Summary
Grisel’s syndrome, defined as subluxation of the atlanto-axial joint, not associated with trauma or bone disease, is found primarily in children. There are few references to this syndrome in the ENT literature but it may occur in association with any condition that results in hyperaemia and pathological relaxation of the transverse ligament of the atlanto-axial joint. Several common otolaryngeal conditions have been associated with the syndrome: pharyngitis, adenotonsillitis, tonsillar abscess, cervical abscess, and otitis media. Moreover, the syndrome has been observed after numerous otolaryngologic procedures such as tonsillectomy, adenoidectomy and mastoidectomy. Non-traumatic subluxation of the atlanto-axial joint should be suspected in cases of persistent neck pain and stiffness. X-rays and computed tomography scans of the cervical spine can confirm the diagnosis. Early management, consisting of cervical immobilization and medical treatment, is considered the key factor for a satisfactory outcome. Inappropriate treatment may result in a permanent and painful neck deformity that may even require surgical fusion. Neurological complications have been reported in the literature, with outcome ranging from mild paresthesia, clonus, to quadriplegia or acute respiratory failure and death. The case is described of an 8-year-old boy who developed Grisel’s syndrome following adenoidectomy. The pathogenesis, classification, diagnosis, and treatment of this condition are discussed.
Keywords: Adenoidectomy, Complications, Grisel’s Syndrome, Atlanto-axial subluxation, Persistent torcicollis
Riassunto
La sindrome di Grisel, definita come sublussazione dell’articolazione atlanto-assiale non associata a trauma o malattia delle ossa, è un’affezione principalmente dei bambini. Non osservata frequentemente nella letteratura otorinolaringoiatrica, questa si può verificare in associazione con qualsiasi condizione che induca iperemia e rilassamento patologico del legamento trasverso dell’articolazione atlanto-assiale. Molte entità comuni otorinolaringoiatriche sono state associate alla sindrome: faringite, adenotonsillite, ascesso tonsillare, ascesso cervicale ed otite media. Inoltre la sindrome si può verificare dopo alcune procedure otorinolaringoiatriche come la tonsillectomia, adenoidectomia e mastoidectomia. La sublussazione atlanto-assiale dovrebbe essere sospettata nei casi di dolore persistente al collo e rigidità. Radiografie e tomografie assiali computerizzate della colonna cervicale stabiliscono la diagnosi. Il trattamento precoce, che consiste in una immobilizzazione cervicale e trattamento medico, viene considerato il fattore chiave per ottenere una guarigione adeguata. Casi trattati inappropriatamente possono manifestarsi con una fissità e deformità dolorosa del collo, tali da poter richiedere una riduzione chirurgica. Nella letteratura sono state riportate complicanze neurologiche, con disturbi che variano da una modesta parestesia, a cloni, a tetraplegia fino ad una insufficienza respiratoria acuta e morte. Noi descriviamo un caso di sindrome di Grisel occorso in un bambino sottoposto ad adenoidectomia. In questo articolo vengono discusse la patogenesi, la classificazione, la diagnosi ed il trattamento di questa condizione.
Introduction
Spontaneous subluxation of the atlanto-axial joint following peri-pharyngeal inflammation is known as Grisel’s syndrome, although it was first described by Sir Charles Bell 1, in 1830. Bell reported a case of death from atlanto-axial subluxation which resulted in spinal cord compression in a patient with a syphilitic ulceration of the pharynx. The eponymous name originated from the French physician Grisel, who described two cases in 1930 2. Children are most frequently affected and classically have torcicollis associated with neck stiffness or pain upon neck movement. Torcicollis may occur spontaneously shortly after the onset of pharyngitis or it may follow mild trauma to the neck. The syndrome has been reported in association with rhinopharyngitis 3 4, cervical osteomyelitis 5, rheumatic conditions, and following surgical procedures such as tonsillectomy or adenoidectomy 6 7, choanal atresia repair, and mastoidectomy. There is no sex predominance, and patients affected are usually between ages 5-12 years 8. However, the condition has also been reported in patients ranging from infancy to the seventh decade of life 8. Distension and abnormal laxity of the ligaments surrounding the atlanto-axial articulation result from direct spread of inflammation from the pharynx and nasopharynx and can result in cervical spine instability with devastating neurological sequelae. Less than 15% of patients have neurological signs or symptoms, with extreme consequences including quadriplegia and sudden death.
