INTRODUCTION
Isocyanates, highly reactive chemicals used to manufacture polyurethane paints, foams and other products, remain a major cause of occupational asthma, especially in end-use settings such as auto body repair shops. Isocyanate exposure assessment and control has focused primarily on respiratory exposures, but skin exposure likely can also contribute to sensitization and asthma (Bello et al., 2007a; Redlich and Herrick, 2008). The auto body industry uses isocyanates, primarily hexamethylene diisocyanate and isophorone diisocyanate, as the hardener component in polyurethane coatings, which typically contain <1% volatile monomers and >99% non-volatile polyisocyanates (Bello et al., 2002, 2007b). Assessing skin exposure to isocyanates in the auto body repair setting presents a significant challenge. The methodologies for assessing isocyanate skin exposure are limited, and further complicated by the nature of auto body repair work, which involves a variety of sporadic tasks, numerous different isocyanate products in multiple small shops and inconsistent use of personal protective equipment (PPE).
The Survey of Painters and Repairers of Autobodies by Yale (SPRAY) study investigating isocyanate dose–response relationships initially focused on respiratory exposures (Redlich et al., 2001; Sparer et al., 2004; Woskie et al., 2004). It was not feasible to obtain detailed exposure data on each auto body shop worker to evaluate exposure–response relationships. Thus, a task-based exposure algorithm was developed, using task-based measured airborne concentrations, daily diaries of tasks performed and use of PPE, to assess personal isocyanate inhalation exposures (Woskie et al., 2004, 2008).
With increased awareness of the potential risks of isocyanate skin exposure and demonstration of skin exposure in a pilot study (Liu et al., 2000), SPRAY was expanded to include evaluation of isocyanate skin exposures using qualitative and quantitative methodologies (Liu et al., 2007; Bello et al., 2008). SWYPE™ colorimetric indicators (CLI, Des Plains, IL, USA) were validated as a tool for isocyanate skin exposure and used to assess task-based skin exposures in auto body shop workers following painting and non-painting tasks (Liu et al., 2007). These colorimetric indicator pads, which measure the aliphatic total isocyanate groups, were used to evaluate isocyanate contamination on skin surfaces exposed during auto body repair tasks or underneath gloves, paint suits or a respirator. A more limited quantitative skin exposure assessment was also conducted in 22 of the 35 SPRAY shops using similar wipe pads, which were analyzed for the total isocyanate group content with the National Institute for Occupational Safety and Health (NIOSH) 5525 method (Bello et al., 2008).
This paper describes the development of a (semiquantitative) algorithm to estimate personal skin exposures (daily and weekly) for an epidemiologic study of auto body shop workers. To account for the variable work pattern in auto body shops, task-based skin exposure data and daily work diaries that included tasks and use of PPE were used to estimate an individual skin exposure metric. The qualitative indicators described above were used in this algorithm rather than the quantitative wipe data due to the larger number of qualitative samples obtained in all surveyed shops and the greater range of tasks sampled. This individual daily and weekly skin exposure index (SEI) was compared to previously developed respiratory exposure metrics (Woskie et al., 2008) to evaluate their relationships and will be used in future analyses to estimate the contribution of skin (as well as respiratory) isocyanate exposures to immunologic, respiratory and other outcomes in the SPRAY epidemiologic study.
MATERIALS AND METHODS
Auto body shop work process and task-based skin exposure assessment
The skin exposure assessment supplemented the ongoing SPRAY study. Study design, study population and work processes are described in previous publications (Redlich et al., 2001; Sparer et al., 2004; Woskie et al., 2004; Liu et al., 2007; Woskie et al., 2008). Briefly, auto body shop work can be classified as painting and non-painting tasks, including paint mixing, spray painting (sealer, primer, base and clear coatings), grinding, sanding, polishing, compounding (use of abrasive compounds to grind the surface layers) and management or office work. As previously described, task-based skin exposure was evaluated in 124 auto body shop workers from 35 shops using colorimetric indicators (Liu et al., 2007). Both unprotected skin areas and skin under the protection of PPE were evaluated following painting and non-painting tasks using SWYPE™ and Permea-Tec™ colorimetric indicators (CLI). Briefly, the SWYPE™ color indicators were used to wipe unprotected skin areas and skin areas covered by a half-facepiece cartridge respirator (skin areas covered by a dust mask or a full-facepiece respirator were not evaluated). The Permea-Tec™ patches were placed on thumb, index and middle fingers and the palm center to evaluate isocyanate breakthrough of gloves and on the right chest or inner clothing to evaluate the breakthrough of protective clothing. Wipes that changed color after a task were recorded as positive and the percent positive (we have previously used the term ‘rate of positive samples’) was calculated as the number of positive samples divided by the total samples for each task.
