Abstract
Objectives:
Adults with ADHD experience considerable functional impairment. However, the extent to which comorbid Axis II personality disorders contribute to their difficulties and whether such comorbidities are associated with the childhood condition or the persistence of ADHD into adulthood remains unclear.
Methods:
This study examined the presence of personality disorders in a longitudinal sample of adolescents diagnosed with ADHD when they were 7 – 11 years-old, as compared to a matched, never-ADHD, control group. Participants were 16-26 years old at follow-up. Based on a psychiatric interview, the ADHD group was subdivided into those with and without persistent ADHD. Axis II symptoms were assessed using the SCID-II. Data were analyzed using logistic regression and odds ratios (OR) were generated.
Results:
Individuals diagnosed with childhood ADHD are at increased risk for personality disorders in late adolescence, specifically Borderline (OR = 13.16), Antisocial (OR = 3.03), Avoidant (OR = 9.77), and Narcissistic (OR = 8.69) personality disorders. Those with persistent ADHD were at higher risk for Antisocial (OR = 5.26) and Paranoid (OR = 8.47) personality disorders when compared to those in whom ADHD remitted, but not the other personality disorders.
Conclusion:
Results suggest that ADHD portends risk for adult personality disorders, but the risk is not uniform across disorders, nor is it uniformly related to child or adult diagnostic status.
Keywords: Attention-deficit/Hyperactivity Disorder, personality disorders, adolescence, longitudinal
Longitudinal studies of children with Attention-deficit/Hyperactivity Disorder (ADHD) demonstrate that the disorder frequently persists into adulthood (1-4) and is associated with significant life-long functional impairment (5). Different sampling methods as well as age at follow-up result in varying rates of persistence, but longitudinal studies suggest persistence rates range from 4% to more than 80% (1,3,5,6). A recent epidemiological study found that nearly 40% of individuals with childhood ADHD have persisting symptoms significant enough for diagnosis in adulthood (7). Thus, among many people, ADHD may be conceptualized as a chronic disorder that is not confined to childhood and adolescence.
As is the case with childhood ADHD, adult ADHD carries with it an increased risk for comorbid Axis I psychopathology (8-10). Among adults with ADHD, several studies have indicated elevated rates of comorbid mood (6,11,12), anxiety (13,14), and substance use (15,16) disorders. In addition, adults with ADHD are oftentimes characterized by affective volatility (17,18), occupational instability (19), poor social relationships (17,20), and impulsive and self-destructive behaviors (7,21) that may or may not be related to the presence of ADHD or other Axis I disorders. As such, investigators (22-26) have recently begun to explore the degree to which Axis II Personality Disorders might account for some of the functional impairment associated with ADHD in adults.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Text Revision (27), personality disorders are enduring, pervasive behavioral and thinking patterns that are inflexible and maladaptive. Rather than reflecting transient mental or emotional states that may be more indicative of Axis I disorders, personality disorders are characterized by stable attributes of personality that cause distress or impairment in multiple environments. Cluster A disorders are characterized by odd or eccentric behaviors and include Paranoid, Schizoid, and Schizotypal Personality Disorders. Cluster B disorders include Antisocial, Borderline, Histrionic, and Narcissistic Personality Disorders, with behaviors that are dramatic or emotional. Avoidant, Dependent, and Obsessive-Compulsive Personality Disorders comprise Cluster C with behaviors that are anxious or fearful in nature.
Numerous studies have shown an association between childhood ADHD and adult antisocial personality disorder (28-31), but only a limited number have examined associations between childhood ADHD and other adult personality disorders. Although the link between ADHD and personality disorders may be phenomenological (i.e., overlapping diagnostic criteria), the disorders may co-occur because of common neurobiological and/or environmental risk factors including dysregulation in the hypothalamic-pituitary-adrenal axis (32), adverse early experiences with fear or anger (33), temperament (34) or some combination of these factors. A recent longitudinal study indicated that young adults with a history of ADHD are more likely than those without such history to have a personality disorder, particularly Antisocial, Histrionic, or Borderline personality disorders (22). Consistent with this, individuals with a retrospectively documented history of disruptive behavior disorders during childhood, including ADHD, were significantly more likely to have Cluster B personality disorders in general, and Borderline Personality Disorder in particular, when compared to individuals with childhood internalizing disorders (26).
Retrospective studies also suggest a link between childhood disruptive behavior disorders, and non-Cluster B disorders. Lewinsohn and colleagues reported that adults with retrospectively-reported disruptive behavior disorders experienced higher rates of Antisocial, Histrionic, Narcissistic, Schizoid, and Schizotypal personality disorders than those not reporting a history of ADHD behaviors (24). Additionally, childhood ADHD without comorbid Axis I psychopathology may also increase risk for particular personality disorders. Adults with a history of pure ADHD have greater rates of Antisocial, Histrionic, Narcissistic, and Borderline personality disorders compared with those with a history of comorbid ADHD and internalizing symptomatology (25). Consistent with this, nearly 90% of a sample of adults with personality disorders reported clinically significant ADHD symptoms in childhood (23).
Taken together, these results suggest an association between childhood ADHD and later personality disorder. However, there are a number of limitations inherent to these studies. All but two of the studies (22,26) linking ADHD with Axis II symptomatology other than Antisocial personality disorder have relied on retrospective reporting by clinically-referred adults to make the diagnosis of childhood ADHD. Yet, reliance on retrospective assessment of childhood status in a clinical sample is problematic because of the questionable validity of childhood diagnosis (3). Additionally, there may be other confounding variables. For example, in several of the studies of adults with personality disorders, there was either no clear control group (25,26) or the control group was poorly matched to the psychiatric group on key demographic characteristics, including sex, age, and comorbid diagnoses (23). Finally, it is unclear from these studies whether adult personality disorders are linked to a history of childhood ADHD per se, without regard to adult outcomes, or to the persistence of ADHD into adulthood.
