Abstract
Ligation of the transmembrane protein Tim-1 can co-stimulate T cell activation. Agonistic antibodies to Tim-1 are also capable of inducing T cell activation without additional stimuli. However, little is known about the biochemical mechanisms underlying T cell stimulation or co-stimulation through Tim-1. We show that a tyrosine in Tim-1 becomes phosphorylated in an lck-dependent manner, whereupon it can directly recruit p85 adaptor subunits of PI 3-kinase. This results in PI3K activation, which is required for Tim-1 function. We also provide genetic evidence that p85 expression is required for optimal Tim-1 function. Thus, we describe a pathway from Tim-1 tyrosine phosphorylation to the PI3K signaling pathway, which appears to be a major effector of Tim-1-mediated T cell activation.
Proteins of the T cell immunoglobulin and mucin domain (TIM) family function to modulate T cell activation and effector function. This family consists of four Tim proteins in the mouse and three TIM proteins in human (1-3). The TIM proteins are cell surface, immunoglobulin (Ig) superfamily, receptors that may also be secreted and which share the following domain structure: an extracellular Ig-like domain, followed by a polymorphic mucin-like domain, a transmembrane domain and a cytoplasmic tail of variable length (1-3).
Of these family members TIM-1 has been implicated in the immune regulation of asthma and atopic diseases (3, 4). More recent studies have shown that ligation of TIM-1 with an agonistic antibody or with a ligand (TIM-4) can co-stimulate proliferation of T cells as well as cytokine production, both in vivo and in vitro, and abrogate tolerance in a Th2 model of respiratory tolerance, collectively suggesting that it usually functions as a positive immune regulator (5, 6). Our own prior work also showed that murine Tim-1 can transmit a co-stimulatory signal for activation and cytokine production of T cells (7). Finally, a recent report demonstrated that human TIM-1 can physically associate with the TCR-CD3 complex to upregulate T cell activation signals (8). Nevertheless, depending on the affinity and targeted epitope of the cross-linking antibody, and also possibly the timing of its application, opposing conclusions have been reached regarding whether TIM-1 positively or negatively regulates T cell activation and disease outcomes (9-12). Thus, a greater understanding of the biochemical signals mediated by TIM-1 is required to mechanistically explain its role in immune activation.
The TCR/CD3 complex and co-stimulatory molecules interact with key intracellular signaling proteins that determine which downstream effector pathways are triggered. Of these, the phosphoinositide 3-kinases (PI3K) have been frequently implicated in co-stimulatory signaling (13). These enzymes regulate diverse biological processes, including cell growth, proliferation, cytoskeletal organization, apoptosis and vesicular trafficking (14). Among the various classes of PI3K, Class IA proteins are linked to tyrosine kinase dependent signaling downstream of lymphocyte antigen receptors, co-stimulatory receptors and cytokine receptors. These proteins generally exist as heterodimers of a regulatory subunit (p85) and a catalytic subunit (p110). Class I phosphoinositide 3-kinases function to phosphorylate inositol rings at the 3' position to generate phosphatidylinositol-3,4-bisphosphate, and phosphatidylinositol 3,4,5 trisphosphate (14). These lipids are stationed at the inner leaflet of the plasma membrane, where their major function appears to be to recruit signaling molecules with pleckstrin homology domains. Additionally, the p85 adaptor subunit contains several other interesting domains, including SH2, SH3 and proline rich domains, and a region with homology to Rho family GTPase-activating proteins. These domains facilitate protein-protein interactions that may be able to mediate signal transduction events independently of p110 (15).
To date, there is little known about the molecular basis for signal transduction downstream of TIM-1. We previously showed that the cytoplasmic tail of Tim-1 could be inducibly tyrosine phosphorylated, and that Tim-1 function in human and murine T cell lines requires a conserved tyrosine in the cytoplasmic tail (7). In this present study, we show that Tim-1 tyrosine phosphorylation and activation of downstream transcription factors require the src family kinase Lck, which is also critical for TCR-mediated signal transduction. Following phosphorylation, Tim-1 recruits the PI3K adaptors p85α and p85β. Finally, we show that Tim-1 can enhance activation of primary murine T cells in a manner that requires p85 expression and PI3K activity.
Materials and Methods
DNA Constructs
Murine Tim-1 (from strain C57BL/6), tagged with an extracellular Flag tag, was described previously (7). Similarly, Flag-Tim-1 lacking the cytoplasmic tail (Tim-1 Δ cyto), and Flag-Tim in which tyrosine 276 was mutated to phenylalanine have also been described elsewhere (7).
Cell Lines and Mice
In addition to parental Jurkat T cells, the lck-deficient variant JCaM.1 and reconstituted JCaM1/Lck were also employed (16, 17). A fast-growing variant of the D10 T cell clone was obtained from M. Krummel and was described previously (7, 18). p85β knockout and p85α/β double knockout mice have been described (19). C57BL/6 mice were purchased from Jackson Laboratories. Jurkat, D10 and primary T cells were cultured as previously described (7).
Antibodies and reagents
Clonotypic antibody to the Jurkat TCR (C305) was from A. Weiss (University of California, San Francisco). Anti-hCD28, anti-mCD3, anti-mCD28 and PE anti-mCD25 were from Caltag (Burlingame, CA). Anti-PI3 kinase p85 (Rabbit anti-serum) and anti-phospho-tyrosine (4G10) were from Upstate/Chemicon (Temecula, CA). Biotin-anti-mCD28 (37.51), biotin-anti-mCD3ε (145 -2C11) and FITC-conjugated anti-CD69 were from BD Biosciences (San Jose, CA). Biotin-anti-mCD4 (L3T4) was from eBioSciences (San Diego). Streptavidin was from Zymed (San Francisco, CA). Rabbit anti- hamster IgG and APC-conjugated anti-rat IgG were from Jackson Immunoresearch (West Grove, PA). Akti 1/2, phorbol myristate acetate (PMA), PP2 and LY294002 were from EMD Biosciences (La Jolla, CA). Anti-flag (M2) and β-actin mAb's and ionomycin were from Sigma (St. Louis, MO). Rat anti-mouse Tim-1 (3B3) was described previously (5). Anti-phospho Akt (S473) rabbit mAb was from Biosource/Invitrogen (Carlsbad, CA).
Transient Transfections and Luciferase Assay
T cell lines were transfected by electroporation using a gene pulser (Bio-Rad Laboratories, Hercules, CA), at a setting of 250-260V and 960μF, in cuvettes containing 1-2 × 107 cells with 0.4 ml antibiotic-free media. The amount and type of DNA plasmids transfected for an experiment are as described in the respective figure legends. Following transfection, cells were cultured in 10 ml complete medium for 16-20 hours, and then stimulated for six hours in 96 U-bottom well plates. Reporter assays were performed as described previously (20). Luciferase activity was determined with an Orion luminometer (Zylux, Oak Ridge, TN).
SH2 domain arrays
A thirteen amino-acid peptide based on the Tim-1 cytoplasmic tail was synthesized, including Y276 and six amino acids on either side (Peptide Synthesis facility, Biotechnology Center, Molecular Medicine Institute, University of Pittsburgh). The peptide was biotinylated on the N-terminus and the tyrosine was phosphorylated. This was then subjected to HPLC; the end product obtained was greater than 90% pure, as determined by mass spectrometry. The purified peptide was incubated with the SH2 domain array, which was processed as per the manufacturer's instructions (Panomics). Processed arrays were imaged on a Kodak Image Station 2000R, with accumulation to 2,000 gray levels. When employed as a competitive inhibitor, phenylphosphate was added both after blocking and during peptide incubation, at 100 mM. Quantitation was performed by averaging the intensity values for the duplicate p85α and p85β spots and dividing by the average of all positive control spots. These values were then compared for experiments performed with or without phenylphosphate to derive a percent inhibition.
TIM-1 tyrosine phosphorylation and endogenous p85 association
Jurkat, or Lck mutants JCaM1.6 or JCam1-Lck cells (2 × 107) were transfected with flag-tagged Tim-1 or flag tagged mutant Tim-1 constructs, stimulated with pervanadate (1:100) (21), and/or coupled with PP2 (10μM). NP-40 lysates were immunoprecipitated with M2-conjugated agarose beads (Sigma), and separated by SDS-PAGE followed by Western blotting onto a PVDF membrane (20). Blots were probed with M2 and HRP-conjugated anti-mouse IgG (Pierce) or with anti-p85 pan antibody and HRP-conjugated Protein A (Pierce). They were developed with Super Signal Pico ECL Substrate (Pierce) and digitally imaged on a Kodak Image Station 2000R, with accumulation set to stop at 2,000 gray levels. For detection of tyrosine phosphorylation, blots were then stripped and re-probed with 4G10.
