Abstract
Objectives
Drawing from cumulative disadvantage theory, this research addresses the following questions: Do hospital admission and discharge rates differ for White and Black adults? If yes, do the differences amplify in later life?
Methods
This study made use of hospital records abstracted from a long-term prospective study of adults in the National Health and Nutrition Examination Survey I: Epidemiologic Follow-up Study (N = 6,833). Semi-Markov models were specified to examine the likelihood of hospital admission and discharge for Black and White adults aged 25 to 74 years old at baseline.
Results
Black adults were less likely than White adults to be admitted to the hospital, but they had longer lengths of stay. The risk of death in the hospital was greater for both Black men and women than for White men and women. In addition, the observed racial differences in hospitalization experiences amplified in later life.
Discussion
Health inequality in America is manifest in how White and Black adults enter and exit hospitals. The findings demonstrate growing heterogeneity in later life by race.
RACIAL health disparities in American society are substantial and manifest on a wide array of indicators, ranging from health ratings to life expectancy. On many but not all measures of life expectancy, morbidity, and mortality, minority or ethnic groups, particularly Black adults, do not manifest the same levels of health as their White counterparts. There is little debate that there is substantial health inequality by racial and ethnic group in American society, but the extent of the gap and the reasons for the inequality are matters of continuing interest (Mechanic, 2005; Smedley, Stith, & Nelson, 2003; Smith, 2005).
As empirical generalizations accumulate on how racial differences in health develop over the life course, recent research points to two innovations that have greatly shaped the course of inquiry. First, research on health disparities in the past decade has moved beyond documentation of Black/White differences in health to more dynamic analyses of health inequality based on longitudinal data. This initiative has been aided by the emergence of the life course perspective in fields such as epidemiology, sociology, and public health, seeking to take the long view in understanding the development of health inequality (Kuh & Ben-Shlomo, 1997).
Second, research has begun to integrate information on the interface between population health and medical care use. Access to and use of medical care are key considerations in understanding racial health disparities, and several studies have prospectively examined medical care use by linking social survey data with Medicare records (e.g., Wolinsky, Culler, Callahan, & Johnson, 1994). These studies have been very helpful for understanding changes in health and medical care use among older people, but their cohort-centric design limits generalizations regarding the life course. Whereas Black people are more likely to experience social and health disadvantages in early life, it is critical to widen the age scope of the analysis when studying racial health inequality.
The present research used a life course perspective to study Black/White disparities in the experience of hospitalization for health problems and accidents during adulthood. We consider hospital episodes as sentinel health events in the life course and sought to determine if there were racial differences in hospital admission, length of stay, and discharge destinations during adulthood. The research draws upon cumulative disadvantage theory to prospectively study the competing risks of hospitalization and mortality in a national sample of adults.
A Cascade of Disadvantage?
Cumulative disadvantage theory provided the framework for this analysis and helped to formulate the research questions. The theory emphasizes how early advantage or disadvantage is critical to how cohorts become differentiated over time. Early risk factors shape trajectories for not only the short-term outcomes but the long-term outcomes as well. On the basis of the theory, one would expect the effects of risk factors to accumulate over the life course, thereby increasing heterogeneity in later life (Dannefer, 1987, 2003; Ferraro, 2006; Ferraro & Kelley-Moore, 2003; O'Rand, 1996). Personal change is seen as closely related to traits or characteristics displayed earlier in the life course. The theory anticipates change, but the nature of the change is conceptually linked with earlier experiences, abilities, and resources (Elder, 1995).
Cumulative disadvantage theory also emphasizes that different trajectories arise from early inequalities. Some persons are advantaged in their early years, and this advantage may compound over time. Others are disadvantaged because of genetic or environmental factors, and these disadvantages also accumulate (Preston, Hill, & Drevenstedt, 1998). In a sense, one may think of this as a cascade of disadvantage whereby early events and experiences precipitate additional risks. As the risks accumulate over the life course, one would anticipate that this would increase diversity in a population.
As it pertains to the study of cumulative disadvantage and health, epidemiologic studies in the past decade have given more attention to the early origins of health problems in adulthood and older ages. According to Wadsworth (1997), there is a growing interest in taking a “lifetime view of the natural history of some common serious illnesses which usually begin in middle or later life” (p. 860). If the inequalities develop earlier in life, then one can expect growing divergence in health trajectories due to the accumulation of risk factors. The life course involves a series of challenges to health for all people, but for those with early disadvantages, the timing and severity of the cascade is distinct (Ferraro, Farmer, & Wybraniec, 1997; Verbrugge & Jette, 1994). Thinking of the structure of disadvantage in American society, one would anticipate that the cascade of disadvantage would occur sooner and be more severe for Black people.
There is ample evidence to show that the Black population is health disadvantaged. For instance, life expectancy for Black people has lagged behind that for White people throughout this century, and there is no compelling evidence that the gap has shrunk in recent years. Indeed, there is some evidence that the gap has widened since the mid-1980s (Kochanek, Maurer, & Rosenberg, 1994; U.S. Department of Health and Human Services, 2003). The substantial health disparity between White and Black Americans led to the formulation of many of the overall aims and specific goals of Healthy People 2000 and Healthy People 2010. Although these objectives have been in place for more than a decade, progress has been limited to a small set of indicators (U.S. Department of Health and Human Services, 1998). And for some objectives, there has been no progress at all (e.g., obesity among Black adults; National Heart, Lung, and Blood Institute, 1998; U.S. Department of Health and Human Services, 2003).
