Abstract
Introduction
The purpose of this study, conducted in a multiethnic population in Hawaii, was to estimate the prevalence of breastfeeding at six months of age, exclusive and otherwise, as well as to identify positively and negatively associated factors.
Methods
A content-valid survey was conducted among a random stratified sample, and a printed questionnaire was sent to mothers of infants aged 7–10 months. A response rate of 70% yielded 701 completed surveys.
Results
At six months after birth, some breastfeeding was practiced by 54% of respondents. The rate of exclusive breastfeeding was ≈16% at six months. Race and ethnicity assessment showed that Whites had the highest rates and Filipinos the lowest. Formula use in the hospital was most significantly associated with lower breastfeeding rates at six months.
Conclusions
Exclusive breastfeeding for six months, even in a state with extremely high initiation rates, is seldom achieved. Formula use in the maternity units should be reduced, and intensive targeted study and education of the Filipino community should be undertaken.
Keywords: Breastfeeding, Exclusive, Prevalence, Racial, Ethnic, Formula Feeding
Introduction
Increasing the prevalence of breastfeeding is recognized as a key means of improving the health outcomes of infants.1–6 The United States lags behind many developed nations in breastfeeding protection, promotion, and support. In 1990, Healthy People 2000 objectives, with a stated goal of reducing disparities, included breastfeeding as one of the parameters to be monitored. Those goals were not met, and for 2010, they were repeated with an extension added to encourage a longer duration of breastfeeding. In 2005, the American Academy of Pediatrics5 reissued its policy statement, originally published in 1997, on “Breastfeeding and the Use of Human Milk.” In this updated version, the major change was the emphasis on exclusive breastfeeding (EBF) for the first six months of life—the “gold standard.” In 2006, a midterm adjustment was added to Healthy People goals that specified the percentages of infants who should still be exclusively breastfed at 3 months (60%) and 6 months (25%) of age, in addition to the previously stated goals for any breastfeeding at 6 months (50%) and at 12 months (25%). Several studies3–5 had suggested that a greater intensity breastfeeding may be accompanied by more positive health outcomes. Notably, Raisler6 demonstrated a dose/response relationship between exclusive and predominant breastfeeding, as opposed to little or no breastfeeding, and reduced gastrointestinal and respiratory illnesses, including otitis media, and illness-related office visits in general.
Early data on breastfeeding in Hawaii, as for the rest of the nation, came from the Ross Laboratories Mothers Surveys7 (by manufacturers of infant formula) They reported relatively highrates of breastfeeding initiation in Hawaii, with rapid decline after hospital discharge. Since 2002, the Centers for Disease Control and Prevention (CDC) National Immunization Survey8 has also included information about breastfeeding. In that survey, the analysis is confined to the national categories of race and ethnicity. Hawaiians are now recognized but are included with other Pacific Islanders, who are considerably different. The Asian category, too, does not distinguish between subgroups. Novotny9 described some interesting ethnic associations with breastfeeding outcomes in Hawaii, but EBF was not a consideration at that time and so was not evaluated. Carmichael10 described a study of the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) population in Hawaii in which ethnic correlates with exclusive breastfeeding were reported.
Hawaii is the most ethnically diverse state in the United States; it has a unique constellation of ethnicities, in which no single group constitutes a majority. The groups involved are primarily Asian, but significant differences are found within the subgroups in many areas, as well as from the other racial groups. For example, African Americans make up a very small percentage of the Hawaii population but are more successful than several other groups in Hawaii, in contrast to findings from mainland studies.5,8,11
The purpose of this study was to estimate the prevalence of EBF at six months in Hawaii and to evaluate factors that may influence the likelihood that a mother may breastfeed her infant to six months, and beyond, exclusively or otherwise.