Herein, a case is described of persistent torcicollis following adenoidectomy. The aetiology, classification, pathogenesis of post-operative muscle spasm and atlanto-axial subluxation are briefly discussed. The clinical management and prognosis of this patient is also evaluated.
Case report
An 8-year-old Italian boy was referred for treatment of adenoid hypertrophy. In April, 2003, the child underwent adenoidectomy, under general anaesthesia. He was placed in the Rose position; the adenoid tissue was removed with a Beck’s adenotome, and bipolar suction electrocautery was used for haemostasis. The surgical procedure was completed without difficulty and did not involve any unusual rotation of the head. In the immediate post-operative phase, painful torcicollis occurred with mild rotation of the patient’s head to the right. The initial physical examination revealed a spasm in the right sternocleidomastoid muscle, and diagnostic assessments were commenced. Radiological evaluation included X-ray of the cervical spine with antero-posterior, lateral, and odontoid projections, as well as Computed Tomography (CT) scan. Following plain roentgenograms of the upper cervical spine, atlanto-axial rotary fixation was suspected, but flexion-extension views revealed a normal atlanto-dens interval. CT scan of the upper cervical spine revealed atlanto-axial rotary subluxation with an increase in the atlanto-dens interval of approximately 4 mm (Fig. 1), confirmed by three-dimensional (3D) reconstruction (Figs. 2, 3). A reduction of the subluxation, under analgesia, was initially attempted, however with no result. The reduction was then performed under general anaesthesia. The patient was placed in five-pound cervical halo traction. A repeat CT scan showed complete reduction of the previous atlanto-axial rotary subluxation. After applying a halo vest, the patient was discharged and sent home on the 14th day of hospitalization. A CT scan, performed post-operatively, after wearing the halo vest for 6 weeks, showed increased ossification and mineralization of the odontoid process. The halo was removed. At 18 months’ follow-up, the patient had a full range of cervical movement with no X-ray evidence of atlanto-axial subluxation.
Fig. 1.
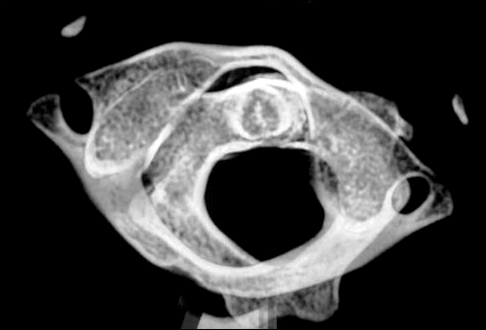
CT scan showing rotatory atlanto-axial subluxation with anterior displacement of atlas relative to axis corresponding to Fielding Type II subluxation.
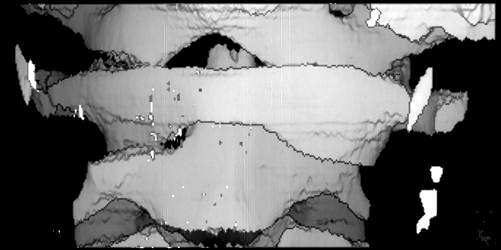
Fig. 2.
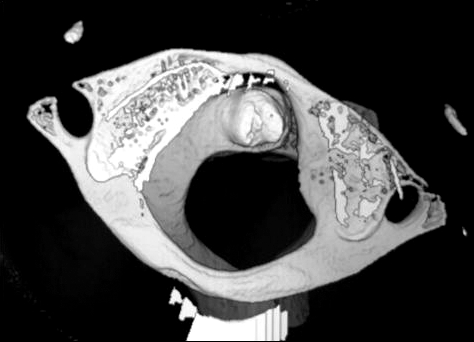
Three-dimensional reconstruction of axial CT scan, showing rotatory atlanto-axial subluxation.
Fig. 3.