To identify the daily tasks with possible isocyanate skin exposures, all tasks each SPRAY auto body participant (n = 232 workers) performed daily were evaluated, using the work diary checklists that had been developed for estimating personal respiratory exposures as previously described (Sparer et al., 2004; Woskie et al., 2008). Briefly, these diaries were obtained on each SPRAY worker during four consecutive workdays (Monday through Thursday) when medical evaluations were performed, noting what tasks a worker had performed and the type of PPE used (if any) every ½ h. Tasks with possible skin exposures were identified based on the task-percent of positive samples obtained from the colorimetric indicators.
Semiquantitative algorithm
Results from task-based qualitative skin wipe sampling with and without use of PPE and the daily work diaries were used to develop the skin exposure algorithm. The fraction of the surface area of each body part protected by PPE (coverall, gloves and respirator) over the total surface area that can be exposed was also taken into account. Spray painters might wear T-shirts with hands, forearms, face and neck exposed. When gloves were used, as indicated in the diary, the hands were covered; when a half-facepiece respirator was worn, a large part of the face was covered. If a nylon or Tyvek suit was used as indicated in the diary, the arms and neck were covered. Reference values for the fractional surface area of body parts likely to be exposed in an auto body workplace were used as a weighting factor in the algorithm.
Reference values for skin areas of body parts were obtained from the burn management algorithm in the ‘Lund–Browder’ charts in Figure 129-1 of Wolf and Prnitt (2008). The surface areas of body parts with potential isocyanate exposure (hands, forearms, face and neck) were expressed as a fraction of the total body surface area: both hands 0.05 (2 × 0.025; i.e. each hand makes up 2.5% of the total body skin surface area), forearms 0.06 (2 × 0.03), face 0.035 (face area is approximately half of the head area or 0.07/2 = 0.035) and the neck area 0.02 (Table A-1, OECD, 1997). The total fractional surface area of hands, forearms, face and neck is 0.165 or 16.5% of the total body surface area.
These data were used to develop a semiquantitative SEI that estimated daily and weekly isocyanate skin exposure for each worker (see Results and Table 3 for more details on skin surface areas and calculations).
Table 3.
Skin surface area of body parts expressed as a fraction of total body surface area and total exposed area (FShand, forearm and face and neck) used in the algorithm
| Body part type | Body part surface area as a fraction of total body areaa | Fraction of potentially exposed skin area that could be covered by PPEb |
| Hands (both) | 0.05 | 0.303 |
| Forearms (both) | 0.06 | 0.364 |
| Face and neck | 0.055 | 0.333 |
| Face | 0.035 | 0.212 |
| Neck | 0.02 | 0.121 |
| Sum of fractions | 0.165 | 1.000 |
Based on Lund–Browder charts in Figure 129-1 of Wolf and Prnitt (2008).
Fraction of potentially exposed skin area that could be covered by PPE is the [body part surface area fraction/sum of total fractions (0.165)]. This is a body part fraction normalized to the surface area available for exposure since each body part can be exposed during a task, but can also be covered by PPE, such as a respirator, gloves or coveralls.
Statistical analysis
All data analysis was conducted using SAS® (Statistical Analysis Software, Version 9.13; SAS Institute, Cary, NC, USA). The qualitative wipe sampling data and work diary data were merged with the sample and shop information by shop and sample IDs. Personal daily SEI data were calculated for all SPRAY participants for each day and averaged for all survey days during the survey week (Monday through Thursday) as the weekly SEI. SEI data were checked for normality. Descriptive statistics (median, 10th–90th percentile, maximum) were calculated for daily SEI and weekly average SEI by self-reported job title (painter, technician and office worker). A Kruskal–Wallis rank sum chi-square test was performed to test the differences in daily SEI and weekly average SEI among the three job groups. Box plots were made for daily and weekly SEIs by job title. A correlation analysis was also performed on the daily and weekly SEIs with daily and weekly respiratory exposure indices (μg NCO m−3) using Spearman's rank correlation coefficients.
