during the three preceding months). For medication, the dating of noncompliance was insufficiently detailed to reliably examine 3-month intervals; thus, 6-month intervals were examined. A latent variable approach to discrete-time survival analyses (DTSA) was performed using Mplus V. 4.21,37,38 and the EM algorithm was used to impute missing data for the covariates (predictors). In preliminary correlational analyses, age at attempt, gender, and family socioeconomic status (SES) were examined for associations with each of the dependent variables of treatment compliance. Since only age at attempt was associated with some of the dependent variables (older age was associated with poorer compliance), it alone was included as a covariate in all subsequent analyses of prediction of the hazard for non-compliance. The proportionality assumption for the regression of the hazard on the various covariates (i.e., the assumption that the influence of the covariates on the hazard was comparable across the time points) was tested prior to conducting all analyses. Results indicated that proportionality could be assumed in all instances except for the prediction of medication compliance from adolescent psychopathology, where a non-proportional model was necessary. Also for medication, a linear hazard model fit the data well, and was used; the hazards were not similarly constrained in the models for psychotherapy conditions.
RESULTS
Descriptive Analyses
All treatments received at any point in the six months prior to each follow-up are noted in Table 1. Individual psychotherapy was the most commonly received form of treatment with pharmacotherapy treatment only slightly less common throughout the 2 years of follow-up. Medications prescribed at T1 were (number of adolescents prescribed medication; percentage): Antidepressants (N=32; 37.6%), Mood Stabilizers (N=14; 16.5%), Antipsychotics (N=5; 5.9%), Stimulants (N=3; 3.5%), and Anti-Parkinsonian (N=1; 1.2%). A sizable percentage of adolescents utilized school counselors and psychologist, in addition to family and group therapies. In general, the percentages of adolescents receiving any services dropped across time.
Table 1.
Numbers (Percentages) of Adolescents Receiving Services at Least Once in the Six Months Prior to Each Time Point
| Time 1 (n=85) | Time 2 (n=81) | Time 3 (n=71) | Time 4 (n=73) | Time 5 (n=60) | |
|---|---|---|---|---|---|
| Type of Service | N (%) | N (%) | N (%) | N (%) | N (%) |
| Pharmacotherapy | 50 (58.8%) | 69 (85.2%) | 48 (67.6%) | 31 (42.5%) | 28 (46.7%) |
| Individual Psychotherapy | 71 (83.5%) | 74 (91.4%) | 51 (71.8%) | 33 (45.2%) | 28 (46.7%) |
| Family Therapy | 61 (71.8%) | 55 (67.9%) | 34 (47.9%) | 22 (30.1%) | 13 (21.7%) |
| Group Therapy | 18 (23.4%) | 25 (31.3%) | 15 (21.1%) | 12 (16.4%) | 7 (11.7%) |
| Psychiatric hospital | 22 (25.9%) | 12 (14.8%) | 14 (19.7%) | 5 (6.8%) | 4 (6.7%) |
| Residential treatment | 4 (4.7%) | 9 (11.1%) | 6 (8.5%) | 7 (9.6%) | 4 (6.7%) |
| Day hospital | 18 (21.2%) | 19 (23.5%) | 5 (7.0%) | 3 (4.1%) | 4 (6.7%) |
| Inpatient substance | 3 (3.5%) | 5 (6.2%) | 3 (4.2%) | 0 (0.0%) | 0 (0.0%) |
| Outpatient substance | 5 (5.9%) | 7 (8.6%) | 5 (7.0%) | 5 (6.8%) | 4 (6.7%) |
| Emergency shelter | 1 (1.2%) | 2 (2.5%) | 2 (2.8%) | 1 (1.4%) | 1 (1.7%) |
| Crisis center | 5 (5.9%) | 3 (3.8%) | 1 (1.4%) | 2 (2.7%) | 0 (0.0%) |
| In-home counseling | 3 (3.5%) | 3 (3.8%) | 2 (2.8%) | 3 (4.1%) | 0 (0.0%) |
| Social Services | 9 (10.6%) | 7 (8.6%) | 3 (4.2%) | 5 (6.8%) | 2 (3.3%) |
| School Guidance Counselor/Psychologist |
44 (52.4%) | 24 (29.6%) | 19 (27.1%) | 17 (23.3%) | 10 (16.7%) |
| Family doctor | 8 (9.4%) | 8 (9.9%) | 2 (2.8%) | 4 (5.5%) | 2 (3.3%) |
| Self-help group | 12 (14.1%) | 15 (18.5%) | 13 (18.3%) | 16 (22.2%) | 14 (23.7%) |
| Crisis hotline | 12 (14.1%) | 1 (1.2%) | 2 (2.8%) | 3 (4.1%) | 2 (3.3%) |
| Minister/Rabbi/etc. | 7 (8.2%) | 5 (6.2%) | 4 (5.6%) | 1 (1.4%) | 1 (1.7%) |
| Healers | 2 (2.4%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
The two most commonly reported mental health services, individual psychotherapy and pharmacotherapy, were examined in subsequent analyses. Adolescent and parent ratings of the helpfulness of these two treatments are presented in Table 2.