The primary goal of the present study was to assess, as compared to controls, personality disorders in a longitudinal sample of late adolescents who were diagnosed with ADHD during childhood. A secondary aim was to determine the degree to which personality disorder diagnoses are linked to the persistence of ADHD symptoms into adulthood as opposed to the childhood condition per se. It was hypothesized that as compared to matched controls, youth previously diagnosed with ADHD would have elevated levels of Cluster B, but not Clusters A or C personality disorders, and that increased rates of personality disorder would be associated primarily with the persistence of ADHD into adolescence.
METHOD
Participants
Participants included 96 individuals (88.5% male) who were clinically-referred and previously diagnosed with Combined Type ADHD when they were 7 – 11 years-old (mean age at initial evaluation = 9.21 years; SD = 1.19). Participants were followed longitudinally from childhood into adolescence (time between evaluations = 9.97 years; SD = 2.01). These participants with childhood ADHD were compared to 85 community controls (87.1% male) who never met diagnostic criteria for ADHD and were enrolled into the study as adolescents. The controls were similar to participants with ADHD in age, sex, race/ethnicity, and socioeconomic status.
All participants were between 16 and 26 years of age (mean age 18.41 years; SD = 1.62); 54.7% were over 18 years. Participants represented a diverse population with 23.8% self-identifying as non-Hispanic Caucasian, 34.8% Latino/Hispanic, 25.4% African American, 1.1% Asian, and 14.9% as mixed or “other” race. The participants were generally of lower- to lower-middle socioeconomic status (Mean socio-economic prestige = 42.38; SD = 17.25) on a measure of socioeconomic prestige developed at the National Opinion Research Center (35), although a wide distribution of socio-economic prestige was represented (Range: 20-96). Most of the participants were urban dwellers living in a large metropolitan area at the time of evaluation. All participants and their participating parent were proficient in English. Demographic characteristics by group are summarized in Table 1.
Table 1.
Comparison of demographic characteristics for ADHD and control groups
|
Controls n = 85 |
Probands n = 96 |
F/χ2* | ||
|---|---|---|---|---|
| Mean age (SD) | 18.52 (1.65) | 18.31 (1.60) | 0.74 | |
| Mean socio-economic prestige (SD) | 40.89 (16.60) | 43.76 (17.82) | 1.21 | |
| % Male | 87.1% | 88.5% | 0.09 | |
| Race | 6.15 | |||
| % African American | 28.2% | 22.9% | ||
| % Asian | 2.4% | 0 | ||
| % Non- Hispanic Caucasian | 23.5% | 24.0% | ||
| % Hispanic | 36.5% | 33.1% | ||
| % Mixed or Other | 9.4% | 19.8% | ||
All comparisons were non-significant (p > .15).
For participants under the age of 18 years, informed consent was provided by the parent and assent by the youth; consent was provided directly by participants who were 18 years of age or older. This study was approved by the institutional review boards for both academic institutions where the study was conducted. Participants were compensated for their time in the evaluation process and received no intervention or treatment services as a result of their participation.
Childhood Evaluation
Individuals with ADHD were initially screened for participation during childhood using the IOWA Conners teacher ratings (36). Those with an Inattention/Overactivity score more than 1.5 SD beyond the normative mean were invited into the lab where parents were administered the Diagnostic Interview Schedule for Children (37) to determine the final diagnoses. The diagnostic process and criteria are described in more detail in previous studies (38,39). In addition to ADHD, during childhood, 45.8% met criteria for comorbid Oppositional Defiant Disorder, 32.3% for Conduct Disorder, 9.4% for a mood disorder, 31.3% for an anxiety disorder other than simple phobia, and 16.7% had no comorbid psychopathology. These diagnoses were collapsed into externalizing comorbidity (ODD and CD) and internalizing comorbidity (mood and anxiety disorders) for post-hoc statistical analyses.
Controls were recruited specifically for the follow-up phase of the longitudinal study to match participants on a number of demographic factors. Control participants were screened for lifetime presence of ADHD symptoms, treatment of ADHD symptoms, and previous difficulties related to ADHD symptoms. Those with evidence of prior or current ADHD symptoms were excluded from the study. Individuals diagnosed with mental retardation, a pervasive developmental disorder, schizophrenia, or a diagnosed neurological disorder (e.g., epilepsy) were not eligible for entry into the study as probands (during childhood) or controls.
