The classification of salivary gland tumours is extremely complex, due to the morphologic heterogeneity of their anatomic structure and the occurrence of metaplastic changes.
The normal parotid gland is composed of several different cell types: acinar cells, myoepithelial cells, intercalated duct cells, striated duct cells. These cells can be distinguished on the basis of their structure and certain cytoplasmic and cell membrane features that can be detected only by electron microscopy (EM). Most of the parotid malignancies originate from, or differentiate toward, these cell lines. More-over, several histotypes are composed of two or more tumour cell lines showing different features that are present in varying amounts within the same neoplasm. The fact that some of these cells may undergo oncocytic, sebaceous, squamous and chondroid metaplasm results in an even more complex classification and can easily lead to misdiagnosis.
The main parotid cell types can be distinguished on the basis of the following ultrastructural features:
Acinar cells: the abundant cytoplasm contains numerous round membrane-bound structures of varying electron density and diameter (secretory granules); these are larger in mucous than in serous acinar cells and often fuse. Microvilli are also present on the luminal surface, together with intercellular junctions (tight and gap junctions and desmosomes) at sites along the lateral borders.
Myoepithelial cells: situated between the acinar and intercalated duct cells and the basal plasma membrane have a flattened, elongated shape. Myoepithelial cells usually present several cytoplasmic processes extending over the acinar and duct cells, and contain numerous microfilaments with focal densities, which are similar to those of smooth muscle cells.
Intercalated duct cells: featuring a normal rough endoplasmic reticulum, Golgi region and mitochondria, they interdigitate with adjacent cells.
Striated duct cells: the peculiar striations, characteristic of their cytoplasm at light microscopy, are due to extensive vertical folds in the basal plasma membrane of these tall columnar cells. Lateral junctional complexes and short luminal microvilli are detectable here, as well as in acinar cells.
Detecting the correct histotype, and making the right diagnosis, within such a complex classification is mandatory and not merely a stimulating exercise for the pathologist. Each tumour presents peculiar clinico-pathological and epidemiologic features, which should be taken into consideration when deciding both management and treatment. Histochemical and immunohistochemical methods, which usually offer a valid contribution, in the pathologic diagnosis, such as ancillary techniques, are of little use in the present situation. EM plays a pivotal, unique role since it offers the possibility to detect features that must be carefully sought in order to make the correct diagnosis.
The presence of micro-glandular spaces or intra-cytoplasmic lumina lined with short microvilli, undetectable at light microscopy, and often large extra-cellular spaces containing abundant proteoglycans and elastic fibres allows differential diagnosis between mixed tumour/pleomorphic adenoma and myoepithelioma. Pleomorphic adenoma is the most common neoplasm of the parotid gland and is composed of modified myoepithelial cells presenting both epithelial and mesenchymal differentiation; if only surgical removal is carried out, the recurrence rate is high. Myoepithelioma is usually a benign tumour of the myoepithelial cells, that may undergo malignant transformation.
Oncocytes or oxyphilic cells may occur in several organs, among which the salivary glands; in the parotid gland, these are large ductal cells with a deeply eosinophilic cytoplasm filled with mitochondria 1. The two major parotid tumour types, composed of oncocytes, are oncocytoma/oxyphilic adenoma and Warthin’s tumour/cystadenoma lymphomatosum papilliferum. These neoplasms have a different pathogenesis and biological behaviour; malignant transformation of oncocytoma is an extremely rare event, while it is more frequent in Warthin’s tumour. It can evolve into malignant lymphoma as well as into several types of carcinoma 2. Oncocytoma tumour cells have a granular eosinophilic cytoplasm, packed with mitochondria; some of these organelles contain large amounts of glycogen, and others are partitioned, suggesting division 3. These mitochondria carry atypical features, that sometimes undergo cystic dilatation resulting in clear cell change. Warthin’s tumour is composed of epithelial mitochondria-rich cells. The mitochondrial partitions commonly seen ultrastructurally, in oxyphilic adenoma, are usually absent here, and the organelles show no atypia; however, cup-shaped and concentric-ring forms of mitochondria can occur 4.
