Summary
Surgery is the treatment of choice for the management of malignant nasal/ethmoidal tumours, followed, in most cases, by external radiotherapy. Two main procedures are adopted to resect these tumours depending upon stage and extension: ethmoidectomy and medial maxillectomy, via a transfacial approach, or craniofacial resection with a combined transcranial and transfacial approach. The nasal cheek flap technique allows complete nasal swing thus obtaining a wide access to both the nasal fossae and the ethmoidal labyrinth. Furthermore, this approach can also be used in the management of small intracranial tumours extended through the skull base to the nasal cavity, paranasal sinuses, upper and middle clivus. We have used the nasal cheek flap since 1992 with good aesthetic and functional results. Aim of the present study was to analyse personal experience, focusing on complications, aesthetic results and self-evaluation expressed by the patients.
Keywords: Paranasal sinuses, Ethmoidal neoplasms, Surgical treatment, Nasal cheek flap
Riassunto
La chirurgia è il trattamento di scelta delle neoplasie maligne naso-etmoidali, seguita per lo più dalla radioterapia. Principalmente vengono utilizzate due tecniche chirurgiche per l’asportazione di questi tumori: l’etmoidectomia e la maxillectomia mediale per via transfacciale, e la resezione cranio-facciale per via combinata transcranica e transfacciale. La tecnica del lembo nasogenieno permette una completa mobilizzazione del naso, che consente un ampio accesso alle cavità nasali ed al labirinto etmoidale. Inoltre, questo approccio può essere utilizzato per l’asportazione di piccoli tumori intracranici, estesi attraverso la base cranica alle cavità nasali, ai seni paranasali e al clivo. Dal 1992 noi utilizziamo il lembo naso-genieno con ottimi risultati funzionali ed estetici. Scopo del presente studio è l’analisi dell’esperienza personale, in particolare per quanto riguarda le complicazioni, i risultati estetici e l’autovalutazione eseguita dai pazienti.
Introduction
Surgery is the treatment of choice for the management of malignant nasal/ethmoidal tumours followed, in most cases, by external radiotherapy 1.
Two main procedures are adopted to resect these tumours, the choice depending upon staging and extension: ethmoidectomy and medial maxillectomy, via a transfacial approach, or craniofacial resection through combined transcranial and transfacial approaches 2 3.
The rationale of both procedures allows the achievement of the complete monobloc resection of the tumour with adequate margins 4 5.
The transfacial approach can excise more or less uninvolved portions of the normal facial skeleton, which may reveal functional and aesthetic morbidity.
In the last 20 years, Curioni et al. introduced and standardized the principle of “splitting face”, namely, resection of the affected bone only 6.
The nasal cheek flap technique (NCF) allows complete nasal swing thus obtaining a wide access to both the nasal fossae and the ethmoidal labyrinth 7.
Good exposure of the surgical field is obtained with this approach, thus allowing easy separation of the specimen and monobloc resection of the tumour.
Furthermore, this approach can also be used for the management of small intracranial tumours extended through the skull base to the nasal cavity, paranasal sinuses, upper and middle clivus (e.g. meningiomas, small clival chordomas, etc.) 8.
We have used the nasal cheek flap since 1992 with good aesthetic and functional results.
Aim of the present study was to analyse personal experience, focusing on complications, aesthetic results and self-evaluation expressed by the patients.
Material and methods
Between 1992 and 2002, 95 consecutive patients with nasal/ethmoidal or skull base tumours underwent surgical resection using NCF as part of the procedure.
Of these patients, 71 (57 male, 14 female, age range 41-69 years, mean 57), were diagnosed with nasal/ethmoidal malignant tumours, extending or not to the anterior cranial fossa (Fig. 1a, b) (Table I); 33 patients underwent anterior cranio-facial resection (ACFR), of whom 7 associated with orbital exenteration (ACFR/OE), 38 patients underwent ethmoidectomy and medial maxillectomy via the NCF only.
Fig. 1a.
CT scan of naso-sinusal tumour: axial image.
Fig. 1b.
CT scan of a naso-sinusal tumour: coronal image.