Table 2.
Adolescent and Parent Ratings of Treatment Helpfulness: Numbers (Percentages) among Participants who Received Each Form of Treatment, Time 2–5
| Time 2: N (%) | Time 3: N (%) | Time 4: N (%) | Time 5: N (%) | |
|---|---|---|---|---|
| Individual Psychotherapy | ||||
| Adolescent Ratings | ||||
| Rated as Helpful | 30 (48.4%) | 25 (58.1%) | 18 (66.7%) | 11 (47.8%) |
| Not Rated as Helpful | 32 (51.6%) | 18 (41.9%) | 9 (33.3%) | 12 (52.2%) |
| Parent Ratings | ||||
| Rated as Helpful | 41 (60.3%) | 30 (58.8%) | 20 (52.6%) | 14 (45.2%) |
| Not Rated as Helpful | 27 (39.7%) | 21 (41.1%) | 18 (47.4%) | 17 (54.8%) |
| Pharmacotherapy | ||||
| Adolescent Ratings | ||||
| Rated as Helpful | 14 (23.7%) | 16 (39.0%) | 9 (37.5%) | 12 (54.5%) |
| Not Rated as Helpful | 45 (76.3%) | 25 (61.0%) | 15 (62.5%) | 10 (45.5%) |
| Parent Ratings | ||||
| Rated as Helpful | 14 (21.5%) | 17 (34.7%) | 15 (44.1%) | 12 (41.4%) |
| Not Rated as Helpful | 51 (78.5%) | 32 (65.3%) | 19 (55.9%) | 17 (58.6%) |
The percentages of participants who were non-compliant with individual psychotherapy and pharmacotherapy were assessed at each time point. Rates of non-compliance at each time point are noncumulative, and are independent of one another, as non-compliant participants could return to treatment in a compliant fashion at later time points. Non-compliance rates for individual psychotherapy for each time point were: 17.6% (T2), 21.6% (T3), 18.2% (T4), and 35.7% (T5). For pharmacotherapies the rates were 25.0% (T2), 27.7% (T3), 19.4% (T4), and 11.1% (T5). Over the course of the 2-year follow-up, 57.7% of participants were non-compliant at some point with individual psychotherapy and 41.3% were non-compliant with medications.
Sixteen adolescents (18.8%) reported making at least one repeat suicide attempt during the 2-year follow-up period, comprised of 13 of the 62 (21%) females and 3 of the 23 (13%) males in the study. There were no significant differences in rates of repeated suicide attempt by gender, age at index attempt, or family socio-economic status. The numbers of adolescents who reported making their first repeated attempt at each time point were 11 at the initial 6-month (T2) period, 4 at T3, 0 at T4, and 1 at T5. Of the 16 adolescents who reported suicidal behavior during the 2-year follow-up, 7 made multiple attempts.
Adolescent Variables and Treatment Compliance
Adolescent baseline psychopathology
At baseline (T1), adolescents met criteria for the following psychiatric DISC diagnoses: Major Depressive Disorder (N=47, 57.3%), Dysthymia (N=39, 47.6%), Bipolar Disorder (N=5, 6.1%), Generalized Anxiety Disorder (N=20, 24.1%), Conduct Disorder (N=23, 27.1%), Oppositional Defiant Disorder (N=27, 31.8%), Attention Deficit/Hyperactivity Disorder (N=10, 11.8%), Substance Dependence (N=20, 23.5%), Marijuana Dependence (N=22, 25.9%), Alcohol Dependence (N=19, 22.4%). Adolescents’ diagnoses were grouped to form broadband binary diagnosis variables of any affective or anxiety disorder (major depressive disorder, dysthymia, bipolar disorder, generalized anxiety disorder) and any disruptive behavior disorder (conduct disorder, oppositional defiant disorder, attention-deficit/hyperactivity disorder). Fifty-two (61.2%) adolescents had one or more affective/ anxiety diagnosis and 36 (42.4%) adolescents had one or more disruptive behavior diagnosis. Twenty-eight (32.9%) adolescents had both affective/anxiety and disruptive behavior diagnoses, while 32 (37.7%) adolescents had no diagnosis within either affective/anxiety or disruptive behavior categories.