RESULTS
The percent of skin positive samples for different spray painting and paint-related tasks performed without PPE and using PPE are shown in Tables 1 and 2, respectively, based on our prior qualitative assessment of skin exposure (Liu et al., 2007). For the exposure algorithm, some tasks were combined, either because they were not significantly different from each other and/or because the diary information did not permit use of subcategories within a task. For example, percent positive for several paint-related tasks were combined, as the tasks were brief and frequently performed within the same ½ h time period in the diaries (Table 1). Similarly for percent positive under gloves, all painting tasks were combined into ‘spray painting’ (Table 2). For a few tasks that were not qualitatively sampled both with and without PPE, percent positive for related or similar tasks were used. For example, the percent positive for gun cleaning with non-protected hands was assumed to be the same as that for the painting task without gloves that occurred right before the spray gun was cleaned (Table 1).
Table 1.
Percent of positive samples for unprotected skin used in the algorithm
| Task | Number of samples (total = 220) | Number of positive samples (%) |
| Spray painting | ||
| Priming/sealing | 51 | 14 (27) |
| Clear coating | 84 | 38 (45) |
| Paint mixing | 23 | 10 (43) |
| Spray gun cleaning | 0 | (27 or 45)a |
| Paint-relatedb | 52 | 12 (23) |
Percent positive was not measured for this task. It was assumed similar to that of the painting task without gloves done right before the gun cleaning.
Including sanding, buffing, compounding and polishing tasks.
Table 2.
Percent of positive samples for protected skin used in the algorithm
| PPE type/task | Number of samples (total = 181) | Number of positive samples (%) |
| Under gloves | ||
| Spray painting | 65 | 15 (23) |
| Paint mixing | 41 | 3 (7) |
| Spray gun cleaning | 5 | 4 (80) |
| Paint-relateda | 0 | (7)b |
| Under respirator | ||
| Spray painting | 27 | 0 (0) |
| Under coverall | ||
| Spray painting | 43 | 1 (2) |
Including sanding, buffing, compounding and polishing tasks.
Percent positive was not measured under gloves for these tasks, which was assumed similar to that in paint mixing under gloves.
A semiquantitative SEI was developed that estimated a body surface area- and PPE use-weighted sum of positive skin exposure events for paint-related tasks. After the SEI was calculated for each painting, mixing, gun cleaning and paint-related and non-paint-related task, they were added together as the daily SEI. SEIs from all workdays were then averaged as the weekly SEI for each worker. For non-paint-related task, a 0% positive was used based on our findings for these tasks (0 positive per 50 samples, Liu Y, Stowe MH, Bello D, Sparer J, Gore RJ, Cullen MR, Redlich CA, Woskie SR, unpublished data).
For spray painting tasks where exposures involve the whole body, the general model for SEI is defined as follows:
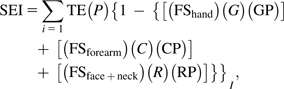 |
(1) |
where i = task type (1, …, I); TE = total number of isocyanate task events (each ½ h counted as one event) per day from the work diary; P = task-based average percent of skin positive samples when no PPE was used (27% for priming/sealing; 45% for clear coating. See Table 1 last column); {1−{[(FShand) (G)(GP)] + [(FSforearm) (C) (CP)] + [(FSface + neck) (R) (RP)]}} = the decrease in the SEI based on the amount of skin surface area covered by PPE (FS) and the PPE protection fraction (GP, CP and RP). When no PPE is worn G or C or R = 0 so the applicable term drops out. When PPE is worn G or C or R =1; and FS = fraction of potentially exposed skin surface area that could be covered by PPE during the task event (i.e. total normalized area of hands, forearms, face and neck equals 1). Specific values for surface areas of body part are given in Table 3.
