Summary
Signs and symptoms obtained by clinical examination and endoscopic observations in consecutive subjects presenting at our Phoniatry and Logopedics Service from 1998 to 2003 for swallowing disorders were reviewed and evaluated statistically. The predictive power of these parameters is discussed in terms of short-term complications of dysphagia (aspiration). Epidemiological considerations are made based on a statistical model.
Keywords: Swallowing disorders, Dysphagia, Aspiration, Diagnosis, Endoscopy, Statistical analysis
Riassunto
Segni clinici desunti da valutazioni cliniche non strumentali e strumentali endoscopiche di clienti consecutivi con disturbi della deglutizione afferiti al nostro servizio di Foniatria e Logopedia dal 1998 al 2003 sono stati considerati e valutati numericamente. Considerazioni vengono fatte in senso predittivo, nei confronti di complicanze a breve termine di disfagia (aspirazione), ed epidemiologico, sulla scorta di un modello statistico, elaborato considerando i parametri suddetti.
Introduction
The demand for consultations for patients with swallowing disorders is destined to increase over the next few years 1 2. The availability of centres for the study and treatment of swallowing disorders represents a useful resource for residential services managing patients with different burdens of care.
At our Health Agency, we have been actively engaged in the issue of swallowing disorders since 1997, and our case series provides a pool of data for statistical retrospective evaluation. Despite changes in the clinical approach and instrumentation, over time, a critical evaluation of this activity has offered the possibility to extract some parameters that may be useful in identifying subjects with dysphagia (predictive value).
Aim of the study was to apply statistical methods to select those parameters with the greatest predictive power for identifying the risk of complications from swallowing disorders (aspiration).
Materials, methods and results
Consecutive subjects seen at our Phoniatry and Logopedics Service for swallowing disorders were evaluated from mid 1998 to 2003. Subjects were submitted to the following diagnostic workup 3–7:
Clinical history;
Clinical evaluation (informal BSE: bedside swallowing examination) that probes the functions listed in Table I, according to the scientific evidence in this field;
Endoscopy (FEES: fiberoptic endoscopic examination of swallow) carried out, as described elsewhere 8, and completed with dynamic tests with bolus 9–13. In our practice, radiological studies (videofluoroscopic assessment and DSI) are limited to selected cases, those with unclear diagnostic questions, to confirm oesophageal disorders and after head and neck surgery or in degenerative neurological disorders.
Table I. Clinical swallowing examination protocol.
| 1.Mental status |
| 2.Language |
| 3. Speech and articulation |
| 4. Respiratory function/expiration |
| 5. Voice and resonance |
| 6. Positioning |
| 7. Lip sensation, strength and seal |
| 8. Mouth opening |
| 9. Muscles of mastication |
| 10. Dentition and periodontium |
| 11. Salivary flow |
| 12. Oral and pharyngeal sensation (gag reflex) |
| 13. Tongue movement and strength |
| 14. Velar elevation |
| 15. Volitional swallow |
| 16. Food and liquid swallows |
The main parameters of the BSE and endoscopic evaluation were considered to determine their level of sensitivity and specificity in order to predict the risk of aspiration (predictive value).
Our case series is heterogeneous and includes acute, subacute, nursing home and rehabilitation in-patients and out-patients. A total of 520 subjects (V = 0), 323 male, 197 female (mean age 67.23 years) were taken into consideration. Based on the endoscopy results, the population was divided into two groups: 378 non-aspirating subjects (V0 = 0) and 142 aspirating subjects (V0 = 1).
The parameters chosen (independent variables) for the individual groups and pooled sample with their means and standard deviation (SD) are reported in Table II. Age was reported as decades and globally evaluated as significant or non-significant.
Table II. Mean and standard deviation (SD) for predictor variables in aspiration, non-aspiration and pooled groups.
