Abstract
Many middle-aged and older people with severe mental illness are interested in working or volunteering. However, very few vocational rehabilitation programs target older clients with psychiatric illness. We examined employment outcomes among 50 middle-aged and older participants with schizophrenia or schizoaffective disorder in a 12-month randomized controlled trial comparing two work rehabilitation programs: Individual Placement and Support (IPS; a supported employment model) and conventional vocational rehabilitation (CVR). Compared with CVR, IPS resulted in statistically better work outcomes, including attainment of competitive employment, number of weeks worked, and wages earned. Cohen's d effect sizes for these variables were medium to large (.66-.81). Treatment group predicted future attainment of competitive work, but demographic and clinical variables (e.g., age, gender, ethnicity, education, illness duration, and medication dose) did not predict employment outcomes. Participants who obtained competitive employment reported improved quality of life over time compared to those who did not. These findings suggest that for middle-aged and older clients with schizophrenia, supported employment results in better work outcomes than does conventional vocational rehabilitation. Furthermore, age was not significantly associated with attainment of competitive work. Finally, the therapeutic value of work is reflected in improved quality of life.
Across the age spectrum, rates of paid employment among people with schizophrenia are less than 15 percent (Anthony and Blanch, 1987). With the graying of the population, the number of middle-aged and older people with these disorders is growing rapidly (Palmer et al., 2002), and like their younger counterparts, most of them are unemployed. Older people with severe mental illness are frequently assumed to be incapable of returning to work and are not actively recruited to participate in work rehabilitation programs. However, just as healthy older people are working well past traditional retirement age, many older people with schizophrenia want to work (Auslander and Jeste, 2002).
Middle-aged and older work rehabilitation clients may be different from younger clients in many ways. Older clients with schizophrenia may have less severe positive symptoms, lower rates of alcohol or substance abuse, and more lifetime work experience (e.g., Jeste et al., 2003). However, compared with younger workers, they may also face unique obstacles, including greater age-associated cognitive and sensory-motor deficits, increased medical comorbidity, slower processing speed, higher rates of side effects of medications such as tardive dyskinesia, longer absences from the workforce, and ageist beliefs among employers (e.g., Jeste et al., 2003; Kurtz, 2005).
Supported employment has emerged as an evidence-based practice in psychiatric rehabilitation, with a number of randomized controlled trials demonstrating its effectiveness over conventional vocational rehabilitation (CVR) (e.g., Bond, 2004; Cook et al., 2005). For clients with schizophrenia and other psychotic disorders, a meta-analysis showed that supported employment was superior to CVR in terms of rates of competitive work (51% vs. 18%, respectively), with an effect size of .79 (Twamley et al., 2003). Most supported employment programs follow the Individual Placement and Support (IPS) model, which provides manualized guidelines for delivering supported employment (Becker and Drake, 2003). IPS is based on a “place-then-train” philosophy, emphasizing rapid job searching, individualized job placement in competitive work, followed by on-the-job training (if needed), and ongoing support from a vocational specialist to help clients keep their jobs. Job placement is tailored to the client's preferences and interests, and services are provided in the client's community as much as possible. IPS links vocational services and mental health care in a treatment team model in order to provide integrated treatment. CVR is provided by most states as part of the federal-state vocational rehabilitation system (Lehman and Steinwachs, 1998; Noble et al., 1997). In contrast to IPS/supported employment principles, most CVR programs use a “train-then-place” approach, emphasizing prevocational training classes and volunteer, transitional, or trial employment before seeking competitive work (i.e., employment in the community at prevailing wages). Clients in these programs tend to have higher dropout rates, possibly because of the delay between initial training and ultimate job placement (Bond et al., 1995). Although the gradual, stepwise approach to seeking employment may be well-intentioned, the prevocational training provided may not correspond to the jobs available to the clients when they seek paid employment. Most CVR programs are time-limited (e.g., services are discontinued after a client has kept a job for 90 days).
