Summary
Head and neck defects following oncological surgery must often be repaired with soft tissue and/or bone from other areas of the body. Significant loss of soft tissue requires flaps of sufficient bulk to adequately reconstruct the defect. Microvascular free tissue transfer is a good method for reconstructing even large defects following oncological surgery for head and neck cancer. Continuous post-operative monitoring of the perfusion of a free flap is vitally important to achieve not only a favourable outcome but also to decrease morbidity. Microvascular thrombosis occurs in 4% of the flaps and the best chance for flap salvage is offered by the earliest possible revision of the microanastomosis. Use of buried flaps in head and neck reconstruction makes monitoring particularly difficult and exteriorization of a segment of the flap permits a direct visualization.
An original technique is presented for harvesting forearm free flaps with a secondary monitor skin paddle to externally check the status of the paddle and, when modified, can also be used for fibula and rectus abdominis flap.
Keywords: Head and neck cancer, Reconstruction surgery, Free flaps, Free flap monitoring
Riassunto
I difetti insorti dopo chirurgia oncologica nel distretto testa-collo spesso devono essere colmati con lembi semplici o compositi prelevati da varie aree del corpo. Una significativa perdita di sostanza richiede lembi sufficientemente spessi per colmare adeguatamente il difetto. I lembi rivascolarizzati sono un’ottima opzione ricostruttiva anche per difetti molto ampi. Il monitoraggio continuo post-operatorio della perfusione di un lembo libero è di vitale importanza nell’ottenere un risultato favorevole e nel minimizzare la morbilità a carico del paziente. Trombosi microvascolari possono occorrere nel 4% e l’unica possibilità di salvare il lembo è costituita da una precoce revisione delle microanastomosi. L’uso di lembi rivascolarizzati sepolti, in sedi nascoste, rende il monitoraggio molto indaginoso e l’esteriorizzazione di parte del lembo permette una sua diretta visualizzazione. Gli Autori presentano una tecnica originale per allestire il lembo rivascolarizzato antibrachiale con un’isola monitor cutanea che permetta di controllare dall’esterno lo stato del lembo sepolto. Tale tecnica è stata adattata anche al lembo rivascolarizzato di fibula e di retto addominale.
Introduction
Micro-vascular free tissue transfer is a widespread, safe and reliable method for the reconstruction of head and neck defects following oncologic surgery.
The incidence of vascular thrombosis in free flap reconstruction is estimated to be around 4% 1. To achieve a favourable outcome, vigilant surveillance of the perfusion of the flap is mandatory, because only early revision of the microanastomosis offers the opportunity to salvage those flaps presenting evidence of suffering.
The majority of free flaps can be directly visualized, and vitality of the flap can be assessed simply by checking the colour of the tissue, turgor, capillary refill and bleeding.
The use of buried free flaps in head and neck reconstruction makes monitoring particularly difficult, because either the flap does not communicate with the outside, or is placed in a region which is practically inaccessible by direct visualisation.
The introduction of a monitor skin paddle, in the event of buried free flaps, offers an easy method to check viability of the flap in the post-operative period.
An ideal monitoring technique should be an objective, clear and continuous indicator of any change in the flap as far as concerns artero-venous circulation, furthermore it needs to be easily manageable and monitored also by the nursing staff.
A series of 9 patients have been submitted to head and neck reconstruction using 3 different types of buried free flaps. A monitor skin paddle was harvested, in all cases, to post-operatively monitor flap viability. An original technique used, in this series, to harvest the monitor skin paddle of the free radial forearm flap is described.
Material and methods
From January to November 2004, 9 consecutive patients underwent head and neck reconstruction, at the Department of Otolaryngology Head and Neck Surgery, National Cancer Institute in Rome, using a buried free flap, with adjunctive monitor skin paddle.
All patients were male, mean age 55 years (range 51-61).
Reconstruction was performed with a free radial forearm flap in 5 cases, with an osseous fibula free flap in 3 cases and in one case with a rectus abdominis muscular flap.
Free radial forearm flap (5 cases)
Three patients underwent total laryngectomy with circumferential total hypo-pharyngectomy for hypo-pharyngeal carcinoma (the pharyngeal defect, after resection, varied from 9 to 12 cm in length).