Methods
The University of Hawaii institutional review board expedited approval was obtained before beginning the study (CHS# 12152). A representative cross-sectional design was employed with a stratified random sample consisting of a subset of the Hawaii 2002–2003 Pregnancy Risk Assessment Monitoring System (PRAMS)12 respondents. The PRAMS respondents were asked if they would consent to receiving a further survey about infant feeding (the Hawaii Infant Feeding Survey). Approximately 70% agreed. An original content-valid questionnaire containing 68 questions, in a printed format resembling that used in the original PRAMS survey, was mailed to these 999 consenting mothers when their infants had reached ≈7–10 months of age. Nonresponders were sent a second and, if necessary, a third questionnaire, each a few weeks apart. Approximately 50% of those polled returned their printed responses. The remainder of the participants were queried by phone. (This system was used in the original PRAMS survey.) A response rate of 72% was achieved, and 701 surveys were analyzed.
To ensure adequate representation of groups believed to be at increased risk, the original PRAMS protocol called for oversampling from the birth certificate data of those self-described as Hawaiian or part-Hawaiian and those living on the neighbor islands (ie, not Oahu). This sampling strategy attempted to compare a rural population with that of urban Honolulu County on the island of Oahu.
The analysis was conducted by using SAS-callable SUDAAN program (RTI International, Research Triangle Park, NC) for logistic regressions and Kaplan-Meier curves. The SUDAAN software produces appropriate standard errors when calculating population estimates. Outcome variables were any breastfeeding at six months age and EBF or full breastfeeding at six months. The word “full” is applied to breastfeeding in the sense of almost exclusive, according to the definitions of Labbok.13. Once the infant has been given some feeding other than breastmilk, even if only on a single occasion, breastfeeding can no longer be considered exclusive. Breastfeeding may be described as full if the substitute feeds are not continued regularly thereafter.
Independent variables included the education level of the mother (college educated or not [more or less than 12 years of education]), race and ethnicity (grouped in six categories: White, Hawaiian/part-Hawaiian, Japanese, Filipino, other Asian, and African American/American Indian), and whether or not formula was given in the maternity hospital. Other variables considered included maternal age, income or poverty level, marital status, parity, infant birth weight >2500 g, prematurity (<37 weeks’ gestation), requiring a stay in a neonatal intensive care unit (NICU), hospital of birth, place of residence (urban or rural), participation during pregnancy in WIG, smoking by mother, and return to work or school by the mother.
Results
Hawaiian, White, Japanese, and Filipino are the predominant ethnic/racial groups in our sample (Table 1). The overall rate of EBF or full breastfeeding at six months was ~16%. Figure 1 shows the rates of decline in breastfeeding, in weeks, that resulted in the low rate of EBF at six months, compared with any breastfeeding.
Table 1.
Demographic characteristics of 701 mothers of infants aged 7–10 months, Hawaii
| Characteristic | n | % (weighted) |
|---|---|---|
| Age (years) | ||
| <20 | 68 | 10.0 |
| 20–24 | 155 | 21.3 |
| 25–34 | 271 | 50.6 |
| ≥35 | 105 | 18.2 |
| Education (years) | ||
| ≤12 | 294 | 47.0 |
| >12 | 303 | 53.0 |
| Marital Status | ||
| Married | 373 | 67.8 |
| Single | 226 | 32.2 |
| Parity | ||
| First | 277 | 48.5 |
| Second | 188 | 30.2 |
| Third or more | 134 | 21.3 |
| Race/Ethnicity | ||
| White | 110 | 24.9 |
| Hawaiian/part-Hawaiian | 284 | 25.9 |
| Japanese | 74 | 13.0 |
| Filipino | 106 | 18.3 |
| Other Asian (including Chinese, Korean, Vietnamese, Laotian, Cambodian, and Pacific Islander) | 92 | 14.8 |
| African American | 3 | 1.1 |
| American Indian | 3 | 1.1 |
| Income (per year) | ||
| <$10,000 | 86 | 13.8 |
| $10,000–30,000 | 166 | 29.4 |
| $30,000–50,000 | 110 | 22.2 |
| >$50,000 | 189 | 34.7 |
| WIC Participation during Pregnancy | ||
| Yes | 258 | 38.5 |
| No | 334 | 61.5 |
WIC = Special Supplemental Nutrition Program for Women, Infants, and Children.