Previous randomized controlled trials of IPS or supported employment have focused on young adults and adults. For example, the mean age of the clients in the IPS studies included in a previous meta-analysis was 39 years (Twamley et al., 2003). Here, we report on the first randomized controlled trial of IPS for middle-aged and older people with schizophrenia or schizoaffective disorder. The purpose of this study was to examine work rehabilitation outcomes among clients aged 45 and older, with schizophrenia or schizoaffective disorder, receiving IPS or CVR services. We hypothesized that: (1) Compared with CVR, IPS would result in better outcomes for this older population in terms of competitive work attainment, time to obtain first job, job tenure (total number of weeks employed), and wages earned; (2) Age and other demographic and clinical variables would not be significant predictors of work outcomes; and (3) Participants who obtained competitive work would experience improved quality of life compared to those who did not.
Method
Participants
All participants were 45 years of age or older, had a DSM-IV (American Psychiatric Association, 1994) diagnosis of schizophrenia or schizoaffective disorder, and were receiving their psychiatric care at an outpatient clinic in San Diego. Diagnoses were made by the treating psychiatrists and were confirmed by a diagnostic chart review by trained research staff. Participants were required to be unemployed but wanting to work at the time of study entry. All participants had worked in the past, and 84% had a history of consecutive employment for at least 12 months. Exclusion criteria were alcohol or substance dependence within the past month and presence of dementia or other major neurological disorders. The study was approved by University of California, San Diego Human Research Protections Program, and written informed consent to participate in the research study was obtained from all participants.
The subjects included 30 men and 20 women who were self-referred or referred by their clinicians for vocational services; 20 subjects were diagnosed with schizophrenia, and 30 were diagnosed with schizoaffective disorder. Twenty-two participants were 45-49 years old, 22 were 50-54 years old, 4 were 50-59 years old, and two were 60. Most (32) of the subjects were Caucasian; 10 were African-American, 5 were Latino/Hispanic, 1 was Native American, and 2 were of mixed ethnicity.
Dropout rates were 21% in the IPS group and 23% in the DVR group, with not wanting to work being the most common reason for dropping out of the study. Study dropouts did not differ from study completers in terms of age, gender, diagnosis, illness duration, antipsychotic medication dose, or treatment group (all Χ2 < 1.2, all t < .73, all p > .265). Dropouts were significantly more likely than completers to be members of ethnic minority groups (65% vs. 28%; Χ2 = 4.7, df = 1, p = .031), to have less education (10.7 vs. 12.8 years; t = 2.59, df = 48, p = .013), and to have a less recent history of working (12 vs. 6 years since last job; t = 2.55, df = 47, p = .014).
Procedure
Following enrollment into the study, participants were randomly assigned to IPS or CVR. Assessments were administered by trained raters who were blind to group assignment and had achieved high levels of reliability (intraclass correlation coefficient [ICC] >0.80). Baseline assessments included the Abnormal Involuntary Movement Scale (AIMS; National Institute of Mental Health, 1975) to assess severity of tardive dyskinesia, the Positive and Negative Syndrome Scale (PANSS; Kay et al., 1987), and the Hamilton Rating Scale for Depression (HAM-D; Hamilton, 1967). The Quality of Life Interview (Lehman, 1983) was administered at baseline, 6-month follow-up, and 12-month follow-up. Employment data were tracked via weekly logs of hours worked and wages earned and confirmed via examination of pay stubs. Antipsychotic medication dosages were converted into chlorpromazine equivalents (CPZE) according to standard formulae (Jeste & Wyatt, 1982; Woods, 2003), except for participants taking clozapine or long-acting injectable medications (n = 2), for which conversion formulae do not exist.