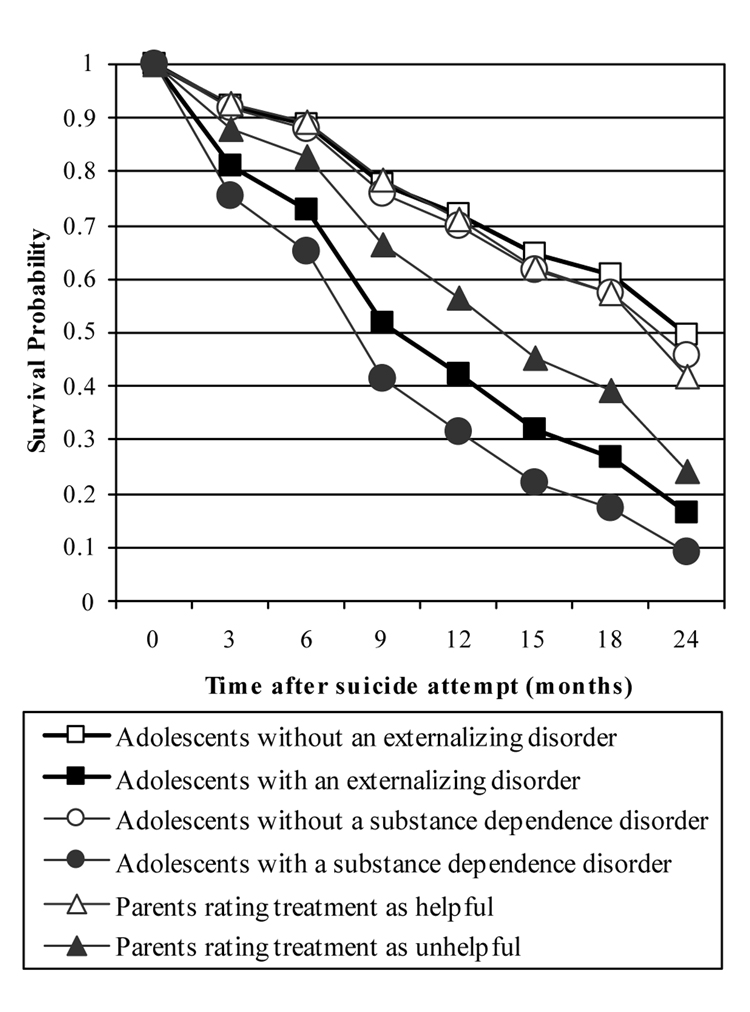
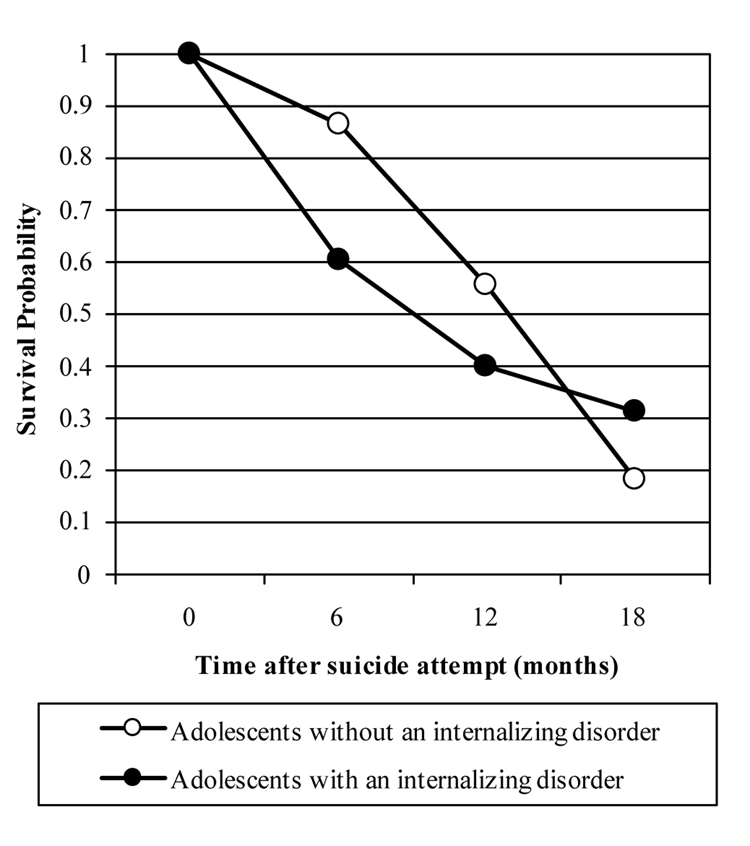
Discrete Time Survival Analyses (DTSA) were run to analyze the effects of adolescent affective/anxiety as well as disruptive disorders on the probability of treatment compliance for individual psychotherapy and pharmacotherapy. The results of the regression of the survival function on the predictor variables indicated that having a disruptive behavior diagnosis at baseline was predictive of an increased risk of non-compliance with individual psychotherapy as compared to adolescents with no disruptive behavior diagnosis (β = 1.045, S.E. = 0.382, p < .01). Survival plots for adolescents with and without a disruptive behavior disorder are shown in Figure 1 for individual psychotherapy. When the hazard analyses were run for medication non-compliance, adolescents with an affective/anxiety diagnosis at baseline, as compared to all other adolescents in the sample, were at increased risk of medication non-compliance at the 6-month follow-up (β = 1.451, S.E..= 0.715, p < .05), but not at later time points (see Figure 2 for plots of survival curves).