Analysis of T cell activation markers
CD4+ T cells were purified from spleens of C57BL/6 mice or from p85 beta k.o. or p85 α/β double k.o. mice by negative selection (Miltenyi; Auburn, CA). T cells were stimulated in 24 well plates coated with rabbit anti-hamster secondary antibody (10μg/ml overnight at 4°C) followed by primary antibodies (2-3 hours at 37°C) of hamster anti-mouse CD3 (0.02-1.0 μg/ml) and anti-mouse CD28 (0.5 μg/ml). T cells were harvested at days one and three post-stimulation and examined for CD69 and CD25 surface expression, respectively, by flow cytometry on a BD LSR II. Tim-1 expression was determined with 3B3 mAb, followed by anti-rat IgG antibody.
IL-2 ELISA
Purified splenic CD4+ T cells from p85β or p85α/β knockout mice were stimulated as indicated at one million per well in a 24 well plate. Supernatants were assayed for murine IL-2 using an OptEIA kit from B-D Biosciences, according to the manufacturer's instructions.
Results
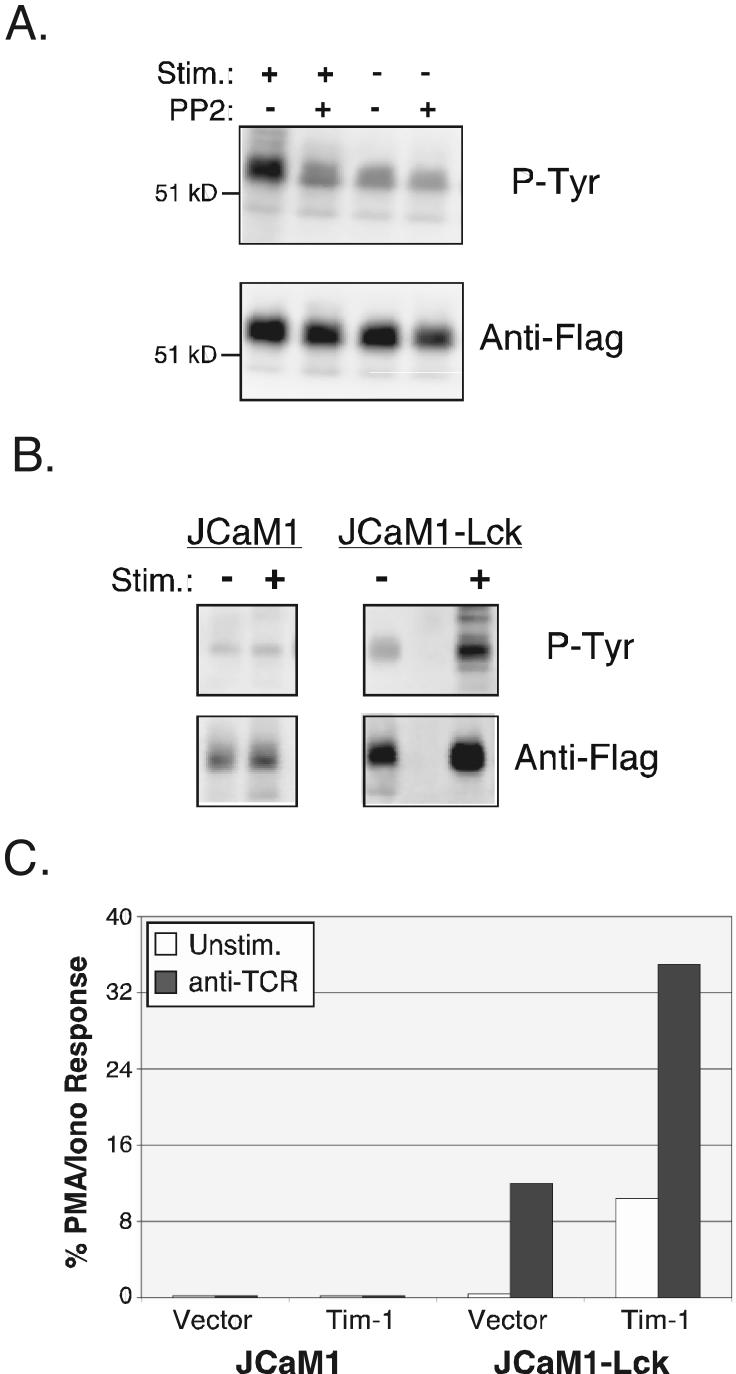
Regulation of Tim-1 tyrosine phosphorylation
We showed previously that Tim-1 can be inducibly phosphorylated on tyrosine and that tyrosine 276 in the cytoplasmic tail is required for Tim-1 mediated co-stimulation of NFAT/AP-1-dependent transcription in T cells (7). This tyrosine is conserved in context between different species (1) and is contained in a motif favorable for recognition by src-family tyrosine kinases, as indicated by the charged residues glutamic acid and aspartic acid upstream (22). In order to ascertain whether src kinases are indeed required for Tim-1 phosphorylation, we examined tyrosine phosphorylation in the presence of PP2, a potent inhibitor of src kinases (23). Jurkat cells were transfected with epitope-tagged Tim-1, and stimulated with pervanadate, in the presence or absence of PP2, followed by immunoprecipitation (IP) of Tim-1 and anti-phosphotyrosine western blotting. As shown in Figure 1A, tyrosine phosphorylation of Tim-1 was induced by treatment with pervanadate. Inclusion of PP2, along with stimulation by pervanadate, led to a significant decrease in the phosphorylation intensity, which was similar to basal levels. This indicates a requirement of src kinases for Tim-1 tyrosine phosphorylation, even under conditions where potent tyrosine kinase activation is induced, i.e. by pervanadate. Since Lck is a prominent src family tyrosine kinase essential for TCR-mediated T cell activation, we used an Lck-deficient mutant variant of Jurkat cells, JCaM1 (17), to probe the role of Lck in Tim-1 phosphorylation and function. The ability of Tim-1 to become tyrosine phosphorylated in JCaM1 cells was severely compromised (Fig. 1B), even after treatment with the potent stimulus pervanadate. In contrast, JCaM1 cells that have been stably reconstituted with Lck (JCaM1-Lck) showed a recovery of inducible Tim-1 phosphorylation (Fig. 1B) similar to what was observed in wild-type cells (Fig. 1A). In order to establish the functional relevance of lck-dependent Tim-1 tyrosine phosphorylation, we examined Tim-1 mediated NFAT/AP-1 activation in JCaM1 cells. Consistent with our previously published data with parental Jurkats (7), Tim-1 expression in Lck-reconstituted JCaM1 cells resulted in enhanced transcription of an NFAT/AP-1 luciferase reporter (Fig. 1C), both basally as well as in conjunction with stimulation through the TCR. In contrast, Lck-deficient JCaM1 cells displayed little if any reporter activity either with or without stimulation, despite the fact that Flag-Tim-1 expression was equivalent on both cell lines (data not shown). These data suggest that Tim-1 enhances T cell activation, at least in part, by coupling to phosphotyrosine-dependent signaling pathways.
Figure 1. Role of Lck in Tim-1 tyrosine phosphorylation and function.
(A) Jurkat T cells expressing Flag-Tim-1 were stimulated as indicated, with or without the Src kinase inhibitor PP2. Anti-Flag IP's were separated by SDS-PAGE and western blotted with anti-Flag (lower panel), then stripped and re-probed with anti-phosphotyrosine antibody 4G10 (P-Tyr - upper panel). (B) Lck-deficient JCaM1 or Lck-reconstituted JCaM1 cells expressing Flag-Tim-1 were stimulated and analyzed as in part A. (C) JCaM1 or JCaM1-Lck cells were transfected with an NFAT/AP-1 luciferase reporter and either empty vector or Flag-Tim-1. Cells were stimulated the next day and luciferase activity was determined. Each experiment is representative of two (A-B) or three (C) that were performed.
