Stapled hemorrhoidopexy (SH) is an accepted procedure for third-degree hemorrhoids; however, recent data show that the complication rate and need for additional hemorrhoid treatment are higher for SH than for conventional hemorrhoidectomy. One of the most serious complications of SH is rectal bleeding, which occurs in 4.2%–7.5% of patients.1 Only a few cases of intra-abdominal or retroperitoneal hemorrhage have been reported. We report the second case of intra-abdominal hemorrhage without rectal bleeding after SH, which was performed without intraoperative complications or technical difficulties.
CASE REPORT
A 52-year-old man with a normal coagulation profile and who did not use anticoagulants or platelet-inhibiting medications underwent elective SH for third-degree hemorrhoids. We used a 33-mm Proximate (PPH-03) hemorrhoidal circular stapler (ETHICON ENDO-SURGERY Inc.). The staple line was intact with no evidence of anastomotic leakage, 3 cm above the dentate line. There was minimal hemorrhage from the rectum, and 2 additional stitches at 12 o'clock were inserted near the anastomotic line.
A few hours later, the patient complained of pelvic fullness and progressive abdominal pain. Physical examination revealed diffuse abdominal tenderness with rebound pain and diminished bowel sounds. Emergency rectoscopy showed a normal anal canal with stapled mucosa and no evidence of active bleeding. Abdominal ultrasonography revealed free intraperitoneal fluid, and computed tomography of the abdomen revealed an area of dense fluid measuring 12 cm in dimension in front of the urinary bladder, then below the spleen and in the left paracolic gutter, with distended rectum measuring 8.5 × 5 cm in diameter (anteroposterior × laterolateral diameter) (Fig. 1).
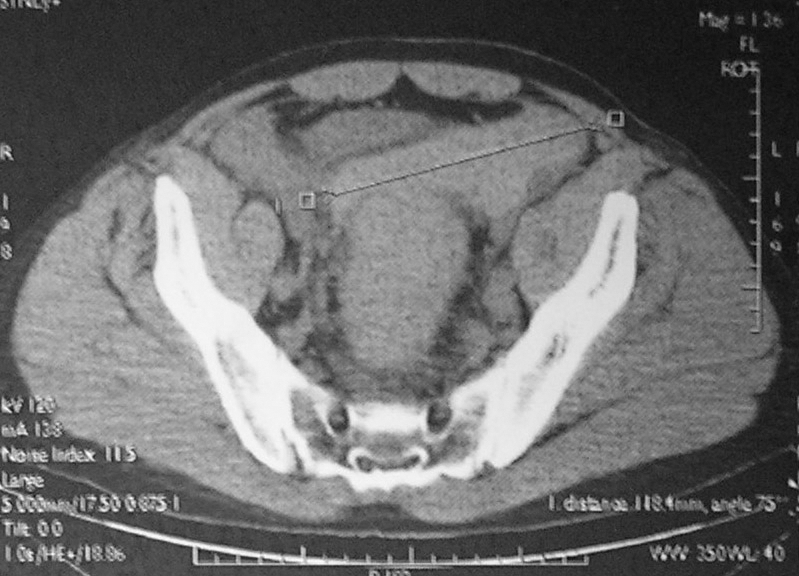
Fig. 1. Postoperative computed tomography scan of the abdomen showing extensive hemoperitoneum below the spleen, in the left paracolic gutter, in front of urinary bladder, measuring 12 cm in dimension, and a distended rectum, measuring 8.5 × 5 cm.
Urgent laparotomy revealed an extensive hemoperitoneum. The rectum was edematous with hemorrhagic infiltration. It contained a huge, tense hematoma, extending 5–7 cm proximal to the peritoneal reflection, with a 4-cm seromuscular tear (SMT) in the anterior tenia of the sigmoid colon, beginning 5 cm above the peritoneal reflection (Fig. 2). Active bleeding was present through the SMT. The point of bleeding was about 1 cm above the staple line, but the exact source could not be identified; hemostasis was not feasible. The patient required a Hartmann's operation owing to edematous and infiltrated colonic wall of questionable viability. The patient's postoperative course was uncomplicated, and he left hospital on postoperative day 12.