FSface + neck = fraction of the surface area of face and neck covered by a respirator that varies by respirator type.
A half-facepiece respirator covers ∼22% of the face surface area only, so FSface + neck = (0.212 × 0.22 + 0.121 × 0) = 0.05.
A full-facepiece respirator (cartridge, powered air-purifying respirator or tight-fitting and loose-fitting supplied air respirators) covers essentially all of the face but none of the neck, so FSface + neck = (0.212 × 1 + 0.121 × 0) = 0.212. A supplied air respirator with hood covers both the face and neck, so FSface + neck = (0.212 × 1+ 0.121×1) = 0.333.
G, C, R = use of PPE 0 = no 1 = yes for gloves, coveralls, respirator; GP = glove protection (percent negative) = 1 − percent positive under gloves for spraying with any type of isocyanate paint = 1 − 0.23 (see Table 2); CP = coverall protection (percent negative) = 1 − percent positive under coverall for spraying with any type of isocyanate paint = 1 – 0.02 (see Table 2); and RP = respirator protection (percent negative) = 1 − percent positive under respirator for all isocyanate spraying = 1 − 0 (see Table 2).
For the following diary tasks: mixing of isocyanate-containing paint, spray gun cleaning and other paint-related tasks such as dry and wet sanding, the exposure was simplified to involve the hands only. Equation (1) is reduced to equation (2):
| (2) |
where TE, G and FShand are defined as in equation (1); P = task-based average percent of skin positive samples from Table 1—mixing isocyanate paints = 43%, other isocyanate paint-related tasks (sanding) = 23% and gun cleaning had no samples, therefore use the percent positive for the type of paint sprayed in the same ½ h as gun cleaning (if more than one type paint, use highest percent positive; if no paint, look at previous ½ h) and GP = glove protection (percent negative) = 1 − percent positive under gloves (see Table 2).
When there was a single task during the ½ h, that task P was used. If there were multiple tasks during the ½ h, the highest P was used for that ½ h. For each worker on each day, the SEI was the sum of SEIs from all tasks (SEIday); for each worker for each week, the total SEI was the sum of the SEIday from 4 days (Monday through Thursday).
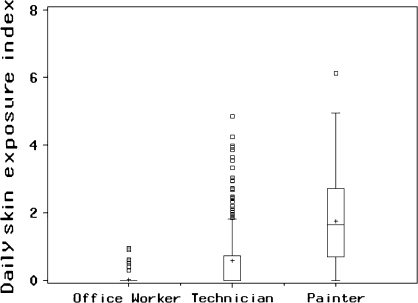
Daily SEIs were then calculated for all 232 SPRAY workers (49 painters, 118 technicians and 65 office workers) from 33 auto body shops, resulting in 893 person-days (245 days for office workers, 458 days for body technicians and 190 days for painters) based on presence during the study week as recorded in the diary, using this algorithm. The daily SEI ranged from 0 to 6.1, and the 10th–90th percentile range was 0–3.5. The median (10th–90th percentile, maximum) daily SEI was 0 (0–0, 1.0), 0 (0–1.9, 4.8) and 1.6 (0–3.5, 6.1) for office workers, technicians and painters, respectively. There was a significant difference in daily SEI between job titles (Kruskal–Wallis rank sum chi-square = 332.6, df = 2, P < 0.0001), with painters having the highest daily SEIs and office workers the lowest SEIs, as shown in Fig. 1. Box plots of daily SEI by job title showed a range of SEIs for each job category with considerable overlap between technicians and painters (Fig. 1) and no skin exposure for most office workers, as expected.
Fig. 1.
Distribution of daily isocyanate SEI by job category (n = 893 worker days). The top of box plots represents the upper quartile (75%tiles), the bottom represents the lower quartile (25%tile), the middle line represents the median (50%tile) and ‘+’ indicates the arithmetic mean. The top bar (whisker) is the maximum value and lower bar is the minimum value which are not outliers. The squares outside the top bar indicate outliers.
