Summary
Although the diagnostic reliability of auditory brainstem responses (ABR) in acoustic neuromas has been revised due to its poor sensitivity (demonstrated above all in smaller tumours), and its limited specificity, this method is still used as the initial otoneurological approach. To contribute to the clinical use of this method, in particular with the aim of reducing the number of false positives, a retrospective study was carried out in two groups of patients affected by unilateral sensorineural hearing loss with auditory brainstem response abnormalities: in the first group (50 cases: true positives) hearing loss was the expression of an acoustic neuroma shown by magnetic resonance imaging, in the second group (130: false positives) magnetic resonance imaging was negative. In both groups, auditory brainstem response recordings showed abnormalities suggesting retro-cochlear disorders such as: 1) complete absence of response not justified by the extent of the hearing loss, 2) presence of only wave I, 3) increase in wave V absolute latency with normal I-V interpeak latency, 4) increase in wave V absolute latency, the sole component, 5) increase in wave V absolute latency and I-V interpeak latency. A comparison between the two groups made it possible to show that the finding of “major” auditory brainstem response alterations (complete absence of response not justified by the extent of the hearing loss or presence of only wave I) is correlated with a high probability of the presence of a neuroma, while other abnormalities (wave V latency and I-V interpeak latency increase) have no particular predictive value since percentages are almost identical in the two groups. Wave V latency increase with normal I-V interpeak latency was observed in only one case of acoustic neuroma and this clinical finding is not easy to interpret. It would not appear possible, based on current knowledge, to further improve the reliability of this test, and, therefore, its use in oto-neurological diagnostics remains limited.
Keywords: Acoustic neuroma, Diagnosis, Auditory Brainstem Responses
Riassunto
Benché l’affidabilità diagnostica delle ABR (Auditory Brainstem Responses) nei neurinomi dell’acustico sia stata ridimensionata a causa della scarsa sensibilità, dimostrata soprattutto nei tumori più piccoli, e della modesta specificità, questa metodica di indagine viene tuttora utilizzata come primo approccio otoneurologico. Per portare un contributo all’impiego clinico di questa indagine, in particolare nell’ottica di ridurre il numero di falsi positivi, è stato condotto uno studio retrospettivo su 2 gruppi di pazienti che presentavano un’ipoacusia percettiva unilaterale con alterazioni della risposta ABR: nel primo gruppo (50 casi: veri positivi) l’ipoacusia era espressione di un neurinoma dell’acustico documentato alla RMN, nel 2° gruppo (130 casi: falsi positivi) la RMN era risultata negativa. In entrambi i gruppi, i tracciati ABR mostravano anomalie suggestive di patologia retrococleare quali: 1) assenza completa di risposta non giustificata dall’entità dell’ipoacusia; 2) presenza della sola onda I; 3) aumento della latenza assoluta dell’onda V con intervallo interpicco I-V normale; 4) aumento della latenza assoluta dell’onda V, unica componente registrabile; 5) aumento della latenza assoluta dell’onda V e dell’intervallo interpicco I-V. Il confronto tra i 2 gruppi ha permesso di evidenziare come il riscontro di alterazioni “maggiori” delle ABR (assenza completa di risposta non giustificata dall’entità dell’ipoacusia o presenza della sola onda I) sia correlato con elevata probabilità alla presenza di un neurinoma, mentre le altre alterazioni (aumento della latenza assoluta della V onda e/o dell’intervallo I-V) non rivestono particolare valore predittivo, in quanto si osservano percentuali pressoché sovrapponibili nei due gruppi. L’aumento di latenza assoluta della V onda con normale intervallo I-V è stato osservato in un solo caso di neurinoma dell’acustico, e tale reperto è di non chiara interpretazione. Allo stato attuale delle conoscenze non sembra possibile migliorare ulteriormente l’affidabilità di questo test, il cui apporto nella diagnostica otoneurologica resta pertanto limitato.