Hospitalization Among Persons of Color
Given the racial health inequality in American society, one might expect higher rates of hospitalization among Black adults. Indeed, some studies have found that health needs are closely related to hospitalization and that Black adults are more likely than White adults to be hospitalized (e.g., Gornick et al., 1996). However, some studies have reported lower rates of hospitalization for Black older adults (e.g., Callahan & Wolinsky, 1996; Wolinsky et al., 1994), and others have found no racial differences at all (Mutchler & Burr, 1991; Stearns, Kovar, Hayes, & Koch, 1996). Perhaps the most striking finding from the literature is that many studies, including some in the past decade, did not even test for differences in the likelihood of hospitalization between White and Black adults (e.g., Miller et al., 1998).
Investigators in recent years have been increasingly interested in the timing of hospitalization, the duration of the stay, and return visits. The timing of a hospital stay is important because delay may be costly in both prognostic and economic terms, especially for selected conditions such as cancer and heart disease. Research based on hospital-record review showed that Black adults were more likely to experience delayed hospitalizations (Weissman, Gatsonis, & Epstein, 1992) that led to “worse processes of care” (Kahn et al., 1994. p. 1169). Although these studies are useful for identifying racial differences in health service use, the reliance on hospital record data means that the sample included only those who were hospitalized during the interval studied. We are unaware of any prospective panel studies of national probability samples of adults that have used continuous time models in order to examine the timing of hospitalization by race.
If it is the case that Black persons’ hospitalizations are delayed, then there may be substantial consequences on health trajectories and subsequent hospitalization. Might delayed hospitalizations lead to longer lengths of stay—to handle more advanced disease sequelae? If Black adults enter hospital care later in the disease process and have similar lengths of stay, might this lead to greater discharge instability and/or rehospitalization? Findings from the extant literature are sketchy on this issue, but it is conceivable that Black adults may be at greater risk than White adults for adverse hospitalization experiences as a result of the delayed entry into the system.
The purpose of the current research is to prospectively examine hospitalization experiences of Black and White adults over 15 years. With data from a national sample of community-dwelling adults, we reconstructed a hospital life history for each participant and examined hospital admissions, lengths of stay, and discharge destinations that occurred during that time period. Three research questions guided the analysis. First, given the greater morbidity and shorter life expectancy of Black adults, is their rate of hospitalization different from or similar to that of White adults? Second, are Black adults less likely than White adults to be discharged alive? Third, if there is a racial difference in the hospitalization experience, does the gap widen, shrink, or remain stable over the adult life course?
Methods
Sample
This study utilized a combination of survey data and hospital records spanning a period of 15 years from the National Health and Nutrition Examination Survey (NHANES) and its Epidemiologic Follow-up Study (NHEFS). NHEFS staff conducted baseline interviews from 1971 to 1975. The sampling design was a multistage, stratified probability sample of noninstitutionalized persons aged 25 to 74 years at baseline (N = 6,833). Further details of the sampling frame and data collection appear elsewhere (Cornoni-Huntley & Huntley, 1990). NHEFS staff conducted three follow-up interviews: the first between 1982 and 1984, the second in 1987, and the third in 1992. Given the substantial changes in federal Medicare policy in 1986 in order to implement a prospective payment system based on diagnostic related groups, we limited the current analysis to the period between 1971 and 1985. (In a separate article now in progress, we examine racial differences in hospitalization before and after the prospective payment system.)
Measurement of Hospitalization
At each follow-up interview, NHEFS staff asked respondents whether they had been hospitalized overnight since the previous interview. For each stay reported by the respondent, the interviewer recorded the length of stay, reason for stay, and approximate date. Each participant gave consent to NHEFS staff to confirm these reported hospital stays through medical records. Independent research staff then attempted to match reported hospital stays with facility records and, in some cases, death certificates. NHEFS staff considered a stay to match an existing record if the reported date was within 1 year of the date of stay for the hospital record and if any of the diagnoses referred to the body system reported by the respondent (e.g., participant admitted for myocardial infarction, and participant reported hospitalized for “heart”). We examined racial differences in the likelihood of a matching record for each reported hospitalization, but observed no significant differences (in willingness to authorize record collection or in matching records to reports).
The NHEFS staff also recorded all other hospitalizations not reported by the respondent (including more than 2,604 stays identified in proxy interviews for deceased respondents). We eliminated from the analyses those hospital stays that had been reported by the respondent but that could not be confirmed or matched with facility records. Thus, the present analysis made use of 77% of all self- or proxy-reported hospital stays for which hospital records could be matched.
