ABSTRACT
As it became clear that patients with paraganglioma (PGL) syndromes had a higher risk of multifocal tumors, we changed our surgical strategy to avoid the possibility of bilateral cranial nerve paralysis. The juxtacondylar approach offers advantages for some jugular foramen tumors, including types C and D temporal PGLs. This approach allows exposure of the jugular foramen without skeletonizing or transposing the facial nerve. It improves the surgeon's ability to distinguish between the pars vascularis and the pars nervosa at the jugular foramen, and it helps to save functioning of the lower cranial nerves. There is already considerable experience using the juxtacondylar approach for patients suffering from schwannomas and meningiomas involving the jugular foramen. Some limitations have been noted for using the juxtacondylar approach with jugular PGLs that are related to their vascular nature. In this article we demonstrate its use for the management of eight patients with locally advanced temporal PGLs and how it can be combined with an infratemporal fossa approach.
Keywords: Intrasurgical neuromonitoring, vertebral artery, cervical nerves, paraganglioma, paraganglioma syndromes
The genes responsible for hereditary head and neck paragangliomas (PGLs) were identified in 2000.1,2 Patients with inherited disease have a higher risk of multifocal disease3 than those with sporadic tumors. For these patients, it is very important to consider the implications of surgical management. In particular, the possibility of inflicting simultaneous or consecutive lower cranial nerve deficits and their consequences must be discussed.4 The infratemporal fossa type A approach (and occasionally the type B approach), as described by Fisch,5,6 is recommended for stages C and D temporal PGLs.7 These approaches give an excellent view of the pars vascularis and pars nervosa of the jugular foramen and the jugular bulb but at the expense of the middle ear and with the need to reroute of the facial nerve. In our hands and those of others,8,9,10 transposition of the facial nerve is associated with significant morbidity despite maintaining anatomical continuity. Modifications to the infratemporal fossa type A approach have been suggested to avoid facial nerve transposition.11 We have employed the juxtacondylar approach for the removal of jugular foramen tumors, including types C and D temporal PGLs. In some, it has been combined with an infratemporal approach. The juxtacondylar approach is familiar to neurosurgeons who use it for the resection of intra- and extracranial tumors of the lateral posterior fossa by uncovering the vertebral artery and reducing the bony condyle.12,13,14,15
PATIENTS AND METHODS
We started our program with several cadaver studies, assisted by an experienced neurosurgeon. In this way we learned the anatomical landmarks of the course of the vertebral artery, of the first and second cervical nerve, and of the bony condyle as described by Day et al.16 We evaluated the different surgical steps for the juxtacondylar approach, which included:
Sigmoid course of the skin incision
Soft tissue preparation to uncover the occipital artery and the adjacent venous plexus
Uncovering the first and second cervical nerve
Uncovering the bony course of the vertebral artery and its course to the vertebral angle
Reducing the bony condyle
Uncovering the sigmoid sinus down to the jugular bulb by preserving the labyrinth and the mastoid course of the facial nerve
After this cadaver study, we felt competent to begin our clinical trial supported by experienced neurosurgeons.
Since the year 2000, we have treated eight patients with jugular PGLs by a juxtacondylar approach or by a combined juxtacondylar and Fisch infratemporal fossa type A approach (Table 1). All tumors were staged as a type C or D temporal PGL.6 Every patient underwent genetic evaluation by means of a blood test. Tumors were staged on the basis of computed tomography (CT), magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA). The possibility of secreting tumors was excluded by urine analysis for products of vanillylmandelic acid (VMA) metabolism. Because this approach is performed with the patient in a sitting position, it was important to make sure that the patient did not have a patent septal defect. Preoperative embolization using resorbable particles was performed for all stage C and D tumors. Intraoperative monitoring of the facial and lower cranial nerves was undertaken using a multichannel neuromonitoring system (Inomed). At the beginning of our program, we felt more comfortable when using a navigation system for a controlled reduction of the bony condyle to avoid an unstable craniocervical junction.
Table 1.
