Summary
Efficacy of the liberatory manoeuvre and of gradual otolitis dispersion technique, with or without associated drug therapy, have been compared. Included in this prospective study were 103 patients with benign paroxysmal positional vertigo seen in the Outpatient Department. Patients were classified into 4 groups according to treatment: Liberatory Manoeuvre according to methods described by Semont et al., with and without betahistine, Gradual Otolitis Dispersion Technique according to Brandt and Daroff, with and without betahistine. Evaluation was performed at baseline and at 3, 7, 14, 30, 60 and 90 days after start of treatment. Response to treatment was evaluated using criteria of Epley. At day 14, liberatory manoeuvre-betahistine and Brandt and Daroff-betahistine groups did significantly better than liberatory manoeuvre and Brandt and Daroff groups (p < 0.05). Improvement reached at day 30 was: 100% in liberatory manoeuvre-betahistine group; 96.30% (p > 0.05) in Brandt and Daroff-betahistine group; these results were significantly better (p < 0.05) than those of liberatory manoeuvre (54.17%) and Brandt and Daroff (25%) groups. As far as concerns differences between disease onset and start of therapy (less and more than 2 weeks), and age (≤ 60 years and ≥ 60 years), response to treatment was similar. In conclusion, both liberatory manoeuvre and Brandt and Daroff, when associated with betahistine, were significantly more effective than manoeuvres alone (p < 0.05). Improvement in liberatory manoeuvre-betahistine group, in the initial phase, was greater that in Brandt and Daroff-betahistine group, albeit, differences were not significant (p > 0.05). Age-related effects of manoeuvres were compared in 71 patients < 60 years and 32 patients ≥ 60 years, showing a similar improvement rate at the end of the investigation in both groups. In our opinion, liberatory manoeuvre and Brandt and Daroff associated with betahistamine produces faster recovery compared to liberatory manoeuvre and Brandt and Daroff alone. Nevertheless, 3 months after onset of treatment, all patients showed complete recovery due to spontaneous evolution of paroxysmal positional vertigo, in other words, treatment does not appear to influence the final improvement rate and its role should be accepted as a significant reduction in persistence of symptoms.
Keywords: Vestibular disorders, Benign Paroxysmal Positional Vertigo, Liberatory manoeuvre, Betahistine
Riassunto
Questo studio valuta l’efficacia della manovra liberatoria e della tecnica di dispersione graduale degli otoliti con e senza terapia medica associate. Si tratta di uno studio prospettico in cui sono stati inclusi 103 nuovi casi di Vertigine Parossitica Posizionale Benigna diagnosticati nel nostro Ambulatorio. I pazienti sono stati divisi in 4 gruppi in base al trattamento effettuato: Manovra Liberatoria di Semont, con e senza Betaistina, e Tecnica di Dispersione Graduale degli Otoliti di Brandt e Daroff, con e senza Betaistina. La valutazione è stata praticata prima di iniziare il trattamento e 3, 7, 14, 30, 60 e 90 giorni dopo il suo inizio. La risposta alla terapia è stata valutata secondo i criteri di Epley. Già 14 giorni dopo l’avvio del trattamento, i gruppi Manovra Liberatoria di Semont-Betaistina e Tecnica di Dispersione Graduale degli Otoliti di Brandt e Daroff-Betaistina hanno raggiunto risultati significativamente migliori rispetto ai gruppi Manovra Liberatoria di Semont e Tecnica di Dispersione Graduale degli Otoliti di Brandt e Daroff (p < 0,05). Un miglioramento del 100% è stato conseguito dal gruppo Manovra Liberatoria di Semont-Betaistina in 30 giorni; nello stesso periodo il miglioramento nel gruppo Tecnica di Dispersione Graduale degli Otoliti di Brandt e Daroff-Betaistina è stato del 96,30% (p > 0,05); questi risultati sono stati significativamente superiori (p < 0,05) a quelli conseguiti dai gruppi Manovra Liberatoria di Semont (54,17%) e Tecnica di Dispersione Graduale degli Otoliti di Brandt e Daroff (25%). La risposta al trattamento è stata simile indipendentemente dal tempo trascorso tra l’inizio della malattia e l’inizio della terapia (± 2 settimane) e indipendentemente dall’età (± 60 anni). Concludendo, entrambe