Reconstruction was performed in a one-stage procedure using a free radial forearm flap. The prevertebral fascia sutured to the posterior wall of the oesophagus and to the posterior wall of the oropharynx created the posterior wall of the neopharynx, the free radial forearm flap then reconstructed the anterior and lateral walls. The flap was harvested in a trapezoid shape, the longer edge of the skin paddle was sutured to the anterior and lateral walls of the oropharyngeal stump, and the shorter edge was sutured inferiorly to the anterior and lateral walls of the oesophageal stump, then, laterally, the skin paddle was sutured to the prevertebral fascia. A salivary stent containing the feeding tube was left in situ, the feeding tube was removed on day 10, the patient was then fed through the stent that was removed transorally on day 21.
One patient presented recurrent posterior wall hypo-pharyngeal carcinoma after previous radiotherapy. The patient underwent posterior wall resection with larynx preservation through a lateral approach. The defect was reconstructed placing a free radial forearm flap sutured to the residual mucosa of the lateral walls of both pyriform sinuses and to the posterior wall of the oropharynx and oesophagus. The naso-gastric feeding tube was removed on day 15 when the patient started deglutitory rehabilitation. The patient was decannulated and tracheotomy was closed on day 23.
One patient underwent subtotal resection of the base of the tongue with partial lateral pharyngectomy through a mandibular swing approach due to carcinoma at the base of the tongue. The defect was reconstructed with a free radial forearm flap, but a pre-existing trismus precluded every possibility of direct flap visualization.
Allen test was performed, pre-operatively, in all cases, to evaluate radial and ulnar artery patency. In these 5 cases, the monitor island was harvested in an original way, in a proximal position and not contiguous to the primary flap (Fig. 1). The cephalic vein is superficial and adherent to the subcutaneous tissue, the monitor flap was harvested as a small paddle in the skin overlying the vein. In the incision connecting the major skin paddle with the cubitus, an elliptic shaped monitor was proximally incised and maintained with the vein during standard dissection (Fig. 2).
Fig. 1.
Pre-operative planning of forearm flap and monitor.
Fig. 2.
Monitor island related to the cephalic vein.
Vascularization of the small monitor is provided by the blood of the vein.
The donor site of the flap was covered with a skin graft from the left thigh. The small defects created by the monitor paddle were closed directly.
In the case of partial resection of the base of the tongue and pharynx, the flap was positioned to cover the defect and sutured to the surrounding tissues.
The radial artery was anastomosed, in 3 cases, to the superior thyroid artery and, in 2 cases, to the facial artery; the cephalic vein was directly sutured to the internal jugular vein with termino-lateral anastomosis in all cases. The monitoring skin paddle was sutured externally between the cervical flaps allowing the physician and nurses to regularly check flap viability and detect early changes in skin perfusion (Fig. 3).
Fig. 3.
Monitor island sutured outside between skin incision.
Fibula osseous free flap (3 cases)
One patient underwent segmental mandibular resection for a recurrent squamous cell carcinoma, localised in the floor of the mouth, after previous surgical resection with marginal mandibulectomy. The two remaining cases were small alveolar ridge carcinomas with mandibular erosion treated with a segmental mandibular resection of 4 cm.
In all cases, the bony defect was reconstructed with free osseous fibula flap and the mucosal defect was closed by direct suture.
The peroneal artery was anastomosed with the lingual artery and the vein was sutured to the internal jugular vein with termino-lateral anastomosis.
The monitor skin paddle was prelevated, in all cases, under the mid-point between the head of the fibula and the lateral malleolus. Doppler examination identified the most valid perforator vessel (2-5 cm under mid-line point). Skin incision was performed along the lateral aspect of the fibula, and to be sure to correctly centre the 2 cm2 skin monitor on the perforant, the incision was curved anteriorly in the region of the perforant vessel, then the perforant was directly visualized with antero-posterior dissection of the skin so that the monitor was incised in correspondence to the vessels.
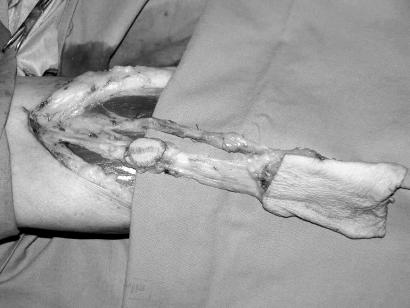
During harvesting of the free osseous fibula flap, to protect the septo-muscular perforant and the skin monitor, a protective cuff of muscle (flexor allucis longus muscle) was included around the bone (Fig. 4).
