Abstract
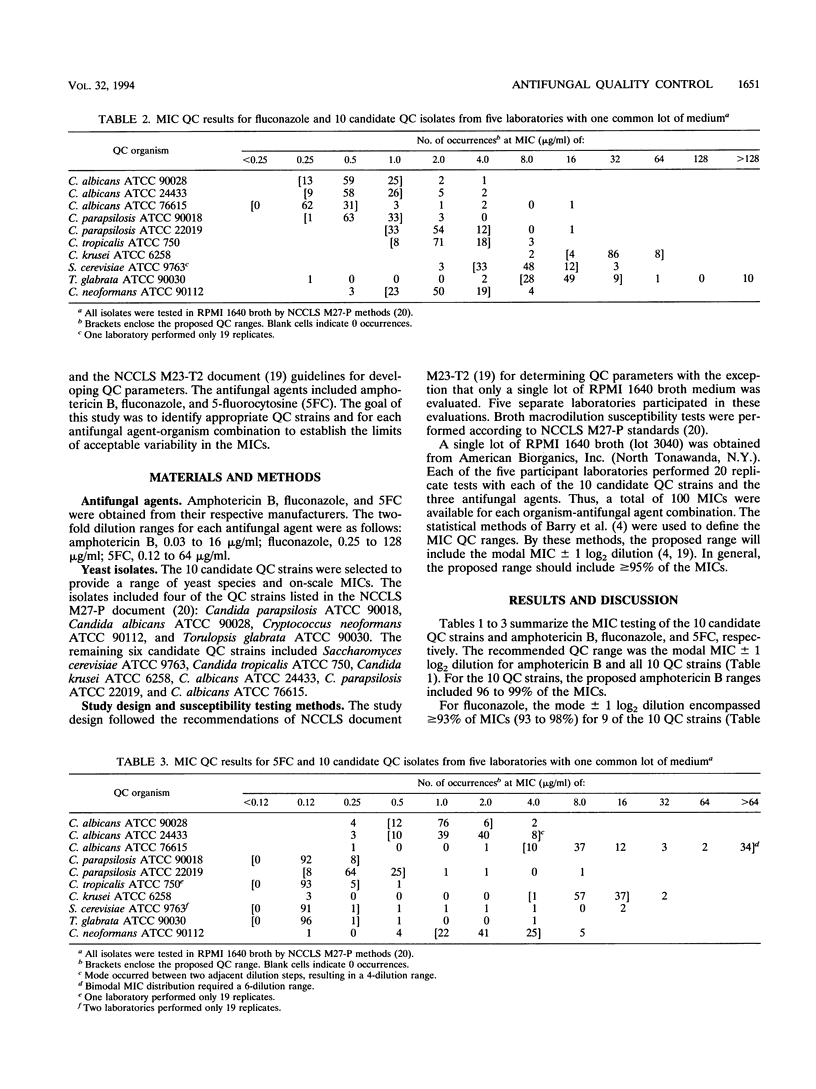
The National Committee for Clinical Laboratory Standards has developed a proposed standard method for in vitro antifungal susceptibility testing of yeast isolates (National Committee for Clinical Laboratory Standards, document M27-P, 1992). In order for antifungal testing by the M27-P method to be accepted, reliable quality control (QC) performance criteria must be developed. In the present study, five laboratories tested 10 candidate QC strains 20 times each against three antifungal agents: amphotericin B, fluconazole, and 5-fluorocytosine. All sites conformed to the M27-P standards and used a common lot of tube dilution reagents and RPMI 1640 broth medium. Overall, 98% of MIC results with amphotericin B, 95% with fluconazole, and 92% with 5-fluorocytosine fell within the desired 3-log2 dilution range (mode +/- 1 log2 dilution). Excellent performance with all three antifungal agents was observed for six strains: Candida albicans ATCC 90028, Candida parapsilosis ATCC 90018, C. parapsilosis ATCC 22019, Candida krusei ATCC 6258, Candida tropicalis ATCC 750, and Saccharomyces cerevisiae ATCC 9763. With these strains, 3-log2 dilution ranges encompassing 94 to 100% of MICs for all three drugs were established. Additional studies with multiple lots of RPMI 1640 test medium will be required to establish definitive QC ranges.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anaissie E. J., Bodey G. P., Rinaldi M. G. Emerging fungal pathogens. Eur J Clin Microbiol Infect Dis. 1989 Apr;8(4):323–330. doi: 10.1007/BF01963467. [DOI] [PubMed] [Google Scholar]
- Armstrong D. Treatment of opportunistic fungal infections. Clin Infect Dis. 1993 Jan;16(1):1–7. doi: 10.1093/clinids/16.1.1. [DOI] [PubMed] [Google Scholar]
- Banerjee S. N., Emori T. G., Culver D. H., Gaynes R. P., Jarvis W. R., Horan T., Edwards J. R., Tolson J., Henderson T., Martone W. J. Secular trends in nosocomial primary bloodstream infections in the United States, 1980-1989. National Nosocomial Infections Surveillance System. Am J Med. 1991 Sep 16;91(3B):86S–89S. doi: 10.1016/0002-9343(91)90349-3. [DOI] [PubMed] [Google Scholar]
- Barry A. L., Fuchs P. C., Jones R. N. Statistical criteria for selecting quality control limits for broth microdilution susceptibility tests with 39 different antimicrobial agents. Collaborative Antimicrobial Susceptibility Testing Group. Diagn Microbiol Infect Dis. 1989 Sep-Oct;12(5):413–420. doi: 10.1016/0732-8893(89)90112-0. [DOI] [PubMed] [Google Scholar]
- Bodey G. P. Azole antifungal agents. Clin Infect Dis. 1992 Mar;14 (Suppl 1):S161–S169. doi: 10.1093/clinids/14.supplement_1.s161. [DOI] [PubMed] [Google Scholar]
- Bryce E. A., Roberts F. J., Sekhon A. S., Coldman A. J. Yeast in blood cultures. Evaluation of factors influencing outcome. Diagn Microbiol Infect Dis. 1992 Mar-Apr;15(3):233–237. doi: 10.1016/0732-8893(92)90118-d. [DOI] [PubMed] [Google Scholar]
