Summary
The introduction, 15 years ago, of extracorporeal shock wave lithotripsy in the treatment of salivary gland calculi, has changed the therapeutic approach in these patients. Aim of this study was to evaluate the efficacy of lithotripsy in sialolithiasis, after 10 years follow-up. A review has been made of the literature to establish current opinions in diagnosis and treatment of sialolithiasis. The role of ultrasonography, radiography and, in particular, of sialo-magnetic resonance imaging in diagnosis of salivary lithiasis has been evaluated. The greater efficiency of the extracorporeal shock wave lithotripsy treatment for parotid, compared to submandibular calculi, has been demonstrated (57% versus 33%). In 68% of our patients, lithotripsy was resolutive after 10 years. Ultrasonograpy should be considered first choice examination in diagnosis of salivary calculi. Sialo-magnetic resonance imaging is a recent, non-invasive diagnostic procedure with the advantage of no radiation exposure, and with better definition of anatomical and functional state of glandular parenchyma and duct, compared to other available techniques.
Keywords: Salivary glands, Sialolithiasis, Diagnosis, Treatment, Sialo-MRI, Lithotripsy
Riassunto
L’introduzione, 15 anni fa, della litotrissia extracorporea con onde d’urto (ESWL) nella terapia della calcolosi salivare ha cambiato radicalmente l’approccio terapeutico di questi pazienti. L’obiettivo del nostro studio è stato quello di valutare l’efficacia terapeutica della litotrissia nei pazienti con scialolitiasi, tramite un follow-up a lungo termine (10 anni). È stata, inoltre, effettuata una revisione della letteratura con lo scopo di valutare le attuali conoscenze riguardanti la diagnosi e la terapia di questa patologia. È stato, poi, valutato il ruolo dell’ecografia, della radiografia ed in particolare della scialo-RM nella diagnosi di calcolosi salivare. La maggiore efficacia della litotrissia è stata riscontrata nella calcolosi della ghiandola parotide, rispetto alla ghiandola sottomandibolare (57% vs. 33%). La litotrissia extracorporea è stata risolutiva in 68% dei nostri pazienti, a 10 anni di distanza. L’ecografia si è confermata indagine di prima scelta nella diagnosi di calcolosi salivare. La scialo-RM è una metodica diagnostica non invasiva con il vantaggio di non esporre a radiazioni ionizzanti e che offre maggiori indicazioni anatomo-funzionali riguardo alle ghiandole salivari e al loro asse escretore, rispetto alle altre metodiche disponibili.
Introduction
The introduction, 15 years ago 1, of extracorporeal shock wave lithotripsy (ESWL) in the treatment of salivary gland calculi, has changed the therapeutic approach in these patients.
Salivary glands lithiasis (sialolithiasis) is the most common disease of the major salivary glands after mumps 2 and accounts for approximately 30% of all salivary disorders and about 0.01-1.0% of the population is held to be affected, with a higher incidence in males aged between 30 and 60 years 3–10. The most common localization is the submandibular gland where 92% of calculi are found, the duct being more frequently affected than the parenchyma. The parotid gland is affected in 6% of cases. The sublingual gland is affected in 2% of cases and other minor salivary glands in another 2% 2. Calculi generally consist of a mixture of different calcium phosphates (mainly hydroxy-apatite and carbonate-apatite) together with an organic matrix. The aetiologic factors involved in the sialolith formation can be classified into two different groups: on the one hand, saliva retention due to morpho-anatomic factors (salivary duct stenosis, salivary duct diverticuli, etc.), on the other, saliva composition factors (high supersaturation, crystallization inhibitor deficit, etc.) 3.
Until a few years ago, the treatment of salivary stones consisted in medical and surgical procedures.
The surgical procedure shows greater efficacy in the elimination of stones, compared to medical therapy (in most cases with poor results), but with not indifferent, post-operative, complications observed in some cases. The innovative (conservative) therapeutic methods consist in extra-corporeal lithotripsy, intra-cannular lithotripsy and interventional sialendoscopy.