Fig. 4.
Free osseous fibula flap in its definitive position, with the 2x2cm monitor skin island centered just above the septo-muscular branch including a protective cuff of muscle (flexor allucis longus muscle) around the bone.
Rectus abdominis free flap (1 case)
One patient underwent wide excision of a Malignant Peripheral Neural Sheet Tumour (MPNST), in the temporal region and deep into the infra-temporal fossa, with removal of the entire temporalis muscle, most of the zygomatic bone, parotid gland, entire temporo-mandibular joint, ascending ramus of the mandible and lateral wall of the maxillary sinus. The defect was filled with a revascularized muscle flap of left rectus abdominis and the skin edges were repositioned. The inferior epigastic artery (branch of the external iliac artery) was anastomosed to the facial artery; the comitants veins were directly sutured to the internal jugular vein with termino-terminal anastomosis. Also in this case, the muscular flap was harvested with a 2 cm2 skin paddle vascularized by muscular-cutaneous perforator (Fig. 5). The harvested flap was larger than necessary, bearing in mind that the volume of the shrinking denervated muscle will be related to atrophy and fat re-absorption (Fig. 6).
Fig. 5.
Rectus abdominis left muscle with skin island harvested just above it in periumbelical region.
Fig. 6.
Monitor skin island of rectus abdominis free flap sutured outside between cervical flaps.
All nine patients received post-operative antibiotic treatment (penicillin 2 g x 2 iv), Plander (Eudextran 40) 12 ml/hour for 24 hours and sodium enoxaparin (4000 IU) every day for 30 days.
The monitor was checked, in all cases, every 2 hours for the first 48 hours post-operatively.
The change in colour, the temperature or the lack of bleeding after needlestick of the monitor and accelerated refilling time were the criteria for immediate revision of the micro-vascular anastomosis.
Results
Eight flaps had a favourable outcome with no monitoring abnormalities. The monitor island in one case (the flap used for reconstruction of the posterior pharyngeal wall), showed signs of venous congestion about 16 hours after surgery. Immediate revision revealed thrombosis of the venous anastomosis. The intraluminal thrombus was removed and a new venous anastomosis was performed on the internal jugular vein, about 3 cm lower than the first. After surgical revision, the colour of the monitor flap returned to normal and the free flap survived without any further problem. Donor site healed within 3 weeks, in all cases. Furthermore, every monitor island had a regular integration between the cervical flaps, with minimal colour differences in the cervical skin.
Discussion
The main problem encountered in the use of micro-vascular buried flaps is the difficulty to check the state of vascularization.
The use of a monitor skin paddle is a simple method to directly check the viability of a buried free flap, the correlation between the viability of the skin monitor and the state of the flap was 100%, in our series.
Several methods have been proposed in the literature to check the viability of free flaps 2.
The methods requiring a direct contact flap-device (laser Doppler flowmeter 3, trans-cutaneous oxygen measurement 4) cannot be used when dealing with buried flaps. As an alternative to the monitor skin paddle, other techniques, such as arteriography, intravenous fluorescein or radioisotope washout have been proposed to control non-accessible flaps, although those techniques, which are expensive, cannot provide continuous information to allow early detection of micro-vascular alterations. The use of buried probes, placed in proximity to the micro-vascular anastomosis can be biased by false positives due to dislocation of the probe and requires a secondary procedure for removal. Surface pulse Doppler to check the patency of the microanastomosis is hampered by the interference of the other vessels in the neck.
In our opinion, the possibility to be able to directly check a monitor flap, the perfusion of which is closely related to the perfusion of the flap, represents a simple and effective method. In some cases, if the flap is placed in the hypopharynx, the endoscopic examination may be very helpful but it can be limited by post-operative oedema and secretions, it has to be performed only by the physician and it is quite impossible to test capillary refill and bleeding after needlestick. Furthermore, the excessive number of daily endoscopic examinations is very uncomfortable for the patient.
Free radial forearm flap
Several Authors have reported the use of an island flap to monitor the viability of the buried forearm flap (Table I).