For each recorded hospital stay, we obtained the following information: date of admission, date of discharge, discharge destination, and diagnosis (based on the International Classification of Diseases, Ninth Revision, Clinical Modification). We determined some stays to be out of the scope of the present study and eliminated them: hospitalizations for child birth (n = 181), mental health facility stays (n = 87), and nursing home (or rehabilitation center) stays (n = 761). We included hospitalizations for pregnancy-related complications, but we excluded visits for birthing without complications. The aim of the analysis was to examine racial differences in hospitalization due to physical health problems or accidents. Given the higher fertility of Black women, inclusion of birthing visits without complications would likely have obscured racial disparities. NHEFS staff did not systematically collect data for stays in psychiatric hospitals and nursing homes, but did so only if linked to a stay in an acute care hospital. We also excluded from the analysis 9 hospital stays that had a psychiatric diagnosis (e.g., schizophrenia) and that were longer than 200 days. Model specification with these stays would not have been representative of the universe of such stays; thus, we coded these persons as not having been in a hospital during the period of a psychiatric or nursing home stay.
There were also 363 hospital stays that involved a transfer to another hospital. We treated the two contiguous stays as one stay if the transfer occurred within 3 days of the first admission and if both stays shared the same basic International Classification of Diseases code. Using these decision rules, we recoded 12 episodes of apparent transfers into single stays. We based the analysis upon 6,114 persons, of whom 2,603 persons (38.09% of the total sample) had not been hospitalized during the period of observation. There were 10,442 confirmed hospitalizations among 3,511 persons during the 15-year period.
Measurement of Predictor Variables
Unless otherwise noted, all of the independent variables were measured at baseline. Table 1 presents descriptive statistics by hospitalization status and by race. We coded age in years reported at the baseline survey, ranging from 24 to 77. Black and female were binary variables (scored with 1 = the category expressed in the title of the variable, 0 = otherwise). We coded income as a binary variable based on income at the baseline survey (1971−1975): 1 = income greater than or equal to $15,000 per year. (Although this amount seems quite low, the threshold in 1971 is equivalent to $72,938 in 2005 with inflation-adjusted dollars.) We constructed morbidity variables from questions that asked the respondents if a doctor had ever told them that they had selected conditions. We classified individuals who either had had a heart attack or had heart failure as having heart trouble. Binary variables also identified diabetes and arthritis.
Table 1.
Means and Standard Deviations of Variables Within Hospitalization Status Stratum by Race
| Hospitalization Status |
||||||
|---|---|---|---|---|---|---|
| Never Hospitalized |
Hospitalizeda |
|||||
| Variable | Total (n = 2,603) | Black (n = 386) | White (n = 2,217) | Total (n = 3,511) | Black (n = 415) | White (n = 3,096) |
| Black | .148 | .118 | ||||
| Age (yrs) | 44.5 (13.9) | 47.6 (14.0) | 43.9***b (13.9) | 51.6 (13.8) | 51.9 (14.0) | 51.6 (13.7) |
| Female | .551 | .572 | .547 | .537 | .528 | .538 |
| Incomec | .484 | .186 | .536*** | .438 | .229 | .466*** |
| Married | .746 | .551 | .779*** | .781 | .612 | .803*** |
| Heart troubled | .045 | .057 | .043 | .093 | .135 | .088** |
| Diabetes | .031 | .051 | .027* | .070 | .113 | .064*** |
| Arthritis | .182 | .215 | .177 | .301 | .333 | .296 |
| Rural | .329 | .228 | .347*** | .439 | .294 | .458*** |
| South | .228 | .199 | .233 | .269 | .260 | .270 |
| Obesity | .190 | .316 | .168*** | .264 | .330 | .255** |
| Smoker | .447 | .502 | .438* | .406 | .513 | .392*** |
Notes: We coded all binary variables 0 and 1 (we have omitted standard deviations for binary variables). The mean of a binary variable scored 0 and 1 is the percentage of cases with that attribute. We included additional independent variables in preliminary analyses but omitted from the final specifications those that were not significant for any outcomes. Data are from the National Health and Nutrition Examination Survey I Epidemiologic Follow-up Study, 1971−1985.
Individuals who were admitted at least once.
Significance is indicated for the comparison between each variable by race within each stratum of hospitalization status.
0 = income less than $15,000 per year at baseline; 1 = income of $15,000 or more per year at baseline.
1 = individuals who responded “yes” to being told they either had had a heart attack or had heart failure.
p < .05
p < .01
p < .001.
Given the importance of location to disparities in health service use, we included binary variables for rural and South (Baiker, Chandra, & Skinner, 2005). We also controlled two variables related to health behavior. We defined obesity as a body mass index greater than or equal to 30 (National Heart, Lung, and Blood Institute, 1998), and we identified smokers based on self-reported use of cigarettes, cigars, and pipes at the time of the survey. Based on research related to variability in health service use by marital status, we also included a binary variable that identified married persons (Iwashyna & Christakis, 2003). We considered additional independent variables in preliminary analyses. The variables considered, but deleted from further consideration due to a lack of a significant relationship with any of the outcomes, included education, private insurance, receipt of Medicaid, recreational exercise, past smoker, and several disease indicators (hypertension, cancer, cataracts, kidney trouble, and hip fracture).
Transition Model
For each respondent, we thought of the 15-year follow-up as a tape measure on which one could mark off periods of time spent in one of three states. As depicted in Figure 1, the states examined in this study were dwelling in the community (State 0), hospitalized (State 1), and dead (State 2). We arrayed the data so that there was a 15-year record for each case that identified daily occupancy in the three states. With the full tape measure demarcated with duration in the three states, we estimated transitions across these states with a generalization of a semi-Markov model. As is shown in Figure 1, all NHEFS participants began the study dwelling in the community. The probability of transitioning between states is indicated by P. Some participants were hospitalized (P01) and returned home (P10), but others died while in the hospital (P12). Still others died without an observed hospitalization (P02). Death is an absorbing state, so P22 = 1.