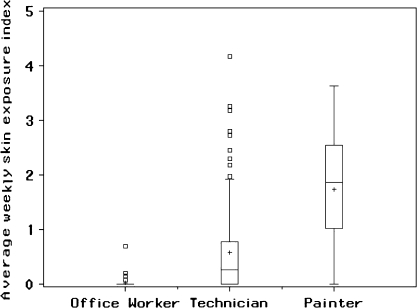
Each worker's weekly average SEI was also calculated for Monday to Thursday (Fig. 2), with similar differences between job categories. The weekly average SEI ranged from 0 to 4.2 and the 10th–90th percentile ranged from 0 to 3.0 with a median value of 0.2 for all workers. Weekly average SEI was 0 (0–0.0, 0.7), 0.3 (0–1.6, 4.2) and 1.9 (0.4–3.0, 3.6) for office workers, technicians and painters, respectively. There was also a significant difference in SEI between job titles (Kruskal–Wallis rank sum chi square = 118.7, df = 2, P < 0.0001), with painters having the highest SEIs. Box plots of weekly average SEI by job title were similar to daily SEI, showing a range of skin exposures, with considerable overlap between technicians and painters (Fig. 2).
Fig. 2.
Distribution of weekly isocyanate average SEI by job category (n = 232 workers). See Fig. 1 for the interpretation of box plots.
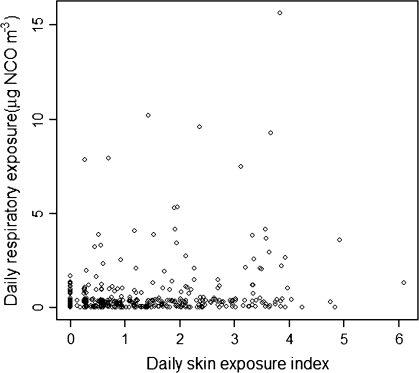
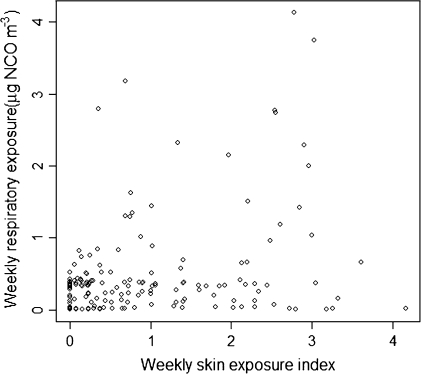
The skin exposure indices estimated for individual workers were compared to the respiratory exposures (μg NCO m−3) estimated for the same workers using the quantitative task-based exposure algorithm previously developed (Woskie et al., 2008), in order to evaluate the relationship between air and skin exposure levels. Daily SEI and the daily time-weighted average (TWA) air concentration (μg NCO m−3) were weakly correlated (r = 0.380; P < 0.0001), as shown in Fig. 3. As expected, there is a general positive trend between SEI and the respiratory exposure. However, there are clearly workers with minimal daily isocyanate respiratory exposure and high daily skin exposure indices and vice versa. The weekly average SEI and the weekly TWA air concentration (μg NCO m−3) were similarly correlated (r = 0.482; P < 0.0001), as shown in Fig. 4.
Fig. 3.
Relationship between daily SEI and daily respiratory exposure to isocyanates (μg NCO m−3), n = 893 worker days.
Fig. 4.
Relationship between weekly average SEI and weekly average respiratory exposure to isocyanates (μg NCO m−3), n = 232 workers.
DISCUSSION
Despite growing concerns about the role of skin exposure in isocyanate sensitization and asthma, methods to evaluate isocyanate skin exposures remain very limited, and skin exposure assessment has rarely been incorporated into occupational epidemiologic studies of isocyanate-exposed workers (Petsonk et al., 2000; Pronk et al., 2006; Bello et al., 2007a). This paper is the third in the series describing isocyanate skin exposures in auto body shops (Liu et al., 2007; Bello et al., 2008). It describes the development of a task-based skin exposure algorithm to estimate daily and weekly isocyanate skin exposures for each auto body shop worker, based on task-based qualitative isocyanate skin exposure data and daily work diaries obtained as part of the SPRAY study (Redlich et al., 2001; Sparer et al., 2004; Woskie et al., 2004).