Fig. 1.
Survival plots comparing the cumulative probability of remaining compliant with individual psychotherapy by month for each of the significant dichotomous independent variables.
Fig. 2.
Survival plots comparing the cumulative probability of remaining compliant with pharmacotherapy by month for each of the significant dichotomous independent variables.
DTSA analyses were also conducted examining the associations of dependence on alcohol, marijuana, or other substances with non-compliance with individual therapy and pharmacotherapy. Neither alcohol nor marijuana dependence were predictive of non-compliance with either form of treatment. However, the regression of the survival function for non-compliance with individual therapy on dependence on other substances yielded a significant effect, (β = 1.274, S.E. = 0.405, p < .01), indicating that suicidal youths with a substance dependence disorder were quicker to drop out of individual therapy, as shown in Figure 1.
Adolescent rating of treatment helpfulness
DTSA were run to test for influence of adolescents’ ratings of helpfulness of individual psychotherapy or pharmacotherapy on the probability of non-compliance with that treatment. None of these survival analyses yielded significant results, indicating that adolescents’ helpfulness ratings for a given therapy did not predict how long they complied with that therapy.
Parent Variables and Treatment Compliance
Parental psychopathology
DTSA analyses were run to examine whether a history of one or more disorders in mothers or fathers was predictive of adolescent compliance with individual psychotherapy or pharmacotherapy. None of the analyses were significant.
Parental rating of treatment helpfulness
Parental ratings of their children’s individual psychotherapy as helpful were significant predictors of a lower risk of adolescents’ non-compliance with individual psychotherapy over the course of the study (β = −0.551, S.E. = 0.244, p < .05), as illustrated in Figure 1, but not of pharmacotherapy.
Treatment Compliance and Suicidality
Suicide re-attempts
Due to the small number of repeated attempts, DTSA could not be utilized in analyzing the effects of treatment compliance on suicidality. Instead Chi- square analyses were run to examine associations between treatment compliance and repeated suicide attempts, at any time during the follow-up. There were no significant findings.
Suicidal ideation
Regression analyses were run in order to determine if compliance with either individual psychotherapy or medications was predictive of change in suicidal ideation between 6-month follow-ups. Analyses tested the relationship between treatment compliance at each time point and suicidal ideation at the immediately succeeding time point, while controlling for ideation at the previous time point. Preliminary analyses indicated that age at T1, gender, and family socioeconomic status (SES) were not correlated with suicidal ideation at T2, T3, T4, or T5; therefore these variables were not covaried in the regression analyses. Of the regression analyses run, only compliance with pharmacotherapy at T4 predicted decreased suicidal ideation at T5 (F [1, 12] = 6.395, p < .05) after controlling for suicidal ideation at T4.
DISCUSSION
The findings indicate that, in the aftermath of a suicide attempt, adolescents are typically engaged in a variety of psychological services, particularly both psychosocial and pharmacotherapy treatments. Parents’ perception of the helpfulness of treatment was predictive of increased compliance, while increased child psychopathology predicted noncompliance, with disruptive disorders predicting psychotherapy noncompliance and affective/anxiety disorders predicting pharmacotherapy noncompliance (at 6 months follow-up).
Service utilization and compliance
Reports indicated that adolescents’ involvement in the most frequently used forms of treatment dropped off progressively at each 6-month follow-up after the suicide attempt. The most notable drops in treatment usage occurred between six and eighteen months after the initial attempt, which may represent the varying end-points of a critical stage after the attempt, at which point therapists, adolescents, and their families note enough improvement to terminate treatment. In examining the different forms of services accessed, it is interesting to note that, beyond the expected high usage of individual psychotherapy and medications, there was a relatively high prevalence of the utilization of school psychologists and guidance counselors, both before (52.4% of the sample) and after (26.9% of the sample) suicide attempts. This finding is heartening in light of studies demonstrating the effectiveness of school-based interventions for suicidal adolescents, which often focus on improving students’ personal and social support resources, increasing self-esteem, and reducing suicidal behaviors.39 Moreover, it may be that ease of access to services in a school-based setting improves the likelihood of engaging in those services. The possibility that such is the case for suicidal adolescents may be worth considering in determining the allocation of resources.
Non-compliance rates for pharmacotherapy tapered off over the course of the follow-up, suggesting that those who continued on medications for extended periods were likely to be compliant. Compliance rates for psychotherapy were stable across time with the exception of greater non-compliance after two years. The overall non-compliance rate of roughly 60% for psychotherapy and 40% for pharmacotherapy are similar to those previously reported in the literature,40 although the 2-year follow-up utilized in this study extends what has been previously investigated.