Figure 1.
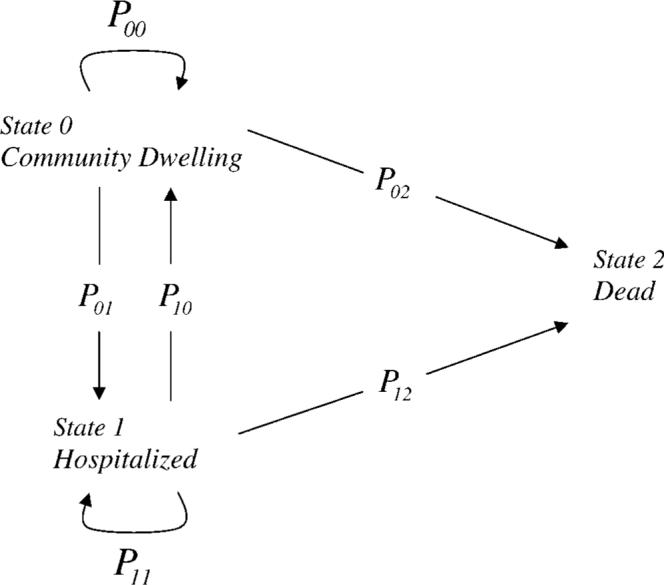
Generalization of the semi-Markov model of the hospitalization of adults. Possible changes of states include entering the hospital (P01), discharge from the hospital (P10), death while dwelling in the community (P02), and death while in the hospital (P12). Probabilities for remaining in the same state are: staying healthy (P00), staying in the hospital (P11), and death (P22 = 1). The probabilities satisfy the condition that the sum of the probabilities assigned the outgoing arrows of a state is 1.
Given the differences in the transition probabilities across the three states, we examined different time periods for the various outcomes. The time periods selected for the final analyses were 1 year for the likelihood of hospital admission, 2 weeks for the likelihood of returning home from the hospital, 2 weeks for death in the hospital, and 5 years for death in the community. These choices were meaningful for each outcome and ensured adequate statistical power in the estimation of parameters. We should note that the time periods specified do not right censor cases from the analysis. We simply used the duration periods in order to identify each risk pool and express the probabilities relative to the likelihood of an event.
Statistical Methods
We analyzed the data by using a framework based on semi-Markov models, whereby the length of time spent in a state was a Weibull random variable with parameters that depended on covariates. We chose Weibull distributions in order to account for the skewness observed in the data.
If we let w represent the (natural) log of the time spent in a state, then the probability density of w is
| (1) |
and the survival distribution function is
| (2) |
One can use the survival distribution function in order to calculate probabilities for any specified value of w. The probability that the log of the time spent in a state is w or less is 1 – S(w). The model includes explanatory variables through the term μ. Specifically, μ = β0 + β1x1 + ... + βpxp where β0, β1, ... βp are parameters to be estimated, and x1, ... , xp are the explanatory variables. This framework provides an analytical tool similar to multiple linear regression in that we can include indicator variables and interactions in our model.
The data analyzed are censored in several ways. First, all respondents were community dwelling at the time of enrollment, but we did not know how long they had been in this state before that time. Thus, all data are left censored for the time in this state. Similarly, for respondents who had not been hospitalized and did not die during the period of observation, the time in the community dwelling state is right censored.
Race, gender, and age were the three primary explanatory variables of interest, but the analyses also included all of the other variables described in Table 1. Because the estimated parameters of the Weibull models are not directly interpretable, we used the models in order to estimate the transition probabilities within selected periods of time. We used the SAS LIFEREG procedure (SAS Institute, Cary, NC) for these analyses. It allows fitting of Weibull distributions with explanatory variables and censoring.
Results
Descriptive statistics in Table 1 revealed that 2,603 (42.6%) respondents were never hospitalized during the study period, whereas 3,511 (57.4%) had been hospitalized at least once. Those respondents who had been hospitalized at least once were more likely to be White, to be older, to be married, to reside in the South or in a rural part of the country, to be obese, and to have lower annual income than respondents who were never hospitalized. In addition, respondents who had been hospitalized were more likely to have the following health conditions compared to respondents who were never hospitalized: heart trouble, diabetes, and arthritis.
We began the multivariate analysis by estimating hospitalization transition probabilities for Black and White men and women. This Weibull model included the covariates listed in Table 1 (including age at baseline) as well as cross-product terms in order to test interactions: Age × Race and Age × Gender. Using the coefficients from this model, we estimated the probability of a transition from residing in the community to the hospital within 1 year (P01 in Figure 1) for each Race × Gender combination as a function of age. The results plotted in Figure 2 are based on participant's age at the baseline interview (e.g., 25−74 years old).
Figure 2.