After positive experience in the treatment of urinary and pancreatic calculi, extra-corporeal shock wave lithotripsy (ESWL) is proposed as an alternative therapeutic approach in the treatment of salivary stones in the early 90s.
The aim of this investigation was to evaluate the efficiency of ESWL, with long-term follow-up study (10 years), in patients submitted to ESWL treatment for sialo-lithiasis and also to determine the role of ultrasonography, radiography and, in particular, of sialo-magnetic resonance imaging (MRI) in the diagnosis of salivary stones.
Materials and methods
A total of 19 patients (11 male, 8 female) with salivary calculi (12 submandibular and 7 parotid), age range 14-70 years (mean 40), were observed at a distance of 10 years, after ESWL treatment.
ESWL was performed using a Minilith SL1 (Storz-Medical) with an electromagnetic shock wave source, equipped with a coaxial 7.5 MHz frequency ultrasound (US) transducer. Patients were treated in 4 sessions (20 minutes each), with 1200 impulses per session.
US with a high frequency (10-13 MHz) transducer was performed in all patients.
Moreover, patients underwent sialo-MRI, for which a one Tesla super conductive Tool, (Siemens Harmony), equipped with a Head coil, was used. The sialo-MRI examination consisted in two parts: first – the morphological part – acquired with 5 mm coaxial scan slices, a gap of 0.5 mm T1 and T2 weighted; second – the sialographic part – acquired with cholangiographic derivation sequences, opportunely modified and adapted, with a volumetric and multi-slice 2D acquisition, then 3D reconstructed.
Results
Data concerning site of salivary stones, results of lithotripsy and clinical evolution of our patients over a 10-year follow-up period, are outlined in Table I*. None of these patients reported any kind of complications during or after treatment.
Table I. Location of salivary calculi and follow-up over 10 years.
| ESWL | Submandibular gland 12 (63%) |
Parotid gland 7 (37%) |
Total 19 |
||
| Duct 10 (83%) |
Parenchyma 2 (17%) |
Duct 5 (71%) |
Parenchyma 2 (29%) |
||
| Complete disintegration | 3 (30%) | 1 (50%) | 3 (60%) | 1 (50%) | 8 (42%) |
| Partial fragmentation | 7 (70%) | 1 (50%) | 2 (40%) | 1 (50%) | 11 (58%) |
| 10-year follow-up: | |||||
| asymptomatic patients | 6 (60%) | 1 (50%) | 5 (100%) | 1 (50%) | 13 (68%) |
Note: (%)
None of the 13 patients (68%) presented further episodes of sialo-lithiasis during the 10-year follow-up period and continued being asymptomatic for 10 years after lithotripsy. The remaining 6 patients underwent different treatments: 2 continued sessions of lithotripsy in another hospital, 3 patients underwent an operation of marsupialization of Wharton’s duct, and 1 patient underwent sialectomy of the submandibular gland due to persistence of hilar calculus 1.5 cm in diameter.
Discussion
US with high frequency linear transducer (10-13 MHz) is first choice investigation for diagnosis of salivary stones. Submandibular and parotid calculi diagnosis can be readily performed with US, for almost all intra-parenchymal stones. US sensibility decreases for ductal and, in particular, for papillary stones. Finally, diagnosis of salivary calculi is correctly performed in > 90% of cases, with the 10-13 MHz US transducer 11. ESWL can be performed in all calculi visualized by US, since the exact location of the stone(s) can be determined during the ESWL session 12.