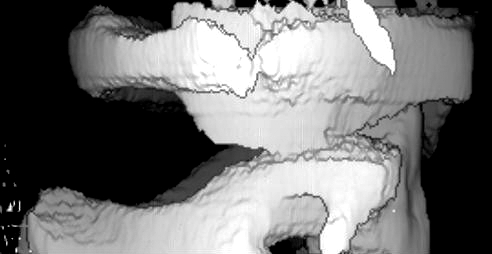
Three-dimensional reconstruction of axial CT scan showing anterior displacement of atlas relative to axis.
Discussion
Most Authors emphasise the appearance and frequency of secondary haemorrhage as a post-operative risk following adeno-tonsillectomy 9, yet only a few articles address the less frequent, but highly dangerous, complications such as neck complaints 10. Non-traumatic subluxation of the atlanto-axial joint is an uncommon and poorly understood condition which occurs mainly in children. It results from a pathological relaxation of the ligaments surrounding the joint following an inflammatory process 11 or otolaryngological surgical procedures 10. A previous infection is the most common cause of inflammation but it can also be a complication of head and neck surgery: it has been described in common otolaryngeal conditions such as tonsillitis, pharyngitis, adenoiditis, parotitis, and tonsillar or cervical abscesses, or after common surgical procedures such as tonsillectomy, adenoidectomy, or mastoidectomy (Table I) 3 6 10 12–21.
Table I. Causes of 110 reported cases of non-traumatic atlanto-axial subluxation (1830-2004).
| Causes | No. cases | |
| Infection | 77 | |
| Upper respiratory infection | 34 | |
| Tosillitis | 12 | |
| Mastoiditis or otitis media | 6 | |
| Acute rheumatic fever | 5 | |
| Retropharyngeal abscess | 5 | |
| Cervical adenitis | 3 | |
| Parotitis | 3 | |
| Tonsillar abscess | 2 | |
| Cervical abscess | 2 | |
| Fever of unknown origin | 2 | |
| Alveolar infection | 1 | |
| Posterior pharyngeal ulcer | 1 | |
| Influenza | 1 | |
| Post-operative | 25 | |
| Tonsillectomy and/or adenoidectomy | 11 | |
| Mastoidectomy | 9 | |
| Pharyngoplasty | 3 | |
| Choanal atresia repair | 1 | |
| Resection para-pharyngeal mass | 1 | |
| Inflammatory | 4 | |
| Arthritis | 4 | |
| Neurological dysfunction | 1 | |
| Primitive neuro-ectodermal tumour | 1 | |
| No cause stated | 2 | |
The atlas is a ring of bone with flat, slanting articulating facets on the lateral masses. The articulating facets form synovial joints with the corresponding anterior articulating surfaces of the axis; each has a loose capsule allowing maximum rotation with minimal lateral displacement. The primary stabilizer of the atlanto-axial joint is the transverse ligament; it is attached to the lateral posterior portion of the anterior arch of the atlas and forms the posterior support of the odontoid process, preventing excessive shift of C-1 on C-2. The paired alar ligaments are secondary stabilizers preventing excessive rotation. Numerous venous tributaries drain the posterior superior region of the nasopharynx. Pharyngovertebral veins cross the prevertebral fascia and drain into the peri-odontoidal plexuses, ultimately emptying into the upper cervical epidural venous sinuses. A possible pathway for the spread of inflammation to the atlanto-axial ligaments has been demonstrated via direct anastomoses between lymphatic vessels and pharyngo-vertebral veins. Naso-pharyngeal inflammation causes hyperaemia that may weaken the transverse and alar ligaments and the articular capsules resulting in atlanto-axial instability, followed by pathological rotation of the atlas on the axis 22. This condition begins as a typical torcicollis caused by spasms in irritated neck muscles, resulting, if prolonged, in distension of the ligaments. This second hypothesis, which presumes lax ligaments as a prerequisite for Grisel’s syndrome, is predominantly seen in children 3. Moreover, there is an increased risk of non-traumatic atlanto-axial subluxation in Down’s syndrome, a condition in which lax ligaments are a recognized feature 23. Nevertheless, in our opinion, excessive passive rotation and/or hyperextension of the head, in children, during surgical procedures, or patients transferred from the operating table to hospital bed without the use of a rollboard, could be the principal causes of atlanto-axial subluxation. Reports in the literature refer to the appearance of the atlanto-axial subluxation only after otolaryngological surgical procedures (Table I), conditions that facilitate excessive passive rotation and hyperextension of the young patient’s head.
