Abstract
Global advances in patient safety have been hampered by the lack of a uniform classification of patient safety concepts. This is a significant barrier to developing strategies to reduce risk, performing evidence-based research and evaluating existing healthcare policies relevant to patient safety. Since 2005, the World Health Organization's World Alliance for Patient Safety has undertaken the Project to Develop an International Classification for Patient Safety (ICPS) to devise a classification which transforms patient safety information collected from disparate systems into a common format to facilitate aggregation, analysis and learning across disciplines, borders and time. A drafting group, comprised of experts from the fields of patient safety, classification theory, health informatics, consumer/patient advocacy, law and medicine, identified and defined key patient safety concepts and developed an internationally agreed conceptual framework for the ICPS based upon existing patient safety classifications. The conceptual framework was iteratively improved through technical expert meetings and a two-stage web-based modified Delphi survey of over 250 international experts. This work culminated in a conceptual framework consisting of ten high level classes: incident type, patient outcomes, patient characteristics, incident characteristics, contributing factors/hazards, organizational outcomes, detection, mitigating factors, ameliorating actions and actions taken to reduce risk. While the framework for the ICPS is in place, several challenges remain. Concepts need to be defined, guidance for using the classification needs to be provided, and further real-world testing needs to occur to progressively refine the ICPS to ensure it is fit for purpose.
Keywords: classification, patient safety, incident, conceptual framework
Since the early 1700s, scientists have attempted to classify disease. Several disease-related classifications were in use until 1837 when William Farr, the first medical statistician in the General Register Office of England and Wales, outlined governing principles for a ‘statistical classification of disease and urged the adoption of a uniform classification’ [1]. He believed that:
[a]dvantages of a uniform statistical nomenclature, however imperfect, are so obvious, that it is surprising no attention has been paid to its enforcement. Each disease has, in many instances, been denoted by three or four terms, and each term has been applied to as many different diseases; vague, inconvenient names have been employed, or complications have been registered instead of primary disease. The nomenclature is of as much importance in this department of inquiry as weights and measures in the physical sciences, and should be settled without delay.
In 1853, members of the International Statistical Congress strongly agreed with the utility of an international classification of causes of death and requested that William Farr and Marc d'Espine ‘prepare an internationally applicable, uniform classification of causes of death’ [1]. This was the beginning of what we now know as the International Classification of Diseases (ICD), which is widely in use throughout the world.
Over 150 years later there are many parallels with the field of patient safety. Several patient safety-related classifications have been developed in different parts of the world. They serve a variety of purposes, were built using different models and contain different concepts, terms and definitions. The ad hoc approaches used to develop many of these classifications, the dissimilar methods used to categorize data and the assortment of definitions for a single concept make data aggregation from disparate sources (medical records, claims data, patient-reported data and coroners' reports) difficult, if not impossible. As a result, the information yielded is of limited value outside the specified purpose for which the classification was initially developed. The absence of an internationally agreed definition for patient safety concepts and a uniform approach to classifying these concepts prevents comparison of information, learning and system improvement.
The project to develop the ICPS
The Fifty-fifth World Health Assembly passed resolution WHA55.18 in May 2002 calling upon Member States to ‘pay the closest possible attention to the problem of patient safety and to establish and strengthen science-based systems necessary for improving patients’ safety and quality of care' [2]. The Assembly urged the WHO to develop global norms and standards and to support efforts by Member States to develop patient safety policies and practices. In October 2004, the WHO launched the World Alliance for Patient Safety. The project to develop an ICPS was identified as one of the key initiatives in the Alliance's 2005 Forward Programme and continues to be of high priority.
A Drafting Group, comprised of experts from the fields of patient safety, classification theory, health informatics, consumer/patient advocacy, law and medicine, was assembled to initiate and take forward a work program. The Drafting Group set itself the task of defining, harmonizing and grouping patient safety concepts into an internationally agreed classification in a way that is conducive to learning and improving patient safety across systems. From the start, the Drafting Group realized that the ‘problems do not lie with the words we use but rather with the underlying concepts’ [3]. Thus, it is the conceptual definitions that are important, as well as the terms or labels assigned to the concepts, for without universally accepted conceptual definitions, understanding will continue to be impeded.