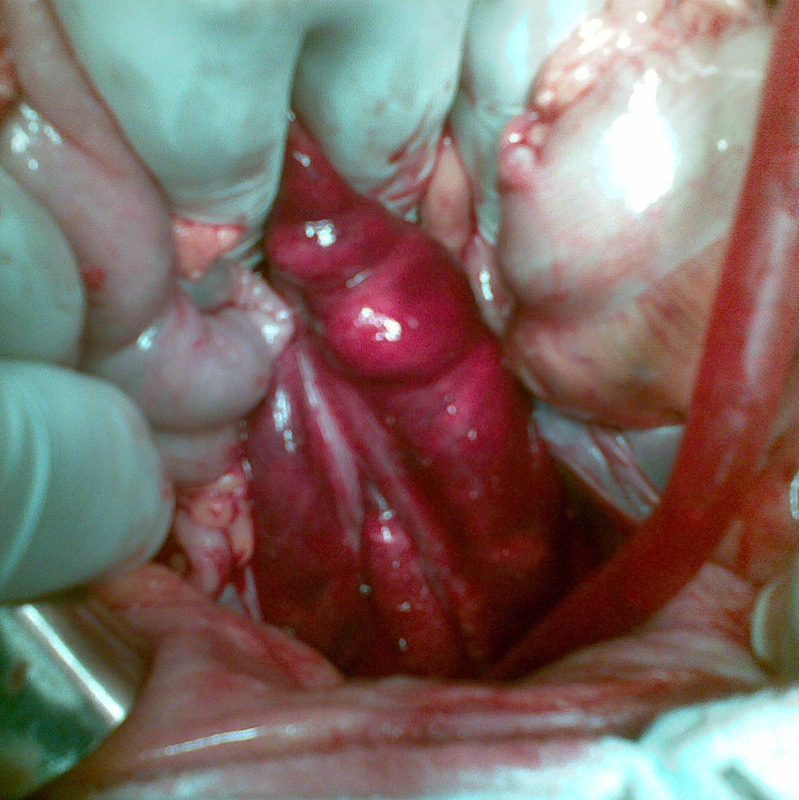
Fig. 2. Surgical view shows an edematous rectal wall with hemorrhagic infiltration of the rectosigmoid. There is a seromuscular tear in the anterior tenia of the sigmoid colon and an intact, bulging mucosa.
DISCUSSION
Stapled hemorrhoidopexy is a standard surgical technique for third-degree hemorrhoids. The most common early complication is rectal bleeding. The cause of minor rectal bleeding is usually hemorrhage from the stapled ring, and requires early reintervention in up to 5% of patients. Major complications, although unusual, are potentially life-threatening. Aumann and colleagues2 reported a case of severe intra-abdominal bleeding after SH, initiated by the intra-abdominal positioning of a stapler caused by an enterocele. A review of the medical literature reveals only 1 report similar to ours, the only difference being the type of the procedure used. Blouhos and colleagues3 peformed a low anterior resection, whereas we used a Hartmann procedure because of the questionable viability of the edematous rectum with hemorrhagic infiltration. Thus, we avoided the risk of anastomotic breakdown in a patient with hemorrhagic shock.
It is important that the coagulation profile be evaluated for every patient. Those with intramural hematoma on anticoagulant therapy should receive 2–4 units of fresh frozen plasma and vitamin K, which corrects coagulation parameters within 72 hours. The addition of red blood cell concentrates and intravenous antibiotics usually leads to improvement within 4–6 days and to resolution of the hematoma. Progression of an intramural hematoma eventually leads to intestinal obstruction, perforation or an SMT, with intra-abdominal bleeding.
Certain morphologic features common to the intestines determine the morphologic characteristics of the SMT. First is the redundancy of the mucosa and submucosa, which is created by the circular plicae in the small bowel; the semilunar folds in the colon allow the inner bowel wall to unfold, stretch and span the muscular gap created by the tear. Second is the high tensile strength of the submucosa that protects the soft mucosa from shearing and stretching forces. Third is the loose attachment of the muscularis to the submucosa that permits formation of a cleavage plane at this junction when subjected to traumatic forces.4 The hematoma forms within the muscular layers and expands until its growth is limited by adjacent structures. The final morphologic feature is that intramural hematomas expand, causing dissection of the anterior teniae coli with subsequent rupture into the peritoneal cavity.5 Our case confirms this pathophysiologic process (Fig. 2).
In conclusion, a diagnosis of intramural hematoma requires acute clinical awareness. Both ultrasonography and abdominal CT improve diagnostic accuracy in such cases. Conservative treatment should be offered first, but surgery is indicated if progressive enlargement of the intramural hematoma, substantial intra-abdominal hemorrhage, generalized peritonitis or intestinal obstruction develop.
Competing interests: None declared.
Correspondence to: Dr. G. Augustin Department of Surgery, Division of Abdominal Surgery University Hospital Center Zagreb 10 000 Zagreb Republic of Croatia augustin.goran@gmail.com
References
- 1.Pavlidis T, Papaziogas B, Souparis A, et al. Modern stapled Longo procedure vs. conventional Milligan–Morgan hemorrhoidectomy: a randomized controlled trial. Int J Colorectal Dis 2002;17:50-3. [DOI] [PubMed]
- 2.Aumann G, Petersen S, Pollack T, et al. Severe intra-abdominal bleeding following stapled mucosectomy due to enterocele: report of a case. Tech Coloproctol 2004;8:41-3. [DOI] [PubMed]
- 3.Blouhos K, Vasiliadis K, Tsalis K, et al. Uncontrollable intraabdominal bleeding necessitating low anterior resection of the rectum after stapled hemorrhoidopexy: report of a case. Surg Today 2007;37: 254-7. [DOI] [PubMed]
- 4.Slavin RE, Borzotta AP. The seromuscular tear and other intestinal lesions in the seatbelt syndrome: a clinical and pathologic study of 29 cases. Am J Forensic Med Pathol 2002;23:214-22. [DOI] [PubMed]
- 5.Calabuig R, Ortiz C, Sueiras A, et al. Intramural hematoma of the cecum: report of two cases. Dis Colon Rectum 2002;45:564-6. [DOI] [PubMed]