| Non-aspiration | Aspiration | Pooled | ||||
| Factors | Mean | SD | Mean | SDcc | Mean | SD |
| X1 = Collaboration | 0.862 | 0.345 | 0.641 | 0.481 | 0.802 | 0.399 |
| X2 = Gurgling voice | 0.071 | 0.258 | 0.106 | 0.308 | 0.081 | 0.273 |
| X3 = Sensation | 0.995 | 0.073 | 0.979 | 0.144 | 0.990 | 0.098 |
| X4 = Dysarthria | 0.217 | 0.413 | 0.254 | 0.437 | 0.227 | 0.419 |
| X5 = Aphasia | 0.087 | 0.283 | 0.070 | 0.257 | 0.083 | 0.276 |
| X6 = Delayed trigger | 0.061 | 0.239 | 0.380 | 0.487 | 0.148 | 0.356 |
| X7 = Age/10 | 6.786 | 1.378 | 6.556 | 1.544 | 6.723 | 1.427 |
| X8 = Sex (0 = M – 1 = F) | 0.397 | 0.490 | 0.387 | 0.489 | 0.394 | 0.489 |
| X9 = TBI | 0.029 | 0.168 | 0.042 | 0.202 | 0.033 | 0.178 |
| X10 = Stroke | 0.772 | 0.420 | 0.697 | 0.461 | 0.752 | 0.432 |
| X11a = Degenerative neurological diseases | 0.093 | 0.290 | 0.106 | 0.308 | 0.096 | 0.295 |
| X11b = Other diseases | 0.114 | 0.318 | 0.169 | 0.376 | 0.129 | 0.335 |
| X12 = Pre-swallow dump | 0.474 | 0.500 | 0.542 | 0.500 | 0.492 | 0.500 |
| X13 = Cough-penetration | 0.127 | 0.333 | 0.718 | 0.451 | 0.288 | 0.453 |
| X14a = Pooling | 0.431 | 0.496 | 0.634 | 0.483 | 0.487 | 0.500 |
| X14b = Post-swallow dump | 0.040 | 0.195 | 0.106 | 0.308 | 0.058 | 0.233 |
| X14c = Dry swallow | 0.373 | 0.484 | 0.507 | 0.502 | 0.410 | 0.492 |
The pooled data were submitted to discriminant analysis and logistic regression which provide similar descriptive information but present peculiarities that help to better understand the impact of individual factors and the mechanisms behind the model used to predict subjects with aspiration.
Outcome of the discriminant analysis is shown in Table III.
Table III. Test of equality of group means for predictor variables.
| Tests of Equality of Group Means Factors | Wilks’ Lambda | F | df1 | df2 | Sig. |
| X1 = Collaboration | 0.9386 | 33.8637 | 1 | 518 | 0.0000 |
| X2 = Gurgling voice | 0.9969 | 1.6255 | 1 | 518 | 0.2029 |
| X3 = Sensation | 0.9948 | 2.7220 | 1 | 518 | 0.0996 |
| X4 = Dysarthria | 0.9985 | 0.7859 | 1 | 518 | 0.3757 |
| X5 = Aphasia | 0.9993 | 0.3865 | 1 | 518 | 0.5344 |
| X6 = Delayed trigger | 0.8394 | 99.0818 | 1 | 518 | 0.0000 |
| X7 = Age/10 | 0.9948 | 2.7036 | 1 | 518 | 0.1007 |
| X8 = Sex (0 = M – 1 = F) | 0.9999 | 0.0389 | 1 | 518 | 0.8438 |
| X9 = TBI | 0.9989 | 0.5631 | 1 | 518 | 0.4533 |
| X10 = Stroke | 0.9940 | 3.1449 | 1 | 518 | 0.0767 |
| X11a = Degenerative neurological diseases | 0.9996 | 0.2013 | 1 | 518 | 0.6539 |
| X11b = Other diseases | 0.9946 | 2.8124 | 1 | 518 | 0.0941 |
| X12 = Pre-swallow dump | 0.9963 | 1.9495 | 1 | 518 | 0.1632 |
| X13 = Cough-penetration | 0.6618 | 264.6835 | 1 | 518 | 0.0000 |
| X14a = Pooling | 0.9674 | 17.4621 | 1 | 518 | 0.0000 |
| X14b = Post-swallow dump | 0.9841 | 8.3597 | 1 | 518 | 0.0040 |
| X14c = Dry swallow | 0.9853 | 7.7522 | 1 | 518 | 0.0056 |
The test of equality of group means provides an estimate of the probability of significance (p value) for the discrimination between the groups (Sig). Values of p ≤ 0.05 are significant and of p ≥ 0.10 not significant.
Since this analysis is univariate, we can also consider borderline values of significance for 0.05 < p < 0.10. The influence of these factors is predictable and including them in the model is not likely to modify the significant values.