le manovre (Manovra Liberatoria di Semont e Tecnica di Dispersione Graduale degli Otoliti di Brandt e Daroff) quando associate alla Betaistina sono state significativamente più efficaci rispetto alle rispettive manovre praticate da sole (p < 0,05). Il miglioramento nel gruppo Manovra Liberatoria di Semont-Betaistina nella fase iniziale è stato maggiore rispetto al gruppo Tecnica di Dispersione Graduale degli Otoliti di Brandt e Daroff-Betaistina, tuttavia la differenza non è stata significativa (p < 0,05). Gli effetti sulle manovre determinati dall’età sono stati valutati in 71 pazienti di età < 60 anni e 32 soggetti di ≥ 60 anni, con un tasso di miglioramento simile tra i 2 gruppi alla fine del periodo di studio. Noi pensiamo che la Manovra Liberatoria di Semont e la Tecnica di Dispersione Graduale degli Otoliti di Brandt e Daroff associate alla Betaistina producano un recupero più rapido rispetto alla Manovra Liberatoria di Semont e Tecnica di Dispersione Graduale degli Otoliti di Brandt e Daroff da sole. Tuttavia, 3 mesi dopo l’inizio del trattamento, tutti i pazienti hanno avuto un completo recupero in accordo alla spontanea evoluzione della vertigine parossistica posizionale benigna, in altre parole il trattamento non sembra influenzare il tasso finale di miglioramento ma il suo ruolo dovrebbe essere quello di ridurre il periodo di persistenza dei sintomi e quindi di accelerare la guarigione.
Introduction
Benign paroxysmal positional vertigo (BPPV) is the most common type of peripheral vertigo 1.
In this condition, a violent and short vertigo, associated with intense nystagmus, is induced by head movement.
BPPV was first described by Barany in 1921 2. In 1969, Shuknecht 3, proposed the pathophysiological mechanism of BPPV: heavy debris, probably detached from the macula of the utriculus, attaches to the cupula of the semicircular canal, making the ampulla sensitive to gravity. In another hypothesis 4 (Canalolithiasis), the otolitis are free to move in the endolymph and, when the head is moved in the provoking position, the viscosity induces an endolymph current that, in turn, induces vertigo and nystagmus. The cause of BPPV is usually idiopathic, it is seldom caused by head trauma, labyrinthitis, stapes surgery, or chronic otitis media.
BPPV is usually a self-limiting disorder, but spontaneous remission can occur over a period ranging from a few days to several months.
In the last 30 years, several forms of physical treatment have been developed to cure BPPV, all of which aimed at dispersing debris in the canal, detaching it from the cupula (if the pathophysiological mechanism is the cupulolithiasis) or removing it from the canal (if canalolithiasis is the cause) 5 6.
Aim of this study is to verify the effectiveness of the Liberatory Manoeuvre (LM), as reported by Semont et al. 7, and of the Gradual Otolitis Dispersion Technique (BD), according to Brandt and Daroff 8.
Both manoeuvres have been evaluated with/without associated medical treatment. Few studies 9 have compared these procedures, associated or not, with medical treatment.
We used Betahistine (N-a-methyl-2-pyridylethylamine) (BE), a histamine-like substance which was introduced in the treatment of vascular and vasomotor disorders 10 and later used in the treatment of vertigo, motion sickness and various peripheral and central vestibular disorders 9 11 12.
The mechanism of action in BE is based on its interaction with histamine receptors. Histamine has been shown to play a significant role in sensory coding, in the vestibular periphery. Histamine was found to increase the spike discharge of the afferent neurons of semicircular canal, in the frog 13. Pharmacological evidence indicates that H1, H2 and H3 histamine receptors exist in the vestibular periphery 14 15 and that histamine modifies the intracellular Ca2+ through action on these receptors 16 17. At vestibular nuclei level, BE significantly reduces the excitation caused by histamine and, at the semicircular canal, BE decreases the spike discharge of the ampullar hair cells 18 19. It has been suggested that BE actions are due to an improvement in the microcirculation of the labyrinth 12 20 and a reduction in endolymphatic pressure 21.