Interventions
CVR
In San Diego, all vocational rehabilitation services for clients in the public mental health system are contracted to an organization called Employment Services. Individuals first become clients of the Department of Rehabilitation (DOR), which entails attending an orientation session and an intake appointment with a DOR counselor. The DOR then has 60 days to determine eligibility for services, after which the clients are referred to Employment Services and assigned a vocational counselor (a bachelor-level or masters-level provider with a typical caseload of 35 clients). Job development and job coaching are provided by additional staff members. Clients receive job readiness coaching and attend prevocational classes before their job search begins. The program consists of four different stages: (1) Vocational Evaluation, a three-to-five week process that includes working with the vocational counselor in a classroom setting to determine the individual's interests, goals, qualifications, supports, and barriers to employment; assessments include aptitude testing and skills surveys; (2) Employment Preparation, an additional three to five weeks in the classroom setting, focusing on work readiness (e.g., preparing resumes, completing applications, practicing interview skills, and benefits counseling to discuss how working will affect the client's entitlements); (3) Job Development, which includes working with a job developer who assists with the interview process, providing transportation to and from interviews; and (4) Job Retention, which includes support from a job coach, if needed, for up to 90 days.
To enhance client participation and prevent attrition in the CVR condition of the study, subjects were provided assistance with appointment-setting, telephone call reminders, and (if needed) transportation for their first three appointments with the Employment Services counselor. We provided this additional assistance to maximize the opportunity for clients to get “hooked in” to the CVR services and thus, to provide a more fair comparison with the IPS condition in terms of access to services.
IPS
The IPS intervention was delivered according to the manual developed by Becker and Drake (2003). All services are provided by the vocational specialist, who is typically a bachelor-level provider with a caseload of 20-25 clients. Clients participate in the following phases of the program, at a pace they and the vocational specialist determine is appropriate: (1) Initial Assessment of the client's job skills, past employment experiences, barriers to employment, and current employment goals and preferences, along with benefits counseling; (2) Job Searching, a collaborative process between the client and the vocational specialist to create resumes, complete applications, and prepare for interviews; the vocational specialist may provide transportation to interviews and accompany the client on interviews, depending on the client's disclosure preferences, and also engages in job development to “carve out” potential jobs in the community; and (3) Time-Unlimited Follow-Along Support provided at the worksite, in the office, or in the client's neighborhood to help clients cope with stressors and keep their jobs. Intervention fidelity was rated by the third author according to the Supported Employment Fidelity Scale (Bond et al., 1997). IPS fidelity was rated as “fair” (63/75 points), losing six points due to it being a research-based program for clients with schizophrenia and having only one vocational specialist.
Statistical Analyses
Based on our experience and that reported in the literature, we assumed that clients who dropped out of the study did not work and imputed zeros for their weekly employment data, the same approach used by Mueser et al. (2004). All data were checked to ensure that normality of distribution and homogeneity of variance assumptions were met. We used t-tests, chi-square, logistic regression, and repeated measures ANOVA techniques to analyze the data. Alpha for significance was set at p < .05, and all tests were two-tailed. We also calculated Cohen's d effect sizes to provide estimates of the magnitude of effects (Cohen, 1988).
Results
Subject Characteristics
Table 1 presents the baseline demographic, clinical, and medication data for IPS and CVR groups. The two intervention groups did not differ significantly with respect to any of the baseline demographic, clinical, medication, or work history variables.
Table 1.