Evaluation of the predictive groups provided by this analysis confirms that 83.1% of the original data were correctly classified (classification error of 16.9%) which means that the number of subjects without aspiration becomes 319 and those with aspiration 113. Results and percentage data are reported in Table IV. From the Table, we can find the values of sensitivity and specificity of the statistical model.
Table IV. Discriminant function and classification obtained.
| Discriminant function | Assigned group | |||||
| Centroid evaluation | Original | Groups | Non-aspiration | Aspiration | Total | |
| Non-aspiration | 0.530125 | Frequency | Aspiration | 319 [TN] | 59 [FN] | 378 |
| Aspiration | -1.41118 | Non-aspiration | 29 [FP] | 113 [TP] | 142 | |
| % | Aspiration | 84.39 | 15.61 | 100 | ||
| Non-aspiration | 20.42 | 79.58 | 100 | |||
TP (true Positives), FP (False Positives), FN (False Negatives), TN (true Negatives)
Sensitivity = 100* 319/319 + 29 = 91.66%
Specificity = 100* 113/113 + 59 = 65.69%
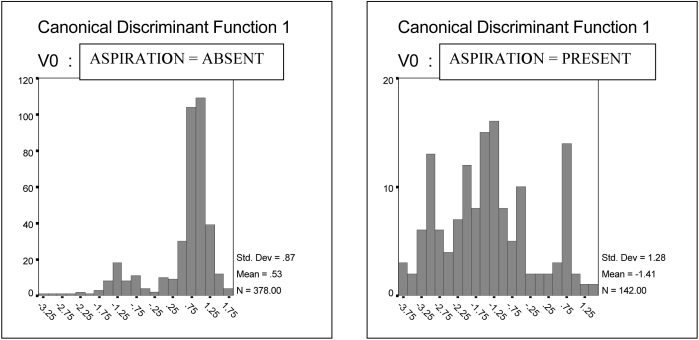
Histograms of the discriminant functions for the two groups are shown separately in Figure 1.
Fig. 1. Distribution (absolute frequency) of value of discriminant function for non-aspiration and aspiration groups.
x-Axis = values of discriminant function
y-Axis = number of subjects
Bars express score of non-aspiration and aspiration groups, respectively.
In the group without aspiration, the distribution is skewed strongly to the right, supporting the prediction made by the model; whereas for the group with aspiration, the distribution is more dispersed, though presenting an appreciable skew to the left, even if a non-negligible number fall in the area of non-aspiration (classification error).
A logistic regression was run on the same data including all the factors in the model and exploiting automatic selection of the most significant factors by the backward method. The recursion was interrupted at the next to last step to provide a model maintaining the sensation factor (X3). The risk of aspiration, in the series examined, includes the following factors in the final model (with the associated levels of significance) (Table V).
Table V. Logistic regression coefficient (B), standard error (SE), Wald statistic, degrees of freedom (DF), probability of significance, adjusted Odds ratio (OR) [Exp(B)] (impact on classification outcome).
| Factors | B | SE | Wald | DF | Significance | Exp(B) |
| X1 = Collaborative | –0.79646 | 0.30303 | 6.90833 | 1 | 0.0086 | 0.45092 |
| X3 = Sensation | –1.88258 | 1.11861 | 2.83239 | 1 | 0.0924 | 0.15220 |
| X6 = Delayed trigger | 2.04341 | 0.34655 | 34.76907 | 1 | 0.0000 | 7.71691 |
| X7 = Age/10 | –0.17599 | 0.08818 | 3.98328 | 1 | 0.0459 | 0.83863 |
| X11a = Degenerative neurological diseases | –0.96930 | 0.45425 | 4.55333 | 1 | 0.0328 | 0.37935 |
| X13 = Cough-penetration | 2.77347 | 0.27306 | 103.16791 | 1 | 0.0000 | 16.01403 |
| Constant | 1.30529 | 1.25307 | 1.08507 | 1 | 0.2976 | 3.68874 |
To correctly interpret the coefficients one must appreciate the negative and positive values since they express opposite effects. Particularly the Exp(B) column expresses an adjusted relationship of a likelihood relationship (Odds Ratio, OR) which is obtained by a simple size holding other variables.
Since the variables considered are dichotomic (with values of 0 or 1) the ratio expresses how many more times the subject has the probability to be in the condition where the dependent variable equals 1 (V0 = 1), namely the aspirating condition. In particular, when the OR is less than 1 (negative B coefficient), the factor characterizes non-aspirators (V0 = 0) viceversa when the OR is greater than 1 (positive B coefficient) the factor characterizes aspirators (V0 = 1). The factors with positive coefficients are X6 (delayed trigger) and X13 (cough-penetration).