- Cameron M. L., Schell W. A., Bruch S., Bartlett J. A., Waskin H. A., Perfect J. R. Correlation of in vitro fluconazole resistance of Candida isolates in relation to therapy and symptoms of individuals seropositive for human immunodeficiency virus type 1. Antimicrob Agents Chemother. 1993 Nov;37(11):2449–2453. doi: 10.1128/aac.37.11.2449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espinel-Ingroff A., Kish C. W., Jr, Kerkering T. M., Fromtling R. A., Bartizal K., Galgiani J. N., Villareal K., Pfaller M. A., Gerarden T., Rinaldi M. G. Collaborative comparison of broth macrodilution and microdilution antifungal susceptibility tests. J Clin Microbiol. 1992 Dec;30(12):3138–3145. doi: 10.1128/jcm.30.12.3138-3145.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fromtling R. A., Galgiani J. N., Pfaller M. A., Espinel-Ingroff A., Bartizal K. F., Bartlett M. S., Body B. A., Frey C., Hall G., Roberts G. D. Multicenter evaluation of a broth macrodilution antifungal susceptibility test for yeasts. Antimicrob Agents Chemother. 1993 Jan;37(1):39–45. doi: 10.1128/aac.37.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galgiani J. N., Rinaldi M. G., Polak A. M., Pfaller M. A. Standardization of antifungal susceptibility testing. J Med Vet Mycol. 1992;30 (Suppl 1):213–224. doi: 10.1080/02681219280000911. [DOI] [PubMed] [Google Scholar]
- Galgiani J. N. Susceptibility testing of fungi: current status of the standardization process. Antimicrob Agents Chemother. 1993 Dec;37(12):2517–2521. doi: 10.1128/aac.37.12.2517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman J. L., Winston D. J., Greenfield R. A., Chandrasekar P. H., Fox B., Kaizer H., Shadduck R. K., Shea T. C., Stiff P., Friedman D. J. A controlled trial of fluconazole to prevent fungal infections in patients undergoing bone marrow transplantation. N Engl J Med. 1992 Mar 26;326(13):845–851. doi: 10.1056/NEJM199203263261301. [DOI] [PubMed] [Google Scholar]
- Hadfield T. L., Smith M. B., Winn R. E., Rinaldi M. G., Guerra C. Mycoses caused by Candida lusitaniae. Rev Infect Dis. 1987 Sep-Oct;9(5):1006–1012. doi: 10.1093/clinids/9.5.1006. [DOI] [PubMed] [Google Scholar]
- Harvey R. L., Myers J. P. Nosocomial fungemia in a large community teaching hospital. Arch Intern Med. 1987 Dec;147(12):2117–2120. [PubMed] [Google Scholar]
- Hitchcock C. A., Pye G. W., Troke P. F., Johnson E. M., Warnock D. W. Fluconazole resistance in Candida glabrata. Antimicrob Agents Chemother. 1993 Sep;37(9):1962–1965. doi: 10.1128/aac.37.9.1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison V. A., Haake R. J., Weisdorf D. J. The spectrum of non-Candida fungal infections following bone marrow transplantation. Medicine (Baltimore) 1993 Mar;72(2):78–89. doi: 10.1097/00005792-199303000-00002. [DOI] [PubMed] [Google Scholar]