Mucoepidermoid carcinoma is the most common malignant epithelial tumour of the salivary glands. At light microscopy, four cell types can be identified: mucin-producing, squamous, intermediate and clear cells 5. Ultrastructural studies have led to a better understanding of the histogenesis of these neoplasms; according to some Authors, the cell population is actually composed of six types: differentiated stem cells, serous and mucoid secretory cells, mucus-producing goblet cells, epidermoid cells, and modified myoepithelial cells 6; further studies support a more simple classification based on two types of cells, luminal and intermediate 7.
Acinic cell carcinoma, which is less common than the former, features two basic cell types also at EM: the main epithelial cells, or acinar cells, which are similar to normal acinar cells (cytoplasm containing multiple membrane-bound granules, vacuoles and a few microvilli) 8 and clear cells, showing a dilated rough endoplasmic reticulum, lipid inclusions, intracytoplasmic pseudolumina, and variable amounts of glycogen.
Morphologically, a subcategory of “monomorphic adenoma” can be considered within the benign epithelial neoplasms, on the basis of the presence of one cell type, among which, there is the basal cell adenoma. At light microscopy, these tumours have a “basaloid” appearance with epithelial nests surrounded by palisading cells; the main differential diagnosis is with adenoid cystic carcinoma, a common parotid malignancy. EM studies suggest that basal cell adenoma is derived from the intercalated duct cells, with a minor involvement of myoepithelial cells 7. Adenoid cystic carcinoma is composed of cell types presenting combined features of intercalated duct cells, myoepithelial cells, secretory cells, and pluripotential reserve cells; pseudocysts, intercellular spaces, abundant basal lamina and true glandular lumina are also detectable. Ultrastructural studies have suggested a similar histogenesis to that of benign mixed tumours 8.
Besides epithelial tumours, which are the most common, malignant lymphoma accounts for a significant percentage of all parotid malignancies. They may derive from intra-parotid lymph nodes or in the gland itself, and can be classified, according to cell type, as: large cells (cleaved, non-cleaved, or immunoblastic) and small cells (small lymphocytic or small cleaved) or mixed. In all cases, neoplastic cells can be easily recognized as non-epithelial at EM due to lack of intercellular junctions and formation of microacini; nevertheless, diffuse large cell lymphoma is composed of lymphocytes with luminal microvilli similar to that expected in an adenocarcinoma. More-over, the presence of large nuclei, featuring prominent peripheral chromatin, is characteristic of lymphoid cells.
The parotid gland may be the site of other metastatic tumours, of which malignant melanoma is quite frequent 9. Diagnosis may be very difficult, at light microscopy, in the amelanotic forms, which may have the general appearance of “large cell” tumours; the presence of melanosomes, which are intra-cytoplas-mic vescicles containing electron dense melanic pigment, in different stages of maturation, allows correct diagnosis of melanoma to be made.
In this brief review, we have stressed that ultrastructural analyses allow a diagnostic hypothesis, based on histological and immuno-histochemical examinations to be confirmed. At times, EM may even reveal a totally unexpected histotype.
For instance, we recently examined the case of a 62-year-old male with a 1-year history of a mass located in the left parotid region. Macroscopic examination of the surgical specimen showed an oval soft greyish tumour, 2.8 cm in the maximum dimension. Light microscopy diagnosis, made on the basis of architectural and cytologic features of the tumour, was of acinar cell carcinoma with a microfollicular pattern. Ultrastructural examination showed the presence of true glandular lumina and pseudocysts, and a reduplication of the basal membrane surrounding the myoepithelail cells; these findings allowed us to finally make the correct diagnosis of tubular type adenoid cystic carcinoma.
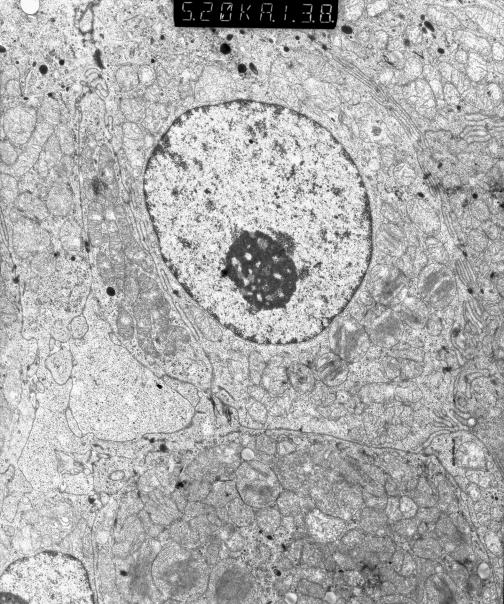
Fig. 1.