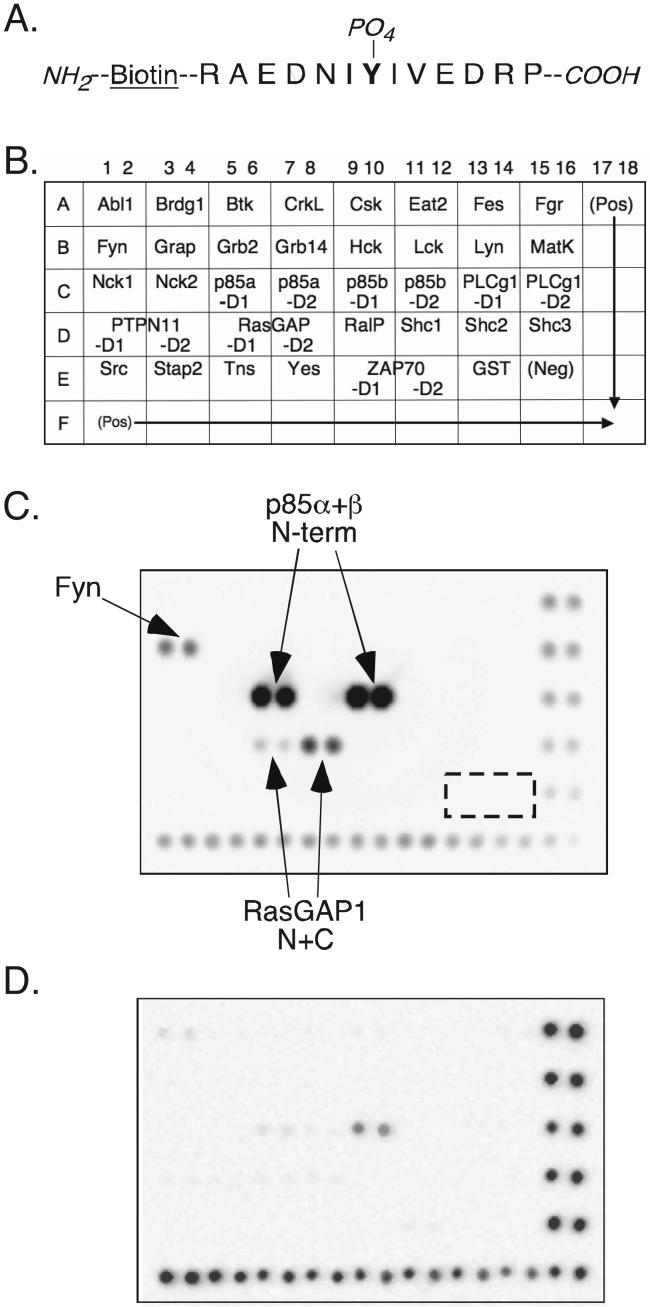
Interaction of Tim-1 with p85 subunits of PI3K
One mechanism by which phosphotyrosine-dependent signaling complexes are formed is through phosphotyrosine-SH2 domain interactions. In order to identify SH2 domain-containing signaling proteins that might specifically bind to phosphotyrosine 276 of the Tim-1 tail, a solid phase screen was performed. The TranSignal™ SH2 domain array from Panomics contains 38 SH2 domains of various signaling proteins, folded in their native conformation and immobilized in duplicate on a membrane. A thirteen amino-acid peptide was synthesized (Fig. 2A), which contained the tyrosine 276 of Tim-1 tail and six amino acids on either side. The peptide was tyrosine phosphorylated and biotinylated and incubated with the SH2 domain array membrane (for key see Fig. 2B). As shown in Figure 2C, two prominent sets of spots were obtained, which correspond to the N-terminal SH2 domain of p85 alpha and p85 beta. Other spots that were not consistent and of a much lower signal intensity corresponded to SH2 domains from RAS-GAP and the tyrosine kinase Fyn. We next performed the assay in the presence of a competitive inhibitor - phenylphosphate - to confirm that the binding observed was dependent on phosphotyrosine. As shown in Figure 2D, a much weaker signal was obtained when the SH2 array was incubated with phosphorylated Tim-1 peptide in the presence of phenylphosphate. By comparing the p85 signal with the positive control spots along the right and bottom edges, we determined that binding of the peptide to the p85α and p85β N-terminal SH2 domains was inhibited by 99% and 95%, respectively.
Figure 2. Specificity of SH2 domain binding to phosphorylated Y276 in the Tim-1 cytoplasmic tail.
(A) Sequence of the peptide, and modifications, used to determine the SH2 specificity of phopsho-Y276. (B) Layout of the SH2 domain array. SH2 domains are present as duplicate spots. For proteins with more than one SH2 domain, “D1” indicates the more N-terminal SH2. (C) Results of the SH2 domain array screen, using the peptide illustrated in part A. The dashed box indicates the location of negative control spots; the bottom and right edge contain positive control spots. These results are representative of those obtained in four separate experiments, using two different lots of membrane. (D) Competitive inhibition of Tim-1 peptide binding by the phosphotyrosine analogue phenylphosphate. The blot shown is representative of two experiments.
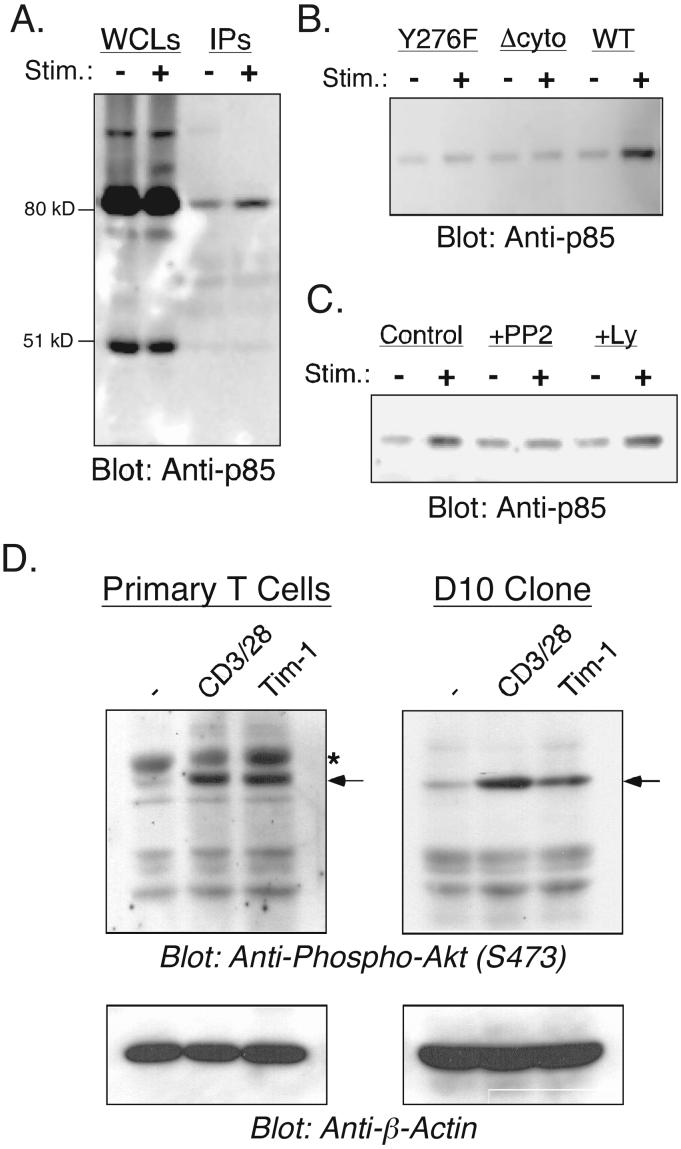
To validate the Tim-1-p85 association with full-length proteins, the interaction was also established in T cells by conventional IP. Flag-Tim-1 transfected Jurkat cells were stimulated with pervanadate, followed by anti-Flag IP and western blotting with a pan-p85 antibody. While there was a reproducibly strong interaction of Tim-1 with p85 under conditions of pervanadate stimulation, a weaker and less consistent association was also detected under resting conditions (Fig. 3A). Consistent with the functional importance of tyrosine 276 in the Tim-1 cytoplasmic tail (7), there was a loss of inducible p85 binding to mutant forms of Tim-1 either lacking the cytoplasmic tail or with Y276 mutated to phenylalanine (Fig. 3B). In agreement with data discussed above, this interaction was also significantly diminished in cells treated with PP2 (Fig. 3C). A major target for PI3K-derived lipids is the serine/threonine kinase Akt, activation of which is absolutely dependent upon PI3K. We therefore examined whether endogenous Tim-1 ligation results in activation of Akt, as assayed by its phosphorylation at serine 473. As shown in Figure 3D, we observed inducible Akt activation, in both primary T cell blasts and the Th2 T cell clone D10, after stimulation (of untransfected cells) with antibodies to CD3 and CD28 or Tim-1. Akt activation by either CD3/CD28 or Tim-1 was completely inhibited by pre-treatment with the PI3K inhibitor LY294002 (data not shown). These results demonstrate that Tim-1 can interact with p85 and activate PI3K signaling, when expressed in T cells, in a phosphotyrosine-dependent manner.
Figure 3. Recruitment and activation of PI3 kinase by Tim-1.
(A) Jurkat T cells expressing Flag-Tim-1 were stimulated as indicated, lysed and IP'd with anti-Flag. Whole cell lysates (WCLs) and IP's were separated by SDS-PAGE and western blotted for p85α/β. (B) Jurkat T cells expressing the indicated wild-type or mutant Flag-Tim-1 constructs were stimulated and analyzed for p85 binding as described for part A. (C) Jurkat T cells expressing wild-type Flag-Tim-1 were stimulated in the presence of 10 μM PP2 (Src kinase inhibitor) or 10 μM Ly294002 (PI3k inhibitor) then analyzed for p85 binding as above. (D) T cell blasts (left panels) or D10 Th2 T cells (right panels) were stimulated as indicated. Lysates were separated by SDS-PAGE and western blotted with a rabbit mAb to phospho-Akt (S473; upper panels). Blots were stripped and re-probed with a mouse mAb to β-actin (lower panels), to control for protein loading. The location of phospho-Akt is indicated by the arrows, while the star indicates a non-specific band that is only observed in primary T cells. Results in each part are representative of three experiments.