Data of Patients with Temporal Paragangliomas; Tumor Classification According to Fisch, 1988
| No. | Patient, Sex, Age | Tumor Stage | Surgical Procedure | Patient's Position during Surgery | Postsurgical Nerve Function |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| N. VII | N. VIII | N. IX | N. X | N. XI | N. XII | |||||
| jc, juxtacondylar approach; vat, vertebral artery transposition; it, combined with Fisch infratemporal fossa type A approach; o, normal; –, palsy. | ||||||||||
| 1 | W.G., f, 59 | C1 | jc, vat | Sitting | o | o | o | o | o | o |
| 2 | W.A., f, 32 | Di2 | jc, vat | Sitting | o | o | o | o | o | o |
| 3 | M.G., f, 63 | B | jc | Laying | o | o | o | o | o | o |
| 4 | B.R., f, 72 | C2 | jc, vat | Sitting | o | o | o | o | o | o |
| 5 | K.E., f, 58 | C1 | jc, vat | Sitting | o | o | o | o | o | o |
| 6 | S.B., f, 47 | C3 | jc/it | Laying | – | o | – | o | – | – |
| 7 | D.G., f. 63 | C1 | jc | Laying | o | o | o | o | o | o |
| 8 | S.E., m, 60 | C2 | jc | Laying | o | o | o | o | o | o |
RESULTS
In the first five cases, we performed an exclusively juxtacondylar approach. Four of these patients had a type C (C1, C2) PGL, and one had a type Di2 temporal PGL (Table 1). Three of them were surgically treated in a sitting position to reduce blood loss when opening the jugular bulb to remove the tumor. In these first three cases, a navigation tool was used to control our reduction of the bony condyle. The surgical steps of the juxtacondylar approach have been described in detail by George et al.17,18 We found it useful to ligate the occipital artery as this reduced tumor blood flow for several hours before new shunts opened. Troublesome bleeding could be encountered close to the occipital artery from a venous plexus, and this could be controlled by electrocoagulation. We also mobilized the internal and external carotid arteries, the jugular vein, and the lower cranial nerves but did not have to ligate the external carotid artery or its branches. The course of the vertebral artery is subject to variation. In all our patients, the vertebral artery was incompletely covered by bone and this simplified its identification. In some cases (Table 1), it had to be displaced in order not to obstruct access to the jugular bulb (Fig. 1). This allowed us to reduce the condyle sufficiently to expose the jugular bulb and the entire sigmoid sinus. A small part of the anterior and posterior bony wall of the jugular bulb remains. Ligation of the jugular bulb is not possible via the juxtacondylar approach, so after opening the jugular bulb and removing the tumor the vessel has to be closed as quickly as possible by inserting oxidized regenerated cellulose. In one case of a recurrence of an advanced temporal PGL restaged as C3, we used a combination infratemporal and juxtacondylar approach (patient 6, Table 1). The advantage of this combined approach was that in this patient the corridor to the juxtacondylar approach had not been used before. In this case, part of the lower cranial nerves (VII, IX, XI, XII) had already been sacrificed or damaged by previous surgery. In all other cases, the lower cranial nerve functions and the facial nerves functions were completely preserved (Table 1).
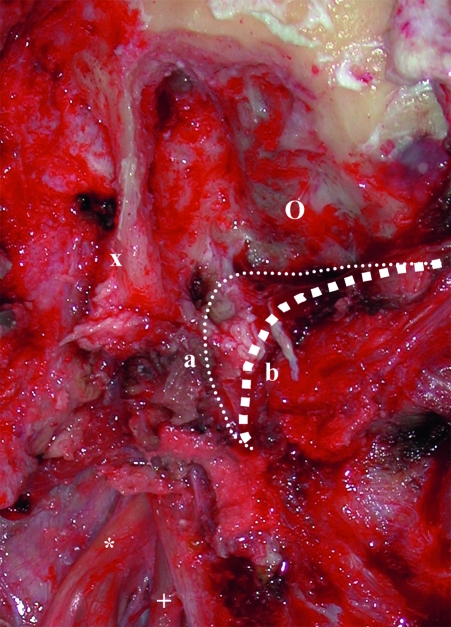
Figure 1.
Intrasurgical view of right-sided juxtacondylar approach with patient in sitting position (patient No. 2 in Table 1). x, bony covered course of the facial nerve; o, course of the sigmoid sinus; *, lower cranial nerves; + , internal carotid artery; small dotted line, former course of the vertebral artery; large dotted line, current course of the vertebral artery following its transposition.
DISCUSSION
The juxtacondylar approach was first described in 1976 by Friedrich and Seeger12 as the “transcondylar approach” and was advocated for the surgical removal of tumors in the foramen magnum and posterior fossa. Several modifications of the juxtacondylar approach have been suggested, such as the supracondylar approach, extreme far lateral transcondylar approach, variations of the extreme lateral craniocervical approach, and others.19,20,21 In 1993, Fukushima,22 and later in 1995, George et al,17,18 described a surgical technique using the juxtacondylar corridor for the resection of temporal PGLs. From the neurosurgical perspective, George and colleagues favored the juxtacondylar approach as an alternative for patients with temporal PGLs18 because it was possible to combine intra- and/or extradural approaches without skeletonizing or transposing the facial nerve. Furthermore, the posterior lateral view to the jugular foramen afforded a good view and allowed differentiation between the pars vascularis and the pars nervosa. We feel that this facilitates removal of the intravascular part of a temporal PGL and aids preservation of lower cranial nerve function. In contrast, when using the infratemporal approach, the surgeon only sees the pars nervosa of the jugular foramen after the tumor has been removed.