Follow-up Assessment
At follow-up, the Kiddie-SADS PL (40) was administered independently to each participant and a parent to assess current ADHD status by a trained clinician who provided a summary score that includes clinical observations as well as information from both reporters. Based on this interview, the previously ADHD group was subdivided into those who continued to meet diagnostic criteria for ADHD (“Persisters” n = 42) and those that did not (“Remitters” n = 32). Persistence was defined as meeting full DSM-IV (1) diagnostic criteria for ADHD, which requires at least six symptoms of inattention and/or at least six symptoms of hyperactivity-impulsivity along with impairment. Remittance was defined as those who had no more than three symptoms of inattention and no more than three symptoms of hyperactivity-impulsivity. Among the Persisters, 38.1% continued to meet full DSM-IV criteria for ADHD – Combined Type, 47.6% met symptom criteria for ADHD Predominantly Inattentive Type and 14.3% met criteria for ADHD-Hyperactive-Impulsive Type. Nevertheless, based upon their childhood status, those presenting as either ADHD-I or ADHD-HI at follow-up are probably more aptly considered to have ADHD-C in partial remission. The remitters group included those individuals with three or fewer symptoms of inattention and three or fewer symptoms of hyperactivity-impulsivity. Those individuals in the sample with more than three symptoms but fewer than six symptoms in either domain were excluded in the second set of analyses (n = 22), which focuses on distinctions between ADHD persisters and remitters. As per the selection criteria, no controls met criteria for ADHD.
All participants were administered the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II; 41). The SCID-II, which has been validated for use with adult clinical populations (42), is a semi-structured interview designed to assess personality disorders. For this study, it was separately administered to the parent and adolescent by two different clinicians. Reports by parent and adolescent were considered separately at the item level. Thus, if either the parent or the adolescent endorsed a particular symptom at a clinically significant level, the adolescent was assumed to exhibit the symptom. This procedure was not expected to reveal higher levels of personality disorders, but rather supplement information provided by a single informant (43,44). Diagnoses were made using DSM-IV TR (27) criteria for each personality disorder. Although personality disorders are typically not diagnosed until very late adolescence or early adulthood, there are a number of studies documenting the validity of personality disorder diagnosis prior to the age of 18 years (45,46). A summary of the personality disorder diagnoses by group is presented in Table 2.
Table 2.
Summary of personality disorder diagnoses
|
Controls n = 85 |
All ADHD n = 96 |
Remitters n = 32 |
Persisters n = 42 |
||
|---|---|---|---|---|---|
| Cluster A | |||||
| Paranoid PD | 4.7% | 12.5% | 3.1% | 21.4% | |
| Schizoid PD | 3.5% | 5.2% | 3.1% | 9.5% | |
| Schizotypal PD | 0 | 2.1% | 3.1% | 0 | |
| Cluster B | |||||
| Borderline PD | 1.2% | 13.5% | 6.3% | 19.0% | |
| Histrionic PD | 0 | 2.1% | 0 | 4.8% | |
| Narcissistic PD | 1.2% | 9.4% | 6.3% | 14.3% | |
| Antisocial PD | 9.4% | 24.0% | 12.5% | 35.7% | |
| Cluster C | |||||
| Avoidant PD | 1.2% | 10.4% | 0 | 19.0% | |
| Dependent PD | 0 | 1.0% | 0 | 2.4% | |
| Obsessive- Compulsive PD | 2.4% | 5.2% | 3.1% | 2.4% | |
| No PD diagnosis | 75.3% | 47.9% | 65.6% | 35.7% | |
Statistical Analyses
All data analyses were completed using SPSS 15.0. The first set of analyses included logistic regression equations focusing on childhood diagnostic status (ADHD versus Controls) as the independent variable, which was entered in the first step of each predictive analysis. The second set of logistic regression equations focused on adolescent ADHD status (Persisters, Remitters, and Controls) as the independent variable. Individual personality disorder diagnoses served as dependent variables in both sets of analyses.
RESULTS
Childhood ADHD Diagnostic Status
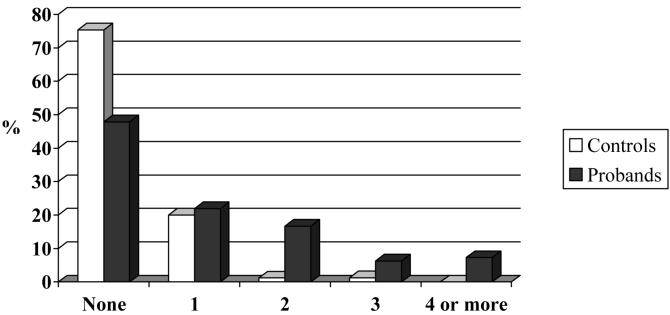
Logistic regression equations focusing on childhood diagnostic status (ADHD versus Controls) indicated that individuals with childhood ADHD were significantly more likely than Controls to be diagnosed with Avoidant (Wald = 4.62, p = .032), Narcissistic (Wald = 4.21, p = .042), Borderline (Wald = 6.03, p = .014), and Antisocial (Wald = 6.30, p = .012) personality disorders. Individuals with childhood ADHD were also marginally more likely to be diagnosed with Paranoid personality disorder (Wald = 3.16, p = .076) than controls. Those with childhood ADHD and Controls did not differ (p > .10) with regard to Dependent, Obsessive-Compulsive, Schizotypal, Schizoid, and Histrionic personality disorders diagnoses. A summary of these results appears in Table 3. Overall, individuals with childhood ADHD were diagnosed with significantly more personality disorders than Controls (Mann-Whitney U = 2743.50, p < .001), and were more likely to be diagnosed with multiple personality disorders. Figure 1 depicts the number of personality disorder diagnoses as a function of childhood ADHD status.
Table 3.