Relationship of Individual and Parental Factors to Treatment Compliance
Adolescent baseline psychopathology
Diagnoses of disruptive behavior disorders and substance dependence other than alcohol or marijuana predicted increased non-compliance with individual psychotherapy, while affective/anxiety disorder diagnoses predicted increased non-compliance with medications at six-months. Considering the implications of these findings, suicidal adolescents with disruptive behavior disorders may be less likely to actively engage in psychosocial therapy, be more guarded, and therefore withdraw more quickly from treatment.41 Adolescents with internalizing disorders, on the other hand, may find it hard to muster the self-discipline that is necessary to comply with medication regimens, which occur on a daily basis (or multiple times a day) and may involve less parental facilitation and monitoring than attendance at psychotherapy sessions. Adolescents with substance dependence disorders are notoriously difficult to sustain in treatment.42 In this sample, 79% of suicidal adolescents meeting diagnostic criteria for substance dependence also met criteria for either alcohol or marijuana dependence. Thus, suicidal adolescents with an alcohol or marijuana dependence who are also dependent on one or more other substances (i.e. polysubstance abusers) may be among the most difficult to engage in treatment. Given the strong links between substance abuse and adolescent suicidal behavior43—particularly when substance abuse is comorbid with other psychiatric disorders—devising ways to improve the treatment compliance of suicidal youth with substance disorders in treatment is of paramount importance.
Parental psychopathology
Very few investigators have examined the influence of parental psychopathology on treatment compliance among adolescents who attempt, despite the possibility that parents with psychopathology may have more difficulties providing the structure and organization to ensure offspring’s compliance with treatment regimes, or may be less inclined to trust or support the treatment providers10 The present findings indicate that a history of one or more disorders in mothers or fathers was unrelated to offspring’s noncompliance. That contrasts with previous reports by King and associates of poorer treatment follow-through among adolescents whose mothers reported greater current or recent symptoms of depression, hostility, or paranoia. In the present study, parents reported on lifetime histories of psychopathology, which may explain the contrasting findings—i.e., a history of previous psychopathology may be less relevant to offspring compliance than current psychopathology.
Ratings of treatment helpfulness
One particular contribution of this study was the assessment of adolescent and parent ratings of helpfulness for each form of treatment, and the examination of the relationship between helpfulness ratings and treatment compliance. A review of the literature found no previous studies which explicitly examined this construct, even though researchers have attempted to increase treatment compliance with interventions directed at improving the perceptions of treatment efficacy.44 Several trends in helpfulness ratings became clear from the study. First, individual therapy was more likely to be mentioned as helpful as compared to pharmaceutical treatments and was the only form of treatment rated as helpful by a plurality of both adolescents and parents at each time point. Second, for both forms of therapy at each time point except one, parents were more likely than adolescents to rate the treatment as helpful. Parents may be in a better position to perceive positive changes in their adolescents, as compared to adolescents’ self-assessments, or they may be more willing than the adolescent to give credit—or at least the benefit of the doubt—to treatment.
Parental ratings of individual psychotherapy as helpful were a significant predictor of decreased drop-out from individual therapy over the course of the study. Although no previous literature was found that specifically examined the importance of parental helpfulness ratings of ongoing treatments (i.e., during the course of treatment), these findings are in line with Kazdin and Wassell’s study45 linking negative parental expectations about treatment with their children’s later non-compliance with individual psychotherapy. In contrast, adolescent ratings of treatment helpfulness were not predictive of treatment compliance. It is possible that parental evaluations of treatment have greater significance in predicting non-compliance because the parents play a crucial role in arranging, transporting, and paying for treatment. When they view treatment as helpful, they may have greater motivation to facilitate treatment compliance.
Relationship of Treatment Compliance to Suicidal Ideation and Re-attempts
No statistically significant results were found for predictions of re-attempts based on treatment noncompliance. Compliance also failed to predict future suicidal ideation when level of ideation at the previous time point was controlled. This suggests that compliance with treatment may not be a significant predictor of re-attempts or changes in suicidal ideation. This seems to be at odds with previous studies that have indicated an association between failure to receive treatment and repeated suicidal gestures and ideation.18 It is possible that suicidal symptoms may be too narrow of an outcome variable, and that a wider variety of psychopathology may be a more appropriate measure of the effect of treatment compliance in the aftermath of a suicide attempt. Alternatively, it is possible that for some adolescents as long as a certain minimal “dose” of treatment is received, the impact of noncompliance on longer term suicidal outcomes may be relatively unimportant, while for others continued compliance with treatment may represent a greater severity of symptoms, including greater suicidal behavior. There also is the possibility that treatment with antidepressant medications may have actually triggered suicidal symptoms in certain adolescents.46
This study is limited in several ways. The recruitment and attrition rates, although comparable to those reported in previous studies of similar populations,33–35 limits the confidence with which we can extrapolate from the findings to the population of adolescents at the private psychiatric hospitals, and reduced the statistical power of the study. Also, since the present study was limited to a sample of adolescents in private inpatient psychiatric units, the results may not be applicable to adolescents from outpatient, residential, or public hospital settings. The large proportion of Caucasian female adolescents, and this sample’s higher than average socioeconomic status, may limit the generalizability of the findings, as well. The inclusion of non-biologically related caretakers (e.g. adoptive, stepparents) in the sample may have led to somewhat systematic biases or inaccurate responses due to histories and perspectives that may contrast with those of biological parents, although very few such distinctions were statistically detected. Additionally, large portions of the data were based on self- report measures, which introduces the possibility of recall bias or dishonest responding that would threaten the validity of the data.