Individual skin exposures were quite variable, with painters and technicians having the highest exposures and skin exposure was uncommon among office workers. An important finding is that individual skin and respiratory exposure indices, although related, are not highly correlated (r = 0.38 for daily exposure). Not unexpectedly, painters have the highest skin exposure, as tasks such as spray painting can have relatively high respiratory and skin isocyanate exposures, which can be modified by factors such as the use of PPE (Woskie et al., 2004; Liu et al., 2006, 2007). However, it is notable that worker isocyanate skin exposures cannot be reliably estimated from respiratory exposure. Isocyanate skin exposures were variable and also relatively high in some technicians as well as painters, consistent with tasks such as mixing or sanding that can have relatively high isocyanate skin exposure (Table 1) and relatively low respiratory exposure (Woskie et al., 2008). Wet sanding in particular is a task that seldom has any respiratory exposure (water is used for sanding), but has relatively high skin exposure (45%). This weak correlation between individual skin and respiratory exposure indices should enable evaluation of the contribution of both respiratory and skin exposure to health-related end points. Pronk et al. (2006) found that skin and airborne exposures were closely correlated. However, the skin exposure assessment in their study was based only on hand exposure (estimated from glove extraction), did not take into account use of PPE or exposure to other body parts such as arms, face and neck and only included spray painters and spray tasks.
The skin exposure algorithm reported here has several strengths. Importantly, it is task based. Isocyanate exposures commonly occur in small end-use settings such as auto body shops, where workers perform a number of different job tasks, frequently with irregular work patterns, leading to sporadic and variable isocyanate exposures (Sparer et al., 2004). Task-based exposure assessment can assess exposures in a range of tasks and, when combined with a work diary, can estimate individual worker exposure (Warren et al., 2006; Woskie et al., 2008). The task-based isocyanate skin exposure used for this algorithm was based on a relatively large number of skin exposure samples (>400), obtained on all major auto body shop tasks with potential isocyanate skin exposure using qualitative colorimetric indicators that have previously been validated (Liu et al., 2007). Detailed daily work diaries obtained on each worker enabled estimation of a daily and weekly personal SEI for each worker, incorporating frequency and duration of exposure during a variety of different tasks.
Another strength of this skin exposure algorithm is that total body skin exposure was estimated and the individual SEIs were adjusted for the use of PPE (respirator, gloves and protective clothing) and the protection achieved. This adjustment was possible since isocyanate skin exposure was evaluated on different body parts (e.g. hands/face) with and without PPE for most tasks and individual PPE use was recorded in the diaries. Thus, the estimated SEI takes into account the use and effectiveness of the PPE worn. Importantly, the daily and weekly average isocyanate SEIs were compared with the comparable quantitative respiratory TWA exposure metrics. The relatively weak correlation between individual skin and respiratory exposures will enable future analyses to determine whether skin and respiratory exposures independently contribute to isocyanate asthma or other end points such as immunologic markers.
Skin exposure assessment is much less developed than respiratory exposure assessment (Schneider et al., 2000; Vermeulen et al., 2002). Several limitations of the skin exposure algorithm should be noted. For one, the SEI depends on the accuracy of the qualitative skin wipes. These wipes have been validated in comparison with quantitative wipes but also have limitations, as previously noted, including less sensitivity than quantitative wipes and probable underestimation of skin exposure (Liu et al., 2007). The percent of skin exposure for different tasks was based on the percent positive qualitative wipes for each task and did not differentiate color intensity or concentration of exposure, which can vary for any task (Liu et al., 2007). The SEI is thus based on exposure fraction and is an index, rather than a quantitative estimate that can be expressed as μg NCO per surface area. As noted above, the quantitative wipe results were not used due to the more limited number of quantitative samples that could be obtained and analyzed. Pronk et al. (2006) used a glove extraction method to evaluate dermal hand exposures during spray painting. Tape stripping has been used to evaluate skin exposure in a single spray painter, but has not yet been utilized to estimate exposure in a larger number of workers (Fent et al., 2006). Petsonk et al. (2000) used questionnaire data to evaluate skin spotting as an indicator of isocyanate skin exposure, but did not confirm or quantify isocyanate skin exposure. Other skin exposure approaches such as theoretical modeling, observational methods or expert judgment have not to our knowledge been applied to isocyanates (Schneider et al., 2000; Vermeulen et al., 2002; van Wendel de Joode et al., 2005). Biomarkers of isocyanate exposure are not specific for skin exposure and have shown variable associations with exposure (Pronk et al., 2006; Bello et al., 2007a). Thus, despite limitations, the task-based skin algorithm developed in this article likely provides the most comprehensive approach to-date to estimate individual worker isocyanate skin exposure.