Summary statistics from logistic regressions examining Personality Disorder diagnoses by childhood status (probands vs. controls).*
| Wald | Sig. | Odds Ratio | 95% CI | ||
|---|---|---|---|---|---|
| Cluster A | |||||
| Paranoid PD | 3.16 | .076 | 2.89 | 0.90-9.34 | |
| Schizoid PD | 0.30 | .586 | 1.50 | 0.35-8.48 | |
| Schizotypal PD | - | - | - | - | |
| Cluster B | |||||
| Histrionic PD | - | - | - | - | |
| Narcissistic PD | 4.12 | .042 | 8.69 | 1.08-70.09 | |
| Borderline PD | 6.03 | .014 | 13.16 | 1.68-102.86 | |
| Antisocial PD | 6.31 | .012 | 3.03 | 1.28-7.21 | |
| Cluster C | |||||
| Avoidant PD | 4.62 | .032 | 9.77 | 1.22-77.99 | |
| Dependent PD | - | - | - | - | |
| Obsessive-Compulsive PD | 0.94 | .332 | 2.28 | 0.43-12.07 | |
Exact statistics cannot be calculated when there are no cases in a cell.
Figure 1.
Number of personality disorders diagnoses for controls and those with childhood ADHD.
Adolescent ADHD Diagnostic Status
As previously described, 22 individuals with childhood ADHD who did not meet criteria for either persistent or remittent ADHD groups were dropped in the second set of analyses focusing on the relationships between adolescent ADHD diagnostic status (Controls vs. Remitters vs. Persisters) and diagnosis of personality disorders. When logistic regression analyses were repeated with adolescent status as the independent variable, as expected, results were similar to the first set of analyses. No statistically significant differences (p > .10) between adolescent groups were noted for Dependent, Obsessive-Compulsive, Schizotypal, Schizoid, and Histrionic personality disorders. Significant differences were noted for Paranoid (Wald = 9.33, p = .009), Narcissistic (Wald = 6.12, p = .05), Borderline (Wald = 8.76, p = .01), and Antisocial (Wald = 12.81, p = .002) personality disorders. Controls were separable from Persisters in all of the significant analyses (all p < .05). In contrast, Persisters and Remitters were only separable for Antisocial personality disorder (p < .001) and Paranoid personality disorder (p < .05), although rates of Borderline, and Narcissistic personality disorders were substantially higher in Persisters than Remitters. Controls and Remitters were not statistically separable for any personality disorders (p > .05). A summary of the results of the second set of analyses is presented in Tables 2 and 4.
Table 4.
Personality Disorder diagnoses by adolescent status [Persisters, Remitters, and Controls].
| Wald | Sig. | Controls v. Remitters | Controls v. Persisters | Remitters v. Persisters | |||||
|---|---|---|---|---|---|---|---|---|---|
|
Odds ratio |
95% CI |
Odds ratio |
95% CI |
Odds ratio |
95% CI | ||||
| Cluster A | |||||||||
| Paranoid PD | 9.33 | .009 | 0.65 | 0.07-6.08 | 5.52** | 1.59-19.19 | 8.47* | 1.01-71.43 | |
| Schizoid PD | 0.00 | 1.00 | 0.00 | - | 0.00 | - | 0.00 | - | |
| Schizotypal PD | 2.25 | 0.33 | 0.88 | 0.09-8.80 | 2.88 | 0.61-13.50 | 0.29 | 0.07-1.63 | |
| Cluster B | |||||||||
| Histrionic PD | 0.00 | .99 | 1.00 | - | 0.00 | - | 0.00 | - | |
| Narcissistic PD | 6.12 | .05 | 5.60 | 0.49-64.02 | 14.00* | 1.63-120-51 | 3.57 | 0.49-33.33 | |
| Borderline PD | 8.76 | .01 | 5.60 | 0.49-64.02 | 19.17** | 2.38-164.12 | 3.57 | 0.69-16.67 | |
| Antisocial PD | 12.81 | .002 | 1.38 | 0.38-4.93 | 5.35*** | 2.40-14.02 | 5.26*** | 2.04-14.29 | |
| Cluster C | |||||||||
| Avoidant PD | 7.63 | .02 | .00 | - | 19.77** | 2.38-164.12 | .00 | - | |
| Dependent PD | - | - | - | - | - | - | - | - | |
| Obsessive-Compulsive PD | 0.60 | .97 | .99 | .09-11.21 | 1.32 | 0.08-21.99 | 0.75 | 0.07-8.33 | |
p < .05
p < .01
p < .001
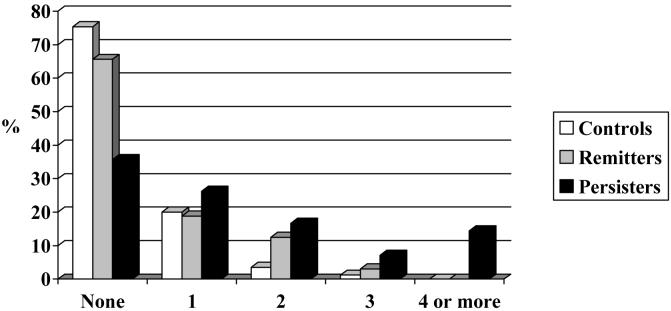
As with the first set of analyses, a post-hoc analysis of the rate of personality disorders by group was also conducted. Persisters, Remitters, and Controls differed significantly on the number of personality disorders diagnosed (Kruskal-Wallis test = 24.98, p < .001), with Persisters having a higher rate of diagnosis than Remitters and Controls. Rates of Axis II diagnoses are summarized in Figure 2.
Figure 2.
Number of personality disorder diagnoses among Controls, Remitters, and Persisters.