As with discriminant analysis, the classification table produced by the regression model, considering the original and predicted distribution, is reported in Table VI. Again the positive predictive value can be expressed as the percentage of correctly classified cases, here 84.23%. The sensitivity and specificity can be calculated from the table using the formulas reported:
Table VI. Classification obtained with logistic regression model.
| Predicted group | Total | ||
| Original Group | Absent | Present | % correct |
| Absent (V0 = 0) | 343 [TP] | 35 [FP] | 90.74 |
| Present (V0 = 1) | 47 [FN] | 95 [TN] | 66.90 |
| Total | 84.23 | ||
TP (true Positives), FP (False Positives), FN (False Negatives), TN (true Negatives)
Specificity = 100* 95/95 + 35 = 73.07%
Sensitivity = 100* 343/343 + 47 = 87.94%
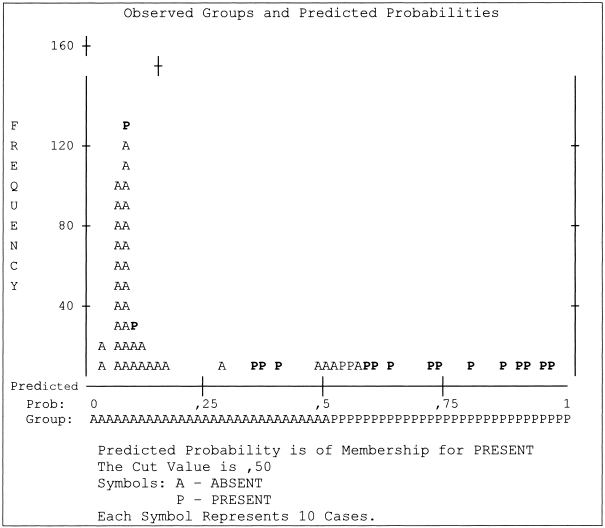
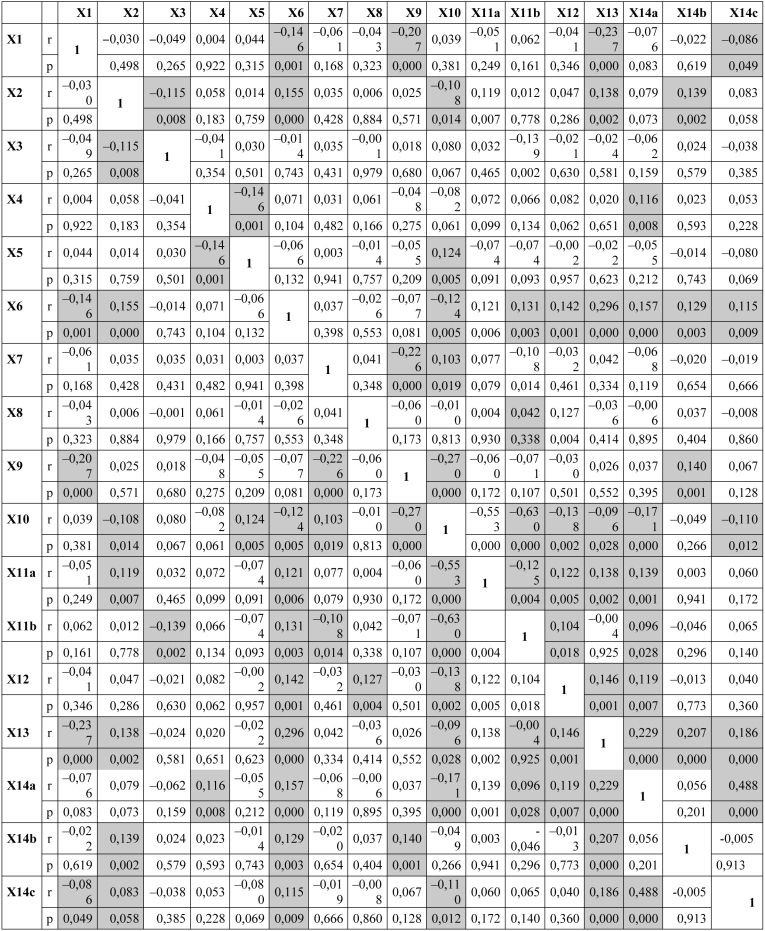
Distribution of the regression constant in the two groups is plotted in Figure 2. Note that the variables defined as significant by the logistic regression model differ, in part, from those obtained at discriminant analysis. This may be explained by the structure of the correlation between the predictor variables. When there is a strong correlation between variables, the introduction of one of these into the model can modify the selection of the other in the recursion since its weight is already accounted for by the information contained in the other variables of the group. A more in depth evaluation of the data can be run on the matrixes of correlation, as reported in Table VII.
