Summary
Schwannoma arising from the cervical sympathetic chain is an uncommon benign nerve tumour. This tumour most often presents as an asymptomatic solitary neck mass, with slow-growing and rare malignant degeneration. Definitive pre-operative diagnosis may be difficult and investigations are not usually helpful. The carotid artery and internal jugular vein may be displaced anterior-laterally. Diagnosis relies on clinical suspicion and confirmation is often obtained by means of surgical pathology. Surgical excision is the treatment of choice for this tumour, with recurrence being rare. Horner’s syndrome is a common post-operative neurological consequence, but does not appear to cause problems to the patient. The case is described of a 42-year-old male who presented an asymptomatic left neck mass. Diagnostic studies included computed tomography, magnetic resonance imaging, and ultrasound which confirmed a circumscribed mass in the upper left portion of the neck next to the thyroid gland. The mass was excised through a transverse left cervical skin incision. Post-operatively the patient showed clinical findings of Horner’s syndrome. The pathologic and radiological evaluations, treatment and post-operative complications of this neoplasm are discussed.
Keywords: Cervical sympathetic chain, Schwannoma, Surgical treatment, Horner’s syndrome
Riassunto
Lo schwannoma derivante dalla catena del simpatico cervicale è un raro tumore benigno di origine nervosa. Questa neoformazione si presenta spesso come un’asintomatica massa solitaria del collo, con un accrescimento lento ed una rara degenerazione maligna. La diagnosi preoperatoria definitiva può essere difficoltosa e le indagini non sono usualmente dirimenti. L’arteria carotide e la vena giugulare interna possono essere lateralizzate. La diagnosi è legata al sospetto clinico e la conferma è spesso ottenuta in sede intraoperatoria. L’asportazione chirurgica è il trattamento di scelta di questo tumore, con recidive rare. La sindrome di Horner è la frequente complicanza neurologica post-operatoria, ma sembra non essere causa di problemi al paziente. Noi descriviamo un caso clinico di un paziente di 42 anni affetto da una massa asintomatica del collo a sinistra. Le indagini includevano una TAC, RMN ed ecografia del collo che confermavano la presenza della massa alla base del collo a sinistra lateralmente alla ghiandola tiroide. La neoformazione è stata escissa chirurgicamente attraverso un’incisione longitudinale della cute del collo a sinistra. Durante il decorso post-operatorio il paziente ha manifestato i segni clinici della sindrome di Horner. In questo articolo vengono discusse la valutazione clinica, radiologica, il trattamento e le complicanze post-operatorie di questa neoformazione.
Introduction
Schwannoma or neurilemmoma are benign neoplasms of Schwann cell origin. The Schwann cell surrounds peripheral nerve tissue and is believed to originate from the neural crest 1. They are typically solitary, well-encapsulated, benign tumours characteristically running along the course of a nerve or attached to peripheral, cranial, or sympathetic nerves. Malignant transformation is rare. In the parapharyngeal space, schwannomas may arise from the last four cranial nerves or the autonomic nerves, the vagus being the most common site. Cervical sympathetic chain schwannomas are uncommon 2–4 and most often appear as an asymptomatic, slow-growing, solitary neck mass; Horner’s syndrome is rarely apparent on physical examination 5. Pre-operative diagnosis may prove difficult, for evaluation of neurilemmoma, contrast-enhancing computed tomography (CT) or magnetic resonance imaging (MRI) and ultrasound (US) are the most appropriate, carotid angiography is not necessary. Post-operative ipsilateral Horner’s syndrome is to be expected following removal of the tumour, due to the necessary division of the cervical sympathetic chain, but this does not appear to have an adverse effect on the patient. Herein, a patient with sympathetic schwannoma arising from the cervical sympathetic chain is described.
Case report
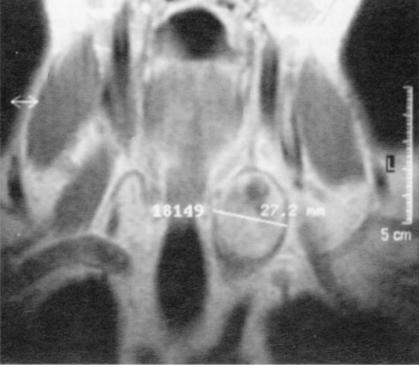
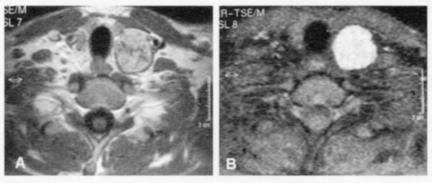
A 42-year-old Italian male presented with an asymptomatic left neck mass found on routine physical examination. The mass, measuring approximately 4.5 X 3 cm, was located below the upper portion of the sternocleidomastoid muscle. It was mobile, non-tender, and non-pulsing, with no associated bruit. The mass had been progressively increasing in size but was not associated with any other symptoms such as dysphonia, dysphagia, pain or weight loss; repeated US examination revealed that the mass had increased by 0.8 mm in 3 months. The patient denied smoking or consumption of alcohol. Diagnostic studies, including CT and MRI, confirmed a well-circumscribed mass in the left parapharyngeal space (Fig. 1), with anterior-lateral displacement of the common carotid artery and the internal jugular vein (Fig. 2). The mass extended from the base of the neck to the area of the thyroid gland. On MRI examination, the mass was slightly heterogeneous, with low signal intensity on T1 and high signal intensity on T2-weighted images and moderate enhancement postcontrast (Fig. 3). In addition to sympathetic schwannoma, the pre-operative differential diagnosis included vagal schwannoma, metastatic or reactive lymphoadenopathy, and paraganglioma. Fine-needle aspiration revealed spindle-shaped cells with irregular fusiform nuclei in a vague interwoven pattern. The mass was excised through a transverse left cervical skin incision. The tumour was found to originate from the cervical sympathetic chain and did not involve the vagus, hypoglossal, spinal, accessory, glossopharyngeal, or lingual nerves. It could not be resected without sacrificing a portion of the cervical sympathetic chain. Post-operatively, the patient showed mild left pupillary miosis with ptosis, enophthalmos (Fig. 4) and facial anhydrosis of the ipsilateral face.