Childhood Comorbid Diagnoses
Childhood psychopathology diagnoses were not available for controls. Thus, to test the extent to which childhood psychopathology, as opposed to ADHD persistence alone, contributed to late adolescent diagnosis of antisocial personality disorder, a post-hoc analysis was conducted using only those with ADHD in childhood. Logistic regression was conducted entering separately the dichotomous variables of presence/absence of childhood comorbid externalizing and internalizing disorders (as defined above) in the first step of the equation and late adolescent status (persistence vs. remittance) was entered in the second step. Results showed externalizing childhood comorbidity to marginally predict Antisocial personality disorder diagnosis (Wald = 3.04, p = .08) but internalizing childhood comorbidity did not (p > .50). After the predictive influence of both internalizing and externalizing comorbidity were taken into account in the first step of the regression (p > .05), late adolescent ADHD status (persistence vs. remittance) continued to be a significant predictor of Antisocial personality disorder diagnosis (Wald = 4.85; p = .03). Similar post-hoc analyses for Paranoid, Narcissistic, and Borderline personality disorders were conducted. Childhood internalizing and externalizing comorbidity did not predict diagnosis of any of these personality disorders in late adolescence (p > .05).
DISCUSSION
The principal finding of this study is that individuals diagnosed with ADHD in childhood were more likely to be diagnosed with a personality disorder in late adolescence. Specifically, diagnoses of Avoidant, Narcissistic, Borderline and/or Antisocial personality disorders are more common. Further, those individuals for whom ADHD persisted were at substantially elevated risk for Antisocial and Paranoid personality disorders when compared with those in whom ADHD remitted. These findings are largely consistent with previous studies suggesting increased risk for Antisocial personality disorder and other cluster B personality disorders in youth with ADHD (26,28,30). Notably, however, there were clear distinctions among the Axis II diagnoses that had elevated rates in those with childhood ADHD as compared to controls. The presence of adolescent Antisocial personality disorder does not appear to be directly linked with the presence of childhood ADHD, nor is it strongly related to childhood comorbid psychopathology. Instead, it appears to be the persistence of ADHD that is strongly predictive of Antisocial personality disorder in late adolescence.
These results raise questions about the nature of the relationship between ADHD and personality disorders. One possibility is that ADHD is a precursor to particular personality disorders, and might be thought of as a child and adolescent prodromal phase of the behaviors typically associated with particular personality disorders (47). Similar to the predictive validity of early odd behaviors in individuals who later develop schizophrenia (48), early inattention and overactivity may foretell later affective instability and irritability in some individuals. Similarly, it may be that personality disorders are the natural outcome of ADHD in some segment of the population, and that ADHD in childhood/adolescence interacts with other factors to produce this outcome. One intriguing possibility is that the frequently reported outcome of childhood ADHD characterized by high rates of failed marriages and unstable relationships is due to the presence of comorbid personality disorders rather than the symptoms of ADHD, per se.
Related to this idea, it may also be that children with ADHD interact with their families and other significant individuals in such a way that these relationships increase the likelihood of developing a personality disorder. More specifically, it may be that abnormal interpersonal interactions that are potentiated by childhood ADHD become risk factors within the personality of the individual. These distorted relationships may be the beginning of future personality disorders.
A more controversial possibility is that ADHD and certain personality disorders may represent different phenotypic manifestations of the same disorder. Recent data have convincingly indicated that ADHD is a chronic or enduring condition which is associated with a maladaptive pattern of behavior that causes impairment in multiple environments (4,6,49). This more current view, which is quite distinct from earlier beliefs that it was a childhood condition, has much in common with the conceptualization of personality disorders in adults. This alternative hypothesis is supported by the high degree of similarity in symptoms of several personality disorders identified in this study (e.g., Paranoid, Borderline, and Antisocial personality disorders) and ADHD: hypersensitivity to interpersonal cues, poor self-regulation, affective instability, and impaired social relationships (1) . These features are present in children as well (50,51), yet the focus on inattention, impulsivity and overactivity may make it seem that the conditions are more distinct than they actually are.
Notably, caution must be used when diagnosing Axis II conditions in the context of Axis I psychopathology. With most Axis I disorders it is important ensure that the personality disorder characteristics persist in between episodes and are not merely an extension or epiphenomenon of the Axis I disorder. However, it is becoming increasingly clear that ADHD symptoms and associated impairment are chronic and persistent rather than episodic. Thus, it is more difficult to determine the extent to which ADHD and these diverse Axis II symptoms are truly distinct as opposed to partially separable manifestations of a single disorder.
Although these different hypotheses offer intriguing explanations for the high rate of comorbidity of ADHD and certain personality disorders in adulthood, two important factors must be considered: multifinality and equifinality. Multifinality is the process through which individuals who experience a particular course of events or circumstances have different outcomes, whereas equifinality is the process wherein individuals experiencing a diverse set of circumstances have the same or highly similar outcomes (52). From the multifinality perspective, not all individuals with either childhood ADHD or persistent ADHD in this study met diagnostic criteria for a personality disorder by late adolescence. Thus, other contributing factors clearly play a role in the development of personality disorders in an ADHD population. Additionally, the results of this study indicate that individuals with ADHD are not at uniformly increased risk for any single personality disorder diagnosis. Risk appears to be specifically focused on certain diagnoses; our data indicate that Schizoid, Schizotypal, Histrionic, Dependent, and Obsessive-Compulsive personality disorders are not likely outcomes of ADHD in adulthood.