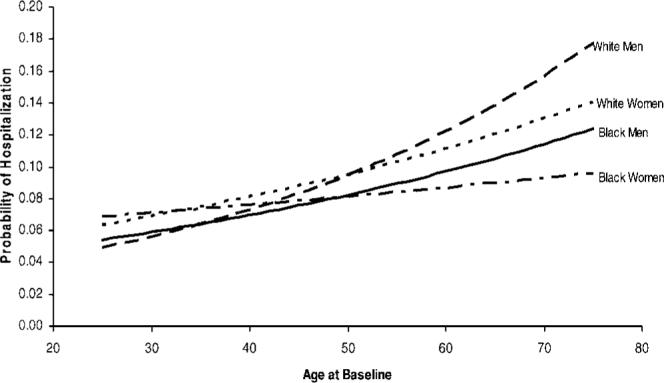
Transition probabilities from Community Dwelling to Hospitalized within 1 year by race and gender.
The results revealed that Black and White adults were hospitalized at fairly similar rates in early adulthood but that Black adults were less likely to be hospitalized in later life. Black and White hospitalization rates increased with age, but the rate of increase was greater for White men and White women than for their Black counterparts—note the racial crossover for men and for women. Women were slightly more likely than men to be hospitalized in early adulthood, but the pattern reversed, and the magnitude of the differences amplified in later life. For example, the youngest men—Black or White—had about a 5% chance of being hospitalized within 1 year compared with a nearly 7% chance for the youngest women (Black or White). By the age of 65, however, Race × Gender differentiation was clear: The chance of being hospitalized was about 9% for Black women, 11% for Black men, 12% for White women, and almost 14% for White men. On the basis of genetics and physiology, one would expect greater similarity by gender than race, but such was not the case with adult hospital admissions.
Figure 3 presents the transition probabilities from hospitalization to death, again controlling for status characteristics and morbidity, but this time with age at hospitalization (instead of age at baseline). The estimated transition probabilities referred to the likelihood of dying in the hospital within 2 weeks of admission (P12 in Figure 1). The results summarized graphically in Figure 3 revealed that women had lower hospital mortality risk in the first 2 weeks after admission than men regardless of race but that Black people of each gender were at much higher risk for dying. For instance, the chance of dying in the hospital within 2 weeks was almost 7% for a young Black man and about 5% for a young White man. The chance of dying in the hospital increased with age for both White and Black men and women, but the racial disparity amplified in later life. The risk of hospital death for the oldest participants was lowest for White women and highest for Black men.
Figure 3.
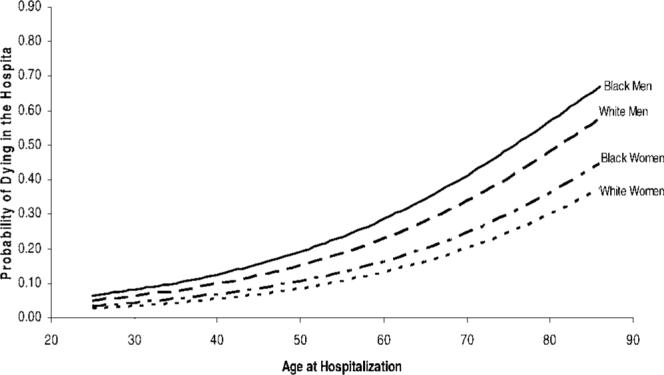
Transition probabilities from Hospital to Dead within 2 weeks by race and gender.
We saw a similar pattern for individuals who died outside of the hospital (P02 in Figure 1). We adjusted these transition probabilities for all of the variables in Table 1 (including age at baseline) as well as product terms for Age × Race and Age × Gender. As is shown in Figure 4, Black men and women had a greater chance of dying within 5 years than did their White counterparts. These differences grew appreciably from early to late adulthood. For instance, the difference in the probability of death between White women and Black men was about 2% at age 25 and 18% by age 74. Among women, the racial disparity increased from 0.5% at the youngest age to about 6% by the oldest age. Among men, the racial disparity grew from less than 2% to more than 5% over the adult life course.
Figure 4.
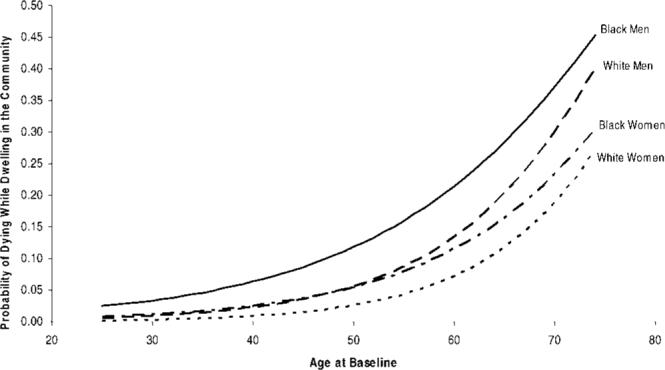
Transition probabilities from Community Dwelling to Dead within 5 years by race and gender.
The final model for transition probabilities from the hospital to the community reflected P10 in Figure 1 and included the covariates in Table 1, but with age at hospitalization and an interaction term for Age × Gender. Transition probabilities are plotted by age at hospitalization in Figure 5. White adults had higher rates of returning to the community than did Black adults. White women had a higher return rate than did White men, but the probability was nearly identical for Black women and Black men. A young White man had about an 86% chance of returning back to the community within 2 weeks, whereas a young Black man had about a 78% chance. Gender differences for White adults were fairly constant across age of hospitalization. The racial difference, however, was fairly substantial and persisted across the life course.