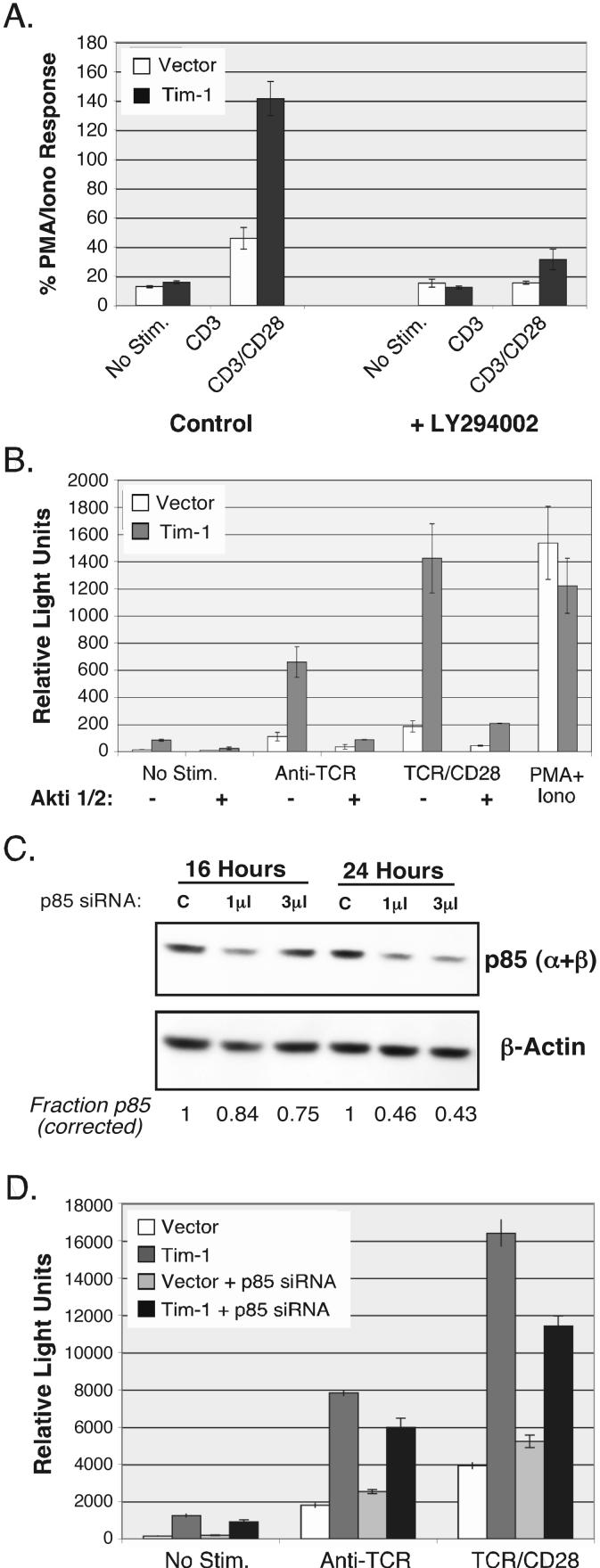
Role of p85 and PI3K in Tim-1 Function
p85 proteins function as regulatory subunits of class IA phosphoinositide 3-kinase (PI3K), and as such control localization and activation of the associated catalytic p110 proteins. In order to determine whether the catalytic property of PI3K is required for Tim-1 mediated co-stimulation of downstream NFAT/AP-1 dependent transcription, D10 cells (which possess a normally regulated PI3K pathway (18)) were co-transfected with an NFAT/AP-1 luciferase reporter, along with either empty vector or Tim-1. These cells were then treated with a range of stimuli, in the presence or absence of LY294002, an inhibitor of PI3K activity (24). As shown in Figure 4A, stimulation through CD3 and CD28 induced an enhanced activation of the reporter in Tim-1 transfected cells, compared with cells transfected with empty vector. However, in the presence of LY294002, the effect mediated by Tim-1 was markedly reduced. These data suggest that one mechanism by which Tim-1 co-stimulates T cell activation is through the catalytic function of PI3K. Therefore, we examined the role of a known downstream target of PI3K - the serine/threonine kinase Akt/PKB (25), which as shown above is activated by Tim-1. A similar reporter assay was performed as in Figure 4A, this time with the addition of the Akt inhibitor Akti 1/2 (26). As shown in Figure 4B, Tim-1-mediated activation of NFAT/AP-1 was effectively inhibited by Akti 1/2.
Figure 4. Role of the PI3K pathway in Tim-1 activation of NFAT/AP-1.
T cells were transfected with an NFAT/AP-1 luciferase reporter and the indicated constructs, then stimulated the next day, as indicated, followed by determination of luciferase activity. (A) Cells were stimulated in the presence or absence of the PI3K inhibitor LY294002. (B) Cells were stimulated in the presence or absence of the Akt inhibitor Akti 1/2 (20 μM). (C-D) T cells were transfected with an NFAT/AP-1 reporter, plus either empty vector or Flag-Tim1, and the indicated amounts of siRNA SmartPool oligos (Dharmacon) specific for p85α and p85β. Twenty-four hours after transfection, cells were stimulated for six hours, followed by determination of luciferase activity. Error bars indicate standard deviation for triplicate points in a single experiment. Results shown in each part are representative of three experiments.
We attempted to more definitively determine the role of p85 in Tim-1 function by siRNA-mediated knock-down of p85 in D10 T cells. We were able to achieve at best approximately 60% decrease of the protein (Fig. 4C), likely due in part to the necessity to eliminate expression of both p85α and p85β; this resulted in a partial inhibition of Tim-1 function, as determined with the NFAT/AP-1 reporter assay (Fig. 4D). Taken together, the data in Figure 4 indicate that Tim-1 exerts an effect on NFAT/AP-1 at least in part through the PI3k/Akt pathway.
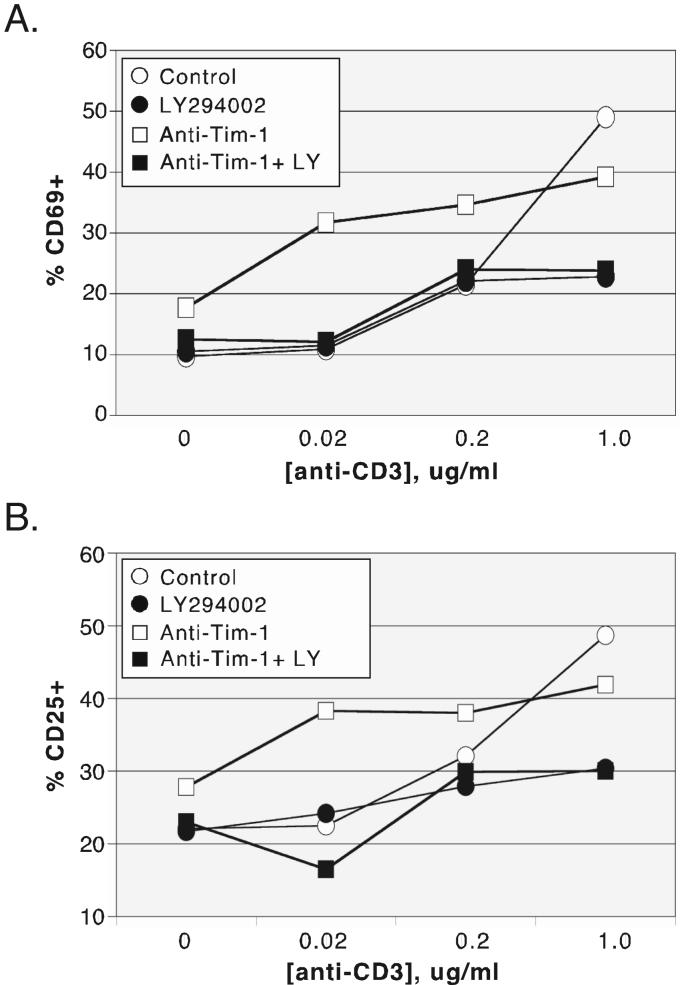
One of the earliest activation markers expressed by T cells is the cell surface glycoprotein CD69, which appears within several hours following TCR cross-linking and persists for approximately three days (27, 28). In order to assess the effect of Tim-1 on CD69 up-regulation, purified CD4+ T cells from C57BL/6 mice were activated with a range of concentrations of plate-bound anti-CD3, together with a fixed amount of anti-CD28, in the presence or absence of Tim-1 antibody. Ligation of Tim-1 substantially enhanced the upregulation of CD69 expression (Fig. 5A), with the greatest effect observed at lower concentrations of anti-CD3. An increase in CD69 expression was also observed on primary T cells treated with anti-Tim-1 alone. In light of data discussed above, we were interested in determining whether PI3K catalytic activity is required for Tim-1 mediated CD69 upregulation. As shown in Figure 5A, LY294002 significantly inhibited CD69 upregulation induced by Tim-1 ligation, either alone or in conjunction with anti-CD3/CD28.
