Abstract
Background
Understanding the patient safety literature has been compromised by the inconsistent use of language.
Objectives
To identify key concepts of relevance to the International Patient Safety Classification (ICPS) proposed by the World Alliance For Patient Safety of the World Health Organization (WHO), and agree on definitions and preferred terms.
Methods
Six principles were agreed upon—that the concepts and terms should: be applicable across the full spectrum of healthcare; be consistent with concepts from other WHO Classifications; have meanings as close as possible to those in colloquial use; convey the appropriate meanings with respect to patient safety; be brief and clear, without unnecessary or redundant qualifiers; be fit-for-purpose for the ICPS.
Results
Definitions and preferred terms were agreed for 48 concepts of relevance to the ICPS; these were described and the relationships between them and the ICPS were outlined.
Conclusions
The consistent use of key concepts, definitions and preferred terms should pave the way for better understanding, for comparisons between facilities and jurisdictions, and for trends to be tracked over time. Changes and improvements, translation into other languages and alignment with other sets of patient safety definitions will be necessary. This work represents the start of an ongoing process of progressively improving a common international understanding of terms and concepts relevant to patient safety.
Keywords: patient safety, definitions, concepts, terminology, classification
Introduction
Understanding patient safety has been compromised by inconsistent use of language. Similar concepts have different terms (e.g. near miss, close call) and terms are used to embrace several concepts (‘medical error’ for errors, violations and system failures). In a survey, 17 definitions were found for error and 14 for ‘adverse event’ [1]. Another review found 24 definitions for error, with a range of opinions as to what constitutes an error [2]. A need was thus identified for a comprehensive classification, populated by concepts with agreed definitions [3, 4], each labelled by ‘preferred terms’.
The core to the classification is the clear definition of a concept (e.g. failure to carry out a planned action as intended or application of an incorrect plan), which is then given a preferred term (in this case error).
An opportunity to address this arose with the launch of the World Health Organization (WHO) World Alliance for Patient Safety [5]. The formation of a drafting group for an International Classification for Patient Safety (ICPS) is described in a companion paper, with some guiding principles for its development [6]. In another paper [7], a Delphi survey and an iterative refinement process are described, undertaken to develop a conceptual framework populated by relevant concepts. In a parallel iterative process, guided by expert opinion and the Delphi respondents' suggestions, definitions of relevant key concepts with preferred terms were agreed. The present paper describes this process, the key concepts and their resulting definitions and preferred terms, and how they relate to each other and to the ICPS conceptual framework. Further development of the classification will support the measurement of safety, for example, through its application in data collection systems such as incident- reporting systems.
Methods
Many sources of concepts and terms were drawn upon (dictionaries, literature, Internet), including the report of a previous Delphi process (itself drawing upon 165 sources) [1], together with examination of over 700 responses to the Delphi process [7, 8]. Many refinements to the definitions were made through exchanges by email and at five face-to-face meetings of the drafting group [9]. Six principles were agreed, two of which overlap with the principles outlined for the development of the ICPS [6]. It was decided:
that concepts and terms should be applicable across the full spectrum of healthcare from primary to highly specialized care and should be consistent with the existing processes and systems.
that concepts should, whenever possible, be consistent with concepts from other terminologies and classifications in the WHO Family of International Classifications [10];
that definitions of the concepts and the preferred terms should reflect colloquial use;
that definitions of the concepts should convey the appropriate meanings with respect to patient safety;
that definitions should be brief and clear, without unnecessary or redundant qualifiers, starting with basic definitions and then ‘building’ upon them for each subsequent definition; and
that key concepts and preferred terms be fit-for-purpose for the ICPS.
Results
Forty-six key concepts were identified (including those describing the 10 ICPS classes), and definitions and preferred terms were agreed upon at the drafting group meetings.
Following this, experts were invited to a ‘challenge group’ meeting to review the concepts and preferred terms, and suggest refinements and/or clarification. Consequently, two additional key concepts were identified, defined and given preferred terms—giving a total of 48 key concepts and preferred terms.