Figure 5.
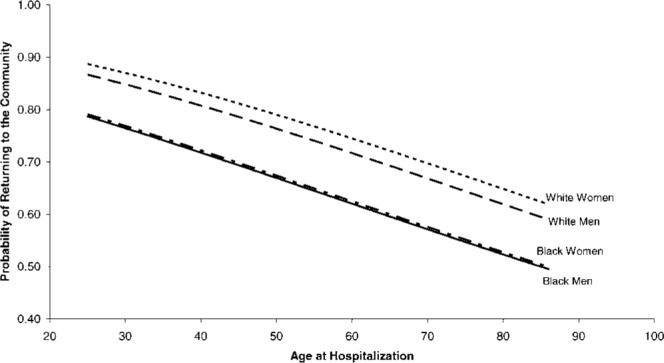
Transition probabilities from Hospitalized to Community Dwelling within 2 weeks by race and gender.
In supplementary analyses we also examined hospital length of stay (P11 in Figure 1). Although Black adults were less likely than White adults to be admitted to the hospital, they had longer lengths of stay. Whether the first or last stay, Black adults spent on average 3 more days in the hospital than did their White counterparts.
Discussion
Findings from the present investigation revealed that hospitalization is both a consequence and cause of racial health inequality in American society. Drawing from cumulative disadvantage theory, we sought to determine if hospitalization experiences are distinct for Black and White adults. Their experiences are clearly distinct and reveal a cascade of disadvantage for Black people.
Our first main research question focused on whether there are racial differences in the rate of hospital admission. Results from a 15-year prospective follow-up of a national sample revealed that the likelihood of hospital admission was greatest for White men and lowest for Black women. In fact, hospital admission rates were higher for both White men and women than for Black men and women. This is an important finding and adds evidence to those studies that show that Black adults, particularly in later life, have lower hospitalization rates (Callahan & Wolinsky, 1996; Wolinsky et al., 1994). The findings of other studies (e.g., Stearns et al., 1996) are not consistent with this pattern, but the conclusion was consistent in our analyses even after we controlled for income (and tested for differences by education, private medical insurance, and receipt of Medicaid). On the basis of genetics, one would expect that gender (i.e., Y chromosome) would be stronger than race in differentiating a population. The differences in later life, however, show that race is more important than gender in predicting hospital admissions, which demonstrates the severe consequences of social inequality by race over the life course.
A related finding is that racial differences in hospital admission increased during adulthood. Hospital admission rates in early adulthood were nearly identical for Black and White men or for Black and White women. Racial differentiation increased in middle age and reached about 5% for older persons. This pattern occurred for both men and women, which provides ample evidence of growing racial inequality and heterogeneity with age.
Entry into the hospital is one dimension of the hospitalization experience, but a second research question addressed racial differences regarding exit from the hospital. First, although Black adults had lower admission rates than Whites, they had longer stays once admitted. This finding may seem paradoxical at first, but it is consistent with interpretations on the consequences and costs of forgoing preventive care. As other investigators have suggested, delayed care leads to additional problems in care (Kahn et al., 1994; Weissman et al., 1992). In terms of cumulative disadvantage theory, delayed entry into the medical system leads to accumulated medical risks.
Not only were Black adults more likely to have longer stays, but their discharge destinations were also different from those of White adults. Black adults, especially Black men, were more likely to die in the first 2 weeks of a hospital stay. This racial disparity for men was about 2% in early adulthood but rose to 7% by the seventh decade of life. The racial disparity for women was present as well but was more modest. To summarize the racial disparity, the Black population had fewer entries into the hospital but more fatal exits after admission. This was especially the case for Black men.
Our interpretation of racial disadvantage for Black people assumes that hospital use among White people was at appropriate or medically reasonable levels. An alternative interpretation is that there were excess (i.e., unnecessary) hospitalizations among White people. Such an interpretation may seem plausible when considering admissions alone, but the higher rate of mortality suffered by Black adults who were admitted to the hospital renders this interpretation less plausible. Indeed there is ample evidence in these analyses, from admission to discharge, of systemic inequality by race that disadvantages people of color.
A third major research question we sought to answer was whether the racial gap widens, shrinks, or remains stable over the adult life course. The answer to this question is unequivocal when it comes to hospitalization: The racial gap in hospitalization increases over the adult life course. There were minor differences in admission rates in early adulthood, but there was a major disadvantage for Black people in later life. Whether it was entry into or exit from the hospital, the racial disparity widened with age. Inequality increased over the life course, and the longer stays and greater hospital mortality for Black people were likely the consequences, at least to some degree, of lower admission rates and untreated morbidity. For the field of gerontology, the evidence herein shows increasing heterogeneity within the Black and White subsamples. At the same time, these results show that race remains an important source of variability over the life course in further differentiating a population as it ages.