Among the noteworthy findings is that adolescents were less likely to drop out of individual therapy if their parents perceived it as relatively helpful. This implies that it may be very important for clinicians to maintain communication with parents in order to address any concerns that parents have about the therapy. Such factors as whether the parents perceive improvement in the adolescent, whether parents believe their own concerns are being addressed, and whether the parent feels respected or understood by the therapist may all contribute to parents’ decisions to continue their child's treatment. Strategies found to be successful in increasing parental involvement and treatment compliance in child-focused therapy include the use of motivational enhancement techniques, attention to treatment participation barriers, pretreatment preparatory interviews and videotapes, increased outreach and reminder calls, and attendance to parents’ adult issues.47–48 The findings also suggest how critical it may be to successfully engage suicidal youth who have a disruptive behavior disorder or a substance dependence disorder. Such youth are notoriously difficult to engage and retain in psychotherapy, and building an alliance with them should be a primary agenda of the early stages of treatment. Finally, the finding that a very sizeable subset of suicidal youths speak to either school psychologists or guidance counselors both preceding the suicide attempt and in the months and years that follow the attempt indicate the importance of training such personnel in suicide risk assessment, and establishing open lines of communication between school providers and other mental health providers as well as parents.
Acknowledgments
This research was supported by a grant from the National Institute of Health awarded to Dr. Wagner (MH51342).
Footnotes
Disclosure: The authors report no conflicts of interest
Contributor Information
Craig D. Burns, University Counseling Services, Boston College, Chestnut Hill, MA.
Ranon Cortell, Department of Psychology, The Catholic University of America, Washington, DC.
Barry M. Wagner, Department of Psychology, The Catholic University of America, Washington, DC.
References
- 1.Rudd MD, Joiner TE, Rajab MH. Relationships among suicide ideators, attempters, and multiple attempters in a young-adult sample. J Abnorm Psychol. 1996;105:541–550. doi: 10.1037//0021-843x.105.4.541. [DOI] [PubMed] [Google Scholar]
- 2.Spirito A, Boergers J, Donaldson D. Adolescent suicide attempters: post-attempt course and implications for treatment. Clin Psychol Psychotherapy. 2000;7:161–173. [Google Scholar]
- 3.King CA, Segal H, Kaminski K, Naylor MW, Ghaziuddin N, Radpour L. A prospective study of adolescent suicidal behavior following hospitalization. Suicide Life Threat Behav. 1995;25:327–338. [PubMed] [Google Scholar]
- 4.Shaffer D, Piacentini J. Suicide and attempted suicide. In: Rutter M, Taylor E, editors. Child Psychiatry: Modern Approaches. 3rd ed. Oxford, England: Blackwell Scientific Publication; 1994. pp. 407–424. [Google Scholar]
- 5.Spirito A, Valeri S, Boergers J, Donaldson D. Predictors of continued suicidal behavior in adolescents following a suicide attempt. J Clin Child Adolesc Psychol. 2003;32:284–289. doi: 10.1207/S15374424JCCP3202_14. [DOI] [PubMed] [Google Scholar]
- 6.Donaldson D, Spirito A, Esposito-Smythers C. Treatment for adolescents following a suicide attempt: Results of a pilot trial. J Am Acad Child Adolesc Psychiatry. 2005;44:113–120. doi: 10.1097/00004583-200502000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Katz LY, Cox BC, Gunasekara S, Miller AL. Feasibility of dialectical behavior therapy for suicidal adolescent inpatients. J Am Acad Child Adolesc Psychiatry. 2004;43:276–282. doi: 10.1097/00004583-200403000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Harrington R, Kerfoot M, Dyer E, et al. Randomized trial of a home based intervention for children who have deliberately poisoned themselves. J Am Acad Child Adolesc Psychiatry. 1998;37:512–519. [PubMed] [Google Scholar]
- 9.Costello EJ, Burns BJ, Angold A, Leaf PJ. How can epidemiology improve mental health services for children and adolescents? J Am Acad Child Adolesc Psychiatry. 1993;32:1106–1114. doi: 10.1097/00004583-199311000-00002. [DOI] [PubMed] [Google Scholar]
