Portal, as opposed to systemic, venous drainage from small intestinal allografts is thought to be preferable because it provides unquestionable physiologic (1–3) and hypothetic, but unverified (4, 5) immunologic advantages. However, in clinical instances, it may be difficult to find a place on the recipient portal or superior mesenteric vein (SMV) where the donor portal vein can be anastomosed. We encountered this problem in two most recent solitary intestinal transplants. One patient was an adult with 15 previous abdominal operations and the other was a child with only one earlier laparotomy.
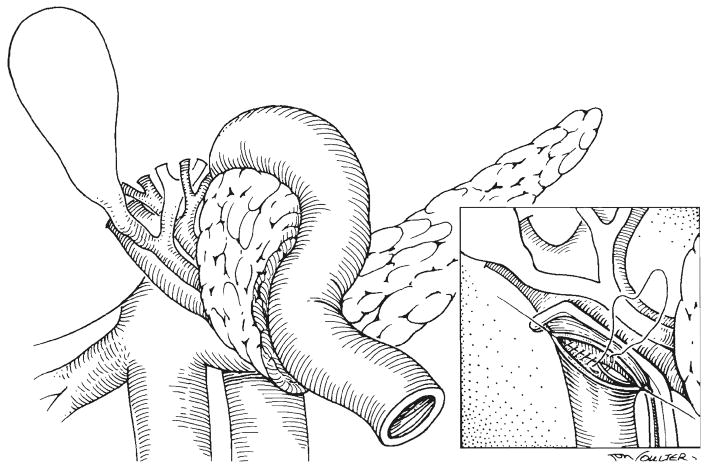
The abdomen was entered through an upper transverse incision. Because of multiple adhesions, the recipient SMV could not be adequately exposed below the pancreas. The duodenum and head of the pancreas were mobilized, exposing the infrarenal aorta for arterialization of the graft. The maneuver helped expose the extrahepatic portal vein as for portacaval shunts (Fig. 1). The common bile duct and, in the pediatric patient, an ectopic right hepatic artery arising from the superior mesenteric artery (SMA) were identified and carefully preserved.
Fig.1.
The recipient duodenum has been kocherized. The portal vein and infrarenal aorta are exposed. Common bile duct and hepatic artery are identified. Inset, technique of end to side anastomosis.
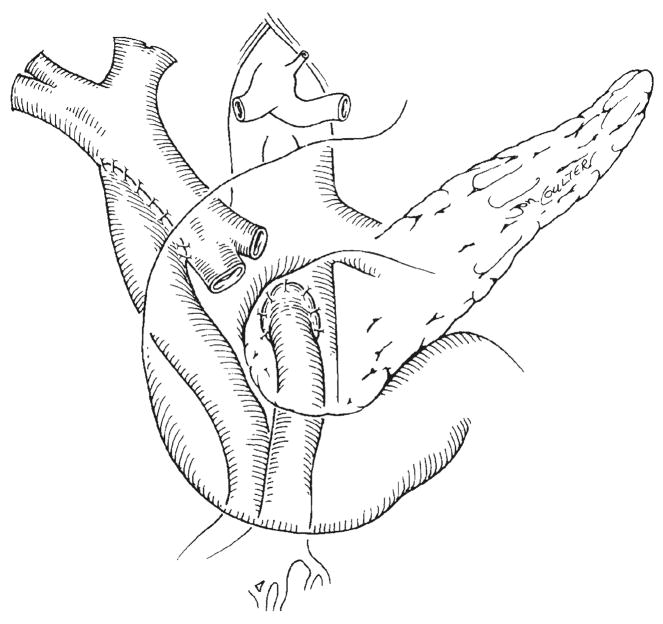
The arterial anastomosis of the donor SMA to the infrarenal aorta was performed first. A side biting vascular clamp was subsequently placed on the recipient portal vein and an end to side anastomosis of the donor to the recipient portal vein was performed (Fig. 1, inset). Arterial and venous reconstructions were satisfactory (Fig. 2).
Fig. 2.
The vascular anastomoses are completed and the duodenum is allowed back to its anatomic position.
A recipient duodenum to donor jejunum anastomosis, a terminal ileostomy and feeding jejunostomy were performed in both patients. In the pediatric patient, a donor ileum to recipient transverse colonic anastomosis was also performed. Immunosuppression was with FK 506 and steroids. There were no technical complications.
Finding a residual portal or SMV stump for end to end anastomosis of the intestinal graft vein is a daunting prospect in patients who have lost their intestine. Although candidates for intestinal transplantation can be expected to have had multiple abdominal operations, the hepatic hilum usually is spared, providing a site onto which the donor SMV or portal vein can be anastomosed piggyback. The aforementioned technique should provide dependable portal drainage in most instances. The splenic vein could be alternatively used, using the same principle.
Acknowledgments
Supported, in part, by research grants from the Veterans Administration and the National Institutes of Health, Bethesda, Maryland
References
- 1.Starzl TE, Todo S, Tzakis A, et al. The many faces of multivisceral transplantation. Surg Gynecol Obstet. 1991;172:335–344. [PMC free article] [PubMed] [Google Scholar]
- 2.Koltan WA, Madera JL, Smith RJ, Kirkman RL. Metabolic aspects of small bowel transplantation in inbred rats. J Surg Res. 1987;42:341–347. doi: 10.1016/0022-4804(87)90167-3. [DOI] [PubMed] [Google Scholar]
- 3.Schraut WH, Rosermurgy AS, Riddle RH. Prolongation of intestinal allograft survival without immunosuppressive drug therapy. J Surg Res. 1983;34:597–607. doi: 10.1016/0022-4804(83)90116-6. [DOI] [PubMed] [Google Scholar]
- 4.Mazzoni G, Benichou J, Porter KA, Starzl TE. Renal homotransplantation with venous outflow or infusion of antigen into the portal vein of dogs or pigs: Transplantation at portal site. Transplantation. 1977;24:268–273. doi: 10.1097/00007890-197710000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murase N, Demetris AJ, Furuya T, et al. Comparison of the small intestine after multivisceral transplantation of the small intestine transplanted with portal versus caval drainage. Transplant Proc. 1992;24:1143–1144. [PMC free article] [PubMed] [Google Scholar]