Table I. Characteristics of patients with malignant nasal/ethmoidal tumours.
| No. patients | 71 | |
| Age (yrs) | ||
| Range | 41-69 | |
| Mean | 57 | |
| Sex | ||
| Male | 57 | |
| Female | 14 | |
| Pathological condition | ||
| Adenocarcinoma | 49 | |
| Squamous cell carcinoma | 6 | |
| Adenoid cystic carcinoma | 8 | |
| Melanoma | 6 | |
| Estesioneuroblastoma | 2 | |
| Surgery | ||
| Anterior craniofacial resection | 26 | |
| Anterior craniofacial resection + | ||
| exenteratio orbitae | 7 | |
| Ethmoidectomy + medial maxillectomy | 38 | |
| External radiotherapy | ||
| Yes | 56 | |
| No | 15 | |
| Extent of invasion | ||
| Apex of the orbit | ||
| Yes | 7 | |
| No | 64 | |
| Dura | ||
| Yes | 8 | |
| No | 63 | |
| Brain | ||
| Yes | 4 | |
| No | 67 |
Another 14 patients underwent NCF for resection of large recurrences of inverted papilloma; 8 of these patients had previously been operated endoscopically and 6 via the external approach.
In 7 cases, the papilloma involved both nasal fossae, in 4 cases the nasal septum, and in 3 cases, histological examination of the specimen revealed malignant transformation.
Eleven patients were diagnosed with skull base tumours. Resection was performed via the NCF in 10 cases; in 1 case, the patient underwent anterior cranio-facial resection (olfactory groove meningioma).
The histological examination of specimens revealed 5 chordomas, 3 craniopharyngiomas, 3 meningiomas.
Of the 75 patients with malignancies, 57 (76%) were submitted to external post-operative radiotherapy.
Six patients affected by melanoma had chemotherapy with Dacarbazine.
A total of 38 patients with a malignant tumour, resected via the NCF approach only, underwent topical chemotherapy with 5-FU, according to Kneft’s protocol 9.
All patients underwent a meticulous endoscopic follow-up, including computed tomography (CT) scan or magnetic resonance imaging (MRI), when required (range 12 → 81 months).
Surgical technique
With the NCF technique, 3 skin incisions are made:
a lateral rhinotomy on the tumour side, which can be extended below to incise the nasal vestibule or the upper lip;
a glabellar incision;
a short contra-lateral incision reaching the medial chantus level (Fig. 1c).
Fig. 1c.
Nasal cheek flap: cutaneous incisions.
The osteotomic lines are then drawn and preplating is carried out using titanium mini-plates.
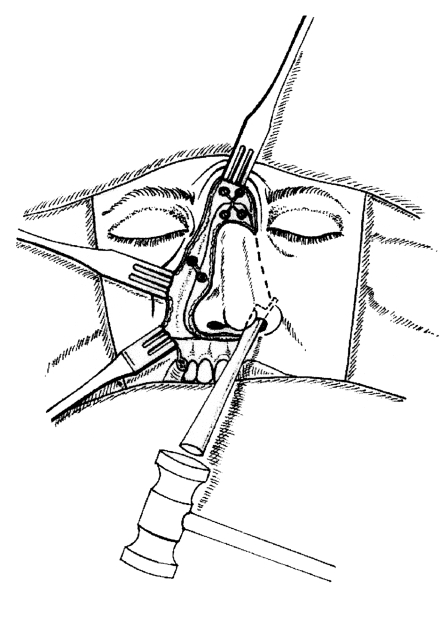
The osteotomies are performed using a sagittal saw on the lateral rhinotomy side and completed contralaterally with a rhinoplastic basal osteotomy (Silver’s osteotome) (Fig. 2).
Fig. 2.
Nasal cheek flap: osteotomic lines and pre-plat-ing.
The nasal septum is then sectioned with a straight osteotome or scissors, having previously cut the nasal mucosa underlying the osteotomies.
Caution is mandatory when performing these incisions in order to maintain a safe distance from the tumour margins.
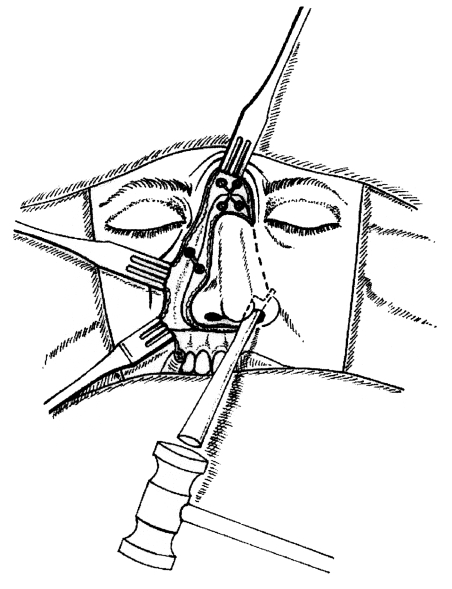
The nasal swing allows wide exposure of both the nasal fossae and ethmoidal labyrinth (Fig. 3).
Fig. 3.
Nasal cheek flap: nasal swing.
After tumour resection, the nose is repositioned and fixed with the miniplates.