Sampling under PPE was determined largely by what PPE was worn by the workers. Gloves worn were predominantly latex despite the recommendation of using nitrile by the paint manufacturers. For respirators, we assessed exposures under half-facepiece respirators with organic vapor cartridges and prefilters as these were most commonly worn (Sparer et al., 2004; Liu et al., 2006). We did not take wipe samples under dust masks, powered air-purifying respirators and full-facepiece supplied air respirators, which were infrequently used. Using the percent positive under half-facepiece cartridge respirators to calculate the SEI for other respirator types might have introduced bias. For underneath protective clothing, the algorithm neither evaluates the type of protective clothing worn by workers (nylon suits versus Tyvek etc.) nor does it account for short-sleeved versus long-sleeved work shirts among those not wearing PPE clothing.
Other limitations relate to the accuracy of the work diary, and how representative the survey week was of more long-term exposure. Efforts were made with the shop management to select a survey week that represented a typical work week, but work could be variable from week to week.
Despite these limitations, this skin exposure algorithm is the first attempt we are aware of that provides the most comprehensive approach to estimate individual worker isocyanate skin exposure based on field isocyanate skin exposure data.
In summary, the skin exposure algorithm developed in this study provides task-based daily and weekly average worker SEIs that are adjusted for individual use of PPE. Comparison of individual worker SEIs with TWA respiratory exposures (μg NCO m−3) estimated for the same workers using a task-based algorithm showed a relatively weak positive correlation. The application of the isocyanate skin exposure metric developed here to the SPRAY epidemiologic study is essential, but is beyond the scope of this article. Extensive analysis of the relative contribution of isocyanate skin and respiratory exposures and other risk factors in the SPRAY study will be presented separately.
FUNDING
US National Heart, Lung and Blood Institute/National Institutes of Health (1R01-HL62932); National Institute for Occupational Safety and Health/Centers for Disease Control and Prevention (1R01OH03457); National Institute of Environmental Health Sciences (K24-ES00355) to C.A.R.
Acknowledgments
We thank shop management and workers, whose participation and support made this study possible.
References
- Bello D, Streicher RP, Woskie SR. Evaluation of the NIOSH draft method 5525 for determination of the total reactive isocyanate group (TRIG) for aliphatic isocyanates in autobody repair shops. J Environ Monit. 2002;4:351–60. doi: 10.1039/b110613a. [DOI] [PubMed] [Google Scholar]
- Bello D, Herrick CA, Smith TJ, et al. Skin exposure to isocyanates: reasons for concern. Environ Health Perspect. 2007a;115:328–35. doi: 10.1289/ehp.9557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bello D, Sparer JA, Redlich CA, et al. Slow curing of aliphatic polyisocyanate paints in automotive refinishing: a potential source for skin exposure. J Occup Environ Hyg. 2007b;4:406–11. doi: 10.1080/15459620701341199. [DOI] [PubMed] [Google Scholar]
- Bello D, Redlich CA, Stowe MH, et al. Skin exposure to aliphatic polyisocyanates in the auto body repair and refinishing industry: II. A quantitative assessment. Ann Occup Hyg. 2008;52:117–24. doi: 10.1093/annhyg/mem066. [DOI] [PubMed] [Google Scholar]
- Fent KW, Jayaraj K, Gold A, et al. Tape-strip sampling for measuring dermal exposure to 1,6-hexamethylene diisocyanate. Scand J Work Environ Health. 2006;32:225–40. doi: 10.5271/sjweh.1003. [DOI] [PubMed] [Google Scholar]