Typical oncocyte showing several enlarged mitochondria occupying more than 80% of entire cytoplasm. Nucleus is round, featuring huge nucleolus (orig. magn. 6600X).
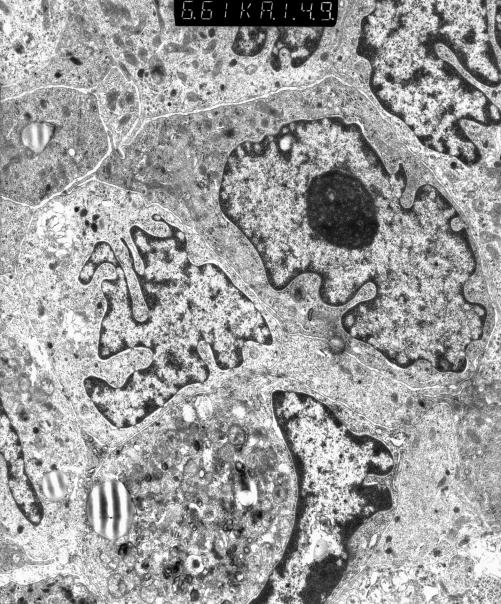
Fig. 2.
Melanoma: large nuclei with irregular profile; characteristic melanosomes and premelanosomes are present in cytoplasm (orig. magn. 5600X).
References
- 1.Chang A, Harawi SJ. Oncocytes, oncocytosis, and oncocytic tumors. Pathol Annu 1992;27:263-304. [PubMed] [Google Scholar]
- 2.Shikhani AH, Shikhani LT, Kuhajda FP, Allam CK. Warthin’s tumor associated neoplasms. Report of two cases and review of the literature. Ear Nose Throat J 1993;72:264-9. [PubMed] [Google Scholar]
- 3.Tandler B, Hutter RVP, Erlandson RA. Ultrastructure of oncocytoma of the parotid gland. Lab Invest 1970;23:567-80. [PubMed] [Google Scholar]
- 4.Kataoka R, Hyo Y, Hoshiya T, Miyahara H, Matsunaga T. Ultrastructural study of mitochondria in oncocytes. Ultrastruct Pathol 1991;15:231-9. [DOI] [PubMed] [Google Scholar]
- 5.Healey WV, Perzin KH, Smith L. Mucoepidermoid carcinoma of salivary gland origin. Classification, clinical-pathologic correlation, and results of treatment. Cancer 1970;26:368-88. [DOI] [PubMed] [Google Scholar]
- 6.Chaudhry AP, Cutler LS, Leifer C, Labay G, Satchidanand S, Yamane GM. Ultrastructural study of the histogenesis of salivary gland mucoepidermoid carcinoma. J Oral Pathol Med 1989;18:400-9. [DOI] [PubMed] [Google Scholar]
- 7.Dardick I, Kahn HJ, van Nostrand AWP, Baumal R. Salivary gland monomorphic adenoma. Ultrastructural, immunoperoxidase, and histogenetic aspects. Am J Pathol 1984;115:334-8. [PMC free article] [PubMed] [Google Scholar]
- 8.Gustafsson H, Carlsö B, Henriksson R. Ultrastructural morphometry and secretory behavior of acinic cell carcinoma. Cancer 1985;55:1706-10. [DOI] [PubMed] [Google Scholar]
- 9.Orenstein JM, Dardick I, van Nostrand AWP. Ultrastructural similarities of adenoid cystic carcinoma and pleomorphic adenoma. Histopathology 1985;9:623-38. [DOI] [PubMed] [Google Scholar]
- 10.Seifert G, Hennings K, Caselitz J. Metastatic tumors to the parotid and submandibular glands. Analysis and differential diagnosis of 108 cases. Pathol Res Pract 1986;181:684-92. [DOI] [PubMed] [Google Scholar]