Fig. 2.
Distribution of classification across the two groups obtained with logistic regression model (obtained by SPSS).
Table VII. Correlation matrixes.
Discussion
Some considerations can be drawn from the numerical analysis described above in terms of the percentage of correct classification of our sample (predictive value) expressed both as comparison of means (83.1%) and logistic regression (84.23%). The predictive value of our model may be considered adequate in the light of the heterogeneity of the sample and large number of variables included. The distribution of subjects with aspiration is more dispersed than those without aspiration who, in any case, can be better identified, despite the lack of instrumental studies. In the logistic regression, some endoscopic parameters that are highly significant at the comparison of means lose their predictive impact since they are overwhelmed by other factors that have a greater statistical weight, even though they are typical features (delayed trigger, pooling, etc.) used to discriminate between subjects with or without aspiration. In these terms, we can consider that although mean of pre-swallow dumping (X12) does not differ significantly in the regression matrix of Table VI, pre-swallow dumping is significantly correlated with the delayed trigger (X6), cough and penetration (X15) and thus expresses the risk of aspiration. Given the type of sample, we extracted a subgroup of specific disorders that place the subject in a high risk population for aspiration (TBI, stroke, degenerative neurological diseases) 7 14–21: this high risk class was also identified as such by our model. Another finding worth mentioning, in keeping with the literature, is the importance of sensation 22–26, collaboration and age 22 27 28 in mediating the risk of aspiration.
This analytical approach may help identify the clinical and instrumental parameters that better identify patients at risk for aspiration and that require more aggressive management and follow-up.
References
- 1.ASHA Desk Reference. Scope of Practice in Speech-Language Pathology. Cardinal Documents of the Association I-22a/2001. [Google Scholar]
- 2.ASHA Special Populations. Dysphagia. Edition Rockville MD 2002. [Google Scholar]
- 3.Agency for Health Care Policy and Research. Diagnosis and treatment of swallowing disorders (dysphagia) in acute-care stroke patients. Evidence Report/Technology Assessment, n. 8; 1999. [PMC free article] [PubMed] [Google Scholar]
- 4.Gonella ML, Viganò M, Cusaro G, Cancialosi P, Buratti MG, Unnia L, et al. Turbe della deglutizione in età adulta. In: Schindler O, editor. Elementi di semeiologia non strumentale. Manuale operativo di fisiopatologia della deglutizione. Turin: Edizioni Omega; 1990. p. 145-60. [Google Scholar]
- 5.Vernero I, Gambino M, Farri A. Percorsi valutativi e rimediativi in età evolutiva, adulta ed involutiva. Acta Phon Lat 2001;23:192-209. [Google Scholar]
- 6.Ruoppolo G, Amitrano A, Accornero A, Di Rosa R. Protocollo diagnostico per la disfagia in età adulta. Acta Phon Lat 2001;23:220-39. [Google Scholar]
- 7.Vernero I, Gambino M, Schindler A, Schindler O. Cartella logopedia. Età adulta ed involutiva. Turin: Edizioni Omega; 2002. [Google Scholar]
- 8.Farneti D. Valutazione videoendoscopica. In: Schindler O, Ruoppolo G, Schindler A, editors. Deglutologia. Turin: Edizioni Omega; 2001. p. 167-88. [Google Scholar]
- 9.Langmore SE, Schatz K, Olsen N. Fiberoptic endoscopic examination of swallowing safety: a new procedure. Dysphagia 1988;2:216-9. [DOI] [PubMed] [Google Scholar]