Atlanto-axial subluxation typically appears in children as spontaneous torcicollis, although rare cases in adults have also been documented 24. The patient’s head is flexed and rotated, with a severely limited range of movement and pain on attempted reduction; the patient is unable to rotate his/her head above the midline, and his/her face may appear flattened. A possible distinguishing feature, from other causes of torcicollis, may be spasm of the longer contralateral sternocleidomastoid muscle, as opposed to spasm of the ipsilateral sternocleidomastoid muscle as seen in most other forms of torcicollis. Naso-pharyngeal examination may show a reduction in size of the naso-pharynx due to anterior displacement of the arch of the atlas; the projecting atlas may be palpable. An acute change in nasal resonance may also be observed. Neurological complications have been reported to occur in 15%, with outcome ranging from mild parasthesias, exaggerated reflex, clonus, or bladder dysfunction to quadriplegia or acute respiratory failure and death 8. These various complications result from the severity of atlanto-axial joint subluxation. Fielding and Hawkins have classified the non-traumatic subluxation of the atlanto-axial joint into four types (Fig. 4) 25. Type I and II subluxations are those most commonly found clinically and have no neurological impairment. The case reported here was consistent with Type II subluxation. Type III and IV subluxations, although rare, are invariably associated with spinal cord compression and have possible fatal consequences.
Fig. 4.
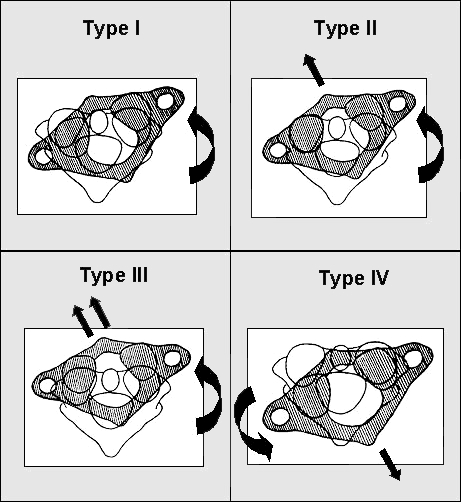
Fielding and Hawkins classification of C1-C2 rotary subluxation. Type I: rotatory fixation without anterior displacement of atlas (≤ 3 mm). Type II: rotatory fixation with anterior displacement of atlas of 3-5 mm. Type III: rotatory fixation with anterior displacement of atlas of > 5 mm. Type IV: rotatory fixation with posterior displacement of atlas.
The diagnosis of atlanto-axial subluxation requires radiological investigation. Plain radiographs of the cervical spine may show asymmetry between the facet joints in the antero-posterior projection and an increased atlanto-dens interval on the lateral projections. The normal atlanto-dens interval is 2.5 to 3 mm, in adults, and ≤ 4.5 mm, in children 11. An increase in the atlanto-dens interval of > 4.5 mm would suggest subluxation. Interpretation of atlanto-dens interval may not be possible on lateral films with rotary subluxation, and normal plain films of the neck do not rule out subluxation. CT is the procedure of choice in the evaluation of the bony cervical spine, whereas magnetic resonance imaging (MRI) provides information related to the surrounding soft tissue structures and the spinal cord.
Broad-spectrum antibiotic therapy is commenced to control wound infection. In the case of persistent torcicollis with no improvement following one week of conservative treatment, a CT scan with 3D reconstruction should be performed 26 (Figs. 2, 3, 5). Additional treatment depends on the degree of subluxation and the duration of symptoms. The patient should be referred for orthopaedic or neurosurgical consultation. Fielding’s Type I and II subluxations may be treated with antibiotics and a cervical collar, but, in some patients, reduction can only be achieved with cervical traction, followed by a period of neck immobilization in a cervical collar or halo vest for 6 weeks, as in our case, to prevent recurrence of the subluxation. Fielding’s Type III and IV subluxations generally need bed rest with cervical traction, followed by a period of neck immobilization. If conservative treatment fails to achieve reduction or is followed by neurological symptoms, arthrodesis of the first and second cervical vertebrae is indicated.