Demographic, Clinical, and Medication Variables in the IPS and CVR Groups
| IPS (n=28) |
CVR (n=22) |
t or χ2 (df) | p | |
|---|---|---|---|---|
| Age in Years (Mean, [SD]) | 50.0 (3.2) | 51.1 (5.0) | 0.95 (34.1) | .323 |
| Education in Years (Mean, [SD]) | 12.4 (2.4) | 12.4 (2.6) | 0.00 (48) | .993 |
| Gender, % male | 71 | 46 | 3.46 (1) | .063 |
| Ethnicity, % minority | 36 | 36 | 0.00 (1) | .962 |
| Diagnosis, % schizophrenia (vs. schizoaffective) |
50 | 27 | 2.65 (1) | .103 |
| Duration of illness | 25.0 (10.3) | 22.3 (11.3) | 0.74 (48) | .463 |
| Antipsychotic medication dose in CPZE | 401.7 (449.6) | 252.0 (277.9) | 1.36 (46) | .182 |
| PANSS positive symptoms | 15.9 (4.3) | 14.5 (6.5) | 0.86 (41) | .394 |
| PANSS negative symptoms | 15.3 (5.3) | 16.6 (5.1) | 0.81 (41) | .424 |
| HAM-D depressive symptoms | 9.8 (6.7) | 11.8 (8.6) | 0.82 (40) | .416 |
| AIMS tardive dyskinesia severity | 2.1 (2.8) | 2.4 (3.7) | 0.25 (39) | .805 |
| Quality of Life Interview Global Satisfaction Index |
4.3 (1.6) | 4.1 (1.6) | 0.43 (40) | .673 |
| Years since last job | 6.5 (7.4) | 7.8 (6.2) | 0.68 (47) | .497 |
| Monthly disability entitlement income, dollars |
807.4 (272.7) | 772.2 (143.4) | 0.54 (47) | .594 |
Hypothesis 1: Treatment Group Comparisons
Among IPS participants, 57% obtained competitive work, compared with 27% of CVR participants (χ2 = 4.5, df = 1, p = .035). The difference in rates of competitive work equates to a Cohen's d effect size of .63, in the range of medium effects according to Cohen's effect size conventions (Cohen, 1988). IPS participants worked an average of 11 weeks during the year, whereas CVR participants worked an average of 3 weeks (t = 2.6, df = 42.9, p = .013; Cohen's d=.71). IPS clients earned more money from competitive work than did CVR participants ($1,964 vs. $467; t = 2.5, df =33.4, p = .020; Cohen's d=.66). Of those who obtained competitive work, IPS clients obtained their jobs somewhat more quickly than did CVR clients (93 days vs. 171 days), but the difference was not statistically significant (t = 1.7, df = 20, p = .096; Cohen's d=.81).
In an exploratory analysis, we examined the speed of service delivery in the two intervention conditions. IPS participants waited an average of 6 days between enrolling in the study and having their first appointment with the vocational specialist, whereas CVR participants waited an average of 21 days between enrollment and their first appointment with the DOR orientation staff (t = 4.26, df = 44, p < .001). The 9 participants who were referred to Employment Services waited an average of 123 days before meeting their vocational counselor.
Even though all participants had initially stated a goal of paid work, one-third of the CVR clients were placed in or elected to pursue education or training programs rather than given assistance finding employment, and another third did not pursue work or training at all, even though they remained in the study. Of the 6 CVR participants who worked competitively, 5 found their jobs on their own, without the assistance of a vocational counselor.
Hypothesis 2: Demographic, Clinical, Medication, and Treatment Predictors of Employment
To test hypothesis 2, we compared clients who obtained competitive work and those who did not (see Table 2). Using t-tests and chi square analyses, these two groups were compared on demographic (age, education, gender, ethnic minority status), clinical (diagnosis, duration of illness, positive and negative symptom severity, depression symptom severity, and severity of tardive dyskinesia), medication dose, work recency, disability entitlement income at baseline, and intervention group variables. Compared with participants who did not work competitively, those who obtained competitive work were more likely to be receiving IPS than CVR services and had worked more recently in the past (see Table 2), but did not differ on any other variables.
Table 2.