Several limitations associated with these findings must be acknowledged. Because data on personality disorders were collected at only one time point, it was not possible to conduct analyses examining the developmental progression of maladaptive personality traits in this sample. Additionally, many of the individuals included in this study are not yet 18years-old, and thus may not yet meet the diagnostic threshold, but may in the future. As these individuals get older, there may be an increase in the rate of personality disorder diagnoses. Finally, because some of the cell sizes in this study are small, there may not have been sufficient power to detect meaningful differences between remitters and the other two groups in the rate of personality disorders. Finally, the sex distribution with predominantly more males may have limited our ability to detect meaningful differences in personality disorders more commonly seen in females, such as histrionic and borderline personality disorders.
In summary, these data suggest that as compared to controls, individuals diagnosed with ADHD during childhood are at greater risk for a diagnosis of a personality disorder in late adolescence. Specifically, we found elevated rates of Narcissistic, Paranoid, Borderline, and Antisocial personality disorders. Further, Antisocial and Paranoid personality disorder appears to emerge primarily when ADHD is persistent. Clinicians treating young adults should be mindful of possible co-occurring ADHD and personality disorders. In particular, those individuals who experience poor outcomes associated with strained interpersonal relationships may be at increased risk to also meet criteria for a personality disorder diagnosis. Identifying and providing treatment for behaviors related to personality disorders may improve overall level of functioning and reduce impairment. Future studies, especially those utilizing prospective longitudinal data, ideally conducted in a slightly older sample and with multiple time points for analysis of personality traits, may further elucidate the relationships between ADHD in childhood and adolescence and personality disorders in early adulthood.
Acknowledgments
This research was supported by NIMH grant# RO1 MH60698.
The authors wish to thank Dana Barowsky and Tobey Busch for their assistance in conducting this study.
References
- 1.Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: I. an 8-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1990;29:546–557. doi: 10.1097/00004583-199007000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Biederman J, Faraone S, Milberger S, Guite J, Mick E, Chen L, Mennin D, Marrs A, Ouellette C, Moore P, Spencer T, Norman D, Wilens T, Kraus I, Perrin J. A prospective 4-year follow-up student of attention-deficit hyperactivity and related disorders. Arch Gen Psychiatry. 1996;53:437–446. doi: 10.1001/archpsyc.1996.01830050073012. [DOI] [PubMed] [Google Scholar]
- 3.Mannuzza S, Klein RG, Klein DF, Bessler A, Shrout P. Accuracy of adult recall of childhood attention deficit hyperactivity disorder. Am J Psychiatry. 2002;159:1882–1888. doi: 10.1176/appi.ajp.159.11.1882. [DOI] [PubMed] [Google Scholar]
- 4.Weiss G, Hechtman L, Milroy T, Perlman T. Psychiatric status of hyperactives as adults: A controlled prospective 15-year follow-up of 63 hyperactive children. J Am Acad Child Psychiatry. 1985;24:211–220. doi: 10.1016/s0002-7138(09)60450-7. [DOI] [PubMed] [Google Scholar]
- 5.Birnbaum HG, Kessler RC, Lowe SW, Secnik K, Greenberg PE, Leong SA, Swensen AR. Costs of attention-deficit hyperactivity disorder (ADHD) in the US: Excess costs of persons with ADHD and their fammily members in 2000. Current Medical Research Opinions. 2005;21:195–206. doi: 10.1185/030079904X20303. [DOI] [PubMed] [Google Scholar]
- 6.Biederman J, Monuteaux MC, Mick E, Spencer T, Wilens T, Silva JM, Snyder LE, Faraone S. Young adult outcome of attention deficit hyperactivity disorder: A controlled 10-year follow-up study. Psychol Med. 2006;36:167–179. doi: 10.1017/S0033291705006410. [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, Adler LA, Barkley J, Conners KC, Faraone SV, Greenhill LL, Jaeger S, Secnik K, Spencer T, Ustun TB, Zaslavsky AM. Patterns and predictors of attention-deficit/hyperactivity disorder persistence into adulthood: Results from the national comorbidity survey replication. Biol Psychiatry. 2005;57:1442–1451. doi: 10.1016/j.biopsych.2005.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barkley RA. Major life activity and health outcomes associated with attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2002;63:10–15. [PubMed] [Google Scholar]
- 9.Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M. Adult psychiatric status of hyperactive boys grown up. Am J Psychiatry. 1998;155:493–498. doi: 10.1176/ajp.155.4.493. [DOI] [PubMed] [Google Scholar]
- 10.Secnik K, Swensen A, Lage MJ. Comorbidities and costs of adult patients diagnosed with attention-deficit hyperactivity disorder. Pharmacoeconomics. 2005;23:93–102. doi: 10.2165/00019053-200523010-00008. [DOI] [PubMed] [Google Scholar]