Fig 1.
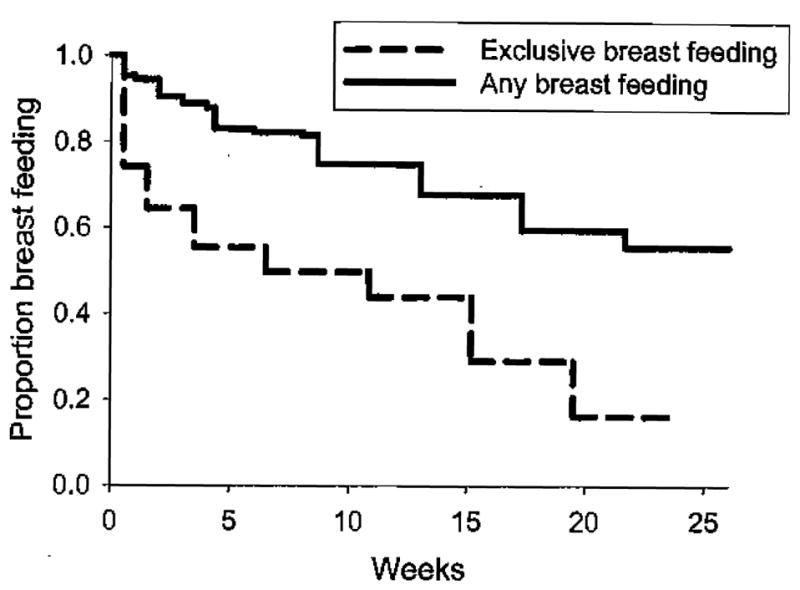
Proportion of exclusive breastfeeding and any breastfeeding by week after birth in Hawaii among mothers.
EBF was significantly associated with ethnicity; 26% of Whites reported full breastfeeding at six months compared with 6% of Filipinos, 14% of Hawaiians, and 15.7% of other Asians. In a regression model that included formula use in the hospital and race/ ethnicity, no formula use in the hospital was strongly associated with EBF at six months (odds ratio [OR] 2.59, 95% confidence interval [CI] 1.31–5.11) (Figure 2).
Fig 2.
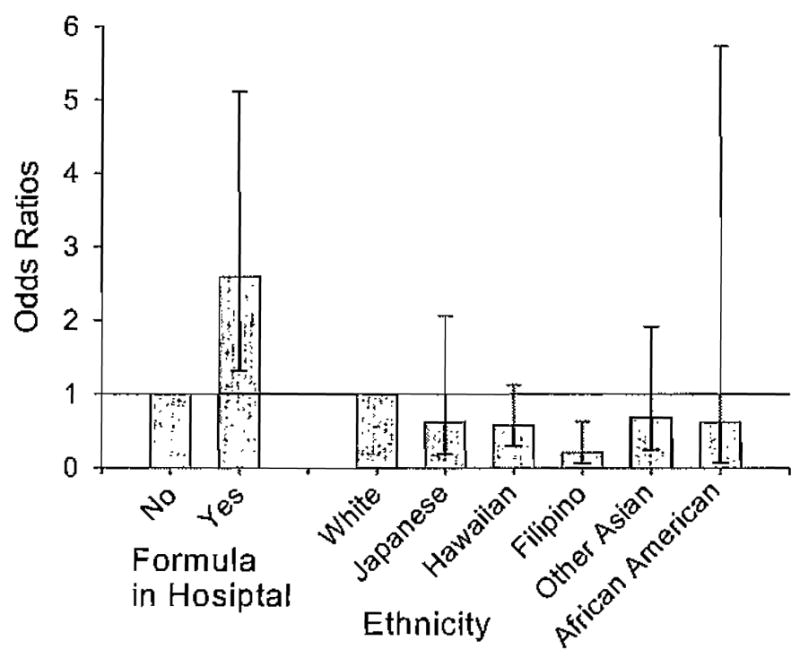
Odds ratios for exclusive breastfeeding at six months by use of formula in the hospital and maternal ethnicity. Error bars represent 95% confidence intervals. Referent group for formula in hospital is no formula, and referent group for ethnicity is White.