Material and methods
A total of 103 outpatients with BPPV of the posterior semicircular canal (PSC), seen in our department between January 2002 and December 2003, have been included in this study. We have not used patients with spontaneous recovery, as controls, since this would give rise to an ethical problem.
The diagnosis of BPPV was based on the following criteria:
symptoms compatible with BPPV (episodes of transient attacks of rotational vertigo induced by sudden head movements without auditory symptoms);
positional vertigo and positional nystagmus provoked by Dix and Hallpike manoeuvre 22 (the nystagmus was of the rotatory type and appeared after a short latency towards the lower ear, in the lateral head position; it ended after approximately 30 seconds and decreased when the positioning test was repeated).
Exclusion criteria were: diseases of central origin, terminal disease, medical or surgical conditions which could interfere with the pharmacokinetics of the drug used in the study, concomitant therapy with anti-vertigo drugs, drugs that act on cerebral circulation (antihistamines, calcium antagonists, anti-aggregants, thiazide diuretics, corticosteroids and benzodiazepines) or concomitant physical treatment of BPPV.
The patients were divided into four groups according to treatment: 1. LM only (LM), 2. LM with BE (LM-BE), 3. BD (BD), 4. BD and BE (BD-BE). Each method was selected at the patient’s first visit in the above-mentioned order. All patients gave their written informed consent before being enrolled in the study.
In the LM-BE and BD-BE groups, betahistine mesylate was administered at a dose of 16 mg twice daily, at 8 a.m. and 8 p.m. after meals, until complete recovery.
LM was performed according to the methods described by Semont et al. 7: the patient was seated, with legs outside the examining table and the head turned horizontally 45° to the unaffected ear. The patients then quickly laid down, on the side of the affected ear, and this position was maintained for a few minutes after disappearance of the nystagmus.
From this critical position, he/she was rapidly turned on the opposite side, maintaining the head rotated. This position was also maintained for a few minutes. Finally, the patient was very slowly sat up, this manoeuvre being performed by the physician or the therapist, at the hospital.
BD was performed according to the methods described by Brandt and Daroff 8: the patient, in the same position as LM, the head straight forward, rapidly reclined to the affected side and held this position for 30 seconds after disappearance of the vertigo. The patient then quickly sat up and maintained the position for 30 seconds. Finally, he/she reclined rapidly on the other side, held the position for 30 seconds, and then sat up again. The complete cycle had to be repeated until disappearance of the vertigo. The exercise was performed, at home, three times daily for several days until vertigo disappeared for two consecutive days. A relative verified the performance of the exercises.
Evaluation was carried out: at baseline and at 3, 7, 14, 30, 60 and 90 days after the beginning of treatment. If the patient continued to have symptoms or nystagmus, the same manoeuvre was performed again.
The response to treatment was evaluated using the criteria of Epley 23:
disappeared: all vertigo and nystagmus disappeared;
improved: BPPV and nystagmus disappeared, but non-positional dizziness was still present;
partially resolved: vertigo and nystagmus improved significantly but persisted;
unchanged.
Statistical analysis was performed using the ANOVA, χ2 test and Student t test; for the statistic reliability a value of p < 0.05 was chosen.
Results
Patient characteristics are outlined in Table I. All effectiveness variables were homogeneous between treatments, at baseline.