- Pfaller M. A., Rhine-Chalberg J., Redding S. W., Smith J., Farinacci G., Fothergill A. W., Rinaldi M. G. Variations in fluconazole susceptibility and electrophoretic karyotype among oral isolates of Candida albicans from patients with AIDS and oral candidiasis. J Clin Microbiol. 1994 Jan;32(1):59–64. doi: 10.1128/jcm.32.1.59-64.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfaller M. A., Rinaldi M. G. Antifungal susceptibility testing. Current state of technology, limitations, and standardization. Infect Dis Clin North Am. 1993 Jun;7(2):435–444. [PubMed] [Google Scholar]
- Pfaller M., Wenzel R. Impact of the changing epidemiology of fungal infections in the 1990s. Eur J Clin Microbiol Infect Dis. 1992 Apr;11(4):287–291. doi: 10.1007/BF01962067. [DOI] [PubMed] [Google Scholar]
- Powderly W. G., Kobayashi G. S., Herzig G. P., Medoff G. Amphotericin B-resistant yeast infection in severely immunocompromised patients. Am J Med. 1988 May;84(5):826–832. doi: 10.1016/0002-9343(88)90059-9. [DOI] [PubMed] [Google Scholar]
- Redding S., Smith J., Farinacci G., Rinaldi M., Fothergill A., Rhine-Chalberg J., Pfaller M. Resistance of Candida albicans to fluconazole during treatment of oropharyngeal candidiasis in a patient with AIDS: documentation by in vitro susceptibility testing and DNA subtype analysis. Clin Infect Dis. 1994 Feb;18(2):240–242. doi: 10.1093/clinids/18.2.240. [DOI] [PubMed] [Google Scholar]
- Rex J. H., Pfaller M. A., Rinaldi M. G., Polak A., Galgiani J. N. Antifungal susceptibility testing. Clin Microbiol Rev. 1993 Oct;6(4):367–381. doi: 10.1128/cmr.6.4.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandven P., Bjørneklett A., Maeland A. Susceptibilities of Norwegian Candida albicans strains to fluconazole: emergence of resistance. The Norwegian Yeast Study Group. Antimicrob Agents Chemother. 1993 Nov;37(11):2443–2448. doi: 10.1128/aac.37.11.2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh T. J., Pizzo A. Treatment of systemic fungal infections: recent progress and current problems. Eur J Clin Microbiol Infect Dis. 1988 Aug;7(4):460–475. doi: 10.1007/BF01962595. [DOI] [PubMed] [Google Scholar]
- Weems J. J., Jr Candida parapsilosis: epidemiology, pathogenicity, clinical manifestations, and antimicrobial susceptibility. Clin Infect Dis. 1992 Mar;14(3):756–766. doi: 10.1093/clinids/14.3.756. [DOI] [PubMed] [Google Scholar]
- Wenzel R. P., Pfaller M. A. Candida species: emerging hospital bloodstream pathogens. Infect Control Hosp Epidemiol. 1991 Sep;12(9):523–524. doi: 10.1086/646403. [DOI] [PubMed] [Google Scholar]
- Willocks L., Leen C. L., Brettle R. P., Urquhart D., Russell T. B., Milne L. J. Fluconazole resistance in AIDS patients. J Antimicrob Chemother. 1991 Dec;28(6):937–939. doi: 10.1093/jac/28.6.937. [DOI] [PubMed] [Google Scholar]
- Wingard J. R., Merz W. G., Rinaldi M. G., Johnson T. R., Karp J. E., Saral R. Increase in Candida krusei infection among patients with bone marrow transplantation and neutropenia treated prophylactically with fluconazole. N Engl J Med. 1991 Oct 31;325(18):1274–1277. doi: 10.1056/NEJM199110313251803. [DOI] [PubMed] [Google Scholar]