Before embarking on the process to develop the ICPS, the Drafting Group, like William Farr, outlined a set of principles. These are: (i) the purpose and potential users and uses for the classification must be clearly articulated; (ii) the classification should be based on concepts as opposed to terms or labels; (iii) the language used for the definitions of the concepts should be culturally appropriate; (iv) the concepts should be organized into meaningful and useful categories; (v) the categories should be applicable to the full spectrum of healthcare settings in developing, transitional and developed countries; (vi) the classification should be complementary to the WHO Family of International Classifications; (vii) the existing patient safety classifications should be used as the basis for developing the international classification's conceptual framework and (viii) the conceptual framework should be a genuine convergence of international perceptions of the main issues related to patient safety [4–9]. The Drafting Group believed that adherence to these principles would allow for maximum comparability of patient safety information across disciplines, organizations, borders and time [10].
The ICPS is intended to define, harmonize and group a standardized set of patient safety concepts, with agreed definitions and labeled with preferred terms, into an internationally acceptable classification in a way that is conducive to learning and improving patient safety across time and borders. Because it is intended that the ICPS be interoperable with the existing international classifications, ministries of health, patient safety organizations, and managers of patient safety reporting systems can implement it to facilitate the measurement and interpretation of information to improve patient safety.
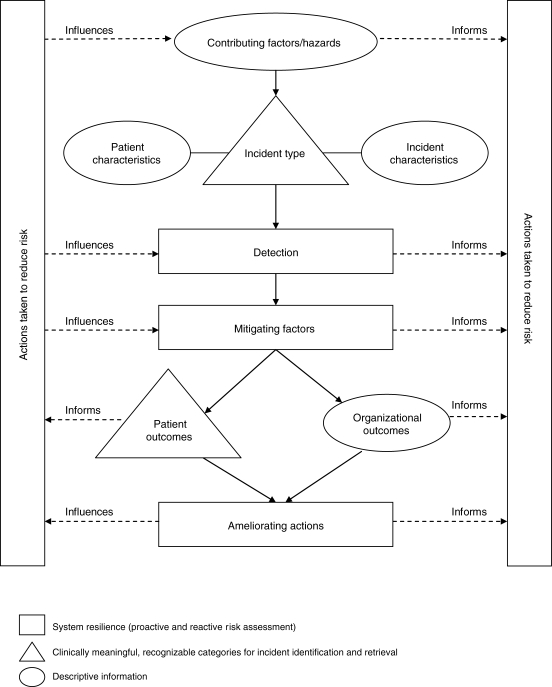
Using these principles as guidance, the Drafting Group developed an initial version of the conceptual framework, and identified and defined relevant key concepts with agreed preferred terms [11]. The conceptual framework and key concepts were then iteratively improved through a two-stage web-based modified Delphi survey and in-person meetings with international stakeholders and safety experts [12–14]. The in-person meetings served two purposes: the first, to theoretically test the validity of the conceptual framework with technical experts from a variety of safety-related fields; and second, to determine the international cultural and linguistic appropriateness of the conceptual framework and key concepts. This process culminated in the conceptual framework shown in Fig. 1 and discussed in the next section. The words or phrases in italics indicate an ICPS key concept.
Figure 1.
Conceptual framework for the ICPS.
It is important to distinguish a patient safety classification from a reporting system. A reporting system provides an interface to enable users to collect, store and retrieve data in a reliable and organized fashion. A classification comprises a set of concepts linked by semantic relationships and forms the structural underpinning of any type of reporting system. It also provides information for a variety of other purposes including national statistics, descriptive studies of safety and evaluative research.