Fig. 5.
Three-dimensional reconstruction of axial CT scan showing lateral tilt of dens in relation to skull base and atlas.
Prognosis with treatment is excellent, but late diagnosis, i.e., more than one month after the initial symptoms, often requires some form of surgical arthrodesis as the deformity is usually immobile 27. In most of these cases, subluxation will decrease spontaneously or after a short period of cervical traction. Persistent torcicollis following tonsillectomy and/or adenoidectomy should alert the surgeon to initial subluxation of the atlanto-axial joint. CT scan with 3D reconstruction has proved to be an excellent method by which to reveal the presence and degree of atlanto-axial subluxation.
Clinical management begins pre-operatively by alerting the child’s parents that Grisel’s syndrome – while being an exceptional complication – may occur after an otorhinolaryngologic procedure. Bipolar suction electrocautery is the only helpful instrument for meticulous haemostasis, since monopolar suction cautery, used in adenoidectomy, is considered to be a risk factor for Grisel’s syndrome 28. Prophylactic antibiotic therapy can be considered, if extensive haemostasis is necessary during the procedure. Nevertheless, we recommend two steps to prevent this rare post-operative complication: excessive passive rotation and hyperextension of the head, in children under general anaesthesia, should be avoided and, when the child wakes up after surgery, a rollboard should be used to transfer the patient from the operating table to the hospital bed, to avoid a cervical trauma.
References
- 1.Bell C. The nervous system of the human body, embracing papers to the Royal Society on the subject of nerves. London: Longman, Rees and Orme; 1830. p. 403. [Google Scholar]
- 2.Grisel P. Enucléation de l’atlas et torcicolis nasopharyngien. Presse Médicale 1930;38:50-3. [Google Scholar]
- 3.Fernandez Cornejo VJ, Martinez-Lage JF, Piqueras C, Gelabert A, Poza M. Inflammatory atlanto-axial subluxation (Grisel’s syndrome) in children: clinical diagnosis and management. Childs Nerv Syst 2003;19:342-7. [DOI] [PubMed] [Google Scholar]
- 4.Berry DS, Moriarty RA. Atlanto-axial subluxation related to pharyngitis: Grisel’ syndrome. Clin Pediatr 1999;38:673-5. [DOI] [PubMed] [Google Scholar]
- 5.Baker LL, Bower CM, Glasier CM. Atlanto-axial subluxation and cervical osteomyelitis: two unusual complications of adenoidectomy. Ann Otol Rhinol Laryngol 1996;105:295-9. [DOI] [PubMed] [Google Scholar]
- 6.Tschopp K. Monopolar electrocautery in adenoidectomy as a possible risk factor for Grisel’s syndrome. Laryngoscope 2002;112:1445-9. [DOI] [PubMed] [Google Scholar]
- 7.Kraft M, Tschopp K. Evaluation of persistent torcicollis following adenoidectomy. J Laryngol Otol 2001;115:669-72. [DOI] [PubMed] [Google Scholar]
- 8.Grobman LR, Stricker S. Grisel’s syndrome. Ear Nose Throat J 1990;69:799-801. [PubMed] [Google Scholar]
- 9.Peterson J, Losek JD. Post-tonsillectomy hemorrhage and pediatric emergency care. Clin Pediatr 2004;43:445-8. [DOI] [PubMed] [Google Scholar]
- 10.Feldmann H, Meister EF, Kuttner K. From the expert’s office. Atlanto-axial subluxation with spastic tortico after adenoidectomy resp. tonsillectomy in Rose position – malpractice surgeon or the anaesthesiologist? Laryngorhinootologie 2003;82:799-804. [DOI] [PubMed] [Google Scholar]