Table I. Different monitoring island harvesting methods.
| Monitor flap based on external component of the main paddle | Monitor flap based on septocutaneous branch of the radial artery | Monitor flap based on venous flow of cephalic vein | |
| Author | Urken et al. | Cho et al. | Pellini et al. |
| Byun et al. | Iwasawa et al. | ||
| Furuta et al. | |||
| Difficulty in harvesting | + | +++ | + |
| Skin monitor paddle mobility | + | +++ | +++ |
| False positive | 0% | 36% | 0% |
Cho et al. used a 4 cm2 island flap supplied by a septocutaneous branch of the radial artery. This monitor skin paddle, with its pedicle, has a wide range of movement and can be sutured at a distance from the mean fascio-cutaneous paddle, but it needs the presence of a perforating artery with an adequate calibre that is not always possible to identify. Moreover, it requires extra dissection during harvesting of the flap and, to protect the pedicle, any torsion or tension should be avoided during fixation. This small pedicle seems to be very delicate and could become involved in thrombosis, presenting, as shown, a false positive rate of 36% 5.
Byun et al. also reported the use of a small island monitor flap based on a branch of the radial artery. According to these authors, since the proximal forearm contains a few fascio-cutaneous branches of the radial artery, this kind of monitor is not always feasible 6.
Urken et al. suggested that the radial forearm flap can be designed with an external component to use as a monitor, created by de-epithelialization of part of the skin paddle to create a separation between the monitor and the main paddle. This is a reliable, well-vascularized cutaneous paddle, is apparently easy to harvest and very reliable for monitoring, but the definitive position of the skin monitor island is strictly related to the definitive position of the primary paddle with little possibility of movement. Furthermore, harvest of this type of monitor decreases the amount of forearm skin available for the reconstruction 7.
Furuta et al. 8 and Akin et al. 9, also reported a similar monitor paddle designed in proximity to the wrist on the ulnar side separated from the main paddle by de-epithelialized skin.
All drew the monitor paddle vascularized from the radial artery, in continuity with the flap.
Our method is based on vascularization of the monitor island from the reflow blood of the cephalic vein.
The poorly oxygenated venous blood is sufficient to vascularize a small skin paddle with limited metabolic requisites.
Furthermore, the surgical technique used to harvest the monitor is very easy and does not require any extra dissection, this is reflected by the lack of risk of false positives due to futher pedicle distorsion or thrombosis; the length of the venous pedicle allows transposition of the monitor island far from the forearm flap in the cervical skin incision line.
In our experience, our original monitor for the free radial forearm flap is reliable and no false positive results occurred. Use of this kind of monitor is related to the need to perform venous anastomosis using the cephalic vein, so that if only the comitant veins are used this monitor obviously cannot be harvested.
Fibula osseous free flap
Free fibula flap is used in oral cavity reconstruction as an osseous cutaneous or osseous flap. Use without skin occurs, principally in secondary reconstruction after mandibular segmental reconstruction, or in primary reconstruction when the mucosal defect can be closed directly without tension.
In these selected cases, when the flap is completely buried, monitoring by direct visualization is impossible.
To check the flap positioning outside, a small skin monitor island, as reported by Al Qattan and Boyol 10 (based on the fasciocutaneous perforator, rising from the peroneal artery) is possible, bearing in mind the risk of false positives.
In 1989, in his initial description of the use of the composite osteocutaneous fibula free flap, Hidalgo reported 4/5 total necrosis of the skin paddle that were used to repair the mucosal defect 11. He concluded that the osteocutaneous free flap cannot be used in the case of large intra-oral mucosal defects.
On the other hand, in 1994, Wei et al. reported 100% skin success rate in 27 cases of mandibular reconstruction 12. Some anatomic studies have been performed by Yoshimura et al. 13 and Beppu et al. 14 to identify the location and the calibre of the skin vessels. Both concluded that most of the perforant vessels are located below the mid point of the fibula and in 71% of the cases are muscolo-cutaneous perforants.
In our opinion, the small monitor skin island must be exactly centered on a perforator vessel, pre-operatively identified by Doppler ultrasonography and then by direct dissection of the skin, the inclusion of a cuff of flexor hallucis longus muscle, even in those cases in which a septal branch is identified, is important to protect the integrity of the perforant of the monitor. In our limited experience, this method is extremely reliable in monitoring flap status.