The conceptual framework for the ICPS
The conceptual framework for the ICPS provides a reasonable understanding of the world of patient safety and contains patient safety concepts to which the existing regional and national classifications can relate. It is comprised of 10 high-level classes and ∼600 concepts that group incidents into clinically meaningful categories, provide descriptive information, represent system resilience, and inform learning and analytical processes.
A patient safety incident is an event or circumstance that could have resulted, or did result, in unnecessary harm to a patient. A patient safety incident can be a reportable circumstance, a near miss, a no harm incident or a harmful incident (adverse event). The class, incident type, is a descriptive term for a category made up of incidents of a common nature grouped because of shared, agreed features, such as ‘clinical process/procedure’ or ‘medication/IV fluid’ incident. Although each concept is clearly defined and distinct from other concepts, a patient safety incident can be classified as more than one incident type. A patient outcome is the impact upon a patient, which is wholly or partially attributable to an incident. Patient outcomes can be classified according to the type of harm, the degree of harm and any social and/or economic impact. Together, the classes incident type and patient outcomes are intended to group patient safety incidents into clinically meaningful categories.
Pertinent descriptive information that provides context for the incident is captured by four classes: patient characteristics, incident characteristics, contributing factors/hazards, and organizational outcomes. Patient characteristics categorize patient demographics, the original reason for seeking care and the primary diagnosis. Incident characteristics classify the information about the circumstances surrounding the incident such as where and when, in the patient's journey through the healthcare system, the incident occurred, who was involved, and who reported. Contributing Factors/Hazards are the circumstances, actions or influences which are thought to have played a part in the origin or development of an incident or to increase the risk of an incident. Examples are human factors such as behavior, performance or communication; system factors such as work environment; and external factors beyond the control of the organization, such as the natural environment or legislative policy. More than one contributing factor and/or hazard is typically involved in a single patient safety incident. Organizational outcomes refer to the impact upon an organization which is wholly or partially attributable to an incident such as an increased use of resources to care for the patient, media attention or legal ramifications.
A complex relationship exists between incident type and contributing factors. Depending on the context, circumstances and outcomes, an incident can be a contributing factor to another incident and/or some contributing factors can be a reportable circumstance in their own right.
The classes detection, mitigating factors, ameliorating actions and actions taken to reduce risk capture information relevant to prevention, error recovery and system resilience. The concept of error recovery, derived from industrial science and error theory, is particularly important if learning from patient safety incidents is to occur. The concept of resilience in the context of the ICPS is defined as ‘the degree to which a system continuously prevents, detects, mitigates or ameliorates hazards or incidents’ so that an organization can ‘bounce back’ to its original ability to provide core functions.
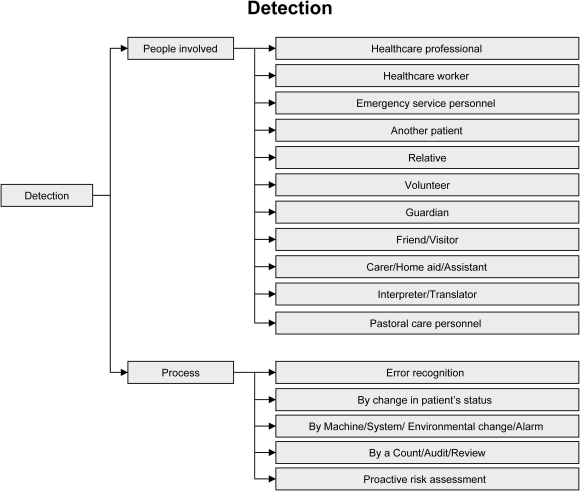
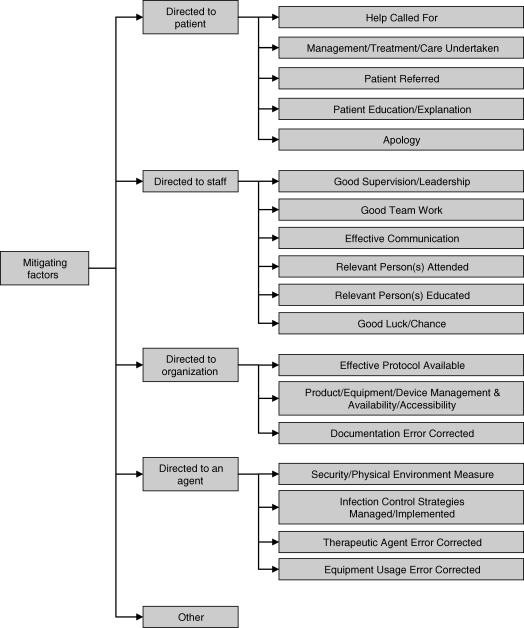