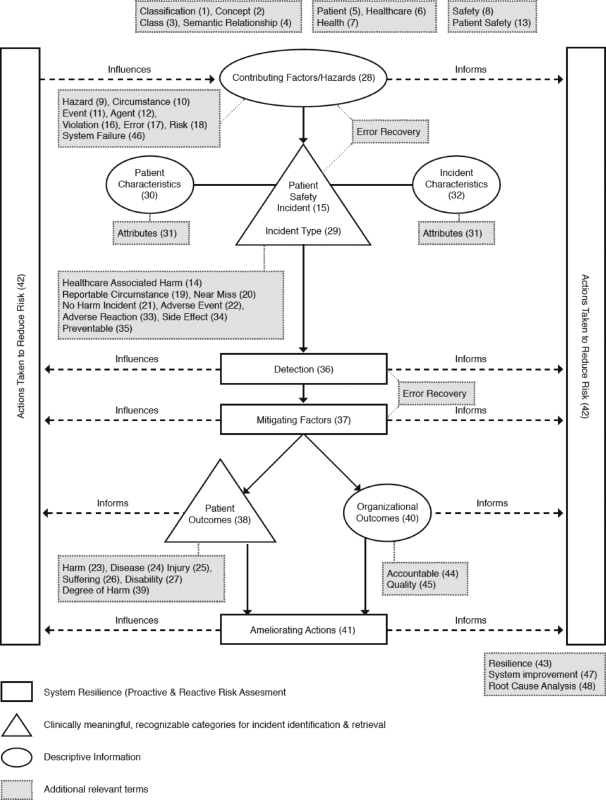
How key terms and concepts chosen relate to the ICPS conceptual framework is shown in Fig. 1. Definitions, labelled by preferred terms, are listed in Table 1 in the sequence in which they are discussed below, with preferred terms listed alphabetically in Table 2.
Figure 1.
Conceptual framework for the ICPS. Solid lines enclose the 10 major classes of the ICPS and represent the semantic relationships between them. The dotted lines link relevant preferred terms to classes. The numbers in parentheses as given in Table 2 represent the sequence in which they appear in the text and in Table 1.
Table 1.
List of preferred terms and definitions for key concepts
|
Table 2.
List of preferred terms for key concepts in alphabetical order
| Accountable (44) | Incident characteristics (32) |
| Actions taken to Reduce Risk (42) | Incident type (29) |
| Adverse reaction (33) | Injury (25) |
| Agent (12) | Mitigating factor (37) |
| Ameliorating action (41) | Near miss (20) |
| Attributes (31) | No harm incident (21) |
| Circumstance (10) | Organizational outcome (40) |
| Class (3) | Patient (5) |
| Classification (1) | Patient characteristic (30) |
| Concept (2) | Patient outcome (38) |
| Contributing factor (28) | Patient safety (13) |
| Degree of harm (39) | Patient safety incident (15) |
| Detection (36) | Preventable (35) |
| Disability (27) | Quality (45) |
| Disease (24) | Resilience (43) |
| Error (17) | Risk (18) |
| Event (11) | Root cause analysis (48) |
| Harm (23) | Safety (8) |
| Harmful incident (adverse event) (22) | Semantic relationship (4) |
| Hazard (9) | Side effect (34) |
| Reportable circumstance (19) | Suffering (26) |
| Health (7) | System failure (46) |
| Healthcare (6) | System improvement (47) |
| Healthcare-associated harm (14) | Violation (16) |
The numbers in parentheses refer to the sequence in which these preferred terms appear in Table 1 and in the text.
Concepts are progressively introduced to allow understanding to be ‘built’, starting with the concepts in the title of the ICPS (classification, patient, safety). The terms in italics have been deemed ICPS-preferred terms. Where terms have been highlighted, the agreed definitions for relevant concepts follow.
A classification is an arrangement of concepts (bearers or embodiments of meaning) into classes (groups or sets of like things, e.g. ‘contributing factors’, ‘incident types’ and ‘patient outcomes’) and their subdivisions linked to express the semantic relationships between them (the way in which they are associated with each other on the basis of their meanings). For example, ‘contributing factors’ precede and play a role in the generation of any ‘incident type’. Similarly, detection precedes ‘mitigating factors’ and is followed by ‘outcomes’; the progression of an incident cannot be limited until it has been detected and its nature determined, and outcomes cannot be described until attempts at limitation have exerted their influence (Fig. 1).