Preservation of vaga function has always been important but has been brought into sharp focus with the recognition of hereditary mutations in the SDH gene.1,2,3 Patients with a PGL syndrome have a higher incidence of simultaneous or consecutive ipsi- or contralateral craniocervical PGLs. These patients also have a high risk of acquired bilateral vagal paralysis with its implications—a permanent tracheostomy and a percutaneous endoscopic gastrostomy (PEG). For these patients, alternative solutions must be sought, and consideration of the juxtacondylar approach may help preserve the lower cranial nerves and facial nerve functions. But it has its limitations, which are imposed by preservation of the fallopian canal. Tumors with significant extension anteriorly around the internal carotid artery or those with an anteriorly enlarged jugular bulb are not suitable for this approach.
Another problem is that closure of the sigmoid sinus with oxidized regenerated cellulose is definitely inferior to that obtained by double ligation as described in the infratemporal approach.23 It should be noted that the infratemporal approach can also be modified, and in this respect an inferior mastoidectomy-hypotympanic approach without skeletonizing or transposing the facial nerve can be useful.24 Such an approach is recommended in cases of type B and some particular cases of type C tumors. In our study, we used the juxtacondylar approach in one patient with a type B temporal PGL (patient 3, Table 1) because the tumor was small, was closely applied to the jugular bulb, and had good access through the mastoid. This approach allowed a good overview to the lateral part of the jugular foramen and the jugular bulb without sacrifice of the middle ear or the need to uncover the facial or lower cranial nerves. Patient 2 (Table 1) demonstrated how one could use the juxtacondylar approach alone for the resection of an extra- and intradural tumor, or in combination with an infratemporal approach to enlarge the surgeon's view and operate through virgin territory, thus avoiding scar tissue.
The use of the juxtacondylar approach requires a degree of experience when preparing the vertebral artery, and this should include management of complications such as damage to the vessel. Our preparation by cadaver dissection, together with the assistance of an experienced neurosurgeon, helped us to become more and more comfortable with the preparation of the vertebral artery and the first and second cervical nerve. The sitting position of the patient for the juxtacondylar approach is not obligatory. The sitting position creates a higher risk of air embolism than a laying position when the surgeon opens the jugular bulb. The anesthetist must be aware of this and prepare accordingly.25 Our surgical outcomes bear testimony to the facility of this approach; consequently, we recommend it to the majority of head and neck surgeons.
REFERENCES
- Neumann H P, Bausch B, McWhinney S R, et al. Freiburg-Warsaw-Columbus Pheochromocytoma Study Group Germ-line mutations in nonsyndromic pheochromocytoma. N Engl J Med. 2002;346:1459–1466. doi: 10.1056/NEJMoa020152. [DOI] [PubMed] [Google Scholar]
- Neumann H P, Pawlu C, Peçzkowska M, et al. European-American Paraganglioma Study Group Distinct clinical features of paraganglioma syndromes associated with SDHB and SDHD gene mutations. JAMA. 2004;292:943–951. doi: 10.1001/jama.292.8.943. [DOI] [PubMed] [Google Scholar]
- Schiavi F, Boedeker C C, Bausch B, et al. European-American Paraganglioma Study Group Predictors and prevalence of paraganglioma syndrome associated with mutations of the SDHC gene. JAMA. 2005;294:2057–2063. doi: 10.1001/jama.294.16.2057. [DOI] [PubMed] [Google Scholar]
- Schipper J, Boedeker C C, Maier W, Neumann H P. Paragangliomas in the head/neck region. Part I: Classification and diagnosis. HNO. 2004;52:569–574. doi: 10.1007/s00106-003-1007-7. [DOI] [PubMed] [Google Scholar]
- Fisch U. Infratemporal fossa approach for glomus tumors of the temporal bone. Ann Otol Rhinol Laryngol. 1982;91:474–479. doi: 10.1177/000348948209100502. [DOI] [PubMed] [Google Scholar]
- Fisch U, Mattox D. Microsurgery of the Skull Base. Stuttgart: Thieme; 1988. pp. 149–153.