- 11.Wetzel FD, La Rocca H. Grisel’s syndrome: a review. Clin Orthopaed Related Res 1989;240:141-52. [PubMed] [Google Scholar]
- 12.Gourin CG, Kaper B, Abdu WA, Donegan JO. Nontraumatic atlanto-axial subluxation after retropharyngeal cellulitis: Grisel’s syndome. Am J Otolaryngol 2002;23:60-5. [DOI] [PubMed] [Google Scholar]
- 13.Wurm G, Aichholzer M, Nussbaumer K. Acquired torcicollis due to Grisel’s syndrome: case report and follow-up of non-traumatic atlanto-axial rotatory subluxation. Neuropediatrics 2004;35:134-8. [DOI] [PubMed] [Google Scholar]
- 14.Corluy L, Pison L, Lauweryns P, Samson I, Westhovens R. An unusual non-traumatic atlanto-axial subluxation in an adult patient: Grisel’s syndrome. Clin Rheumatol 2004;23:182-3. [DOI] [PubMed] [Google Scholar]
- 15.Hirth K, Welkoborsky HJ. Grisel’s syndrome following ENT – surgery: report of two cases. Laryngorhinootologie 2003;82:794-8. [DOI] [PubMed] [Google Scholar]
- 16.Martinez-Lage JF, Morales T, Fernandez Cornejo V. Inflammatory C2-3 subluxation: a Grisel’s syndrome variant. Arch Dis Child 2003;88:628-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Akpinar G, Tekkok IH, Sumer M. Grisel’s syndrome: a case of potentially lethal spinal cord injury in the adult. Br J Neurosurg 2002;16:592-6. [PubMed] [Google Scholar]
- 18.Ugur HC, Caglar S, Unlu A, Erdem A, Kanpolat Y. Infection-related atlanto-axial subluxation in two adults: Grisel syndrome or not? Acta Neurochir 2003;145:69-72. [DOI] [PubMed] [Google Scholar]
- 19.Kasten P, Zeichen J, Gosling T, Krettek C. Grisel syndrome – a trauma surgery rarity. Unfallchirurg 2002;105:565-8. [DOI] [PubMed] [Google Scholar]
- 20.Mezue WC, Taha ZM, Bashir EM. Fever and acquired torcicollis in hospitalized children. J Laryngol Otol 2002;116:280-4. [DOI] [PubMed] [Google Scholar]
- 21.Okada Y, Fukasawa N, Tomomasa T, Inoue Y, Morikawa A. Atlanto-axial subluxation (Grisel’s syndrome) associated with mumps. Pediatr Int 2002;44:192-4. [DOI] [PubMed] [Google Scholar]
- 22.Parke WW, Rothman RH, Brown MD. The pharyngovertebral veins: an anatomical rationale for Grisel’s syndrome. J Bone Joint Surg 1984;66:568-74. [PubMed] [Google Scholar]
- 23.Harley EH, Collins MD. Neurologic sequelae secondary to atlanto-axial instability in Down syndrome. Arch Otolaryngol Head Neck Surg 1994;120:159-65. [DOI] [PubMed] [Google Scholar]
- 24.Mathern GW, Batzdorf U. Grisel’s syndrome. Cervical spine: clinical, pathologic and neurologic manifestations. Clin Orthop 1989;244:131-46. [PubMed] [Google Scholar]
- 25.Fielding JW, Hawkins RJ, Hensinger RN, Francis WR. Atlanto-axial rotary deformities. Orthop Clin North Am 1978;9:955-67. [PubMed] [Google Scholar]
- 26.Samuel D, Thomas DM, Tierney PA, Patel KS. Atlanto-axial subluxation (Grisel’s syndrome) following otolaryngological diseases and procedures. J Laryngol Otol 1995;109:1005-9. [DOI] [PubMed] [Google Scholar]
- 27.Phillips WA, Hawkins RJ. The management of rotatory atlanto-axial subluxation in children. J Bone Joint Surg 1989;71:664-8. [PubMed] [Google Scholar]
- 28.Tschopp K. Monopolar electrocautery in adenoidectomy as a possible risk factor for Grisel’s syndrome. Laryngoscope 2002;112:1445-9. [DOI] [PubMed] [Google Scholar]