Introduction
The study of evoked auditory brainstem responses (ABRs) has represented a fundamental investigation in the differential diagnosis of perceptive hearing loss and other oto-vestibular disorders, in the belief that the sensitivity of this method made it possible to exclude, with sufficient probability, a retro-cochlear organic lesion (in particular an acoustic neuroma), and thus avoiding the need to carry out complex and expensive neuro-radiological tests such as magnetic resonance imaging (MRI).
The first reports published in the literature did, in fact, attribute ABRs with mean percentages of false positives and false negatives of around 15% and 5%, respectively 1.
The experience acquired over the last few years, the ever-increasing use of MRI and the need for greater clinical and forensic sensitivity have, however, led to a re-evaluation of the diagnostic reliability of ABRs, both in terms of sensitivity and specificity.
The sensitivity of ABRs in this type of disease is, in fact, directly proportional to the size of the tumour, and a varying percentage of tumours (up to 37% of intra-canalicular tumours, 9-11% of small-medium size extra-cananalicular tumours) may escape identification with this method 2 3.
On the basis of this evidence, due to the difficulty in performing MRI in all patients presenting unilateral audio-vestibular symptoms, it was believed that ABRs should be used only as a preliminary filter in the differential diagnosis of clinical situations considered to be “low risk” 4.
The specificity of ABRs has also been considerably revised, since recent non-selected series have reported much higher percentages (82%-96%) of false positives 3.
To improve the diagnostic accuracy of the method, a particular technique (stacked ABR) was proposed in 1997 2. This technique consists of recording a series of responses obtained under high-pass ipsilateral masking with various cut-off frequencies in order to obtain the selective response of various areas of the cochlea. The subsequent sum of all the responses gives a cumulative wave V, the amplitude of which, reflecting the discharge synchrony of the nerve fibers, represents the assessment parameter for distinguishing a cochlear lesion from a retro-cochlear lesion. Despite the great scientific interest shown in this technique, which would make it possible to identify small neuromas missed by traditional ABR, it does not seem to have become part of routine practice, probably due to the technical difficulties related to its use.
Despite the diagnostic limitations of ABRs, the difficulty in gaining access to MRI (at least in some regions) and the need to limit health costs have led to this test being considered as a means of screening 5 and, in this light, the use of this method in oto-neurological diagnosis can still be justified, especially if combined with meticulous patient follow-up.
In addition, the current tendency not to treat small acoustic neuromas, especially in certain categories of patient (such as the elderly), and, above all, the relatively slow growth of these tumours make the failure to diagnose them early of less importance (at least in certain cases).
The diagnostic potentials of ABRs should, therefore, be continuously improved in order to reduce both “false negatives” (i.e., diagnostic errors) and “false positives” (i.e., cases “unnecessarily” submitted to MRI).
In clinical practice, even in the presence of sensorineural hearing loss, absolutely normal electrophysiological responses not requiring any interpretation may be observed, and in these cases the possibility of false negatives must only be taken into consideration from a statistical point of view.
A pathological ABR response can, on the other hand, present with different types of alterations, and, in certain cases, a clinical/statistical interpretation is necessary to establish whether the detected abnormality depends solely on the deterioration in sensitivity of the cochlear receptor or, instead, on a retro-cochlear disorder.
Evaluation of ABR recordings is based on parameters which are now consolidated and agreed upon 6 7, such as the presence of morphological abnormalities, the complete absence of response disproportionate to the extent of the hearing loss the I-V interpeak latency 8 9 (if the complete response pattern is recorded), and the wave V absolute latency. This last parameter can be compared with the wave V latency in the contra-lateral ear (IT V index) 10 or with a latency value foreseen on the basis of the hearing loss (Delta V index) 11 12 or taken from a sample of confirmed cochlear hearing loss values 13, taking into account the fact that these assessments also include correction factors to compensate for the effect of the hearing loss on wave V latency (which in cochlear hearing loss increases proportionally with the hearing threshold for high frequencies) 14.
The IT V index, despite being one of the most commonly used, cannot always be employed and presents many variability factors (and, therefore, a different degree of sensitivity), due to the use or not of correction factors and the selected cut-off value (0.2-0.3-0.4 msec) 3 7 10 15, and, above all, the functionality of the contralateral reference ear, which can represent a, by no means, negligible source of error.