Table I. Characteristics of the patients at baseline.
| LM | LM-BE | BD | BD-BE | P* | |
| N. patients | 24 | 28 | 24 | 27 | NS |
| Sex (% male) | 33.3 | 35.7 | 37.5 | 33.3 | NS |
| Age (years) | |||||
| Mean ± SE | 51.6 ± 10.6 | 48.6 ± 9.7 | 49.6 ± 11.4 | 50.5 ± 9.1 | NS |
| Youngest | 22 | 20 | 19 | 21 | |
| Oldest | 73 | 71 | 72 | 70 | |
| Pre-treatment period (days) | |||||
| Mean ± SE | 15.4 ± 9.3 | 13.1 ± 6.2 | 14.6 ± 9.9 | 12.9 ± 9.8 | NS |
| Minimum | 2 | 0 | 2 | 0 | |
| Maximum | 30 | 24 | 38 | 30 | |
| Smokers | 7 | 9 | 6 | 8 | NS |
| Arterial blood pressure (mm Hg) | |||||
| Systolic | 120.8 ± 5.9 | 121.1 ± 7.1 | 119.8 ± 6.5 | 121.7 ± 6.5 | NS |
| Diastolic | 78 ± 4 | 78.8 ± 4.2 | 79.7 ± 1.6 | 79.5 ± 1.6 | NS |
Comparison between the four groups.
NS = not significant; LM = Liberatory Manoeuvre; LM-BE = Liberatory Manoeuvre with Betahistine; BD = Gradual Otolitis Dispersion Technique according to Brandt and Daroff; BD-BE = Brandt and Daroff Technique with Betahistine.
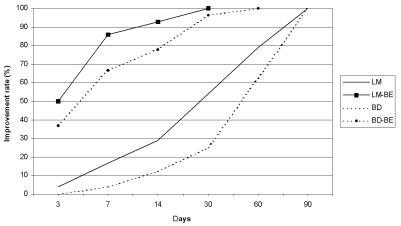
The rate of improvement, including disappeared and improved, according to the criteria of Epley, during the investigation period, is shown in Figure 1.
Fourteen days after start of treatment, the LM-BE and the BD-BE groups did significantly better than the LM and BD groups (92.86% and 77.78% vs. 29.17% and 12.5%, respectively, p < 0.05).
The LM technique (with and without BE) showed better results than BD (with and without BE), however, no significant difference was found (p > 0.05).
While a 100% improvement rate was reached in all our patients, the time in which it was achieved was significantly shorter in those in whom BE was associated with the physical treatment (LM or BD). The improvement rate, at 30 days, was: 100% in the LM-BE group, 96.30% (p > 0.05) in the BD-BE group, being significantly better (p < 0.05) than in LM (54.17%) and BD (25%) groups.
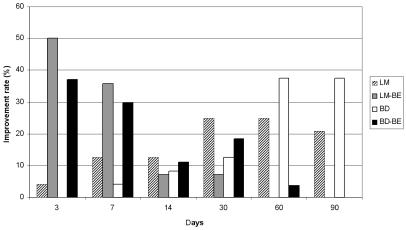
LM-BE and BD-BE groups showed a faster recovery in the first week, with a maximum improvement peak on the third day (50% and 37%, respectively) (Fig. 2). In the LM and BD groups, the best results were reached starting from the thirtieth day.
Fig. 2.
Improvement rate at each evaluation period.
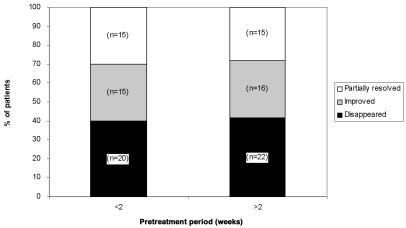
The treatment results, for all the patients, were compared according to the time period elapsing between disease onset and start of treatment (less or more than 2 weeks). We found that the response to treatment, in each subgroup, was comparable (Fig. 3).
Fig. 3.
Relationship between treatment results and pre-treatment period. Effects are shown according to intervals between disease onset and start of treatment.
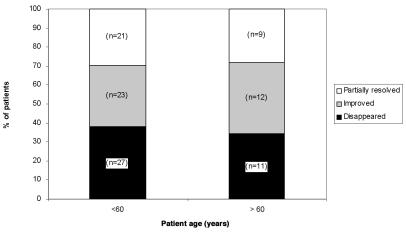
Patients were classified into two subgroups: ≤ 60 years and ≥ 60 years. The response to treatment in each subgroup was comparable (Fig. 4).
Fig. 4.
Relationship between treatment results and age.