There are at least three important limitations to consider when interpreting these findings. First, the conclusions may not apply to current hospitalization patterns. We took advantage of a unique data archive in order to answer several questions about minority aging and hospitalization over a 15-year observation period. We also addressed the theoretical issue in gerontology of increasing heterogeneity with age. It is possible, however, that the racial disparities observed here vanished with the prospective payment system based on diagnostic related groups and/or the move toward managed care. We doubt the validity of this interpretation, and we are considering racial disparities in hospitalization before and after the prospective payment system in analyses for a related article.
Second, the NHANES data do not have official hospital records for all reported stays. Although more than 75% of the reported stays have abstracted records, it is possible that some of the reported stays for which there are no abstracted records might influence the conclusions. Readers should interpret the findings with caution because of the missing data as well as the exclusion of nursing home stays from the data. We anticipate, however, that bias due to incomplete hospital records is small for at least two reasons. First, the NHEFS criteria for matching a self-reported hospital stay with a hospital record were quite generous. If the reported stay was within 1 year of the actual hospitalization and included the same general bodily system, study organizers considered the stay to be a match. Second, the two greatest sources of discontinuity between self-reported and abstracted hospital records were (a) respondent-reported visits to the hospital that did not result in an overnight stay and that we thus considered out of the scope of this study, and (b) the fact that some respondents with a substantial number of hospitalizations may have given an inflated estimate of hospital events (e.g., participant reported 60 hospitalizations, but NHEFS found records for only 54).
Third, we should note that NHANES had a cap on the age of respondents at the first interview: 74 years. By the end of the study, the respondents who survived were 89 years old, but the age ceiling limits conclusions from the study. The applicability of the findings to people in advanced old age awaits further study. Although the racial mortality crossover in life expectancy may suggest that the Black/White differences in hospitalization would reduce in advanced age (Ferraro, 2006), the NHEFS data do not permit a thorough test of this issue.
Even after considering the limitations of the present research, we believe this article makes important contributions to both health services research and gerontology. A prospective 15-year follow-up of a national sample revealed that, compared with White people, Black people are less likely to be admitted to the hospital, are more likely to have longer lengths of stay after admission, and are less likely to be discharged alive within 2 weeks after an admission. Less entry and more fatal exits show clearly that Black people in need of hospitalization have experiences distinct from those of White persons. The analyses presented herein compared the hospitalization experiences of Black and White adults, and we welcome research on other ethnic groups to better understand the breadth and depth of disparities in health service use. There is a dearth of equivalent data for other groups, but we hope that these analyses will stimulate parallel studies on other groups of color.
Two additional areas of research hold great promise for advancing researchers’ understanding of disparities in health service use. First, a growing body of research shows that the physicians who provide the majority of medical care to people of color are different from physicians whose caseloads are largely populated by non-Hispanic White people (Bach, Pham, Schrag, Tate, & Hargraves, 2004; Smith, 1998). Black and White people who use medical care may activate different networks of service—networks that may be quite consequential to health outcomes. Second, future research that can identify the services used while in the hospital may hold the key to understanding racial disparities after admission. Do the patterns observed in this study apply to cardiac intensive care as well? Do procedures vary for Black and White people presenting with similar conditions? Many factors are involved in the generation of racial disparities in health and health service use, but these questions are logical next steps for this line of inquiry.
These findings also provide evidence for cumulative disadvantage theory, pointing to a cascade of disadvantage for Black people. It is clear from these analyses that race is a major axis of accumulating risk and inequality in American society, even after controlling for socioeconomic resources. Aging was associated with greater heterogeneity over the adult life course, and the racial differences amplified in later life.
Acknowledgments
Support for this research was provided by grants AG11705 and AG01055 from the National Institute on Aging to Kenneth F. Ferraro. An earlier version of this article was presented at the 2003 Annual Scientific Meeting of The Gerontological Society of America, San Diego, CA. We thank Angela C. Henderson, Tetyana P. Shippee, and Douglas A. Wolf for helpful comments on an earlier version of the article. The data were made available by the Inter-University Consortium for Political and Social Research, Ann Arbor, MI. Neither the collector of the original data nor the Consortium bears any responsibility for the analyses or interpretations presented here.