Formula use in the hospital was significantly associated with race/ethnicity and hospital of delivery. Japanese were the most likely (60%) to use formula while in the hospital, followed by Filipinos (53%) and Hawaiians (52%). Whites were least likely (28%). Other variables, as noted above, were not significant.
At six months, 54% of mothers did some breastfeeding. Regression models were used to analyze race/ethnicity, education level of the mother, and formula use in the hospital. Statistical significance was documented for all these variables. In Japanese mothers, the rate of any breastfeeding at six months was comparable to the rate for Whites, whereas breastfeeding rates reported by Filipinos and Hawaiians were significantly lower. Mothers with less than a college education were 40% as likely to report any breastfeeding at six months. Infants who were fed formula in the hospital were half as likely to be breastfeeding at six months. The logistic regression analyses showed formula use in the hospital after delivery was very strongly, but inversely, associated with any breastfeeding at 6 months (OR 2.03, 95% CI 1.28–3.20) (Table 2).
Table 2.
Associations of independent variables with odds of any breastfeeding at six months in Hawaii among mothers
| Independent Variable | Odds Ratio ( 95% Confidence Intervals) |
|---|---|
| Formula Use in Hospital | |
| Yes | 1.0 |
| No | 2.0 (1.3–3.2) |
| Race/Ethnicity | |
| White | 1.0 |
| Hawaiian/part-Hawaiian | .4 (.2–.8) |
| Japanese | .94 (.3–2.6) |
| Filipino | .34 (.2–.7) |
| Other Asian | .33 (.1–.8) |
| African American/American Indian | .51 (0–3.6) |
| Mother has College Education | |
| Yes | 1.0 |
| No | .4 (.2–.6) |
Discussion
Our results show that even though breastfeeding initiation rates are high in Hawaii (85%–90%), the rates of exclusive breastfeeding at six months (16%), are barely above the national average (14.7%).8 Formula was used soon after birth by almost half the sample (46%), and only approximately one third of those mothers stopped using formula on a regular basis and resumed full breastfeeding. Breastfeeding rates declined in both groups, but the decline was more gradual in the full or EBF group. Demographic factors, especially race/ ethnicity,8–11 may influence the rate of formula use in the hospital. Many of the variables commonly associated with premature cessation of breastfeeding in other studies 8–11,14 were not significant in this analysis. This difference may be related to the shorter recall period (nine months vs up to three years).15
The influence of race/ethnicity on breastfeeding was strong, as reported by other investigators,8–11 though different in effect. Hawaii is populated by many different Asian subgroups. These groups historically arrived in Hawaii at different times, the most recent coming from Vietnam and neighboring countries. Similarly, the indigenous Hawaiian population has been joined by several waves of other Polynesian groups, and other Pacific Island peoples have settled in Hawaii, the most recent coming from Micronesia and the Marshall Islands. These cultures traditionally breastfeed, but as with many other migrant groups, a trend to the increasing use of formula feeding is seen, which may be perceived by them to be part of the assimilation process.
Many of the groups identified were too small in number to permit valid analysis. For example the Chinese (the earliest Asian group to come to Hawaii) were included in the other Asian category, which also included other Pacific Islanders. Overall, this group achieved somewhat better-than-average breastfeeding outcomes. Japanese represent about 25% of Hawaii’s population but only 13% of the births in this study. Novotny9 reported that Japanese mothers stopped breastfeeding sooner than their socioeconomic status would have predicted. Although not statistically significant, our results support this finding, especially for exclusive breastfeeding but less so for any breastfeeding, much of which may well be only token breastfeeding.13 Filipinos, by contrast, who also constitute close to 25% of the population (19% of the births in this study), achieved much lower breastfeeding rates, which were statistically significant, both for EBF and any breastfeeding. Hawaiians’ breastfeeding rates compared favorably with the national average.