Figure 5. PI3K activity is required for upregulation of early activation markers by endogenous Tim-1 on primary T cells.
Purified CD4+ T cells from C57 Bl/6 spleen and lymph node were stimulated for 24 hours with the indicated concentrations of anti-CD3 antibody (and a fixed concentration of anti-CD28 antibody - 0.5 μg/ml), with or without anti-Tim-1 antibody (6 μg/ml), in the presence or absence of PI3K inhibitor LY294002 (10 μM). Cells were stained with fluorescently labeled antibodies to CD69 (A) or CD25 (B) and analyzed by flow cytometry. Results in each panel are representative of three experiments that were performed.
Another inducible cell surface marker essential for T cell commitment to effector function is the high affinity IL-2 receptor alpha chain (CD25). To evaluate whether Tim-1 selectively enhanced expression of the early activation antigen CD69, or if this phenomenon was a more general consequence of its effects on T cell activation, we also examined CD25 up-regulation (Fig. 5B). As observed with CD69, Tim-1 cross-linking co-stimulated CD25 surface expression and this effect was more evident with lower concentrations of anti-CD3. Again, as with CD69, Tim-1 ligation alone led to some up-regulation of CD25 expression. Treatment with LY294002 significantly inhibited Tim-1-mediated CD25 upregulation, both by itself and in conjunction with CD3/CD28 signals. Thus, data presented in Figure 5 suggest that Tim-1 induces expression of the activation markers CD25 and CD69 in a PI3K-dependent manner.
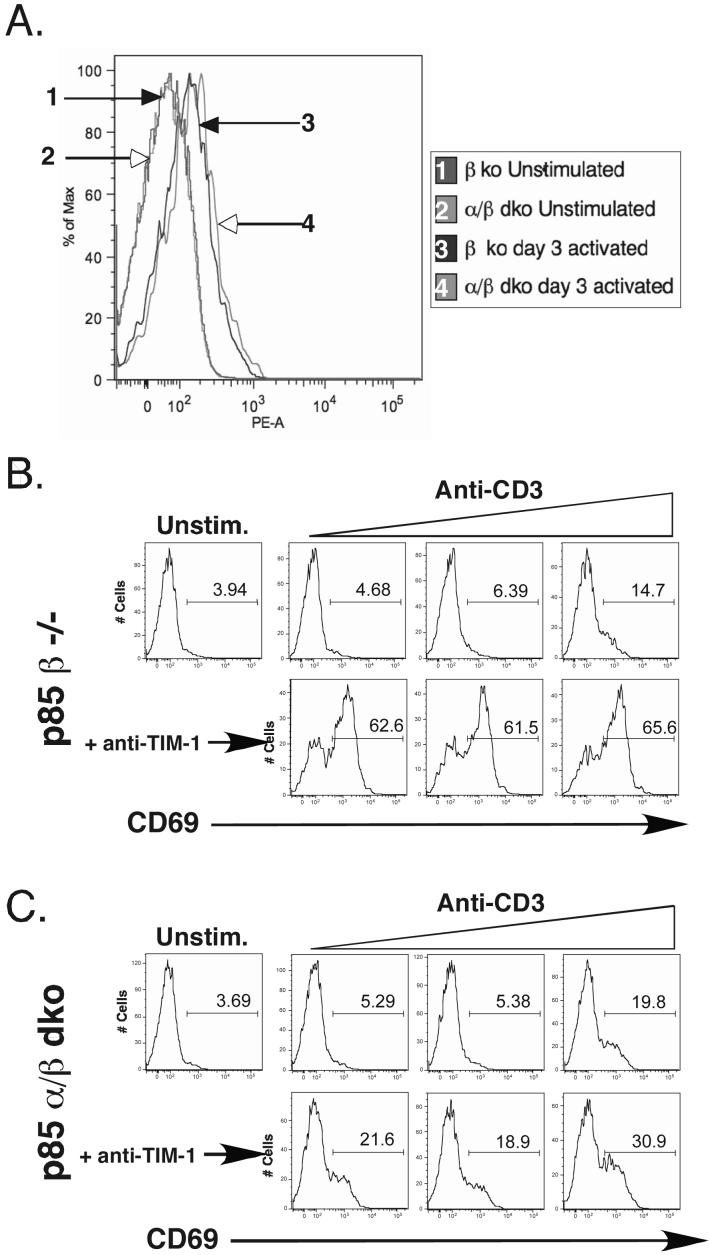
In order to determine more conclusively the relevance of the p85 interaction for endogenous Tim-1 function, a mouse model of p85 deficiency mice was employed (19). These mice were generated by crossing Pik3r1f mice, which have floxed alleles of Pik3r1 (encoding p85α, p50α and p55α), with Pik3r2n mice, which are deficient in the germ line for Pik3r2 (encoding p85β). The resulting mice were then bred to Lck-Cre transgenic mice, yielding mice with T cells specifically lacking expression of PI3K regulatory subunits from the double negative stage of thymocyte development forward. T cells from p85β null mice develop normally and possess no detectable defects in PI3K signaling or any compensatory changes in PI3K isoform expression, so these mice served as controls (19, 29). p85 double knockout mice also possess T cells with no gross developmental problems but have selective defects in TCR dependent signaling and cytokine production (19).
We first assessed expression of Tim-1 on T cells from p85-deficient mice. Importantly, expression of Tim-1 was not impaired on p85α/β knockout T cells, with expression in the resting (low levels) and activated (higher levels) state indistinguishable from p85β or wild-type mice (Fig. 6A). To confirm and extend the inhibitor studies performed with T cells from C57BL/6 mice, we examined co-stimulatory Tim-1 effects on surface expression of CD69 and CD25 in CD4+ T cells from these p85 mutant mice. Representative flow cytometry plots for results obtained with CD69 are shown in Figure 6, panels B-C. Thus, while stimulation with anti-CD3/CD28 alone was relatively unaffected by the complete lack of p85 in this experiment (compare part C with B), the ability of Tim-1 to co-stimulate CD69 upregulation was severely impaired.
Figure 6. p85 is required for Tim-1-mediated co-stimulation of CD69 expression.
(A) Expression of Tim-1 on resting or activated CD4+ T cells from spleens of p85β or p85α/β knockout mice. Splenocytes from p85β (B) or p85α/β (C) deficient mice were stimulated overnight with various concentrations anti-CD3 antibody (0.05, 0.2 and 1 μg/ml), along with a fixed concentration of anti-CD28 (1 μg/ml). Anti-Tim-1 antibody was also added to some cultures, at a concentration of 8 μg/ml. Cells were stained the next day for CD4 and CD69 and analyzed by flow cytometry. Results shown were gated on CD4+ cells.
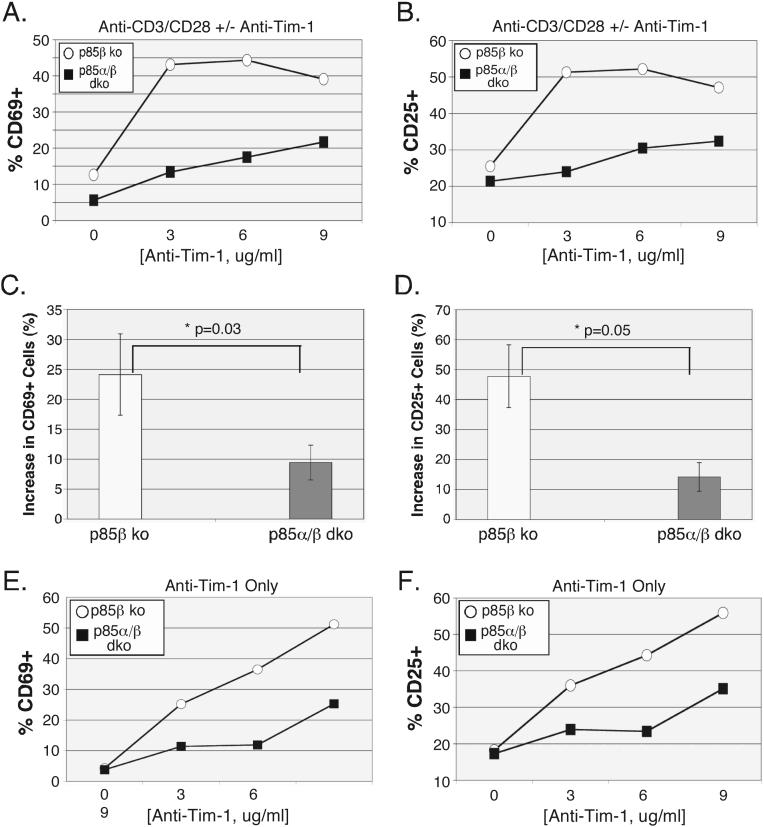
Because we an others have observed both stimulatory and co-stimulatory effects of Tim-1 ligation, we wanted to determine whether both or either of these activities would be affected by p85 deficiency. We therefore examined the effects of Tim-1 antibody 3B3 on upregulation of CD69 (Fig. 7 A,C and E) and CD25 (Fig. 7 B,D and F), either in the presence of CD3/CD28 engagement (Fig. 7 A-D) or without any additional stimuli (Fig. 7 E-F). As can clearly be seen from these data, the absence of p85 expression, in the p85α/β double knockout (dko) T cells, had a profound effect on the ability of Tim-1 to induce increases in CD69 and CD25, either by itself or in conjunction with CD3/CD28 signaling. Previous studies with p85-deficient mice had demonstrated that the proliferation defect was largely corrected with the addition of exogenous IL-2 (19). Although activation markers were assessed relatively early in the course of T cell activation, we wanted to ensure that proliferation differences did not underlie the effects we had observed. Thus, as expected, addition of IL-2 to the cultures had no effect on the results (data not shown).