- 11.Blackman GL, Ostrander R, Herman KC. Children with ADHD and depression: A multisource, multimethod assessment of clinical, social, and academic functioning. Journal of Attention Disorders. 2005;8:195–207. doi: 10.1177/1087054705278777. [DOI] [PubMed] [Google Scholar]
- 12.Mick E, Spencer T, Wozniak J, Biederman J. Heterogeneity of irritability in attention-deficit/hyperactivity disorder subjects with and without mood disorders. Biol Psychiatry. 2005;58:576–582. doi: 10.1016/j.biopsych.2005.05.037. [DOI] [PubMed] [Google Scholar]
- 13.Biederman J, Monuteaux MC, Mick E, Spencer T, Wilens T, Silva JM, Snyder LE, Faraone S. Young adult outcome of attention deficit hyperactivity disorder: A controlled 10-year follow-up study. Psychol Med. 2006;36:167–179. doi: 10.1017/S0033291705006410. [DOI] [PubMed] [Google Scholar]
- 14.McGough JJ, Smalley SL, McCracken JT, Yang M, Del'Homme M, Lynn DE, Loo S. Psychiatric comorbidity in adult attention deficit hyperactivity disorder: Findings from multiplex families. Am J Psychiatry. 2005;162:1621–1627. doi: 10.1176/appi.ajp.162.9.1621. [DOI] [PubMed] [Google Scholar]
- 15.Kalbag AS, Levin FR. Adult ADHD and substance abuse: Diagnostic and treatment issues. Substance use and Misuse. 2005;40:1955–1981. doi: 10.1080/10826080500294858. [DOI] [PubMed] [Google Scholar]
- 16.Wilson JJ, Levin FR. Attention-deficit/hyperactivity disorder and early-onset substance abuse disorders. J Child Adolesc Psychopharmacol. 2005;15:751–763. doi: 10.1089/cap.2005.15.751. [DOI] [PubMed] [Google Scholar]
- 17.Maedgen JW, Carlson CL. Social functioning and emotional regulation in the attention deficit hyperactivity disorder subtypes. J Clin Child Psychol. 2000;29:30–42. doi: 10.1207/S15374424jccp2901_4. [DOI] [PubMed] [Google Scholar]
- 18.Wilens T, Dodson W. A clinical perspective of attention-deficit/hyperactivity disorder into adulthood. J Clin Psychiatry. 2004;65:1301–1313. doi: 10.4088/jcp.v65n1003. [DOI] [PubMed] [Google Scholar]
- 19.Bellack L, Black RB. Attention-deficit hyperactivity disorder in adults. Clinical Therapy. 1992;14:138–147. [PubMed] [Google Scholar]
- 20.Paulson JF, Buermeyer C, Nelson-Gray RO. Social rejection and ADHD in young adults: An analogue experiment. Journal of Attention Disorders. 2005;8:127–135. doi: 10.1177/1087054705277203. [DOI] [PubMed] [Google Scholar]
- 21.Shaw-Zirt B, Popali-Lehane L, Chaplin W, Bergman A. Adjustment, social skills, and self-esteem in college students with symptoms of ADHD. Journal of Attention Disorders. 2005;8:109–120. doi: 10.1177/1087054705277775. [DOI] [PubMed] [Google Scholar]
- 22.Fischer M, Barkley RA, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: Self-reported psychiatric disorders, comorbidity, and the role of childhood conduct problems and teen CD. J Abnorm Child Psychol. 2002;30:463–475. doi: 10.1023/a:1019864813776. [DOI] [PubMed] [Google Scholar]
- 23.Fossati A, Novella L, Donati D, Donini M, Maffei C. History of childhood attention deficit/hyperactivity disorder symptoms and borderline personality disorder: A controlled study. Compr Psychiatry. 2002;43:369–377. doi: 10.1053/comp.2002.34634. [DOI] [PubMed] [Google Scholar]
- 24.Lewinsohn PM, Rohde P, Seeley JR, Klein DN. Axis II psychopathology as a function of axis I disorders in childhood and adolescence. J Am Acad Child Adolesc Psychiatry. 1997;36:1752–1759. doi: 10.1097/00004583-199712000-00024. [DOI] [PubMed] [Google Scholar]
- 25.May B, Bos J. Personality characteristics of ADHD adults assessed with the millon clinical multiaxial inventory-II: Evidence of four distinct subtypes. J Pers Assess. 2000;75:237–248. doi: 10.1207/S15327752JPA7502_5. [DOI] [PubMed] [Google Scholar]
- 26.Rey JM, Morris-Yates A, Singh M, Andrews G, Stewart GW. Continuities between psychiatric disorders in adolescents and personality disorders in young adults. Am J Psychiatry. 1995;152:895–900. doi: 10.1176/ajp.152.6.895. [DOI] [PubMed] [Google Scholar]
- 27.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- 28.Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: Antisocial activities and drug use. Journal of Child Psychology, Psychiatry, and Allied Disciplines. 2004;45:195–211. doi: 10.1111/j.1469-7610.2004.00214.x. [DOI] [PubMed] [Google Scholar]
- 29.Bernstein DP, Cohen P, Skodol A, Bezirganian S, Brook JS. Childhood antecedents of adolescent personality disorders. Am J Psychiatry. 1996;153:907–913. doi: 10.1176/ajp.153.7.907. [DOI] [PubMed] [Google Scholar]
- 30.Loeber R, Burke JD, Lahey BB. What are the adolescent antecedents to antisocial personality disorder? Criminal Behavior and Mental Health. 2002;12:24–36. doi: 10.1002/cbm.484. [DOI] [PubMed] [Google Scholar]
- 31.Murphy KR, Barkley RA, Bush T. Young adults with attention deficit hyperactivity disorder: Subtype differences in comorbidity, educational, and clinical history. Journal of Nervous and Mental Disorders. 2002;190:147–157. doi: 10.1097/00005053-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Gollan JK, Lee R, Coccaro EF. Developmental psychopathology and neurobiology in aggression. Developmental Psychopathology. 2005;17:151–171. doi: 10.1017/s0954579405050546. [DOI] [PubMed] [Google Scholar]