The nasal cavity is then packed with a double balloon catheter and medicated strips of gauze.
Self-evaluation of aesthetic results
Patients were asked to complete a short validated questionnaire when attending for follow-up examination (range 6-24 months post-operatively).
The questionnaire focused on aesthetic and functional domains, with multiple choice answers (Table II).
Table II. Questionnaire on functional and aesthetic domains.
| You are kindly asked to indicate all the symptoms you had in the last seven days | ||||
| PN | VP | A | M | |
| a) Not liking one’s physical appearance | ||||
| b) Difficulty in physical contacts with family members and friends | ||||
| c) Difficulty in breathing through the nose | ||||
| d) Olfactory difficulties | ||||
| e) Testing difficulties | ||||
PN: nothing ; VP: a little; A: moderate; M: severe.
The questionnaire was analysed according to Aaronson et al. criteria 10.
Questions 1-2 and 3-4-5 were grouped on 2 scales evaluating the aesthetic and functional results, respectively. The total sum of the scores obtained was then divided by the number of items on the scale.
The results were recalculated on a 0-100 scale for better comprehension, with 100, the best result and 0 the worst.
Results
One patient who underwent ACFR died in the early post-operative period of myocardial infarction.
Actuarial cumulative survival for all patients with malignant tumour is 53.4% at follow-up 20 → 98 months.
In patients who underwent ACFR or ACFR/OE, the actuarial survival is 46.4%. Two patients with local recurrences are alive, one patient died of a second primary tumour (bladder cancer), 10 patients died of local recurrence of the disease and 2 died due to distant metastases. In patients who underwent ethmoidectomy and medial maxillectomy, the survival is 57.5%. Three patients are alive with disease (one with local recurrence, 2 with distant metastases); 2 patients died from other causes (myocardial infarction and colon cancer). 10 patients died of the disease, 6 of local recurrence, 4 of distant metastases (3 melanomas, 1 adenoidocystic cancer).
All patients suffering from inverted papilloma are still alive.
Complications included 3 cases of stenoses of the nasal vestibule (slight in 2 cases, closed in the other) and a widening of the nasal ala in 2 cases. A change in the orbital contour occurred in 2 patients and another patient developed dehiscence of the skin wound. Aesthetic results were not good in 3 of the patients with nasal pyramid cyphoscoliosis, being less evident in 2 patients and evident in the other.
Three patients had epiphora, intermittent in 2 cases, severe in the other. All 3 patients underwent dacryocystorhinostomy. One patient complained of transitory diplopia.
Of the 95 patients, 35 had massive nasal crusting, removal of which was necessary. This condition was more frequent in patients who underwent radiotherapy (24/56) (Table III).
Table III. Complications.
| 17/95 | |
| Death (myocardial infarction) | 1 |
| CSF leakage | 2 |
| Stenosis of nasal vestibule | 3 |
| Change in facial contour | 3 |
| Dehiscence of skin wound | 1 |
| transient dyplopia | 3 |
| Change in orbit contour | 2 |
| Widening of nasal ala | 2 |
| Massive nasal crusting | 35/95 |
| Non-irradiated patients | 11/39 |
| Irradiated patients | 24/56 |
Results emerging from the self-evaluation questionnaire revealed good aesthetic outcomes: 82.738 (range 0 → 100, SD 18.613), whereas questions regarding functional outcomes were less good, with a high standard deviation: 66.751 (range 0 → 100, SD 31.576) (Table IV).
Table IV. Self evaluation of aesthetic and functional outcomes.
| Scale A | |
| N. | 95 |
| Mean | 82.7381 |
| SD | 18.6139 |
| Min | 0 |
| Max | 100 |
| Scale B | |
| N. | 95 |
| Mean | 66.75 |
| SD | 31.57 |
| Min | 0 |
| Max | 100 |
A: Aesthetic scale
B: Functional scale
Discussion
Surgical resection is considered the main treatment for all tumours of the nasal cavity and paranasal sinuses since tumour extent plays a major role in the choice of surgical approach 11 12. In our opinion, the transfacial approach should always allow good exposure of the operating field. In fact, adequate exposure reduces the risk of unsatisfactory margins, especially when resection is performed only through the transfacial approach.
Furthermore, we consider it important to carry out resection attempting to spare the relatively uninvolved portions of the normal facial skeleton 13.
The NCF technique provides satisfactory surgical resection, thus avoiding aesthetic morbidity or disfigurement due to loss of skeleton support 14.