- 10.King CA, Hovey JD, Brand E, Wilson R, Ghaziuddin N. Suicidal adolescents after hospitalization: parent and family impacts on treatment follow-through. J Am Acad Child Adolesc Psychiatry. 1997;36:85–93. doi: 10.1097/00004583-199701000-00021. [DOI] [PubMed] [Google Scholar]
- 11.Litt IF, Cuskey WR, Rudd S. Emergency room evaluation of the adolescent who attempts suicide: compliance with follow-up. J Adolesc Health Care. 1983;4:106–108. doi: 10.1016/s0197-0070(83)80028-x. [DOI] [PubMed] [Google Scholar]
- 12.Taylor EA, Stansfield SA. Children who poison themselves II: prediction of attendance for treatment. Br J Psychiatr. 1984;145:132–136. doi: 10.1192/bjp.145.2.132. [DOI] [PubMed] [Google Scholar]
- 13.Trautman PD, Stewart N, Morishima A. Are adolescent suicide attempters non-compliant with outpatient care? J Am Acad Child Adolesc Psychiatry. 1993;32:89–94. doi: 10.1097/00004583-199301000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Granboulan V, Roudot-Thoraval F, Lemerle S, Alvin P. Predictive factors of post-discharge follow-up care among adolescent suicide attempters. Acta Psychiatr Scad. 2001;104:31–36. doi: 10.1034/j.1600-0447.2001.00297.x. [DOI] [PubMed] [Google Scholar]
- 15.Piacentini J, Rotheram-Borus MJ, Gillis JR, et al. Demographic predictors of treatment adherence among adolescent suicide attempters. J Consult Clin Psych. 1995;63:469–473. doi: 10.1037//0022-006x.63.3.469. [DOI] [PubMed] [Google Scholar]
- 16.Spirito A, Plummer B, Gispert M, et al. Adolescent suicide attempts: outcomes at follow-up. Am J Orthopsychiatry. 1992;62:464–468. doi: 10.1037/h0079362. [DOI] [PubMed] [Google Scholar]
- 17.Pillay AL, Wassenaar DR. Psychosocial intervention, spontaneous remission, hopelessness, and psychiatric disturbance in adolescent parasuicides. Suicide Life Threat Behav. 1995;25:386–392. [PubMed] [Google Scholar]
- 18.Rotheram-Borus MJ, Piacentini J, Cantwell C, Song J. The 18-month impact of an emergency room intervention for adolescent female suicide attempters. J Consult Clin Psych. 2000;68:1081–1093. doi: 10.1037//0022-006x.68.6.1081. [DOI] [PubMed] [Google Scholar]
- 19.Callor WB, Petersen E, Gray D, Grey T, Lamoreaux T, Bennett PJ. Preliminary findings of noncompliance with psychotropic medication and prevalence of methamphetamine intoxication associated with suicide completion. Crisis. 2005;26:78–84. doi: 10.1027/0227-5910.26.2.78. [DOI] [PubMed] [Google Scholar]
- 20.Haw C, Houston K, Townsend E, Hawton K. Deliberate self-harm patients with depressive disorders: treatment and outcome. J Affect Disord. 2002;70:57–65. doi: 10.1016/s0165-0327(01)00317-2. [DOI] [PubMed] [Google Scholar]
- 21.Rotheram-Borus MJ, Piacentini J, Van Rossem R, et al. Treatment adherence among Latina female adolescent suicide attempters. Suicide Life Threat Behav. 1999;29:319–331. [PubMed] [Google Scholar]
- 22.Hollingshead AB. Four factors index of social status. New Haven, CT: Yale University Department of Sociology; 1975. [Google Scholar]
- 23.O’Carroll PW, Berman A, Maris RW, Moscicki EK. Beyond the tower of babel: a nomenclature for suicidology. Suicide Life Threat Behav. 1996;26:237–252. [PubMed] [Google Scholar]
- 24.Smith K, Conroy RW, Ehler BD. Lethality of suicide attempt rating scale. Suicide Life Threat Behav. 1984;14:215–242. doi: 10.1111/j.1943-278x.1984.tb00678.x. [DOI] [PubMed] [Google Scholar]
- 25.Asher BH, Farmer E, Burns BJ, Angold A. The child adolescent services assessment (CASA): Description and psychometrics. J Emot Beh Dis. 1996;4:12–20. [Google Scholar]
- 26.Cohen P. Family History Interview. New York: New York State Psychiatric Clinic; 1990. [Google Scholar]
- 27.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd edition - revised. Washington, DC: Author; 1987. [Google Scholar]
- 28.Shaffer D, Fisher P, Piacentini J, Schwab-Stone M, Wicks J. Diagnostic Interview Schedule for Children – Version 2.3. New York: New York State Psychiatric Institute; 1992. [Google Scholar]
- 29.Brent DA, Kalas R, Edelbrock C, Costello AJ, Dulcan MK, Conover M. Psychopathology and its relationship to suicidal ideation in childhood and adolescence. J Am Acad Child Adolesc Psychiatry. 1986;25:666–673. doi: 10.1016/s0002-7138(09)60292-2. [DOI] [PubMed] [Google Scholar]