The two formal contraindications are pregnancy and failure of US detection of the stone 13. Before treatment, a radiographic examination can be performed, considering that stones are radio-opaque in > 80% of cases 11. In this study, we propose a sialo-MRI examination in the diagnostic workup of sialolithiasis. Sialo-MRI is a diagnostic, non-invasive, method recently introduced, with promising results, in the evaluation of salivary gland disease. This technique produces sialographic images but without contrast medium injection and without the disadvantage of ionizing radiation (CT and contrast sialography). An important advantage of sialo-MRI is the fact that the structural anatomy of the salivary glands remains unchanged with this technique, which allows an exact delimitation of the glandular acini and duct (Fig. 1). In US, the acini and ducts may be compressed by the US transducer, moreover, in sialography, the acini and ducts can be dilated by contrast medium injection 14. The Sialo-MRI study consists of two parts: i. anatomical – which also contributes to determine the relationship with adjacent structures thanks to its dimensional, morphological and structural examination of the parotid and submandibular gland (Fig. 3); and ii. sialographic – which shows only the ductal components and possible liquid areas taken by the slices, which improves after stimulation using citric acid. Moreover, sialo-MRI offers a simultaneous evaluation both of the parotid and submandibular glands. Finally, sialo-MRI allows acute, to be differentiated from chronic, inflammation, on the basis of the signal intensities, T2 weight in particular, since it is possible to perform this method even during acute inflammation 14. After citric acid stimulation, functional evaluation of the glandular parenchyma and duct is possible. Sialo-MRI is an instrumental technique to be performed also in combination with US and/or radiographic examinations due to the impossibility of visualizing the stones directly by sialo-MRI, these being hypointense both in T1 and T2 weights and, in particular, in the presence of small calculi (Fig. 2). Sialo-MRI can indirectly identify the presence of a stone by demonstrating proximal salivary duct dilatation. The major disadvantages of the sialo-MRI examination are the relatively long time required for the scanning examination (45 min), the high costs, lack of compliance in the claustrophobic patient and the presence of artefacts in patients with dental bridges or a metallic prosthesis 15.
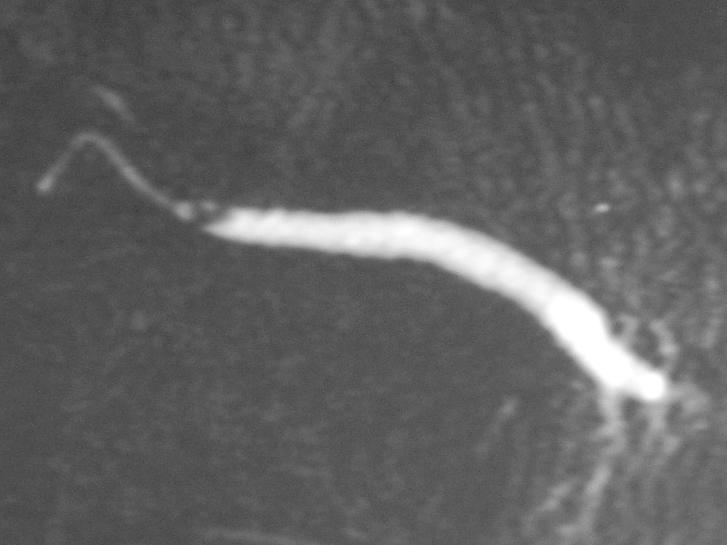
Fig. 1.
Sialo-MRI of parotid gland with evidence of two intraductal calculi.
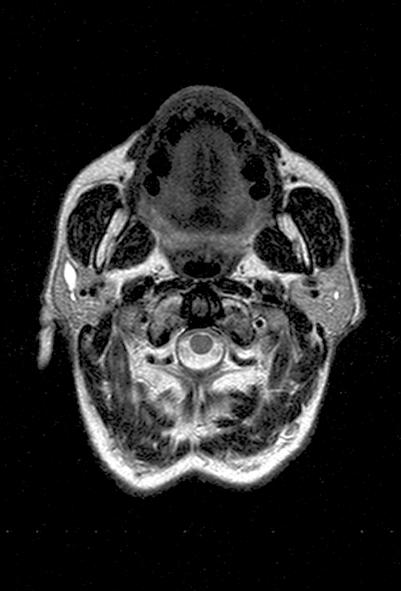
Fig. 3.
Axiall MRI of parotid gland with initial intraparenchymal dilatation of the duct.