Demographic, Clinical, Medication, and Treatment Differences between Competitive Workers and Non-Competitive Workers
| Competitive workers (n=22) |
Non- competitive workers (n=28) |
t or χ2 (df) | p | |
|---|---|---|---|---|
| Age in Years (Mean, [SD]) | 50.4 (4.5) | 50.6 (3.9) | 0.18 (48) | .862 |
| Education in Years (Mean, [SD]) | 12.8 (2.6) | 12.0 (2.5) | 1.03 (48) | .307 |
| Gender, % male | 64 | 57 | .22 (1) | .642 |
| Ethnicity, % minority | 23 | 46 | 3.00 (1) | .083 |
| Diagnosis, % schizophrenia (vs. schizoaffective) | 46 | 36 | 0.49 (1) | .485 |
| Duration of illness | 24.3 (10.5) | 22.9 (11.0) | 0.45 (48) | .653 |
| Antipsychotic medication dose in CPZE | 357.1 (494.0) | 314.4 (280.1) | 0.38 (46) | .707 |
| PANSS positive symptoms | 14.9 (4.7) | 15.8 (5.8) | 0.53 (41) | .600 |
| PANSS negative symptoms | 15.6 (4.6) | 16.1 (5.9) | 0.31 (41) | .756 |
| HAM-D depressive symptoms | 9.2 (5.8) | 12.0 (8.8) | 1.22 40) | .230 |
| AIMS tardive dyskinesia severity | 2.0 (3.0) | 2.5 (3.4) | 0.55 (39) | .585 |
| Years since last job | 4.2 (4.9) | 9.4 (7.4) | 2.81 (47) | .007 |
| Monthly disability entitlement income, dollars | 751.9 (205.9) | 825.3 (238.5) | 1.14 (47) | .260 |
| Intervention group, % receiving IPS | 73 | 43 | 4.46 (1) | .035 |
A logistic regression predicting competitive work attainment among study completers was computed with the independent variables of age, education, duration of illness, antipsychotic medication dose, work recency, and intervention group. All of the independent variables were included in the same block, with a probability of .05 to enter and .10 to remove variables. In the presence of multiple predictor variables, only intervention group predicted later competitive work attainment, with IPS completers being about 6 times more likely than CVR completers to work competitively (odds ratio = 5.8; see Table 3). The model explained 30% of the variance in work status (Nagelkerke R2=.30) and correctly classified 70% of the sample.
Table 3.
Multivariate Logistic Regression Predicting Competitive Work Status
| Wald | df | p | |
|---|---|---|---|
| Age | .645 | 1 | .422 |
| Education | .001 | 1 | .974 |
| Duration of illness | .178 | 1 | .673 |
| Antipsychotic medication dose in CPZE | .019 | 1 | .891 |
| Years since last job | 2.425 | 1 | .119 |
| Intervention group (IPS, CVR) | 4.915 | 1 | .027 |
Note. Nagelkerke R2=.30
Hypothesis 3: The Effect of Work on Quality of Life
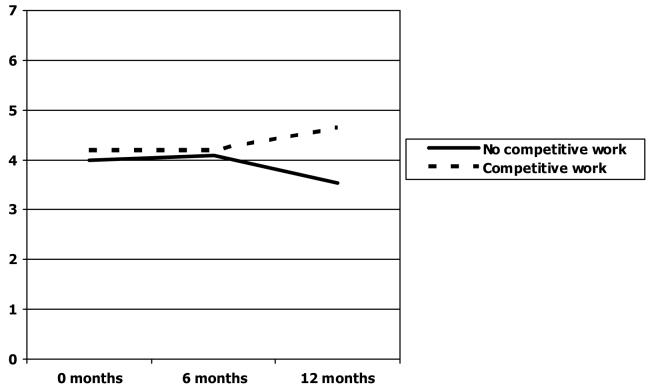
Finally, to test hypothesis 3, we conducted a repeated measures ANOVA to assess the effect of competitive work status on self-reported quality of life among the participants with quality of life data at all three time points of the study (n=29). The Global Satisfaction index (the mean of the two Global Satisfaction items on the QOLI) at baseline, 6-month follow up, and 12-month follow up was used as the within-subjects variable, and competitive work status was the between-subjects variable. As shown in Figure 1, for participants who worked competitively during the study, global satisfaction with life increased over the course of the year and was highest at 12-month follow up (a mean of 4.65 on a 7-point scale), whereas those who did not work competitively reported their lowest quality of life at the 12-month follow-up (a mean of 3.54). The time by work status interaction effect was significant (F = 3.92, df = 2, p = .026).
Figure 1.
Competitive Work and Quality of Life over Time
Discussion
Our results indicate that middle-aged and older people with schizophrenia or schizoaffective disorder benefited from work rehabilitation and obtained competitive employment, regardless of most demographic and clinical variables. IPS participants were more likely to work than were CVR participants, suggesting that as with their younger counterparts, the supported employment model is more effective than is traditional vocational rehabilitation in helping middle-aged and older clients with schizophrenia obtain work. It may be that the rapid and individualized nature of the IPS “place-then-train” approach suits these clients better than does the “train-then-place” approach.