Figure 7. p85 is required for Tim-1-mediated CD69 and CD25 upregulation.
Purified CD4+ T cells from p85β or p85α/β deficient mice were stimulated in vitro with anti-CD3/CD28 antibodies (20 ng/ml and 0.5 μg/ml, respectively) and the indicated concentrations of Tim-1 antibody (A-D) or with anti-Tim-1 antibody alone (E-F). Cells were harvested and stained for CD69 (A,C,E) or CD25 (B,D,F) expression, and analyzed by flow cytometry. Results in A-B and E-F are single experiments, representative of three, or two, separate experiments, respectively. Panels C-D show effects of Tim-1 co-stimulation (+/- S.D.) averaged over those experiments, with p values indicated.
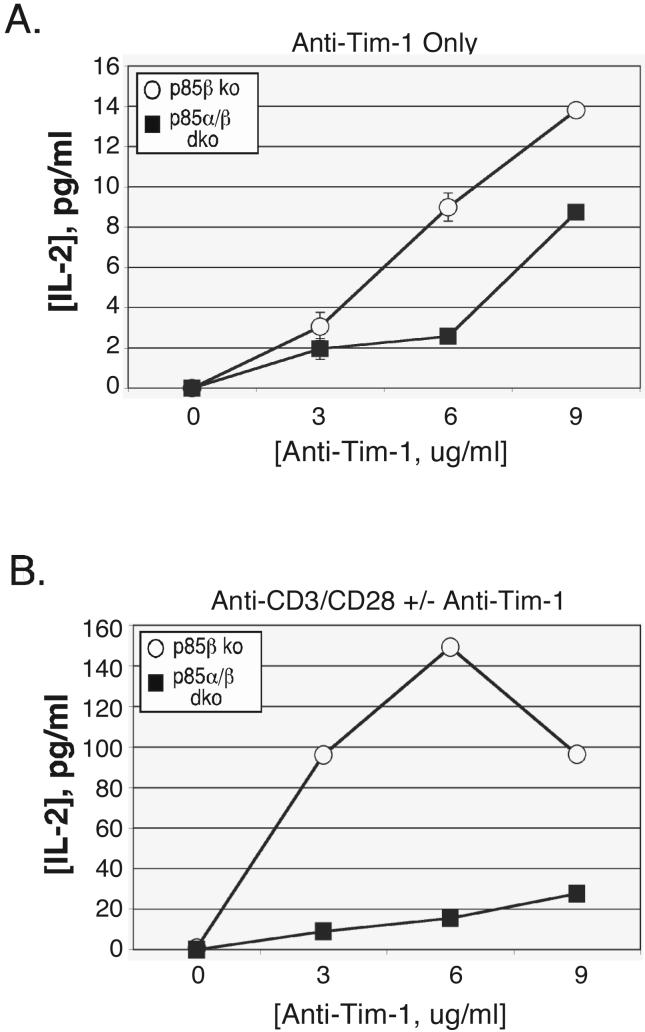
Finally, we examined cytokine production by the p85 mutant T cells and found that Tim-1 induction of IL-2 secretion was impaired in the p85 double knockout cells, compared with T cells lacking p85β alone (Fig. 8). In contrast to the more potent stimulatory effects of Tim-1 antibody on CD69 and CD25 induction, Tim-1 crosslinking by itself had a small effect on IL-2 secretion (note difference in scales between panels A and B), which was partially impaired in the p85 α/β deficient T cells (Fig. 8A). However, in the presence of anti-CD3/CD28 stimulation, Tim-1 ligation significantly enhanced the production of IL-2, an effect that is severely impaired in the p85 α/β deficient T cells (Fig. 8B).
Figure 8. p85 is required for Tim-1-mediated IL-2 production.
Purified CD4+ T cells from p85β or p85α/β deficient mice were stimulated in vitro with anti-CD3/CD28 antibodies (20 ng/ml and 0.5 μg/ml, respectively) and the indicated concentrations of Tim-1 antibody (A) or with anti-Tim-1 antibody alone (B). Supernatants were harvested after one day and analyzed by ELISA for IL-2. Error bars (obscured by the marker is most cases) indicate standard deviation for triplicate points within a single experiment, which is representative of three that were performed.
Discussion
Recent studies have demonstrated that the transmembrane protein Tim-1 can influence the course of an immune response through direct effects on T cell activation. However, the biochemical signaling pathways underlying these effects of Tim-1 ligation are not understood. Employing a combination of biochemical, pharmacological and genetic approaches, we delineate a signaling pathway, starting with Src kinase-mediated phosphorylation of Tim-1, to recruitment and activation of PI3K and Akt, which are required for induction of NFAT/AP-1-dependent transcription and up-regulation of surface activation markers and cytokines that are important for T cell activation and function.
The data we present here reveal a requirement for the Src family kinase Lck for Tim-1 tyrosine phosphorylation and subsequent NFAT/AP-1-dependent transcription. Our current model is that Lck first phosphorylates the cytoplasmic tail of Tim-1, which allows subsequent recruitment of signaling proteins to Y276, a residue that is required for Tim-1 function in T cell lines (7). It should be noted that our data are also consistent with a possible role for the related tyrosine kinase Fyn in the regulation of Tim-1 function. Thus, the JCaM.1 cell line, while lacking expression of Lck, also contains little if any Fyn protein (30). In addition, the kinase inhibitor PP2, although relatively specific for Src family kinases, cannot distinguish between possible functions for Lck or Fyn. Finally, in some SH2 domain array experiments, we noted weak binding of the Tim-1 phospho-Y276 peptide to the SH2 domain of Fyn. Further investigation is therefore warranted to address whether Fyn contributes to Tim-1 function.
Using an unbiased approach, we find that phosphorylation of Y276 leads to recruitment of the p85 subunits of PI3K, and we further confirm this interaction with endogenous p85 in T cells expressing Tim-1. Interestingly, interaction with p85 is a common feature shared by other T cell accessory molecules such as CD28, ICOS, and CTLA-4. However, in contrast to these molecules, which preferentially bind the carboxy-terminal SH2 domain of p85 (31-35), Tim-1 binds the amino-terminal SH2 domain, as revealed by the SH2 domain array. Another difference is that p85 binds to the CD28 family members via a consensus YXXM motif, whereas it binds to Tim-1 at a non-canonical sequence (YIVE). Although the amino-terminal p85 SH2 domain has a ten-fold lower avidity for the YXXM motif than does the carboxy-terminal SH2 domain (31), work from Songyang and colleagues suggests that YMXM is the preferred target for both domains (36). We have attempted to co-IP an isolated N-terminal p85α SH2 domain construct with Tim-1, but have been unable to do so (unpublished data), possibly due to the low affinity of the interaction in the absence of other sequences. Further investigation will be required to more precisely define how the Tim-1:p85 complex forms, and what other proteins may be involved. Nonetheless, our ability to co-IP p85 with Tim-1 in a phosphotyrosine-dependent manner (Fig. 3) and the observed interaction between the purified N-SH2 and peptide (again, phosphotyrosine-dependent; Fig. 2) suggest that this is a direct interaction.