- 10.Langmore SE, Schatz K, Olson N. Endoscopic and videofluoroscopic evaluations of swallowing and aspiration. Ann Otol Rhinol Laryngol 1991;100:678-81. [DOI] [PubMed] [Google Scholar]
- 11.Bastian RW. Contemporary diagnosis of the dysphagic patient. In: Dysphagia in children, adults, and geriatrics. Otolaryngol Clin North Am 1998;31:489-506. [DOI] [PubMed] [Google Scholar]
- 12.Farneti D. Ruolo e contributo infermieristico nella odierna gestione del cliente con disturbi della deglutizione. Biblioteca informatica IPASVI 2003. [Google Scholar]
- 13.Farneti D. Utilità della valutazione fibroscopica nella gestione del cliente con disturbi della deglutizione. I Care 2001;3:75-8. [Google Scholar]
- 14.Splaingard ML, Hutchins B, Chaudhuri G. Aspiration in rehabilitation patients: videofluoroscopy vs bedside clinical assessment. Arch Phys Rehabil 1988;68:637-40. [PubMed] [Google Scholar]
- 15.Bisch EM, Logemann JA, Rademaker AW, Kahrilas PJ, Lazarus CL. Pharyngeal effects on bolus volume, viscosity and temperature in patients with dysphagia from neurologic impairment and in normal subjects. JSHR 1994;37:1041-9. [DOI] [PubMed] [Google Scholar]
- 16.Schindler O, Vernero I, Miletto AM, Ruoppolo G, Gonella ML, Travalica Cupillo B. Aspetti particolari legati al coma e al danna iatrogeno causato dalle necessità di assistenza. Acta Phon Latina 1997;19:61-74. [Google Scholar]
- 17.Smithard DG, O’Neill PA, Park C, Renwik DS, Wyatt R, Morris J, et al. Can bedside assessment reliably exclude aspiration following acute stroke? Age Aging 1998;27:99-106. [DOI] [PubMed] [Google Scholar]
- 18.Hallewell B, Katz RC. Technological applications in the assessment of acquired neurogenic communication and swallowing disorders in adults. Seminars in Speech and Language 1999;20:149-67. [DOI] [PubMed] [Google Scholar]
- 19.Mackay LE, Morgan AS, Berstein BA. Factors affecting oral feeding with severe traumatic brain injury. J Head Trauma Rehabil 1999;14:435-47. [DOI] [PubMed] [Google Scholar]
- 20.Mackay LE, Morgan AS, Berstein BA. Swallowing disorders in severe brain injury: risk factors affecting return to oral intake. Arch Phys Med Rehabil 1999;80:365-71. [DOI] [PubMed] [Google Scholar]
- 21.Miletto AM, Affilastro N, Di Rosa R. Protocollo terapeutico nel cliente traumatizzato cranico. Acta Phon Latina 2001;23:248-63. [Google Scholar]
- 22.Aviv JE, Martin JH, Jones ME, Diamond B, Keen MS, Wee TA, et al. Age related changes in pharyngeal and supraglottic sensation. Ann Otol Rhinol Laryngol 1994;103:749-52. [DOI] [PubMed] [Google Scholar]
- 23.Aviv JE, Martin JH, Sacco RL, Zagar D, Diamond B, Keen MS, et al. Supraglottic and pharyngeal sensory abnormalities in stroke patients with dysphagia. Ann Otol Rhinol Laryngol 1996;105:92-7. [DOI] [PubMed] [Google Scholar]
- 24.Aviv JE, Sacco RL, Mohr JP, Thompson JLP, Levin B, Sunshine S, et al. Laryngopharyngeal sensory testing with modified barium swallow as predictor of aspiration pneumonia after stroke. Laryngoscope 1997a;7:1254-60. [DOI] [PubMed] [Google Scholar]
- 25.Aviv JE, Sacco RL, Thomson J, Tandon R, Diamond B, Martin JH, et al. Silent laryngopharyngeal sensory deficits after stroke. Ann Otol Rhinol Laryngol 1997b;106:87-93. [DOI] [PubMed] [Google Scholar]
- 26.Langmore SE. Laryngeal sensation: a touchy subject. Dysphagia 1998;13:93-4. [PubMed] [Google Scholar]
- 27.Bannister P, Stanners AJ, Mountford RA. Dysphagia in the elderly: what does it mean to the endoscopist? JRSM 1990;83:552-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Frederick MG, Ott DJ, Grishaw EK, Gelfand DW, Chen MYM. Functional abnormalities of the pharynx: a prospective analysis of radiographic abnormalities relative to age and symptoms. Am J Rad 1996;166:353-7. [DOI] [PubMed] [Google Scholar]