Each class has hierarchically arranged subdivisions populated by concepts (e.g. ‘fatigue/exhaustion’ under the class ‘contributing factors/hazards’). Concepts may be represented by a number of terms that allow for regional dialects, different languages, different clinical disciplines and/or provider or patient preferences.
A patient is a person who is a recipient of healthcare, itself defined as services received by individuals or communities to promote, maintain, monitor or restore health. Patients are referred to rather than clients, tenants or consumers, although it is recognized that many recipients such as a healthy pregnant woman or a child undergoing immunization may not be regarded, or regard themselves, as patients. Healthcare includes self-care. Health is ‘a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’—the WHO definition [11].
Safety is the reduction of risk of unnecessary harm to an acceptable minimum, and hazard a circumstance, agent or action with the potential to cause harm. A circumstance is a situation or factor that may influence an event, agent or person(s), an event is something that happens to or involves a patient, and an agent is a substance, object or system that acts to produce change.
Patient safety is the reduction of risk of unnecessary harm associated with healthcare to an acceptable minimum. Healthcare-associated harm is harm arising from or associated with plans or actions taken during the provision of healthcare, rather than an underlying disease or injury.
A patient safety incident is an event or circumstance that could have resulted, or did result, in unnecessary harm to a patient. In the context of the ICPS, a patient safety incident will be referred to as an incident. The use of the term ‘unnecessary’ in this definition recognizes that errors, violations, patient abuse and deliberately unsafe acts occur in healthcare and are unnecessary incidents, whereas certain forms of harm, such as an incision for a laparotomy, are necessary. The former are incidents, whereas the latter is not.
Incidents arise from either unintended or intended acts. Errors are, by definition, unintentional, whereas violations are usually intentional, though rarely malicious, and may become routine and automatic in certain contexts. An error is a failure to carry out a planned action as intended or application of an incorrect plan. Errors may manifest by doing the wrong thing (commission) or by failing to do the right thing (omission), at either the planning or execution phase [12, 13]. Thus, if screening for bowel cancer involves regular testing for occult blood, then a screening colonoscopy in the absence of prior occult blood testing comprises an error of commission (the application of an incorrect plan), whereas failure to arrange testing for occult blood would constitute an error of omission. Violation is a deliberate deviation from an operating procedure, standard or rule. Both errors and violations increase risk, even if an incident does not actually occur [12, 13]. Risk is the probability that an incident will occur.
A reportable circumstance is a situation in which there was significant potential for harm, but no incident occurred, for example, a busy intensive care unit remaining grossly understaffed for an entire shift, or taking a defibrillator to an emergency and discovering it does not work, although it was not needed. A near miss is an incident which did not reach the patient, for example, a unit of blood being connected to the wrong patient's IV line, but the error detected before the infusion started. A no harm incident is one in which an event reached a patient but no discernable harm resulted, for example, if the unit of blood was infused, but was not incompatible. A harmful incident (adverse event) is an incident that results in harm to a patient, for example, if the wrong unit of blood was infused, and the patient died from a haemolytic reaction.
Harm implies impairment of structure or function of the body and/or any deleterious effect arising there from, including disease, injury, suffering, disability and death, and may be physical, social or psychological. Disease is a physiological or psychological dysfunction, injury is damage to tissues caused by an agent or event and suffering is the experience of anything subjectively unpleasant. Suffering includes pain, malaise, nausea, depression, agitation, alarm, fear and grief. Disability implies any type of impairment of body structure or function, activity limitation and/or restriction of participation in society, associated with past or present harm.
A contributing factor is a circumstance, action or influence (such as poor rostering or task allocation) that is thought to have played a part in the origin or development, or to increase the risk, of an incident. Contributing factors may be external (not under the control of a facility or organisation), organizational (e.g. unavailability of accepted protocols), related to a staff factor (e.g. an individual cognitive or behavioural defect, poor team work or inadequate communication) or patient-related (e.g. non-adherence). A contributing factor may be a necessary precursor of an incident and may or may not be sufficient to cause the incident.
Incidents are classified into a number of different types. An incident type is a category made up of incidents of a common nature, grouped because of shared agreed features (Table 3) and is a ‘parent’ natural category under which many concepts may be grouped.
Table 3.
Incident type
|
An incident can be assigned to several incident types. Thus, for example, an incident in which an infusion pump was set up wrongly and delivered a sedative overdose, causing respiratory arrest, would be allocated both ‘medication’ and ‘equipment’ incident types.