When carrying out the procedure, which must be meticulous and delicate, caution must be taken with the following points:
Anterior extension of the tumour: scrupulous assessment avoids cutting the bone too close to the tumour. Radiologic investigations (CT scan, MRI) and endoscopy are usually sufficient to define anterior advancement of the cancer, even if the tumour rarely reaches anterior structures. Only in one case was the tumour larger than expected, with an extension reaching the frontal sinus. The time elapsing (1 month) between the CT scan and surgical treatment, associated with high spread of the tumour, would account for this finding. Therefore, the operation had to be extended with craniofacial resection, including the nasal bones and the anterior part of the frontal bone.
Osteotomies should be performed using an ultrafine saw to reduce bone loss. We rarely use a fine Linderman burr.
Preplating allows easy and correct replacement of the nose. We normally perform preplating with the use of miniplates and screws (Leibingher mini series).
Surgical exposure obtained with the NCF is usually sufficient for resection of nasal/ethmoidal and small clival tumours (upper and medium clivus). We use the transfacial approach for tumours limited to the anterior ethmoid, not reaching the fovea ethmoidalis, the frontal sinus or the posterior part of the orbit. However, when the posterior ethmoid, frontal or sphenoidal sinuses, the orbital apex and, obviously, the lamina cribra are involved, ACFR is always performed. In order to better divide the specimen in the posterior ethmoid, we always excise the vertical lamina of the ethmoid even in tumours not reaching the midline. NCF offers excellent exposure and thus sectioning of the superior and middle turbinates is quite easy.
The lamina papiracea is easily resected mono- or bilaterally, depending upon tumour extension, as also the medial periorbit, when involved. On the other hand, if the tumour has invaded the apex of the orbit, thus reaching the optic nerve, we always perform a craniofacial resection with orbital exenteratio, resecting, intracranially, the optic nerve in the prechiasmatic area.
Tha naso-lacrymal duct is always excised and the sac marsupialised to the nasal mucosa in order to reduce post-operative epiphora.
The naso-maxillary muco-osteo-cutaneous flap has always been found to be very resistant even to radiotherapy. In all cases but one, we no longer experienced cutaneous dehiscence and necroses of the medial canthus; these were common when extensive resections of the nasal bones and upper process of the maxillary bone were carried out 15.
In one case presenting cancer recurrence in the lamina cribra following the transfacial approach, the NCF was raised combined with anterior craniofacial resection. The aesthetic result was equally good.
The technique offers excellent aesthetic outcomes, as shown in the present analysis. No scars are evident and good restoration of the facial contour is also achieved (Figs. 4– 6).
Fig. 4.
Nasal cheek flap: aesthetic outcome one year later (anterior view).
Fig. 6.
Nasal cheek flap: aesthetic outcome one year later (superior view).
When scarifying part of the nasal bone or the superior process of the maxilla, reconstruction can be guaranteed using a double plaque between the dorsum of the nose and the glabella (Fig. 7).
Fig. 7.
Nasal cheek flap: bad aesthetic outcome two years later.
On the other hand, with complete exenteratio of the upper part of the nasal cavity only satisfactory functional results are obtained.
Of the 67 patients submitted to surgery, only 14 had complications, 7 severe and 7 slight. In our opinion, this is a good percentage, bearing in mind the entity of the resection carried out.
Correct realignment of the bony segments and care to avoid excessive packing of the nasal cavity, which in one case caused widening of the nasal ala, greatly contribute to reducing complications.
We gently pack the cavity with ribbon gauze and a slightly inflated double balloon catheter.
The most frequent complication is crusting of the nasal cavity. This is often severe and causes a foul smell in the first post-operative year, especially in irradiated patients 15–19. Patients benefit from normal or hypertonic saline irrigations and moisturizing solutions. A well-humidified bedroom is also very useful. We invite these patients to have their naso-sinusal cavities cleaned monthly in the clinic, with the aid of endoscopy.
Crusts may also cause transient epiphora, which we encounter in approximately 8% of such patients, as crusts may plug the lacrimal sac even if it is marsupialized to the nasal mucosa.
Endoscopic follow-up is easily achieved, allowing early detection of recurrences and the possibility, when necessary, to commence topical chemotherapy with 5-FU.
Conclusions
The key principles of oncological cranio-maxillo-facial surgery are: performing monobloc resection with safe margins, avoiding major endocranical complications and obtaining good aesthetic results.
The “dismantling and reassembling” techniques have greatly contributed towards these aims.
In our experience, the NCF approach for nasal/ethmoidal and small clival tumours is easy to perform and easily extendible. We have achieved good aesthetic long-term results with few complications, both in limited and extended resections. Therefore, for these reasons, we systematically use this transfacial approach.
Fig. 5.
Nasal cheek flap: aesthetic outcome one year later (lateral view).