African Americans in Hawaii are very few in number (1%) and predominantly (85%) involved with the military, but because of their importance in most other US studies,5,8,11,14 their (reasonably good) outcomes were reported here, despite lack of statistical significance.
After adjusting for race and poverty, maternal age was not statistically significant. Also not significant were marital status, parity, birth weight, preterm delivery, NICU stay, hospital of delivery, or urban or rural residence of mother at the time of birth. WIC participation during pregnancy was associated with slightly reduced breastfeeding outcomes but not significantly so.
Returning to work (or school) is commonly regarded as the obvious reason why mothers fail to continue EBF for the recommended six months. Our preliminary results do not support this belief. A similar percentage of nonworking mothers failed to continue EBF for six months. CDC is currently addressing this issue by educating employers about the benefits of breastfeeding and the need to assist their employed new mothers to breastfeed for a longer period of time.
Implications for Improving Health Disparities
Successful breastfeeding has been associated with improved health outcomes1–6 for both infants and their mothers. Communities benefit, and healthcare costs are reduced. Increasing EBF in particular may benefit communities where HIV/AIDS17 is a concern. Breastfeeding may provide the primary immunization. Development and systematic testing of innovative programs to improve breastfeeding rates with early exclusivity may reduce health disparities in Hawaii.
Conclusions and Recommendations
Initiation rates of breastfeeding are high (85%–90%) in Hawaii. Yet the rate of exclusive breastfeeding at six months (16%) is barely above the national average (15%). As in the United States as a whole, Whites in Hawaii have the highest rates of breastfeeding, including EBF at six months. The finding that Filipinos had the poorest outcomes in breastfeeding has not previously been documented in the general population. Early use of formula in the maternity hospital by almost half the study sample was strongly associated with early cessation of breastfeeding.
Increased efforts to limit formula use by mothers of newborn infants, unless truly medically necessary, will require creative interventions to bring about changes in attitudes and practice both in the professionals providing care,18,20 the health systems in which they practice,19 and in the vulnerable new mothers.14 A community-based study of the Filipino population in Hawaii may result in new insights into possible approaches that may reverse the disparity found in their breastfeeding outcomes.
References
- 1.Duncan B, Ey J, Holberg CJ, Wright AL, Martinez FD, Taussig LM. Exclusive breastfeeding for at least 4 months protects against otitis media. Pediatrics. 1993;91:867–872. [PubMed] [Google Scholar]
- 2.Dewey KG, Heinig MJ, Nommsen-Rivers LA. Differences in morbidity between breast-fed and formula-fed infants. J Pediatr. 1995;126:696–702. doi: 10.1016/s0022-3476(95)70395-0. [DOI] [PubMed] [Google Scholar]
- 3.Kramer MS, Chalmers B, Hodnett ED, et al. Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA. 2001;285(4):413–420. doi: 10.1001/jama.285.4.413. [DOI] [PubMed] [Google Scholar]
- 4.Chantty CJ, Howard CR, Auinger P. Full breastfeeding duration and associated decrease in respiratory tract infection in US children. Pediatrics. 2006;117(2):425–432. doi: 10.1542/peds.2004-2283. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics, Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2005;115(2):496–506. doi: 10.1542/peds.2004-2491. [DOI] [PubMed] [Google Scholar]