Consistent with its recruitment of p85, Tim-1 requires PI3K and Akt activity to enhance T cell activation, since LY294002 and Akti 1/2 inhibit Tim-1 function. We also employed a recently described genetic model, in which there is a complete lack of expression of the p85 regulatory subunits of PI3K selectively in T cells (19). This is accompanied by a significant reduction in levels of the catalytic p110 subunit isoforms (which are normally stabilized by p85 binding), resulting in specific abrogation of Class IA PI3K activity in T cells. Consistent with previous data (19), CD25 and CD69 upregulation triggered by TCR stimulation was only mildly affected in the p85β and double k.o. T cells. However, the ability of Tim-1 to co-stimulate CD25 and CD69 is severely impaired in the double k.o. T cells, when compared with p85β-deficient T cells. Again consistent with previous findings (19), p85β-deficient T cells behave identically to wild-type T cells with regard to CD25 and CD69 induction (data not shown).
T cell activation induced by Tim-1 alone was observed in our earlier studies performed in Jurkat T cells and is also in agreement with other studies where hyperproliferation of T cells was observed in mice treated with soluble mTim-1 molecules, as well as activation of primary human cells treated with anti-Tim-1 antibody (6-8). A recent study has shown that Tim-1 can associate with the TCR-CD3 complex in the basal state, an interaction that is increased by Tim-1 or TCR/CD3 ligation (8). Tim-1 association with the TCR/CD3 complex could lead to aggregation of both, which may facilitate Tim-1 phosphorylation and activation of downstream signaling pathways through both TCR dependent and independent pathways. Indeed, we show that increasing amounts of agonistic anti-Tim-1 alone are accompanied by increased surface expression of CD69 and CD25. While there is a significant dampening of this response in T cells from p85 double knockout mice, higher concentrations of anti-Tim-1 are eventually sufficient to induce CD69 and CD25 expression. Though these T cells completely lack p85 regulatory subunits, proximal TCR-induced signaling seems relatively unaffected, since ZAP-70 phosphorylation is intact (19). Given that Tim-1 may also induce ZAP-70 phosphorylation through its interaction with the TCR (8), the residual effects of Tim-1 observed in p85-deficient T cells may be TCR-dependent.
Data presented here support the model that Tim-1 functions as a positive co-stimulatory molecule. However, anti-Tim-1 antibodies targeting different epitopes of the Tim-1 extracellular domain have been shown to initiate either positive or negative effects on T cell activation (9, 10, 12). Thus, two anti-Tim-1 antibodies, RMT1-10 and 3B3, differing by 17-fold in binding affinity to the same or closely related Tim-1 epitope in the IgV domain, exert opposite effects on T cell function (9). While Tim-1 ligation by RMT1-10 apparently inhibits T cell activation, cross-linking with the higher affinity antibody 3B3 potentiates T cell activation. Recent structural studies also predict different ligand binding modes for the TIM family members (37, 38), consistent with direct and indirect evidence for multiple ligands for these proteins (2, 6, 7, 39-41). Thus, it is possible that more than one ligand might interact with Tim-1 concurrently on different faces of the molecule. Furthermore, homotypic interactions between individual Tim-1 molecules are mediated through their Ig domains, interactions that may be affected by glycosylation of the polymorphic mucin domain (38). The ultimate outcome of Tim-1 engagement may therefore depend upon the nature of the ligand(s) with which it interacts, as well as the timing and stoichiometry of such interactions. Differences in functional outcomes after Tim-1 ligation may result from divergent effects of Tim-1 ligation on T cell signaling pathways under such circumstances.
While our study indicates that PI3K plays an important role in mediating Tim-1 signaling, this does not exclude the possibility that additional molecules can also bind to Tim-1, and transmit signals to other downstream pathways. Based on data presented here, we suggest that ligation of Tim-1, when coupled with TCR stimulation, enhances downstream signaling pathways that induce T cell activation, at least in part through PI3K and its downstream effector Akt. Future studies will focus on the mechanisms by which Tim-1-mediated PI3K activation affects T cell activation.
Acknowledgements
We are grateful to A. Weiss for providing C305 antibody. We also thank V. Kuchroo for sharing data prior to publication.
This work was supported by grants from the National Institutes of Health (AI67544 to L.P.K., AI50831 to D.A.F., P01 AI054456 and HL069507 to R.H.D. and T32 AI60573 (J.S.O.))
Footnotes
Disclosures The authors have no financial conflict of interest.
References
- 1.McIntire JJ, Umetsu SE, Akbari O, Potter M, Kuchroo VK, Barsh GS, Freeman GJ, Umetsu DT, DeKruyff RH. Identification of Tapr (an airway hyperreactivity regulatory locus) and the linked Tim gene family. Nat Immunol. 2001;2:1109–1116. doi: 10.1038/ni739. [DOI] [PubMed] [Google Scholar]
- 2.Kuchroo VK, Umetsu DT, DeKruyff RH, Freeman GJ. The TIM gene family: emerging roles in immunity and disease. Nat Rev Immunol. 2003;3:454–462. doi: 10.1038/nri1111. [DOI] [PubMed] [Google Scholar]
- 3.Meyers JH, Sabatos CA, Chakravarti S, Kuchroo VK. The TIM gene family regulates autoimmune and allergic diseases. Trends Mol Med. 2005;11:362–369. doi: 10.1016/j.molmed.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 4.de Souza AJ, Kane LP. Immune regulation by the TIM gene family. Immunol Res. 2006;36:147–155. doi: 10.1385/IR:36:1:147. [DOI] [PubMed] [Google Scholar]
- 5.Umetsu SE, Lee WL, McIntire JJ, Downey L, Sanjanwala B, Akbari O, Berry GJ, Nagumo H, Freeman GJ, Umetsu DT, Dekruyff RH. TIM-1 induces T cell activation and inhibits the development of peripheral tolerance. Nat Immunol. 2005;6:447–454. doi: 10.1038/ni1186. [DOI] [PubMed] [Google Scholar]
- 6.Meyers JH, Chakravarti S, Schlesinger D, Illes Z, Waldner H, Umetsu SE, Kenny J, Zheng XX, Umetsu DT, Dekruyff RH, Strom TB, Kuchroo VK. TIM-4 is the ligand for TIM-1, and the TIM-1-TIM-4 interaction regulates T cell proliferation. Nat Immunol. 2005;6:455–464. doi: 10.1038/ni1185. [DOI] [PubMed] [Google Scholar]
- 7.de Souza AJ, Oriss TB, O'Malley K, Ray A, Kane LP. TIM-1 is expressed on in vivo-activated T cells and provides a co-stimulatory signal for T cell activation. Proc Natl Acad Sci U S A. 2005;102:17113–17118. doi: 10.1073/pnas.0508643102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Binne LL, Scott ML, Rennert PD. Human TIM-1 Associates with the TCR Complex and Up-Regulates T Cell Activation Signals. J Immunol. 2007;178:4342–4350. doi: 10.4049/jimmunol.178.7.4342. [DOI] [PubMed] [Google Scholar]
- 9.Xiao S, Najafian N, Reddy J, Albin M, Zhu C, Jensen E, Imitola J, Korn T, Anderson AC, Zhang Z, Gutierrez C, Moll T, Sobel RA, Umetsu DT, Yagita H, Akiba H, Strom T, Sayegh MH, DeKruyff RH, Khoury SJ, Kuchroo VK. Differential engagement of Tim-1 during activation can positively or negatively costimulate T cell expansion and effector function. J Exp Med. 2007;204:1691–1702. doi: 10.1084/jem.20062498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sizing ID, Bailly V, McCoon P, Chang W, Rao S, Pablo L, Rennard R, Walsh M, Li Z, Zafari M, Dobles M, Tarilonte L, Miklasz S, Majeau G, Godbout K, Scott ML, Rennert PD. Epitope-dependent effect of anti-murine TIM-1 monoclonal antibodies on T cell activity and lung immune responses. J Immunol. 2007;178:2249–2261. doi: 10.4049/jimmunol.178.4.2249. [DOI] [PubMed] [Google Scholar]
- 11.Mesri M, Smithson G, Ghatpande A, Chapoval A, Shenoy S, Boldog F, Hackett C, Pena CE, Burgess C, Bendele A, Shimkets RA, Starling GC. Inhibition of in vitro and in vivo T cell responses by recombinant human Tim-1 extracellular domain proteins. Int Immunol. 2006 doi: 10.1093/intimm/dxh388. [DOI] [PubMed] [Google Scholar]