References
- Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat Blacks and Whites. New England Journal of Medicine. 2004;351:575–584. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- Baiker K, Chandra A, Skinner JS. Geographic variation in health care and the problem of measuring racial disparities. Perspectives in Biology and Medicine. 2005;48:S42–S53. [PubMed] [Google Scholar]
- Callahan C, Wolinsky FD. Hospitalization for pneumonia among older adults. Journal of Gerontology: Medical Sciences. 1996;51A:M276–M282. doi: 10.1093/gerona/51a.6.m276. [DOI] [PubMed] [Google Scholar]
- Cornoni-Huntley JC, Huntley RR. Health status and well-being of the elderly: National Health and Nutrition Examination Survey I: Epidemiologic follow-up study. Oxford University Press; New York: 1990. [Google Scholar]
- Dannefer D. Aging as intracohort differentiation: Accentuation, the Matthew effect, and the life course. Sociological Forum. 1987;2:211–236. [Google Scholar]
- Dannefer D. Cumulative advantage/disadvantage and the life course: Cross-fertilizing age and the social science theory. Journal of Gerontology: Social Sciences. 2003;58B:S327–S337. doi: 10.1093/geronb/58.6.s327. [DOI] [PubMed] [Google Scholar]
- Elder GH., Jr. The life course paradigm: Social change and individual development. In: Moen P, Elder GH Jr., Luscher K, editors. Examining lives in context: Perspectives on the ecology of human development. American Psychological Association; Washington, DC: 1995. pp. 101–139. [Google Scholar]
- Ferraro KF. Health and aging. In: Binstock RH, George LK, editors. Handbook of aging and the social sciences. 6th ed. Elsevier; 2006. pp. 238–256. [Google Scholar]
- Ferraro KF, Farmer MM, Wybraniec J. Health trajectories: Long-term dynamics among Black and White adults. Journal of Health and Social Behavior. 1997;38:38–54. [PubMed] [Google Scholar]
- Ferraro KF, Kelley-Moore J. Cumulative disadvantage and health: Long-term consequences of obesity? American Sociological Review. 2003;68:707–729. [PMC free article] [PubMed] [Google Scholar]
- Gornick M, Eggers P, Reilly T, Mentnech R, Fitterman L, Kucken L, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. New England Journal of Medicine. 1996;335:791–799. doi: 10.1056/NEJM199609123351106. [DOI] [PubMed] [Google Scholar]
- Iwashyna TJ, Christakis NA. Marriage, widowhood, and health-care use. Social Science & Medicine. 2003;57:2137–2147. doi: 10.1016/s0277-9536(02)00546-4. [DOI] [PubMed] [Google Scholar]
- Kahn KL, Pearson ML, Harrison ER, Desmond KA, Rogers WH, Rubenstein LV, et al. Health care for Black and poor hospitalized Medicare patients. Journal of the American Medical Association. 1994;271:1169–1174. [PubMed] [Google Scholar]
- Kochanek KD, Maurer JD, Rosenberg HM. Why did Black life expectancy decline from 1984 through 1989 in the United States? American Journal of Public Health. 1994;84:938–944. doi: 10.2105/ajph.84.6.938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuh D, Ben-Shlomo Y. A life course approach to chronic disease epidemiology. Oxford University Press; New York: 1997. [PubMed] [Google Scholar]
- Mechanic D. Policy challenges in addressing racial disparities and improving population health. Health Affairs. 2005;24:335–338. doi: 10.1377/hlthaff.24.2.335. [DOI] [PubMed] [Google Scholar]
- Miller JE, Russell LB, Davis DM, Milan E, Carson JL, Taylor WC. Biomedical risk factors for hospital admissions in older adults. Medical Care. 1998;36:411–421. doi: 10.1097/00005650-199803000-00016. [DOI] [PubMed] [Google Scholar]
- Mutchler JE, Burr J. Racial differences in health and health care service utilization in later life: The effect of socioeconomic status. Journal of Health and Social Behavior. 1991;32:342–356. [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute . Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults (National Institutes of Health Publication No. 98−4083) National Institutes of Health; Bethesda, MD: 1998. [Google Scholar]
- O'Rand A. The precious and the precocious: Understanding cumulative disadvantage and cumulative advantage over the life course. The Gerontologist. 1996;36:230–238. doi: 10.1093/geront/36.2.230. [DOI] [PubMed] [Google Scholar]
- Preston SH, Hill ME, Drevenstedt GL. Childhood conditions that predict survival to advanced ages among African Americans. Social Science & Medicine. 1998;47:1231–1246. doi: 10.1016/s0277-9536(98)00180-4. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal treatment confronting racial and ethnic disparities in health care. National Academies Press; Washington, DC: 2003. [PubMed] [Google Scholar]
- Smith DB. The racial segregation of hospital care revisited: Medicare discharge patterns and their implications. American Journal of Public Health. 1998;88:461–463. doi: 10.2105/ajph.88.3.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DB. Racial and ethnic health disparities and the unfinished civil rights agenda. Health Affairs. 2005;24:317–324. doi: 10.1377/hlthaff.24.2.317. [DOI] [PubMed] [Google Scholar]
- Stearns SC, Kovar MG, Hayes K, Koch GG. Risk indicators for hospitalization during the last year of life. Health Services Research. 1996;31:49–69. [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . Healthy people 2000: Progressive review of Black Americans. U.S. Government Printing Office; Washington, DC: 1998. [Google Scholar]
- U.S. Department of Health and Human Services . Health, United States 2003. U.S. Department of Health and Human Services, Centers for Disease and Control, National Center for Health Statistics; Hyattsville, MD: 2003. [Google Scholar]
- Verbrugge LM, Jette AM. The disablement process. Social Science & Medicine. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Wadsworth ME. Health inequalities in the life course perspective. Social Science & Medicine. 1997;44:859–869. doi: 10.1016/s0277-9536(96)00187-6. [DOI] [PubMed] [Google Scholar]
- Weissman JS, Gatsonis C, Epstein AM. Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland. Journal of the American Medical Association. 1992;268:2388–2394. [PubMed] [Google Scholar]
- Wolinsky FD, Culler SD, Callahan C, Johnson RJ. Hospital resource consumption among older adults: A prospective analysis of episodes, length of stay, and charges over a seven-year period. Journal of Gerontology: Social Sciences. 1994;49:S240–S252. doi: 10.1093/geronj/49.5.s240. [DOI] [PubMed] [Google Scholar]