- 6.Raisler J, Alexander C, O’Campo P. Breastfeeding and infant illness: a dose response relationship? Am J Public Health. 1999;89(1):25–30. doi: 10.2105/ajph.89.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ryan AS, Pratt WF, Wysong JL, Lewandowski G, McNally JW, Krieger FW. A comparison of breast-feeding data from the National Surveys of Family Growth and the Ross Laboratories Mothers Surveys. Am J Public Health. 1991;81:1049–1052. doi: 10.2105/ajph.81.8.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Breastfeeding: data and statistics: breastfeeding practices—results form the National Immunization Survey, 2002. Pediatrics. 2005;115(1):e31–37. [Google Scholar]
- 9.Novotny R, Hla MM, Kieffer EC, Park CB, Mor J, Thiele M. Breastfeeding in a multiethnic population in Hawaii. Birth. 2000;27(2):91–96. doi: 10.1046/j.1523-536x.2000.00091.x. [DOI] [PubMed] [Google Scholar]
- 10.Carmichael SL, Prince CB, Burr R, et al. Breastfeeding practices among WIC participants in Hawaii. J Am Diet Assoc. 2001;101(1):57–62. doi: 10.1016/S0002-8223(01)00016-5. [DOI] [PubMed] [Google Scholar]
- 11.Li R, Grummer-Strawn L. Racial and ethnic disparities in breastfeeding among United States infants: Third National health and Nutrition Examination Survey, 1988—1994. Birth. 2002;29:251–257. doi: 10.1046/j.1523-536x.2002.00199.x. [DOI] [PubMed] [Google Scholar]
- 12.Colley Gilbert B], Shulman HB, Fischer L, Rogers MM. The pregnancy risk assessment monitoring system (PRAMS): methods and 1996 response rates from 11 states. Maternal Child Health J. 1999;3:199–209. doi: 10.1023/a:1022325421844. [DOI] [PubMed] [Google Scholar]
- 13.Labbok MH, Coffin CJ. A call for consistency in definition of breastfeeding behaviors. Soc Sci Med. 1997;44:1931–1932. doi: 10.1016/s0277-9536(97)00013-0. [DOI] [PubMed] [Google Scholar]
- 14.Ertem IO, Votto N, Leventhal JM. The timing and predictors of the early termination of breastfeeding. Pediatrics. 2001;107(3):543–548. doi: 10.1542/peds.107.3.543. [DOI] [PubMed] [Google Scholar]
- 15.Bland RM, Rollins NC, Solarsh G, Van den Broeck J, Coovadia HM Child health Group. Maternal recall of exclusive breast feeding duration. Arch Dis Child. 2003;88:778–783. doi: 10.1136/adc.88.9.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kimbro R. On-the-job moms: work and breastfeeding initiation and duration for a sample of low-income women. Maternal Child Health J. 2006;10(1):19–26. doi: 10.1007/s10995-005-0058-7. [DOI] [PubMed] [Google Scholar]
- 17.Iliff P, Piwoz EG, Tavengwa NV, et al. Early exclusive breastfeeding reduces the risk of postnatal HIV-1 transmission and increases HIV-free survival. AIDS. 2005;19(7):699–708. doi: 10.1097/01.aids.0000166093.16446.c9. [DOI] [PubMed] [Google Scholar]
- 18.Li R, Hsia J, Fridinger F, Hussain A, Benton-Davis S, Grummer-Strawn L. Public beliefs about breastfeeding policies in various settings. J Am Diet Assoc. 2004;104(7):1162–1168. doi: 10.1016/j.jada.2004.04.028. [DOI] [PubMed] [Google Scholar]
- 19.Guise JM, Palda V, Westhoff C, Chan BKS, Helfand M, Lieu TA. The effectiveness of primary-care based interventions to promote breastfeeding: systematic evidence review and meta-analysis for the US Preventive Services Task Force. Ann Fam Med. 2003;1(2):70–80. doi: 10.1370/afm.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Freed GL, Clark SJ, Sorenson J, Lohr JA, Cefalo R, Curtis P. National assessment of physicians’ breastfeeding knowledge, attitudes, training and experience. JAMA. 1995;273:472–476. doi: 10.1001/jama.1995.03520300046035. [DOI] [PubMed] [Google Scholar]