Patient characteristics are selected attributes of a patient, such as patient demographics or the reason for presentation to healthcare. Attributes are qualities, properties or features of someone or something. Incident characteristics are selected attributes of an incident, e.g. care setting, treatment status, specialties involved and date of an incident.
With reference to medication, an adverse reaction is unexpected harm arising from a justified treatment, for example, unexpected neutropenia due to a drug not known to have this effect. Recurrence of a previously encountered adverse reaction may be preventable (e.g. avoiding re-exposure of a patient with drug allergy). Side effect is a known effect, other than that primarily intended, related to a medicine's pharmacological properties, such as nausea after morphine has been given to alleviate pain.
Preventable is being accepted by the community as avoidable in the particular set of circumstances. Detection is an action or circumstance that results in the discovery of an incident, e.g. by noticing an error, by a monitor or alarm, by a change in patient condition or by a risk assessment. Detection mechanisms may be part of the system (such as low pressure disconnect alarm in a breathing circuit), may result from a checking process or from vigilance and ‘situation awareness’.
A mitigating factor is an action or circumstance that prevents or moderates the progression of an incident towards harming a patient. The mechanism by which damage may occur is already in train, but has not yet led to either any or the maximum possible harm.
The term ‘recovery’ has been used to describe the combination of detection and mitigation; it does not refer to clinical recovery (recuperation) but to the process of recovering from an incident that has started. Reconnecting a breathing circuit after a disconnect alarm warning is an example of recovery. By collecting information about how and why ‘saves’ are made, system design, training and education can be informed.
Patient outcome is the impact upon a patient which is wholly or partially attributable to an incident. Where harm has occurred, the degree of harm is the severity and duration of any harm, and any treatment implications, that result from an incident. It would seem, from first principles, desirable to record the nature, severity and duration of harm separately. However, there are problems in doing this with substantial overlap existing between these parameters and previous attempts to rank the degree of harm tend to conflate these parameters into one scale [14–16].
Incidents also affect healthcare organizations. Organizational outcome is the impact upon an organization that is wholly or partially attributable to an incident, e.g. adverse publicity or additional use of resources.
Ameliorating action is an action taken or circumstance altered to make better or compensate any harm after an incident. Patient ameliorating factors are actions taken or circumstances altered to make good harm to a patient, such as fixing a fracture after a fall, whereas healthcare system ameliorating factors reduce loss or damage to an organization, e.g. good public relations management after a publicized disaster will ameliorate the effects on a facility's reputation.
Actions taken to reduce risk are actions taken to reduce, manage or control any future harm, or probability of harm, associated with an incident. Such actions can affect incidents, contributing factors, detection, mitigating factors or ameliorating actions, and can be pro-active or reactive. Pro-active actions may be identified by techniques such as failure mode and effects analysis [17] and probabilistic risk analysis [18], whereas reactive actions are taken in response to insights gained after incidents (e.g. root cause analysis).
Resilience refers to the degree to which a system continuously prevents, detects, mitigates or ameliorates hazards or incidents. Resilience allows an organization to ‘bounce back’ to its original ability to provide core functions as soon as possible after incurring damage.
A number of terms are commonly used regarding organizational management. Accountable is being held responsible. Quality is the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge. System failure refers to a fault, breakdown or dysfunction within an organization's operational methods, processes or infrastructure. Factors contributing to system failure can be latent (hidden or apt to elude notice) or apparent, and can be related to the system, the organization, staff or a patient. A latent factor might be a breathing circuit disconnect alarm with no power failure warning or battery backup [19]. System improvement is the result or outcome of the culture, processes and structures that are directed towards the prevention of system failure and the improvement of safety and quality. Processes to counter the latent failure described would include modification of the equipment to alarm when the power supply is compromised, or use of an additional device, such as a capnograph, to alarm if carbon dioxide is not detected in expired air.
Finally, root cause analysis, a reactive form of risk assessment to inform the development of actions taken to reduce risk, is a systematic iterative process whereby the factors that contribute to an incident are identified by reconstructing the sequence of events and repeatedly asking ‘why?’ until the underlying root causes (contributing factors or hazards) have been elucidated.