Despite our efforts to ensure improved access to vocational services in the CVR condition, many participants were not given assistance finding work. All participants had a stated goal of paid work at the time of study enrollment, yet many were steered toward education or training by DOR staff, which probably deterred them from looking for work. Speed of access to services also differed between IPS and CVR. Many IPS clients met with their vocational specialist and began looking for work within a week of enrolling in the study, whereas CVR clients were unable to access services quickly and may have lost their motivation to work while waiting for services to begin.
Treatment group was a significant predictor of employment outcomes, but demographic and clinical variables were not associated with success in obtaining competitive employment. These results are consistent with other research suggesting that most clients with severe mental illness who want to work can do so, given the appropriate support (Bond, 2004; Bond et al., 2001; Twamley et al., 2003). The number of years since last employment in the participants who obtained competitive work ranged from 0-16, suggesting that even those clients who have not worked for over a decade can return to work. Previous studies including younger patients have found that age does not predict attainment of competitive work (see Bond et al., 2001, for review), but this study extends those results into an older age group. Clients who obtained competitive work reported improved quality of life throughout the course of the study, which may reflect a combination of factors, including increased income, activity, structure, socialization, and self-efficacy.
Several limitations of this study should be considered, including the relatively small sample sizes within the IPS and CVR groups. These findings should be considered preliminary until replicated with a larger sample. Those who participate in work rehabilitation programs represent a self-selected group; these results may not generalize to clients who are less motivated to work or who have no desire to return to work. The oldest subjects in our study were 60 years of age, and more research is needed to address the feasibility and efficacy of vocational rehabilitation for seniors with mental illness. The present study only examined competitive work attainment, job tenure, and wages earned as employment outcomes; future studies will address other types of work situations as well as volunteer work. Further research is also needed to determine other predictors of future employment, such as work-related skills and cognitive functioning.
Finally, although IPS services resulted in higher rates of competitive work, not all clients receiving IPS attained competitive employment, suggesting that adaptations to IPS may be needed for certain clients. Middle-aged and older clients with psychiatric illness face multiple obstacles to employment (e.g., stigma in the workplace, fear of losing benefits, negative symptoms, lack of confidence, limited employment history, and lack of transportation), and more knowledge is needed regarding how to best help them overcome these barriers.
Acknowledgments
This research was supported by a grant from the National Institute of Mental Health (MH066011).
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th Edition American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Anthony WA, Blanch A. Supported employment for persons who are psychiatrically disabled: An historical and conceptual perspective. Psychosocial Rehabilitation Journal. 1987;11:5–23. [Google Scholar]
- Auslander LA, Jeste DV. Perception of problems and needs for service among older outpatients with schizophrenia and related psychotic disorders. Community Mental Health Journal. 2002;38:391–402. doi: 10.1023/a:1019808412017. [DOI] [PubMed] [Google Scholar]
- Becker DR, Drake RE. A Working Life: The Individual Placement Support (IPS) Program. New Hampshire-Dartmouth Psychiatric Research Center; Concord, NH: 1993. [Google Scholar]
- Bond GR. Supported employment: evidence for an evidence-based practice. Psychiatric Rehabilitation Journal. 2004;27:345–359. doi: 10.2975/27.2004.345.359. [DOI] [PubMed] [Google Scholar]