Fig. 1.
Coronal MRI T1-weighted image reveals mass in left parapharyngeal space.
Fig. 2.
Axial post-contrast CT scan shows tumour in left parapharyngeal space. Mass displaces common carotid artery (closed arrow) and internal jugular vein (open arrow) in anterior-lateral direction, with medial compression of thyroid gland.
Fig. 3.
A) Post-contrast T1-weighted image demonstrates moderate enhancement of mass. B) T2-weighted image reveals high signal intensity of mass.
Fig. 4.
Ptosis resulting from Horner’s syndrome; NB ptosis of upper left eyelid and very mild “upside ptosis” of lower eyelid.
The presence of all these features was indicative of a preganglionic lesion. The post-operative course was uneventful and the patient was discharged on the fifth post-operative day. Histology showed the tumour to be a benign schwannoma originating within the cervical sympathetic chain.
Ocular examination showed that the best corrected visual acuity was 20/20 in each eye (-3.75 sph.). Intra-ocular pressure was normal. Bilateral fundus: myopic aspect. On Hertel exophathalmometry, the left eye showed an enophthalmos of 2 mm and a normal pupillary reaction with a bright diameter of the right eye 2.5 mm and 2 mm for the left. The marginal reflex distance (MRD1) was 5 mm in the right eye and 3 mm in the left. The elevator function was 16 mm in the right and 15 mm in the left. After one year, ophthalmologic symptoms were unchanged.
Discussion
A review of the literature disclosed fewer than 45 cases 3 6–8 of schwannoma sympathetic chain. This is a benign nerve sheath tumour that occurs along the length of the nerves. It is a solitary, slowly growing, tumour generally observed in patients between 20 and 50 years of age. Frequency is the same in both sexes and malignant change is rare 5.
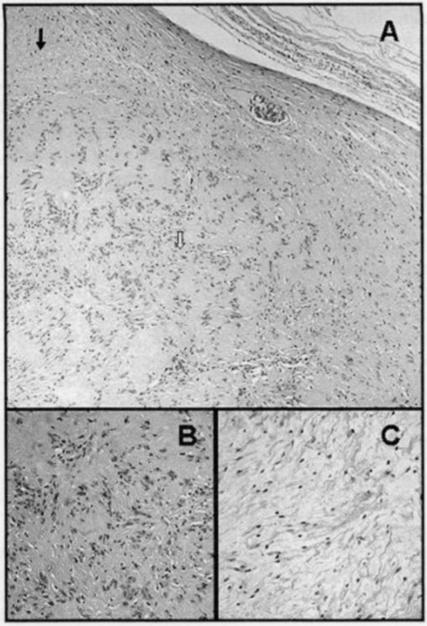
Microscopically, we found a fibrous capsule within the Antoni A and B areas. Antoni A regions are composed of more densely arranged cells with specific areas of palisanding nuclei arranged in rows; Antoni B regions tend to be more hypocellular, with a loose and disorderly arrangement (Fig. 5).
Fig. 5.
Histological appearance of sympathetic chain schwannoma. (Haematoxylin and eosin stain – orig. X100). A) Peripheral areas of Schwannoma with Antoni A region (closed arrow) and Antoni B region (open arrow). B) Detail of Antoni A region with dense arrangements of cells and palisanding nuclei (orig. X200). C) Detail of Antoni B region with loose organization and lower cell count (orig. X200).
Pre-operative diagnosis is difficult and further investigations are needed such as MRI, CT, US and angiography. The patient described here was examined by MRI, CT and US. Imaging studies are necessary in the diagnosis of head and neck schwannoma. The principal aim is to distinguish between a vagal or sympathetic schwannoma and a paraganglioma. On CT examination without contrast, a Schwannoma is generally hypodense compared to the muscle; with contrast, this lesion shows some degree of enhancement (Fig. 2). MRI reveals low signal intensity on T1 and high signal intensity on T2-weighted images (Fig. 3). Paraganglioma, on the other hand, is classically isodense when compared to muscle on pre-contrast CT, with more reliable homogeneous enhancement post-contrast 9. The post-gadolinium MRI sequences of paraganglioma show extremely bright contrast enhancement in a characteristic “salt-and-pepper” pattern, representing the low signal intensity of vascular flow voids which is not, however, pathognomic for paraganglioma, but may be found with hypervascular lesions 10. Usually, the origin of the paraganglioma is more cranial in the superior-medium latero-cervical neck region with respect to the schwannoma; the mass, in our patient, was situated at the base of the neck in the thyroid gland area. It may also be difficult to distinguish which is the nerve of origin of the schwannoma.