Discussion
The consistent use of key concepts with agreed definitions and preferred terms, in conjunction with a comprehensive but adaptable classification, will pave the way for researchers to understand each others' work, and facilitate the systematic collection, aggregation and analysis of relevant information. This will allow comparisons between facilities and jurisdictions, and allow trends to be tracked over time.
Forty-eight concepts were identified, and definitions and preferred terms agreed. The concepts defined and terms chosen so far represent a collection of basic building blocks to enhance the study of patient safety. Definitional refinement will be necessary as our understanding widens and further needs are identified. Translation into other languages is ongoing. More concepts will need to be identified and defined, and decisions made with respect to which terms should be preferred and which terms avoided. An on-going process is planned by which patient safety experts from different cultures and parts of the world will test the ICPS for the appropriateness and relevance of the concepts to ensure they are fit-for-purpose in all the contexts in which the classification will be used. This will ensure that the concepts defined and terms chosen will facilitate the understanding and transfer of information among the increasing number of people with an interest in patient safety.
Some terms for concepts were excluded because their meanings vary across jurisdictions (e.g. ‘negligence’); they have discipline-specific meanings (e.g. ‘accident’—in aviation meaning the loss of an aircraft hull) or are already being used with special meanings in a WHO classification (e.g. ‘complication’, ‘misadventure’ or ‘sequela’). The term ‘healthcare-associated’ was preferred to ‘iatrogenic’ and ‘nosocomial’; these terms are associated with physicians and hospitals, respectively, and the classification is intended to be of relevance across all healthcare.
Other sets of definitions and terms of relevance to patient safety have been developed. Our primary consideration was to try to ensure that our definitions would be ‘fit-for-purpose’ in the specific context of the ICPS. Given the plethora of terms, concepts and definitions, it was inevitable that ours would differ from many others. For example, a Canadian set of patient safety definitions exist, which [20] is somewhat discursive but provides insightful, valuable reflections on 26 concepts, 8 of which terms are defined in our current paper. Comparing the Canadian definitions with the ICPS definitions of the same terms underlines the complexity of trying to unify language and understanding. For example, in the Canadian dictionary, one definition of safety is given that describes a concept similar to that agreed by the ICPS, but the ‘recommendation’ is for another definition to be used which describes the ‘processes’ for ‘enhancing’ safety (‘ … the reduction and mitigation of unsafe acts within the healthcare system … ’).
A European set of definitions [21] was also developed at the same time as the ICPS. Although the World Alliance and the Australian Council for Safety and Quality are cited as sources for this work, of the 6 definitions in their list of 24, which are also in the ICPS set, only 1 (risk) describes a similar concept. The concept of risk is the only one similar in both the Canadian and European definitions to the concept agreed by the World Alliance. Alignment of concepts, terms and definitions in the ICPS with those in other extant sets is highly desirable; they include definitions that should be considered for adoption by the ICPS.
In summary, definitions for 48 concepts relevant to patient safety, with their preferred terms, have been agreed. Their relationships to each other and to the conceptual framework of the ICPS have been described. This represents the start of a necessary on-going process of progressively improving a common international understanding of terms and concepts relevant to patient safety, as a pre-requisite for properly prosecuting some of the action areas identified by the WHO resolution on patient safety: the determination of global norms, and standards and guidelines for the definition, measurement and reporting of adverse events and near misses in healthcare; the promotion and framing of evidence-based policies; and international benchmarking.
Funding
The Project to Develop the ICPS was funded by the World Health Organization World Alliance for Patient Safety, Geneva, Switzerland. The conceptual framework for the ICPS in the intellectual property of the World Health Organization.
Acknowledgements
The members of the challenge group are thanked. They were: Dr Ahmed Al-Mandhari, Dr Mahi Al-Tehewy, Dr Rene Amalberti, Mr Brian Capstick, Dr Mark Chassin, Dr Peter Goldschmidt, Dr Harold Kaplan, Dr Tebogo Kgosietsile Letlape, Professor James Reason, Dr Pedro Saturno, Dr Kenirchiro Taneda, Dr Mikel Torrontegui.
Conflict of interest: Some of the members of the Drafting Group have interests in and ties to the existing classifications used as the basis for the development of the International Classification for Patient Safety.