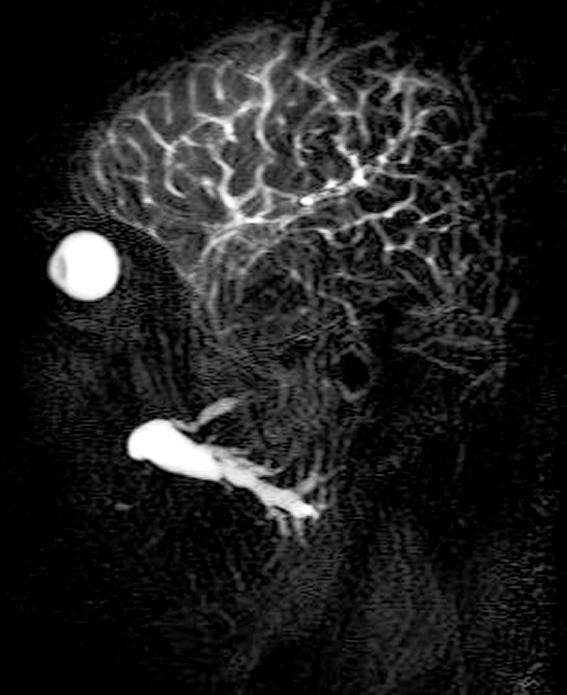
Fig. 2.
Sialo-MRI of parotid gland with remarkable dilatation of duct without evidence of calculi.
The aim of ESWL is to reduce the calculi into smaller fragments, the diameter of which does not block the flow of saliva and can be washed away. This is supported by the demonstration of a decrease in clinical symptoms, in both group of patients, with complete disintegration and partial fragmentation of the stones 12 16 17. Success of treatment depends on the dimension, location and number of stones. Our study confirms data in the literature 16 18 19 concerning the greater efficiency of ESWL for calculi localized in the parotid gland (57% vs. 33%). This could be explained, on the one hand, by easier positioning of the ESWL transducer and, on the other, by the prevalent serous composition of parotid gland secretion. The stones with a diameter > 10 mm are difficult to reduce in fragments with ESWL. Acute inflammation is the only local contraindication to the EWSL treatment. Even if chronic inflammation is not a contraindication for ESWL, decreased salivary flow may not permit the expulsion of the stone fragments following ESWL. Haemorrhagic diathesis, cardiological risk and patients with non-schermated pacemaker are general contraindications to the treatment 12.
Long-term follow-up studies are necessary to evaluate the efficacy of ESWL, as a conservative therapeutic approach. Escidier et al. 18, in 122 cases, observed that 68% of the patients were free of symptoms over the 3-year follow-up study. Capaccio et al. 17, in 322 cases with sialo-lithiasis reported 87.6% asymptomatic patients, over the 5 years following treatment. Results of the present study on 19 cases of sialo-lithiasis, demonstrate 68.5% asymptomatic patients after 10 years of follow-up.
Conclusions
ESWL is an effective, non-invasive treatment approach, to be performed in all patients with sialo-lithiasis, reserving surgery for recurrent or complicated salivary lithiasis. ESWL is particularly important when treating parotid gland calculi on account of its great efficacy in this site. Parotid gland stones should be treated with ESWL even when dealing with recurrent calculi due to the surgical risk in this area. It should be performed in the submandibular gland, as well as a first approach modality, except for calculi localized in the proximal part of Warton’s duct where the surgical approach (marsupialization) is preferable. In our study, ESWL was resolutive after a period of 10 years in 68% of cases. After 10 years, these patients were free of all kinds of symptoms related to sialo-lithiasis. Sialo-MRI proved to be a non-invasive diagnostic method without ionizing radiation exposure and with a higher definition of the glandular parenchyma and ductal system, compared to the other methods available.