- Bond GR, Becker DR, Drake RE, Rapp CA, Meisler N, Lehman AF, Bell MD, Blyler CR. Implementing supported employment as an evidence-based practice. Psychiatric Services. 2001;52:313–322. doi: 10.1176/appi.ps.52.3.313. [DOI] [PubMed] [Google Scholar]
- Bond GR, Becker DR, Drake RE, Vogler KM. A fidelity scale for the Individual Placement and Support model of supported employment. Rehabilitation Counseling Bulletin. 1997;40:265–84. [Google Scholar]
- Bond GR, Dietzen LL, McGrew JH, Miller JD. Accelerating entry in to supported employment for persons with severe psychiatric disabilities. Rehabilitation Psychology. 1995;400:94. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- Cook JA, Leff HS, Blyler CR, Gold PB, Goldberg RW, Mueser KT, Toprac MG, McFarlane WR, Shafer MS, Blankertz LE, Dudek K, Razzano LA, Grey DD, Burke-Miller J. Results of a multisite randomized trial of supported employment interventions for individuals with severe mental illness. Archives of General Psychiatry. 2005;62:505–512. doi: 10.1001/archpsyc.62.5.505. [DOI] [PubMed] [Google Scholar]
- Hamilton M. Development of a rating scale for primary depressive illness. British Journal of Social and Clinical Psychology. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- Jeste DV, Twamley EW, Eyler Zorrilla LT, Golshan S, Patterson TL, Palmer BW. Aging and outcome in schizophrenia. Acta Psychiatrica Scandinavica. 2003;107:336–343. doi: 10.1034/j.1600-0447.2003.01434.x. [DOI] [PubMed] [Google Scholar]
- Jeste DV, Wyatt RJ. Understanding and treating tardive dyskinesia. Guilford Press, Inc; New York, NY: 1982. [Google Scholar]
- Kay SR, Opler LA, Fiszbein A. Positive and Negative Syndrome Scale (PANSS) Rating Manual. Social and Behavioral Sciences Documents; San Rafael, CA: 1987. [Google Scholar]
- Kurtz MM. Neurocognitive impairment across the lifespan in schizophrenia: an update. Schizophrenia Research. 2005;74:15–26. doi: 10.1016/j.schres.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Lehman AF. The effects of psychiatric symptoms on quality of life assessments among the chronic mentally ill. Evaluation and Program Planning. 1983;6:143–151. doi: 10.1016/0149-7189(83)90028-9. [DOI] [PubMed] [Google Scholar]
- Lehman AF, Steinwachs DM, Dixon L, Postrado L, Scott J, Fahey M, Fischer P, Hoch J, Kasper J, Lyles A, Shore A, Skinner A. Patterns of usual care for schizophrenia: Initial results from the Schizophrenia Patients Outcomes Research Team (PORT) client survey. Schizophrenia Bulletin. 1998;24:11–20. doi: 10.1093/oxfordjournals.schbul.a033303. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Clark RE, Haines M, Drake RE, McHugo GJ, Bond GR, Essock SM, Becker DR, Wolfe R, Swain K. The Hartford study of supported employment for persons with severe mental illness. Journal of Consulting and Clinical Psychology. 2004;72:479–490. doi: 10.1037/0022-006X.72.3.479. [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health Abnormal Involuntary Movement Scale (AIMS) Early Clinical Drug Evaluation Unit Intercom. 1975;4:3–6. [Google Scholar]
- Noble JH, Honberg RS, Hall LL, Flynn LM. A legacy of failure: The inability of the federal-state vocational rehabilitation system to serve people with severe mental illness. National Alliance for the Mentally Ill; Arlington, VA: 1997. [Google Scholar]
- Palmer BW, Heaton RK, Gladsjo JA, Evan JD, Patterson TL, Golshan S, Jeste DV. Heterogeneity in functional status among older outpatients with schizophrenia: employment history, living situation, and driving. Schizophrenia Research. 2002;55:205–215. doi: 10.1016/s0920-9964(01)00218-3. [DOI] [PubMed] [Google Scholar]
- Twamley EW, Jeste DV, Lehman AF. Vocational rehabilitation in schizophrenia: A literature review and meta-analysis of randomized controlled trials. The Journal of Nervous and Mental Disease. 2003;191:515–523. doi: 10.1097/01.nmd.0000082213.42509.69. [DOI] [PubMed] [Google Scholar]
- Woods SW. Chlorpromazine equivalent doses for the newer atypical antipsychotics. Journal of Clinical Psychiatry. 2003;64:663–667. doi: 10.4088/jcp.v64n0607. [DOI] [PubMed] [Google Scholar]