References
- Runciman WB. Shared meanings: preferred terms and definitions for safety and quality concepts. Med J Aust. 2006;184(10 Suppl):S41–S43. doi: 10.5694/j.1326-5377.2006.tb00360.x. [DOI] [PubMed] [Google Scholar]
- Elder NC, Pallerla H, Regan S. What do family physicians consider an error? A comparison of definitions and physician perception. BMC Fam Pract. 2006;7:73. doi: 10.1186/1471-2296-7-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runciman WB, Williamson JA, Deakin A, et al. An integrated framework for safety, quality and risk management: an information and incident management system based on a universal patient safety classification. Qual Saf Health Care. 2006;15(Suppl 1):i82–i90. doi: 10.1136/qshc.2005.017467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang A, Schyve PM, Croteau RJ, et al. The JCAHO patient safety event taxonomy: a standardized terminology and classification schema for near misses and adverse events. Int J Qual Health Care. 2005;17:95–105. doi: 10.1093/intqhc/mzi021. [DOI] [PubMed] [Google Scholar]
- World Health Organization. World Alliance for Patient Safety: Forward Programme 2005. Geneva: World Health Organization; 2004. [Google Scholar]
- Sherman H, Castro G, Fletcher M, et al. Towards an International Classification for Patient Safety: the Conceptual Framework. Int J Qual Health Care. doi: 10.1093/intqhc/mzn054. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson R, Lewalle P, Sherman H, et al. Towards an International Classification for Patient Safety: a Delphi Survey. Int J Qual Health Care. doi: 10.1093/intqhc/mzn055. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drafting Group of the Project to Develop the International Classification for Patient Safety. Geneva: World Health Organization; 2007. Report on the results of the web-based modified Delphi survey of the International Classification for Patient Safety. [Google Scholar]
- Project to Develop the International Classification for Patient Safety. Geneva: World Health Organization; 2007. Report of the WHO World Alliance for Patient Safety Drafting Group, 6–7 December 2007. [Google Scholar]
- Madden R, Sykes C, Ustun TB. World Health Organization Family of International Classifications: Definition, Scope and Purpose. Geneva: World Health Organization; 2007. [Google Scholar]
- World Health Organization. Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference; 19–22 June; New York. 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, no. 2, p. 100) and entered into force on 7 April 1948. www.who.int/en/ [Google Scholar]
- Reason J. Human Error. New York: Cambridge University Press; 1990. [Google Scholar]
- Runciman WB, Merry AF, Tito F. Error, blame and the law in health care – an Antipodean perspective. Ann Intern Med. 2003;138:974–9. doi: 10.7326/0003-4819-138-12-200306170-00009. [DOI] [PubMed] [Google Scholar]
- NSW Health. Sydney: New South Wales Health; 2007. Incident Management. [Google Scholar]
- VA National Center for Patient Safety. VA National Patient Safety Improvement Handbook. Washington DC: Department of Veterans Affairs, US Veterans Health Administration; 2002. [Google Scholar]
- National Patient Safety Agency. eForm User Guide v4. http://www.eforms.npsa.nhs.uk/staffeform/help/ALL/eForm_Help.htm. (27 November 2008, date last accessed) [Google Scholar]
- Senders JW. FMEA and RCA: the mantras of modern risk management. Qual Saf Health Care. 2004;13:249–50. doi: 10.1136/qshc.2004.010868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marx DA, Slonim AD. Assessing patient safety risk before the injury occurs: an introduction to sociotechnical probabilistic risk modelling in health care. Qual Saf Health Care. 2003;12(Suppl 2):ii33–8. doi: 10.1136/qhc.12.suppl_2.ii33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myerson K, Ilsley AH, Runciman WB. An evaluation of ventilator monitoring alarms. Anaesth Intens Care. 1986;14:174–85. doi: 10.1177/0310057X8601400213. [DOI] [PubMed] [Google Scholar]
- Davies JM, Hébert P, Hoffman C. The Canadian Patient Safety Dictionary. Ottawa, Canada: Royal College of Physicians and Surgeons of Canada; 2003. [Google Scholar]
- Kristensen S, Mainz J, Bartels P. Patient Safety – a Vocabulary for European Application. Aarhus, Denmark: SIMPATIE European Society for Quality in Healthcare – Office for Quality Indicators; 2007. [Google Scholar]