References
- 1. Iro H, Nitsche N, Schneider TH, Ell C. Extracorporeal shockwave lithotripsy of salivary gland stones. Lancet 1989;2:115. [DOI] [PubMed] [Google Scholar]
- 2. El Deeb M, Holte N, Gorlin RJ. Submandibular salivary gland sialoliths perforated through the oral floor. Oral Surg Oral Med Oral Pathol 1981;51:134-9. [DOI] [PubMed] [Google Scholar]
- 3. Grases F, Santiago C, Simonet BM, Costa-Bauza A. Sialolithiasis: mechanism of calculi formation and etiologic factors. Clin Chim Acta 2003;334:131-6. [DOI] [PubMed] [Google Scholar]
- 4. Chu DW, Chow TL, Lim BH, Kwok SPY. Endoscopic management of submandibular sialolithiasis. Surg Endosc 2003;17:876-9. [DOI] [PubMed] [Google Scholar]
- 5. Austin T, Davis J, Chan T. Sialolithiasis of submandibular gland. J Emerg Med 2004;26:221-3. [DOI] [PubMed] [Google Scholar]
- 6. Antoniadis D, Mendonidou L, Papanayotou P, Trigonidis G. Clinical study of sialolithiasis. Findings from 100 cases. Hell Stomatol Chron 1989;33:245-51. [PubMed] [Google Scholar]
- 7. Laforgia PD, Favia GF, Chiaravalle N, Lacaita MG, Laforgia A. Clinico-statistical, morphologic and microstructural analysis of 400 cases of sialolithiasis. Minerva Stomatol 1989;38:1329-36. [PubMed] [Google Scholar]
- 8. Williams MF. Sialolithiasis. Otolaryngol Clin North Am 1999;32:819-34. [DOI] [PubMed] [Google Scholar]
- 9. Zenk J, Constantinidis J, Kydles S, Hornung J, Iro H. Clinical and diagnostic findings in sialolithiasis. HNO 1999;47:963-9. [DOI] [PubMed] [Google Scholar]
- 10. Koudelka BM. Surgical pathology of the salivary gland. Philadelphia: WB Saunders 1991. p. 26-38. [Google Scholar]
- 11. Gritzmann N. Sonography of the salivary glands. AJR 1989;153:161-6. [DOI] [PubMed] [Google Scholar]
- 12. Rubaltelli L, Stramare R, Candiani F, Bianco A, Andretta M. Extracorporeal shock-wave lithotripsy for salivary gland calculi: role of ultrasonography. Radiol Med 1996;92:274-8. [PubMed] [Google Scholar]
- 13. Aidan P, De Kerviler E, LeDuc A, Monteil JP. Treatment of salivary stones by extracorporeal lithotripsy. Am J Otolaryngol 1996;17:246-50. [DOI] [PubMed] [Google Scholar]
- 14. Huisman TA, Holzmann D, Nadal D. MRI of chronic recurrent parotitis in childhood. J Comput Assist Tomogr 2001;25:269-73. [DOI] [PubMed] [Google Scholar]
- 15. Becker M, Marchel F, Becker CD, Dulguerov P, Georgakopoulos G, Lehmann W, et al. Sialolithiasis and salivary duct stenosis: diagnostic accuracy of MR sialography with a three-dimensional extended conjugate-symmetry rapid spin-echo sequence. Radiology 2000;217:347-58. [DOI] [PubMed] [Google Scholar]
- 16. Kater W, Meyer WW, Wehrmann T, Hurst A, Buhne P, Schlick R. Efficacy, risks and limits of extracorporeal shock wave lithotripsy for salivary gland stones. J Endourol 1994;8:21-4. [DOI] [PubMed] [Google Scholar]
- 17. Ottaviani F, Capaccio P, Rivolta R, Cosmacini P, Pignataro L, Castagnone D. Salivary gland stones: US evaluation in shock wave lithotripsy. Radiology 1997;204:437-41. [DOI] [PubMed] [Google Scholar]
- 18. Schlick RW, Hessling KH, Djamilian MH. ESWL in patients suffering from sialolithiasis. Minim Invasive Ther 1993;2:129-33. [Google Scholar]
- 19. Escudier MP, Brown JE, Drage NA, McGurk M. Extracorporeal shockwave lithotripsy in the management of salivary calculi. Br J Surg 2003;90:482-5. [DOI] [PubMed] [Google Scholar]