- 12.Encinas JA, Janssen EM, Weiner DB, Calarota SA, Nieto D, Moll T, Carlo DJ, Moss RB. Anti-T-cell Ig and mucin domain-containing protein 1 antibody decreases TH2 airway inflammation in a mouse model of asthma. J Allergy Clin Immunol. 2005;116:1343–1349. doi: 10.1016/j.jaci.2005.08.031. [DOI] [PubMed] [Google Scholar]
- 13.Rudd CE, Schneider H. Unifying concepts in CD28, ICOS and CTLA4 co-receptor signalling. Nat Rev Immunol. 2003;3:544–556. doi: 10.1038/nri1131. [DOI] [PubMed] [Google Scholar]
- 14.Vanhaesebroeck B, Leevers SJ, Ahmadi K, Timms J, Katso R, Driscoll PC, Woscholski R, Parker PJ, Waterfield MD. Synthesis and function of 3-phosphorylated inositol lipids. Annu Rev Biochem. 2001;70:535–602. doi: 10.1146/annurev.biochem.70.1.535. [DOI] [PubMed] [Google Scholar]
- 15.Okkenhaug K, Vanhaesebroeck B. New responsibilities for the PI3K regulatory subunit p85 alpha. Sci STKE 2001:E1. 2001 doi: 10.1126/stke.2001.65.pe1. [DOI] [PubMed] [Google Scholar]
- 16.Goldsmith MA, Weiss A. Isolation and characterization of a T-lymphocyte somatic mutant with altered signal transduction by the antigen receptor. Proc Natl Acad Sci USA. 1987;84:6879–6883. doi: 10.1073/pnas.84.19.6879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Straus DB, Weiss A. Genetic evidence for the involvement of the lck tyrosine kinase in signal transduction through the T cell antigen receptor. Cell. 1992;70:585–593. doi: 10.1016/0092-8674(92)90428-f. [DOI] [PubMed] [Google Scholar]
- 18.Kane LP, Mollenauer MN, Weiss A. A proline-rich motif in the C terminus of Akt contributes to its localization in the immunological synapse. J Immunol. 2004;172:5441–5449. doi: 10.4049/jimmunol.172.9.5441. [DOI] [PubMed] [Google Scholar]
- 19.Deane JA, Kharas MG, Oak JS, Stiles LN, Luo J, Moore TI, Ji H, Rommel C, Cantley LC, Lane TE, Fruman DA. T cell function is partially maintained in the absence of class IA phosphoinositide 3-kinase signaling. Blood. 2007;109:2894–2902. doi: 10.1182/blood-2006-07-038620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kane LP, Shapiro VSS, Stokoe D, Weiss A. Induction of NF-κB by the Akt/PKB kinase. Curr Biol. 1999;9:601–604. doi: 10.1016/s0960-9822(99)80265-6. [DOI] [PubMed] [Google Scholar]
- 21.O'Shea JJ, McVicar DW, Bailey TL, Burns C, Smyth MJ. Activation of human peripheral blood T lymphocytes by pharmacological induction of protein-tyrosine phosphorylation. Proc Natl Acad Sci U S A. 1992;89:10306–10310. doi: 10.1073/pnas.89.21.10306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Songyang Z, Cantley LC. Recognition and specificity in protein tyrosine kinase-mediated signalling. Trends Biochem Sci. 1995;20:470–475. doi: 10.1016/s0968-0004(00)89103-3. [DOI] [PubMed] [Google Scholar]
- 23.Bain J, McLauchlan H, Elliott M, Cohen P. The specificities of protein kinase inhibitors: an update. Biochem J. 2003;371:199–204. doi: 10.1042/BJ20021535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davies SP, Reddy H, Caivano M, Cohen P. Specificity and mechanism of action of some commonly used protein kinase inhibitors. Biochem J. 2000;351:95–105. doi: 10.1042/0264-6021:3510095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parry RV, Reif K, Smith G, Sansom DM, Hemmings BA, Ward SG. Ligation of the T cell co-stimulatory receptor CD28 activates the serine-threonine protein kinase protein kinase B. Eur J Immunol. 1997;27:2495–2501. doi: 10.1002/eji.1830271006. [DOI] [PubMed] [Google Scholar]
- 26.Narayan P, Holt B, Tosti R, Kane LP. CARMA1 is required for Akt-mediated NF-kappaB activation in T cells. Mol Cell Biol. 2006;26:2327–2336. doi: 10.1128/MCB.26.6.2327-2336.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Testi R, Phillips JH, Lanier LL. Leu 23 induction as an early marker of functional CD3/T cell antigen receptor triggering. Requirement for receptor crosslinking, prolonged elevation of intracellular [Ca++] and stimulation of protein kinase C. J Immunol. 1989;142:1854–1860. [PubMed] [Google Scholar]
- 28.Yokoyama WM, Koning F, Kehn PJ, Pereira GM, Stingl G, Coligan JE, Shevach EM. Characterization of a cell surface-expressed disulfide-linked dimer involved in murine T cell activation. J Immunol. 1988;141:369–376. [PubMed] [Google Scholar]
- 29.Deane JA, Trifilo MJ, Yballe CM, Choi S, Lane TE, Fruman DA. Enhanced T cell proliferation in mice lacking the p85beta subunit of phosphoinositide 3-kinase. J Immunol. 2004;172:6615–6625. doi: 10.4049/jimmunol.172.11.6615. [DOI] [PubMed] [Google Scholar]
- 30.Denny MF, Patai B, Straus DB. Differential T-cell antigen receptor signaling mediated by the Src family kinases Lck and Fyn. Mol Cell Biol. 2000;20:1426–1435. doi: 10.1128/mcb.20.4.1426-1435.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prasad KV, Cai YC, Raab M, Duckworth B, Cantley L, Shoelson SE, Rudd CE. T-cell antigen CD28 interacts with the lipid kinase phosphatidylinositol 3-kinase by a cytoplasmic Tyr(P)-Met-Xaa-Met motif. Proc Natl Acad Sci U S A. 1994;91:2834–2838. doi: 10.1073/pnas.91.7.2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.August A, Dupont B. CD28 of T lymphocytes associates with phosphatidylinositol 3-kinase. Int Immunol. 1994;6:769–774. doi: 10.1093/intimm/6.5.769. [DOI] [PubMed] [Google Scholar]
- 33.Truitt KE, Shi J, Gibson S, Segal LG, Mills GB, Imboden JB. CD28 delivers costimulatory signals independently of its association with phosphatidylinositol 3-kinase. Journal of Immunology. 1995;155:4702–4710. [PubMed] [Google Scholar]
- 34.Schneider H, Cai YC, Prasad KV, Shoelson SE, Rudd CE. T cell antigen CD28 binds to the GRB-2/SOS complex, regulators of p21ras. Eur J Immunol. 1995;25:1044–1050. doi: 10.1002/eji.1830250428. [DOI] [PubMed] [Google Scholar]
- 35.Coyle AJ, Lehar S, Lloyd C, Tian J, Delaney T, Manning S, Nguyen T, Burwell T, Schneider H, Gonzalo JA, Gosselin M, Owen LR, Rudd CE, Gutierrez-Ramos JC. The CD28-related molecule ICOS is required for effective T cell-dependent immune responses. Immunity. 2000;13:95–105. doi: 10.1016/s1074-7613(00)00011-x. [DOI] [PubMed] [Google Scholar]
- 36.Songyang Z, Shoelson SE, Chaudhuri M, Gish G, Pawson T, Haser WG, King F, Roberts T, Ratnofsky S, Lechleider RJ, et al. SH2 domains recognize specific phosphopeptide sequences. Cell. 1993;72:767–778. doi: 10.1016/0092-8674(93)90404-e. [DOI] [PubMed] [Google Scholar]
- 37.Cao E, Zang X, Ramagopal UA, Mukhopadhaya A, Fedorov A, Fedorov E, Zencheck WD, Lary JW, Cole JL, Deng H, Xiao H, Dilorenzo TP, Allison JP, Nathenson SG, Almo SC. T cell immunoglobulin mucin-3 crystal structure reveals a galectin-9-independent ligand-binding surface. Immunity. 2007;26:311–321. doi: 10.1016/j.immuni.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 38.Santiago C, Ballesteros A, Martinez-Munoz L, Mellado M, Kaplan GG, Freeman GJ, Casasnovas JM. Structures of T Cell Immunoglobulin Mucin Protein 4 Show a Metal-Ion-Dependent Ligand Binding Site where Phosphatidylserine Binds. Immunity. 2007;27:941–951. doi: 10.1016/j.immuni.2007.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhu C, Anderson AC, Schubart A, Xiong H, Imitola J, Khoury SJ, Zheng XX, Strom TB, Kuchroo VK. The Tim-3 ligand galectin-9 negatively regulates T helper type 1 immunity. Nat Immunol. 2005;6:1245–1252. doi: 10.1038/ni1271. [DOI] [PubMed] [Google Scholar]
- 40.Chen TT, Li L, Chung DH, Allen CD, Torti SV, Torti FM, Cyster JG, Chen CY, Brodsky FM, Niemi EC, Nakamura MC, Seaman WE, Daws MR. TIM-2 is expressed on B cells and in liver and kidney and is a receptor for Hferritin endocytosis. J Exp Med. 2005;202:955–965. doi: 10.1084/jem.20042433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Savill J, Gregory C. Apoptotic PS to Phagocyte TIM-4: Eat Me. Immunity. 2007;27:830–832. doi: 10.1016/j.immuni.2007.12.002. [DOI] [PubMed] [Google Scholar]