The tumour may arise from the neural structures of the parapharyngeal space, including cranial nerves IX, X, XI, and XII, but, in this case, the differential diagnosis was between a schwannoma of the vagus nerve and a schwannoma of the cervical sympathetic chain. Often the schwannoma of the vagus nerve grows between the common carotid artery and the internal jugular vein, causing a separation between the two vascular structures. In schwannoma of the cervical sympathetic chain, no separation is observed between the internal jugular vein and the common carotid artery (Fig. 2) 11. Fine-needle aspiration, which may be conclusive in many cases of neck masses, provides far less valuable information for the compact neural tumour. The most appropriate surgical excision of the parapharyngeal tumour is the external approach not only in order to gain control of the large vessels but also to avoid injury to other nerves in the area. In our patient, the mass could not be dissected from the sympathetic chain due to involvement with the nerve that would require resection of a segment of the sympathetic chain. Post-operatively, the patient developed complete Horner’s syndrome with facial anhydrosis of the ipsilateral face (Fig. 4).
Surprisingly, despite the clinical ophthalmologic findings, the patient did not present any adverse effects or complaints. The ptosis due to paralysis of Müller’s muscle can be repaired through slight advancement of the levator aponeurosis, or resection of the conjunctiva and Müller’s muscle 12 13. Horner’s syndrome is a common sequela of the schwannoma that originates from the section of the cervical sympathetic chain and should be discussed during pre-operative counselling. Since these tumours are very rare, the physician may not be familiar with the lesion and, indeed, have limited knowledge on the subject. Close follow-up is mandatory.
References
- 1.Wenig B. Atlas of head and neck pathology. Philadelphia: WB Saunders; 1993. p. 56-162. [Google Scholar]
- 2.Sheridan MF, Yim DWS. Cervical sympathetic schwannoma: a case report and review of the English literature. Otolaryngol Head Neck Surg 1997;117(Suppl):206-10. [DOI] [PubMed] [Google Scholar]
- 3.Leu YS, Chang KC. Extracranial head and neck schwannoma: a review of 8 years experience. Acta Otolaryngol 2002;122:435-7. [DOI] [PubMed] [Google Scholar]
- 4.Al-Ghamdi S, Black M, Lafond G. Extracranial head and neck schwannomas. J Otolaryngol 1992;21:186-8. [PubMed] [Google Scholar]
- 5.Ganesan S, Harar RPS, Owen RA, Dawkins RS, Prior AJ. Horner’s syndrome: a rare presentation of cervical sympathetic chain schwannoma. J Laryngol Otol 1997;111:493-5. [DOI] [PubMed] [Google Scholar]
- 6.Kara CO, Topuz B. Horner’s syndrome after excision of cervical sympathetic chain schwannoma. Clinical photograph. Otolaryngol Head Neck Surg 2002;127:127-8. [DOI] [PubMed] [Google Scholar]
- 7.Souza JW, William JT, Dalton ML. Schwannoma of the cervical sympathetic chain: it’s not a carotid body tumor. Am Surg 2000;66:52-5. [PubMed] [Google Scholar]
- 8.Hood RJ, Jensen ME, Reibel JF, Levine PA. Schwannoma of the cervical sympathetic chain, the Virginia experience. Ann Otol Rhinol Laryngol 2000;109:48-51. [DOI] [PubMed] [Google Scholar]
- 9.Silver AJ, Mawad ME, Hilal SK, Ascherl GF Jr, Chynn KY, Baredes S. Computed tomography of the carotid space and related cervical spaces (part II: neurogenic tumors). Radiology 1984;150:729-35. [DOI] [PubMed] [Google Scholar]
- 10.Lufkin RB, Hanafee WN. MRI of the head and neck. New York, NY: Raven Press; 1991. p. 150-1, 225. [Google Scholar]
- 11.Furukawa M, Furukawa MK, Katoh K, Tsukuda M. Differentiation between schwannoma of the vagus nerve and schwannoma of the cervical sympathetic chain by imaging diagnosis. Laryngoscope 1996;106:1548-52. [DOI] [PubMed] [Google Scholar]
- 12.Nerad JA. Oculoplastic surgery. The requisites in ophthalmology. St Louis, MO:Mosby ed. 2001;7:157-92. [Google Scholar]
- 13.Parmar DN, Lim N, Joshi N. Paravertebral primitive neuroectodermal tumour presenting with Horner’s syndrome. Br J Ophthal 2003;87:366-7. [DOI] [PMC free article] [PubMed] [Google Scholar]