Discussion and conclusions
In our study, in the long period (3 months), both groups (LM and BD) recovered completely, albeit the 100% improvement rate was achieved more rapidly in the LM group compared to the BD group (in 30 days 54.17% vs. 25%) (Fig. 1).
Fig. 1.
Accumulative improvement rate during investigation period.
The exercise therapy, reported by Brandt and Daroff, is considered vestibular habituation therapy since the hydrodynamics of endolymph are not taken into account.
LM, unlike the BD, is a liberatory manoeuvre: rapid movements in the PSC plane could detach debris adhering to the cupula and this would allow complete recovery in a shorter time.
Both manoeuvres (LM and BD) associated with BE were significantly more effective than the manoeuvres alone (p < 0.05) (Fig. 1). Furthermore, as in the LM and BD groups, the improvement rate in the LM-BE group, in the initial phase (7 and 14 days), was greater compared to that in the BD-BE group; however, these differences were not significant (p > 0.05). Thirty days after the onset of treatment, results were almost comparabe in the two groups.
Comparison between the LM and BD technique is shown in Table II; the BD technique is quite feasible by the patient at home and does not require either identification of the pathological side or detection of the liberatory nystagmus.
Table II. Comparison between LM e BD.
| LM | BD | |
| Technique | Sometimes difficult | Easy |
| Liberatory nystagmus | Mark of correct execution | Not necessary |
| Pathological side identification | Necessary | Not necessary |
LM = Liberatory Manoeuvre; BD = Gradual Otolitis Dispersion Technique according to Brandt and Daroff
Since the BD-BE improvement rate is almost the same as that of LM, we prefer the former in patients not living close to the hospital, since LM should be carried out exclusively in the Outpatient Department.
In our study, we also evaluated the time elapsing between disease onset and start of therapy. For a period of less or more than 2 weeks, the improvement rate, at the end of the investigation, showed no differences, as reported by other Authors 24 25. This suggests that it is better to start the rehabilitative treatment when the patient agrees to do so, considering the stress of the therapy.
The age-related effects of manoeuvres were compared in 71 patients < 60 years and in 32 patients ≥ 60 years, showing a similar improvement rate at the end of the investigation. in both groups (Fig. 4). It is difficult to offer an explanation for this result since, in older patients, the improvement in vestibular disease is expected to decrease with increasing age 26. This implies that vestibular manoeuvres (LM and BD) are also indicated in older patients with vertigo.
In conclusion, LM and BD associated with BE, in our opinion, produces faster recovery in comparison with LM and BD alone.
Nevertheless, three months after the onset of the treatment, all the patients showed complete recovery which is definitely due to the spontaneous evolution of BPPV, in other words, the treatment does not seem to influence the final improvement rate and its role should be seen as a significant reduction in the persistence of symptoms.
References
- 1.Baloh RW. The dizzy patient. Postgrad Med 1999;105:161-4. [DOI] [PubMed] [Google Scholar]
- 2.Barany R. Diagnose von Krankheitserscheinungen im bereische des Otolithenapparates. Acta Otolaryngol 1921;2:434-7. [Google Scholar]
- 3.Schuknecht HF. Cupulolithiasis. Arch Otolaryngol 1969;90:765-78. [DOI] [PubMed] [Google Scholar]
- 4.Hall SF, Ruby RRF, McClure JA. The mechanism of benign paroxysmal vertigo. J Otolaryngol 1979;8:151-8. [PubMed] [Google Scholar]