- 30.Jensen PS, Rubio-Stypec M, Canino G, et al. Parent and child contributions to diagnosis of mental disorder: are both informants always necessary? J Am Acad Child Adolesc Psychiatry. 1999;38:1569–1579. doi: 10.1097/00004583-199912000-00019. [DOI] [PubMed] [Google Scholar]
- 31.Costello EJ, Edelbrock CS, Costello AJ. Validity of NIMH Diagnostic Interview Schedule for Children: a comparison between psychiatric and pediatric referrals. J Abnorm Child Psychol. 1985;13:579–595. doi: 10.1007/BF00923143. [DOI] [PubMed] [Google Scholar]
- 32.Wagner BM, Cohen P. Adolescent sibling differences in suicidal symptoms: the role of parent-child relationships. J Abnorm Child Psychol. 1994;22:321–337. doi: 10.1007/BF02168077. [DOI] [PubMed] [Google Scholar]
- 33.Rudd MD, Joiner TE, Rajab MH. Help negotiation after acute suicidal crisis. J Consult Clin Psych. 1995;63:499–503. doi: 10.1037//0022-006x.63.3.499. [DOI] [PubMed] [Google Scholar]
- 34.Brent DA, Kolko DJ, Wartella ME, et al. Adolescent psychiatric inpatients’ risk of suicide attempt at 6-month follow-up. J Am Acad Child Adolesc Psychiatry. 1993;32:95–105. doi: 10.1097/00004583-199301000-00015. [DOI] [PubMed] [Google Scholar]
- 35.Nardini-Maillard D, Ladmane FG. The results of a follow-up study of suicidal adolescents. J Adolesc. 1980;3:253–260. doi: 10.1016/s0140-1971(80)80058-3. [DOI] [PubMed] [Google Scholar]
- 36.Singer J, Willett J. It’s about time: using discrete-time survival analysis to study duration and the timing of events. J Educ Stat. 1993;18:155–195. [Google Scholar]
- 37.Muthen LK, Muthen BO. Mplus V. 4. Los Angeles: Muthen & Muthen; 2006. [Google Scholar]
- 38.Muthen B, Masyn K. Discrete-time survival mixture analysis. J Educ Beh Stat. 2005;13:27–58. [Google Scholar]
- 39.Thompson EA, Eggert LL, Randell BP, Pike KC. Evaluation of indicated suicide-risk prevention approaches for potential high school dropouts. Am J Public Health. 2001;91:742–752. doi: 10.2105/ajph.91.5.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ghaziuddin N, King CA, Hovey JD, Zaccagnini J, Ghaziuddin M. Medication non-compliance in adolescents with psychiatric disorders. Child Psychiatry Hum Dev. 1999;30:103–110. doi: 10.1023/a:1021950301932. [DOI] [PubMed] [Google Scholar]
- 41.Kazdin AE, Mazurick JL, Bass D. Risk for attrition in treatment of antisocial children and families. J Clin Child Psych. 1993;22:2–16. [Google Scholar]
- 42.Substance Abuse and Mental Health Services Administration, Office of Applied Studies. [Accessed February 2, 2008];Trends in rates of treatment completion. 2008 http://www.oas.samsha.gov/txtrends.htm.
- 43.Fleischmann A, Bertolote JM, Belfer M, Beautrais A. Completed suicide and psychiatric diagnosis in young people: A critical examination of the evidence. Am J Orthopsychiatry. 2005;75:676–683. doi: 10.1037/0002-9432.75.4.676. [DOI] [PubMed] [Google Scholar]
- 44.Spirito A, Boergers J, Donaldson D, Bishop D, Lewander W. An intervention trial to improve adherence to community treatment by adolescents after a suicide attempt. J Am Acad Child Adolesc Psychiatry. 2002;41:435–442. doi: 10.1097/00004583-200204000-00016. [DOI] [PubMed] [Google Scholar]
- 45.Kazdin AE, Wassell G. Barriers to treatment participation and therapeutic change among children referred for conduct disorder. J Clin Child Psych. 1999;28:160–172. doi: 10.1207/s15374424jccp2802_4. [DOI] [PubMed] [Google Scholar]
- 46.Bridge JA, Ivengar S, Salary CB, et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: A meta-analysis of randomized controlled trials. JAMA. 2007;297:1683–1696. doi: 10.1001/jama.297.15.1683. [DOI] [PubMed] [Google Scholar]
- 47.Nock MK, Ferriter C. Parent management of attendance and adherence in child and adolescent therapy: A conceptual and empirical review. Clin Child Fam Psych Rev. 2005;8:149–166. doi: 10.1007/s10567-005-4753-0. [DOI] [PubMed] [Google Scholar]
- 48.Nock MK, Kazdin AE. randomized controlled trial of a brief intervention for increasing participation in parent management training. J Consult Clin Psych. 2005;73:872–879. doi: 10.1037/0022-006X.73.5.872. [DOI] [PubMed] [Google Scholar]