References
- 1.Karim AB, Kralendonk JH, Njo KH, Tabak JM, Elsenaar WH, van Balen AT. Ethmoid and upper nasal cavity carcinoma: treatment, results and complications. Radiother Oncol 1990;19:109-20. [DOI] [PubMed] [Google Scholar]
- 2.Mazzoni A, Pareschi R, Sanna M, Bagatella F, Curioni C, Clauser L, et al. Surgery of the base of the skull. Acta Otorhinolaryngol Ital 1989;9:225-59. [PubMed] [Google Scholar]
- 3.Schramm VL Jr, Myers EN, Maroon JC. Anterior skull base surgery for benign and malignant disease. Laryngoscope 1979;89:1071-91. [PubMed] [Google Scholar]
- 4.Lund VJ, Harrison DF. Craniofacial resection for tumors of the nasal cavity and paranasal sinuses. Am J Surg 1988;156:187-90. [DOI] [PubMed] [Google Scholar]
- 5.Cantù G, Solero CL, Mariani L, Mattavelli F, Pizzi N, Licitra L. A new classification for malignant tumors involving the anterior skull base. Arch Otolaryngol Head Neck Surg 1999;125:1252-7. [DOI] [PubMed] [Google Scholar]
- 6.Curioni C, Clauser L. The facial split in tumor surgery. Dismantling and reassembly of the face. In: Caronni EP, editor. Proceedings of the second International Congress of the International Society of Cranio-Maxillo-Facial Surgery Craniofacial Surgery. Bologna: Monduzzi; 1989. p. 223-5. [Google Scholar]
- 7.Curioni C, Clauser L, Squaquara R, Barasti P, Curri D. Craniofacial resections. Acta Otorhinolaryngol Ital 1990;10:27-48. [PubMed] [Google Scholar]
- 8.Hernandez Altemir F. Transfacial access to the retromaxillary area. J Max Fac Surg 1986;14:165-70. [DOI] [PubMed] [Google Scholar]
- 9.Knegt PP, de Jong PC, van Andel JG, de Boer MF, Eykenboom W, van der Schans E. Carcinoma of the paranasal sinuses: results of a prospective pilot study. Cancer 1985;56:57-62. [DOI] [PubMed] [Google Scholar]
- 10.Aaronson NK, Ahmedzai S, Bergman B, Bullinger M. The E.O.R.T.C. QLQ-C-30: A quality of life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85:365-76. [DOI] [PubMed] [Google Scholar]
- 11.Panje WR, Dohrmann GJ3rd, Pitcock JK, Scher N, Weichselbaum RR, Sutton HG Jr, et al. The transfacial approach for combined anterior craniofacial tumor ablation. Arch Otolaryngol Head Neck Surg 1989;115:301-7. [DOI] [PubMed] [Google Scholar]
- 12.Session RB, Larson DL. En bloc ethmoidectomy and medial maxillectomy. Arch Otolaryngol 1977;103:195-202. [DOI] [PubMed] [Google Scholar]
- 13.Wei WI, Lam KH, Sham JS. New approach to the nasopharynx: the maxillary swing approach. Head Neck 1991;13:200-7. [DOI] [PubMed] [Google Scholar]
- 14.Shah JP. Surgery of the anterior skull base for malignant tumors. Acta Otorhinolaryngol Belg 1999;53:191-4. [PubMed] [Google Scholar]
- 15.Sakai S, Kubo T, Mori N, Iton M, Myaguchi M, Kitaoku S, et al. A study of the late effects of radiotherapy and operation on patients with maxillary cancer. A survey more than 10 years after initial treatment. Cancer 1988;62:2114-7. [DOI] [PubMed] [Google Scholar]
- 16.Bagatella F, Mazzoni A. Microsurgery in juvenile nasopharyngeal angiofibroma: a latero-nasal approach with nasomaxillary pedicled flap. Skull Base Surg 1995;5:219-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Danesi G, Panizza B, Mazzoni A, Calabrese V. Anterior approaches in juvenile nasopharyngeal angiofibromas with intracranial extension. Otolaryngol Head Neck Surg 2000;122:277-83. [DOI] [PubMed] [Google Scholar]
- 18.Jian XC, Liu JP. A new surgical approach to extensive tumors in the pterygomaxillary fossa and the skull base. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:156-62. [DOI] [PubMed] [Google Scholar]
- 19.Clauser L, Vinci R, Curioni C. Dismantling and reassembling of the facial skeleton in tumor surgery of the cranio-maxillofacial area. History, surgical anatomy and notes of surgical techniques: Part 1. J Craniofac Surg 2000;11:318-25. [DOI] [PubMed] [Google Scholar]