Rectus abdominis free flap
The rectus abdominis flap is reliable and easy to harvest. It has been extensively used as a pedicled or free flap for breast reconstruction. It can be harvested as a muscular flap or as a myocutaneous flap. This flap is quite bulky and represents an excellent option to reconstruct large head and neck defects. This flap is most commonly used after total glossectomy, for orbital/maxillary defects, and skull base reconstructions. Although the rectus abdominis free flap is a highly reliable flap with vessels of great calibre, monitoring of its viability, when buried, remains important. The use of a monitor skin paddle sutured between the cervico-facial skin incision line is useful. The skin of the flap is generously supplied by musculocutaneous perforants rising directly from the inferior and superior epigastric artery, so that there is no need to precisely identify a perforant as in the fibula flap and a small island, randomly chosen in the peri-umbilical area, can be used. In our case, we used the flap to fill a surgical cavity suturing the skin monitor in the pre-auricular incision. On account of the very rich vascularization of the flap, the skin monitor, in our opinion, always reflects the status and the viability of the entire flap.
Conclusions
Monitoring of buried flaps is very difficult. The use of an external monitor with the same vascularization of the flap is a valid proposal.
In our experience, using a monitoring flap, no false-positive results occurred.
The flap is easy to harvest and does not require additional operation time. For these reasons, its use is recommended.
References
- 1.Buncke HJ, Lineaweaver W, Valauri F, Buncke GH. Microsurgery transplantation-replantation. Philadelphia: Lea & Febiger; 1991. p. 715-21. [Google Scholar]
- 2.Lineaweaver W, Valauri F, Buncke G. Monitoring. In: Buncke HJ, editor. Clinical atlas of reconstructive microsurgery and replantation. Philadelphia: Lea & Febiger; 1988. p. 87. [Google Scholar]
- 3.Jenkens S, Sepka R, Barwick W, Serafin D, Klitzam B. Routine clinical use of laser doppler flowmeter to monitor free tissue transfer: preliminary results. J Reconstr Microsurg 1987;3:281-3. [DOI] [PubMed] [Google Scholar]
- 4.Smith A, Sonneveld J, Kort W, van der Meulen J. Clinical application of transcutaneous oxygen measurements in replantation surgery and free tissue transfer. J Hand Surgery 1983;8:139-45. [DOI] [PubMed] [Google Scholar]
- 5.Cho BC, Shin DP, Byun JS, Park JW, Baik BS. Monitoring flap for buried free tissue transfer: its importance and reliability. Plast Reconstr Surg 2002;110:1249-58. [DOI] [PubMed] [Google Scholar]
- 6.Byun JS, Baik BS, Park JS. An effective pharyngoesophageal reconstruction with free radial forearm flaps. Eur J Plast Surg 1992;15:173-6. [Google Scholar]
- 7.Urken ML, Weinberg H, Vickery C, Buchbinder D, Biller H. Free flap design in head and neck reconstruction to achieve an external segment for monitoring. Arch Otolaryngol Head Neck Surg 1989;115:1447-53. [DOI] [PubMed] [Google Scholar]
- 8.Furuta S, Hataya Y, Ishigaky Y, Watanabe T. Monitoring the free radial forearm flap in pharyngo-oesophageal reconstruction. Br J Plast Surg 1997;50:40-2. [DOI] [PubMed] [Google Scholar]
- 9.Akin S, Basut O. A new flap designed for monitoring the circulation of a buried free radial forearm flap in pharyngoesophageal reconstruction. J Reconstr Microsurg 2002;18:591-4. [DOI] [PubMed] [Google Scholar]
- 10.Al Qattan M, Boyol BJ. “Mini paddle” for monitoring the fibular free flap in mandibular reconstruction. Microsurgery 1994;15:153-4. [DOI] [PubMed] [Google Scholar]
- 11.Hidalgo D. Fibula free flap: a new method of mandible reconstruction. Plastic Reconstr Surg 1989;84:71-4. [PubMed] [Google Scholar]
- 12.Wei F, Seah C, Tsai L, Liu S, Tsai M. Fibula osteoseptocutaneous flap for reconstruction of composite mandibular defect. Plastic Reconstr Surg 1994;39:294-6. [PubMed] [Google Scholar]
- 13.Yoshimura M, Shimada T, Hosokawa M. The vasculature of the peroneal tissue transfer. Plastic Reconstr Surg 1990;85:917-21. [DOI] [PubMed] [Google Scholar]
- 14.Beppu M, Hanel D, Johnston G, Carmo J, Tsai T. The osteocutaneous fibula flap: an anatomic study. J Reconstr Microsurg 1992;8:215-23. [DOI] [PubMed] [Google Scholar]