- Schipper J, Boedeker C C, Maier W, Neumann H P. Paragangliomas of the head and neck. Part 2: Therapy and follow-up. HNO. 2004;52:651–660. doi: 10.1007/s00106-003-1006-8. [DOI] [PubMed] [Google Scholar]
- Schipper J, Arapakis I, Ridder G J, Maier W, Spetzger U. Microsurgical resection of jugular foramen tumors with hearing preservation and without facial nerve palsy. HNO. 2003;51:721–727. doi: 10.1007/s00106-003-0805-2. [DOI] [PubMed] [Google Scholar]
- Leonetti J P, Brackmann D E, Prass R L. Improved preservation of facial nerve function in the infratemporal approach to the skull base. Otolaryngol Head Neck Surg. 1989;101:74–78. doi: 10.1177/019459988910100112. [DOI] [PubMed] [Google Scholar]
- Jackson C G, Harris P F, Glasscock M E, III, et al. Diagnosis and management of paragangliomas of the skull base. Am J Surg. 1990;159:389–393. doi: 10.1016/s0002-9610(05)81279-6. [DOI] [PubMed] [Google Scholar]
- Bertalanffy H, Seeger W. The dorsolateral, suboccipital, transcondylar approach to the lower clivus and anterior portion of the craniocervical junction. Neurosurgery. 1991;29:815–821. doi: 10.1097/00006123-199112000-00002. [DOI] [PubMed] [Google Scholar]
- Friedrich H, Seeger W. Microsurgery in pre-pontine tumours. Neurochirurgia (Stuttg) 1976;19:246–259. doi: 10.1055/s-0028-1090419. [DOI] [PubMed] [Google Scholar]
- Goel A, Desai K, Muzumdar D. Surgery on anterior foramen magnum meningiomas using a conventional posterior suboccipital approach: a report on an experience with 17 cases. Neurosurgery. 2001;49:102–106. doi: 10.1097/00006123-200107000-00016. [DOI] [PubMed] [Google Scholar]
- Heros R C. Lateral suboccipital approach for vertebral and vertebrobasilar artery lesions. J Neurosurg. 1986;64:559–562. doi: 10.3171/jns.1986.64.4.0559. [DOI] [PubMed] [Google Scholar]
- Kaye A H, Hahn J F, Kinney S E, Hardy R W, Jr, Bay J W. Jugular foramen schwannomas. J Neurosurg. 1984;60:1045–1053. doi: 10.3171/jns.1984.60.5.1045. [DOI] [PubMed] [Google Scholar]
- Day J D, Kellogg J X, Tschabitscher M, Fukushima T. Surface and superficial surgical anatomy of the posterolateral cranial base: significance for surgical planning and approach. Neurosurgery. 1996;38:1079–1084. [PubMed] [Google Scholar]
- George B, Lot G, Tran Ba Huy P. The juxtacondylar approach to the jugular foramen (without petrous bone drilling) Surg Neurol. 1995;44:279–284. doi: 10.1016/0090-3019(95)00174-3. [DOI] [PubMed] [Google Scholar]
- George B, Tran P B. Surgical resection of jugulare foramen tumors by juxtacondylar approach without facial nerve transposition. Acta Neurochir (Wien) 2000;142:613–620. doi: 10.1007/s007010070103. [DOI] [PubMed] [Google Scholar]
- Gilsbach J M, Sure U, Mann W. The supracondylar approach to the jugular tubercle and hypoglossal canal. Surg Neurol. 1998;50:563–570. doi: 10.1016/s0090-3019(97)00378-9. [DOI] [PubMed] [Google Scholar]
- Babu R P, Sekhar L N, Wright D C. Extreme lateral transcondylar approach: technical improvements and lessons learned. J Neurosurg. 1994;81:49–59. doi: 10.3171/jns.1994.81.1.0049. [DOI] [PubMed] [Google Scholar]
- Salas E, Sekhar L N, Ziyal I M, Caputy A J, Wright D C. Variations of the extreme-lateral craniocervical approach: anatomical study and clinical analysis of 69 patients. J Neurosurg. 1999;90(suppl):206–219. doi: 10.3171/spi.1999.90.2.0206. [DOI] [PubMed] [Google Scholar]
- Fukushima T. In: Sekhar LN, Janecka IP, editor. Surgery of Cranial Base Tumors. New York: Raven Press; 1993. Combined supra- and infra-parapetrosal approach for petroclival lesions. pp. 661–669.
- Sasaki T. Surgical approaches to the tumors in and around the jugulare foramen. No Shinkei Geka. 1994;22:1111–1118. [PubMed] [Google Scholar]
- Maniglia A J, Sprecher R C, Megerian C A, Lanzieri C. Inferior mastoidectomy-hypotympanic approach for surgical removal of glomus jugulare tumors: an anatomical and radiologic study emphasizing distances between critical structures. Laryngoscope. 1992;102:407–414. doi: 10.1288/00005537-199204000-00007. [DOI] [PubMed] [Google Scholar]
- Zentner J, Albrecht T, Hassler W. Prevention of an air embolism by moderate hypoventilation during surgery in the sitting position. Neurosurgery. 1991;28:705–708. doi: 10.1097/00006123-199105000-00011. [DOI] [PubMed] [Google Scholar]