Detection is defined as an action or circumstance that results in the discovery of an incident. For example, an incident could be detected by a change in the patient's status, or via a monitor, alarm, audit, review or risk assessment (see Fig. 2). Detection mechanisms may be built into the system as official barriers or informally developed. Mitigating factors are actions or circumstances that prevent or moderate the progression of an incident toward harming the patient. Mitigating factors are designed to minimize the harm to the patient after the error has occurred and triggered damage control mechanisms (see Fig. 3). Together, detection plus mitigation can impede the progression of an incident from reaching and/or harming a patient. If the incident does result in harm, ameliorating actions can be introduced. Ameliorating actions are those actions taken or circumstances altered to make better or compensate any harm after an incident. Ameliorating actions apply to the patient (clinical management of an injury, apologizing) and to the organization (staff debriefing, culture change and claims management). Actions taken to reduce risk concentrate on steps taken to prevent the reoccurrence of the same or similar patient safety incident and on improving system resilience. Actions taken to reduce risk are those actions taken to reduce, manage or control any future harm, or probability of harm, associated with an incident. These actions may be directed toward the patient (provision of adequate care, decision support), toward staff (training, availability of policies/protocols), toward the organization (improved leadership/guidance, proactive risk assessment), and toward therapeutic agents and equipment (regular audits, forcing functions). Detection, mitigating factors and ameliorating actions both influence and inform the actions taken to reduce risk.
Figure 2.
Detection.
Figure 3.
Mitigating factors.
The conceptual framework for the ICPS is a continuous learning and improvement cycle emphasizing prevention, detection and reduction of risk. Contributing factors relate to the precursors to an incident. By addressing these, the risk to the patient can be reduced or eliminated through system redesign or policy implementation. In epidemiological terms, contributing factors equate to primary prevention. Detection and mitigating factors together represent error recovery and equate to secondary prevention. Ameliorating actions are those used in the rescue phase of error recovery, i.e. tertiary prevention. Actions taken to reduce risk represent the learning necessary to result in system improvement.
The future
The use of internationally standardized concepts with agreed definitions and preferred terms allows for comparison and thus greater analysis and interpretation of patient safety data and information. Organizing these concepts into a uniform classification facilitates description, measurement, and monitoring to improve patient care, conduct epidemiological research, and to inform health policy planning. The ICPS, though, is not yet fully developed. The conceptual framework provides the foundation, but several challenges remain. Definitions for each concept in the ICPS are required; currently, only the key concepts have fully been defined. Further work on definitions is a prerequisite for use of the classification and translation into other languages. Because the ICPS is based on classifications from developed countries, but is intended for use in developing and transitional countries as well, a guide for using it is necessary to ensure it is appropriate for use in a range of locations. Finally, the detail with which incidents may be classified so that the information captured and retrieved is useful to those who wish to devise correctives strategies must be progressively increased.
Whether the ICPS will be adopted on a broad scale is yet uncertain. Several reporting and data collection systems are currently in use in various healthcare settings, and changes to their underlying structures may be costly. The benefits must clearly outweigh the costs for users to adopt the new approach and revamp the existing systems. The acceptance of the ICPS will require a combination of solid scientific evidence of the relevance and utility of the classification, training and education, and political influence.