- 5.Brandt T, Steddin S, Daroff RB. Therapy for benign paroxysmal positioning vertigo, revisited. Neurology 1994:44:796-800. [DOI] [PubMed] [Google Scholar]
- 6.Epley JM. Positional vertigo related to semicircular canalolithiasis. Otolaryngol Head Neck Surg 1995;112:154-61. [DOI] [PubMed] [Google Scholar]
- 7.Semont A, Freyss G, Vitte E. Curing the BPPV with a liberatory maneuver. Adv Otorhinolaryngol 1988;42:290-3. [DOI] [PubMed] [Google Scholar]
- 8.Brandt T, Daroff RB. Physical therapy for benign paroxysmal positional vertigo. Arch Otolaryngol 1980;106:484-5. [DOI] [PubMed] [Google Scholar]
- 9.Itaya T, Yamamoto E, Kitano H, Yazawa Y, Kitajima K. Comparison of effectiveness of maneuvers and medication in the treatment of benign paroxysmal positional vertigo. ORL 1997;59:155-8. [DOI] [PubMed] [Google Scholar]
- 10.Horton BT, von Leden H. Clinical use of beta-2-pyridiyl-alkylamines. Mayo Clinic Proc 1962;37:692-702. [PubMed] [Google Scholar]
- 11.Gordon CR, Shupak A. Prevention and treatment of motion sickness in children. CNS Drugs 1999;12:369-81. [Google Scholar]
- 12.Lamm K, Arnold W. The effect of blood flow promoting drugs on cochlear blood flow, perilymphatic pO2 and auditory function in the normal and noise-damaged hypoxic and ischemic guinea pig inner ear. Hearing Res 2000;141:199-219. [DOI] [PubMed] [Google Scholar]
- 13.Valli P. Betahistine reduces the resting firing rate of vestibular receptors in the frog. Acta Otolaryngol (Stockh) 2000;544(Suppl):8-10. [DOI] [PubMed] [Google Scholar]
- 14.Housley GD, Norris CH, Guth PS. Histamine and related substances influence neurotransmission in the semicircular canal. Hearing Res 1988;25:87-98. [DOI] [PubMed] [Google Scholar]
- 15.Tomoda K, Motoki N, Harada N, Iwai H, Yamashita T. Effect of histamine on intracellular Ca2+ concentration in guinea pig isolated vestibular hair cells. Acta Otolaryngol 1997;528:37-40. [PubMed] [Google Scholar]
- 16.Arrang JM, Garbarg M, Quach TT, Dam Trung Tong M, Yeramian E, Schwartz JC. Action of betahistine at histamine receptors in the brain. Europ J Pharmacol 1985;111:73-84. [DOI] [PubMed] [Google Scholar]
- 17.van Cauweberge PB, de Moor SEG. Physiopathology of H3 receptors and pharmacology of betahistine. Acta Otolaryngol 1997;526(Suppl):43-6. [DOI] [PubMed] [Google Scholar]
- 18.Lacour M, Sterkers O. Histamine and betahistine in treatment of vertigo. Elucidation of mechanisms of action. CNS Drugs 2001;15:853-70. [DOI] [PubMed] [Google Scholar]
- 19.Dutia MB. Betahistine, vestibular function and compensation: in vitro studies of vestibular function and plasticity. Acta Otolaryngol (Stockh) 2000;544(Suppl):11-4. [DOI] [PubMed] [Google Scholar]
- 20.Laurikainen E, Miller JF, Rachel JD, Quirk WS. Betahistine effects on cochlear blood flow: from the laboratory to the clinic. Acta Otolaryngol (Stockh) 2000;544(Suppl):5-7. [DOI] [PubMed] [Google Scholar]
- 21.Martinez DM. The effect of Serc (betahistine hydrochloride) on the circulation of the inner ear in experimental animals. Acta Otolaryngol 1972;305(Suppl):29-47. [DOI] [PubMed] [Google Scholar]
- 22.Dix MR, Hallpike CS. The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Ann Otol Rhinol Laryngol 1952;6:987-1016. [DOI] [PubMed] [Google Scholar]
- 23.Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg 1992;107:399-404. [DOI] [PubMed] [Google Scholar]
- 24.Fujino A, Tokumasu K, Yosio S, Naganuma H, Yoneda S, Nakamura K. Vestibular training for benign paroxysmal positional vertigo. Arch Otolaryngol Head Neck Surg 1994;120:497-504. [DOI] [PubMed] [Google Scholar]
- 25.Norre ME, Deweedt WD. Treatment of vertigo based on habituation. J Laryngol Otol 1980;94:971-7. [DOI] [PubMed] [Google Scholar]
- 26.Shitara T. Age-related changes in the otorhinolaryngological field. Tokyo: Seiki Shuppansha; 1980. p. 105-6. [Google Scholar]