- 33.Lara DR, Pinto O, Akiskal K, Akishal HS. Toward an integrative model of the spectrum of mood, behavioral and personality disorder based on fear and anger traits: 1. clinical implications. J Affect Disord. 2006;94:67–87. doi: 10.1016/j.jad.2006.02.025. [DOI] [PubMed] [Google Scholar]
- 34.Clark LA. Temperament as a unifying basis for personality and psychopathology. J Abnorm Psychol. 2005;114:505–521. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- 35.Nakao K, Treas J. Updating occupational prestige and socioeconomic scores: How the new measures measure up. Sociological Methodology. 1994;24:1–72. [Google Scholar]
- 36.Loney J, Milich R. Hyperactivity, inattention, and aggression in clinical practice. Advances in Developmental and Behavioral Pediatrics. 1982;3:113. [Google Scholar]
- 37.Shaffer D, Fisher P, Piancentini J, Schwab-Stone M, Wicks J. Diagnostic Interview Schedule for Children (DISC-2.1P) - Parent Version. New York State Psychiatric Institute; New York, NY: 1989. [Google Scholar]
- 38.Halperin JM, Newcorn JH, Kopstein I, McKay KE, Schwartz ST, Siever LJ, Sharma V. Serotonin, aggression, and parental psychpathology in children with attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 1997;26:1391–1398. doi: 10.1097/00004583-199710000-00021. [DOI] [PubMed] [Google Scholar]
- 39.Halperin JM, Sharma V, Siever LJ, Schwartz ST, Matier K, Wornel G, Newcorn JH. Serotonergic function in aggressive and non-aggressive boys with attention-deficit hyperactivity disorder. Am J Psychiatry. 1994;151:243–248. doi: 10.1176/ajp.151.2.243. [DOI] [PubMed] [Google Scholar]
- 40.Kaufman J, Brimaher B, Brent D, Rao U, Ryan N. Kiddie-SADS - Present and Lifetime Version. University of Pittsburgh School of Medicine; Pittsburgh, PA: 1996. [Google Scholar]
- 41.First MB, Gibson M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders. American Psychiatric Press; Washington, DC: 1997. [Google Scholar]
- 42.Farmer RF, Chapman AL. Evaluation of DSM-IV personality disorder criteria as assessed by the structured clinical interview for DSM-IV personality disorders. Compr Psychiatry. 2002;43:285–300. doi: 10.1053/comp.2002.33494. [DOI] [PubMed] [Google Scholar]
- 43.Bernstein DP, Kasapis C, Bergman A, Weld E, Mitropoulou V, Horvarth T, Klar HM, Silverman J, Siever LJ. Assessing axis II disorders from informant interview. J Personal Disord. 1997;11:158–167. doi: 10.1521/pedi.1997.11.2.158. [DOI] [PubMed] [Google Scholar]
- 44.Kraemer HC, Measelle JR, Ablow JC, Essex MJ, Boyce WT, Kupfer DJ. A new approach to integrating data from multiple informants in psychiatric assessment and research: Mixing and matching contexts and perspectives. Am J Psychiatry. 2003;160:1566–1577. doi: 10.1176/appi.ajp.160.9.1566. [DOI] [PubMed] [Google Scholar]
- 45.Bernstein DP, Cohen P, Velez N, Schwab-Stone M, Siever LJ, Shinsato L. Prevalence and stability of the DSM-III-R personality disorders in a community-based survey of adolescents. Am J Psychiatry. 1993;150:1237–1243. doi: 10.1176/ajp.150.8.1237. [DOI] [PubMed] [Google Scholar]
- 46.Kasen S, Cohen P, Skodol A, Johnson JG, Brook JS. Influence of child and adolescent psychiatric disorders on young adult personality disorder. Am J Psychiatry. 1999;156:1529–1535. doi: 10.1176/ajp.156.10.1529. [DOI] [PubMed] [Google Scholar]
- 47.Caspi A, Roberts BW, Shiner RL. Personality development: Stability and change. Annual Reviews of Psychology. 2005;56:453–584. doi: 10.1146/annurev.psych.55.090902.141913. [DOI] [PubMed] [Google Scholar]
- 48.Johnstone EC, Ebmeier KP, Miller P, Owens DG, Lawrie SM. Predicting schizophrenia: Findings from the edinburgh high-risk study. British Journal of Psychiatry. 2005;186:18–25. doi: 10.1192/bjp.186.1.18. [DOI] [PubMed] [Google Scholar]
- 49.Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: I. an 8-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1990;29:546–557. doi: 10.1097/00004583-199007000-00007. [DOI] [PubMed] [Google Scholar]
- 50.Hoza B, Mrug S, Gerdes AC, Hinshaw SP, Bukowski WM, Gold JA, Kraemer HC, Pelham WE, Wigal T, Arnold LE. What aspects of peer relationship are impaired in children with attention-deficit/hyperactivity disorder? Journal of Clinical and Consulting Psychology. 2005;73:411–423. doi: 10.1037/0022-006X.73.3.411. [DOI] [PubMed] [Google Scholar]
- 51.Latimer WW, August GJ, Newcomb MD, Realmuto GMH, Mathy RM. Child and familial pathways to academic achievement and behavioral adjustment: A prospective six-year study of children with and without ADHD. Journal of Attention Disorders. 2003;7:101–116. doi: 10.1177/108705470300700204. J.M. [DOI] [PubMed] [Google Scholar]
- 52.Curtis WJ, Cicchetti D. Moving research on resilience into the 21st century: Theoretical and methodological considerations in examining the biological contributors to resiliences. Developmental Psychopathology. 2003;15:773–810. doi: 10.1017/s0954579403000373. [DOI] [PubMed] [Google Scholar]