- Liu Y, Sparer J, Woskie SR, et al. Qualitative assessment of isocyanate skin exposure in auto body shops: a pilot study. Am J Ind Med. 2000;37:265–74. doi: 10.1002/(sici)1097-0274(200003)37:3<265::aid-ajim4>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Liu Y, Stowe MH, Bello D, et al. Respiratory protection from isocyanate exposure in the autobody repair and refinishing industry. J Occup Environ Hyg. 2006;3:234–49. doi: 10.1080/15459620600628704. [DOI] [PubMed] [Google Scholar]
- Liu Y, Bello D, Sparer JA, et al. Skin exposure to aliphatic polyisocyanates in the auto body repair and refinishing industry: a qualitative assessment. Ann Occup Hyg. 2007;51:429–39. doi: 10.1093/annhyg/mem021. [DOI] [PubMed] [Google Scholar]
- OECD. Environmental health and safety publications series on testing and assessment no. 9: guidance document for the conduct of studies of occupational exposure to pesticides during agricultural application. OECD. Paris: 1997. [Google Scholar]
- Petsonk EL, Wang ML, Lewis DM, et al. Asthma-like symptoms in wood product plant workers exposed to methylene diphenyl diisocyanate. Chest. 2000;118:1183–93. doi: 10.1378/chest.118.4.1183. [DOI] [PubMed] [Google Scholar]
- Pronk A, Yu F, Vlaanderen J, et al. Dermal, inhalation, and internal exposure to 1,6-HDI and its oligomers in car body repair shop workers and industrial spray painters. Occup Environ Med. 2006;63:624–31. doi: 10.1136/oem.2005.023226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redlich CA, Herrick CA. Lung/skin connections in occupational lung diseases. Curr Opin Allergy Clin Immunol. 2008;8:115–9. doi: 10.1097/ACI.0b013e3282f85a31. [DOI] [PubMed] [Google Scholar]
- Redlich CA, Stowe MH, Wisnewski AV, et al. Subclinical immunologic and physiologic responses in hexamethylene diisocyanate-exposed auto body shop workers. Am J Ind Med. 2001;39:587–97. doi: 10.1002/ajim.1058. [DOI] [PubMed] [Google Scholar]
- Schneider T, Cherrie JW, Vermeulen R, et al. Dermal exposure assessment. Ann Occup Hyg. 2000;44:493–9. [PubMed] [Google Scholar]
- Sparer J, Stowe MH, Bello D, et al. Isocyanate exposures in autobody shop work: the SPRAY study. J Occup Environ Hyg. 2004;1:570–81. doi: 10.1080/15459620490485909. [DOI] [PubMed] [Google Scholar]
- van Wendel de Joode B, Vermeulen R, van Hemmen JJ, et al. Accuracy of a semiquantitative method for dermal exposure assessment (DREAM) Occup Environ Med. 2005;62:623–32. doi: 10.1136/oem.2004.018564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermeulen R, Stewart P, Kromhout H. Dermal exposure assessment in occupational epidemiologic research. Scand J Work Environ Health. 2002;28:371–85. doi: 10.5271/sjweh.689. [DOI] [PubMed] [Google Scholar]
- Warren ND, Marquart H, Christopher Y, et al. Task-based dermal exposure models for regulatory risk assessment. Ann Occup Hyg. 2006;50:491–503. doi: 10.1093/annhyg/mel014. [DOI] [PubMed] [Google Scholar]
- Wolf SE, Prnitt BA., Jr . Burn management. In: Irwin RS, Rippe JM, editors. Irwin & Rippe's intensive care medicine. 6th. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. Figure 129–1, pp. 1930. [Google Scholar]
- Woskie SR, Sparer J, Gore RJ, et al. Determinants of isocyanate exposures in auto body repair and refinishing shops. Ann Occup Hyg. 2004;48:393–403. doi: 10.1093/annhyg/meh021. [DOI] [PubMed] [Google Scholar]
- Woskie SR, Bello D, Gore RJ, et al. Comparison of task-based exposure metrics for an epidemiologic study of isocyanate inhalation exposures among autobody shop workers. J Occup Environ Hyg. 2008;5:588–98. doi: 10.1080/15459620802275429. [DOI] [PubMed] [Google Scholar]