Global advances in patient safety have been hampered by the lack of a uniform classification of patient safety concepts. Developing strategies to reduce risk, performing evidence-based research and evaluating the existing healthcare policies related to patient safety require an internationally acceptable approach to the classification of patient safety information. When fully developed, the ICPS will provide a basis for sharing the knowledge necessary for improving care and reducing the risk of healthcare-associated harm to patients.
Funding
The Project to Develop the ICPS was funded by the World Health Organization World Alliance for Patient Safety, Geneva, Switzerland. The conceptual framework for the ICPS is the intellectual property of the World Health Organization.
Acknowledgments
The Drafting Group thanks all members of the World Alliance for Patient Safety for their continued input and support.
Conflict of interest: Some of the members of the Drafting Group have interests in and ties to the existing classifications used as the basis for the development of the International Classification for Patient Safety.
References
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems. Geneva: World Health Organization; 2004. p. 109. vol. 2., 10th Revision. [Google Scholar]
- Fifty-Fifth World Health Assembly. 2002 Res. WHA55.18. 18 May. [Google Scholar]
- Perneger T. Borges on classification. Int J Qual Health Care. 2006;28:264–65. doi: 10.1093/intqhc/mzl008. [DOI] [PubMed] [Google Scholar]
- Chang A, Schyve P, Croteau R, O'Leary D, Loeb J. The JCAHO patient safety event taxonomy: a standardized terminology and classification schema for near misses and adverse events. Int J Qual Health Care. 2005;17:95–105. doi: 10.1093/intqhc/mzi021. [DOI] [PubMed] [Google Scholar]
- The National Reporting and Learning System. National Health Service, National Patient Safety Agency. http://www.npsa.nhs.uk. (14 August 2007, date last accessed) [Google Scholar]
- Runciman WB, Williamson JAH, Deakin A, Benveniste KA, Bannon K, Hibbert PD. An integrated framework for safety, quality and risk management: an information and incident management system based on a universal patient safety classification. Qual Safety Health Care. 2006;15(Suppl. 1):i82–i90. doi: 10.1136/qshc.2005.017467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Schaafe TW PRISMA-Medical. A brief description. Eindhoven: Eindhoven University of Technology, Faculty of Technology Management, Patient Safety Systems, 2005 . [Google Scholar]
- Reason J. Human Error. Cambridge: Cambridge University Press; 1990. [Google Scholar]
- Rasmussen J. Information Processing and Human-Machine Interaction: An Approach to Cognitive Engineering. New York: North-Holland; 1986. [Google Scholar]
- World Health Organization. Project to Develop the International Patient Safety Event Taxonomy: Report of the WHO World Alliance for Patient Safety Drafting Group. Vancouver: British Columbia; 2005. World Alliance for Patient Safety. [Google Scholar]
- Runciman W, Hibbert P, Thomson R, van der Schaaf T, Sherman H, Lewalle P. Towards an international classification for patient safety: key concepts and terms. Int J Qual Health Care. doi: 10.1093/intqhc/mzn057. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Report on the Results of the Web-based Modified Delphi Survey of the International Classification for Patient Safety. Geneva: Switzerland; World Alliance for Patient Safety. Project to Develop the International Classification for Patient Safety. http://www.who.int/patientsafety/taxonomy/delphi/en/index.html , 2007. [Google Scholar]
- Thomson R, Lewalle P, Sherman H, Castro G, Hibbert P, Runciman W. Towards an international classification for patient safety: a Delphi survey. Int J Qual Health Care. doi: 10.1093/intqhc/mzn055. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Report of the WHO World Alliance for Patient Safety Challenge Group Meeting: Validity Testing of the Conceptual framework of the International Classification for Patient Safety. Geneva: Switzerland; World Alliance for Patient Safety. Project to Develop the International Classification for Patient Safety. http://www.who.int/patientsafety/taxonomy/Report_WHO_ICPS_Challenge_Group_10-11Apr08_Geneva.pdf , 2008. [Google Scholar]