Even very recent contributions 16 17 have confirmed that this evaluation parameter can involve a significant number of “false negatives” (10-15%).
Obviously the choice of the diagnostic criteria may condition the access to neuroradiological tests and, consequently, the diagnostic efficiency of the method.
The aim of this study was to provide a further contribution to the clinical use of ABRs, analyzing and comparing the electrophysiological alterations observed in patients without an organic retro-cochlear disorder with those recorded in patients with an acoustic neuroma, in order to gather any further information that can be used in the otoneurological diagnosis.
Materials and methods
The ABR responses of two groups of patients were retrospectively considered and compared.
The first group (FP = false positive group) consisted of 130 cases of unilateral or prevalently unilateral sensorineural hearing loss, with ABR alterations suggestive of a retro-cochlear disorder but without evidence, at subsequent MRI, of organic lesions [in particular cranial nerve (cn) VIII neuromas].
This group included sudden and evolutive hearing loss and hearing loss with uncertain onset, all, however, with an initially unknown aetiology.
Cases of fluctuating hearing loss with a rising tonal curve which, as is known, can be associated with retro-cochlear lesions were also included in this group. Mean hearing threshold at 2 KHz and 4 KHz was respectively 34 dB HL (SD = ± 23) and 47 dB HL (SD = ± 24).
The second group (T = tumour group) consisted of 50 cases of unilateral sensorineural hearing loss, with ABR alterations correlated with the presence of an acoustic neuroma, confirmed by MRI. Mean hearing threshold at 2 KHz and 4 KHz was, respectively, 44 dB HL (SD = ± 23) and 52 dB HL (SD = ± 12).
The selected cases were not patients examined in sequence and it must not, therefore, be assumed that 50 cn VIII neuromas were diagnosed in 180 cases of perceptive hearing loss with altered ABRs.
In all cases, in both groups the ABR recordings showed at least one of the following alterations indicative of a retro-cochlear disorder:
complete absence of response not justified by the extent of the hearing loss (threshold at 2-4 KHz < 70 dB HL);
presence of only wave I;
increase in absolute wave V latency with normal I-V interpeak latency;
increase in absolute wave V latency (sole recordable component);
increase in absolute wave V latency and I-V interpeak latency (> 4.4 msec).
Wave V absolute latency was compared with the normal value (5.65 msec ± 0.188) as a reference, after subtracting a correction factor obtained from a sample of 200 cases of cochlear hearing loss (0.1 msec every 10 dB of hearing loss at 4000 Hz starting from 30 dB HL) 13.
In actual fact, latency values higher, after correction, than 6 msec (i.e., 2 SD above the normal value) were considered as suspected retro-cochlear hearing loss.
All cases of hearing loss in which a complete absence of ABRs could be justified by a high hearing threshold (average hearing threshold at 2-4 KHz > 70 dB HL) 18 were excluded from the study.
Assessment of the wave V latency inter-aural difference (IT V) did not represent a primary criterion of access to MRI, in our series, both to avoid previously recorded variability factors and in order to have a homogeneous and strictly mono-aural assessment of all the ABR responses obtained.
However, we never recorded a positive IT V (≥ 0.3 msec.) without other concomitant alterations which, in any case, indicated the need to proceed with neuro-radiological diagnosis.
Furthermore, no slight or isolated morphological alterations of the response were evaluated; in fact, all the MRIs performed exclusively for this type of anomaly (24 patients, not included in the sample) were negative.
Even if the size of the tumour represents the fundamental aspect in the therapeutic approach and in prognosis, it was not taken into consideration as the preliminary diagnostic stage (the object of this study) must not be influenced by speculations of this nature, particularly in patients with an altered ABR response which is, in any case, a precise indication for MRI. The diagnosis of an acoustic neuroma (or of other retrocochlear lesions) must, moreover, always be made as early as possible even for small tumours, at least in order to allow adequate follow-up to be carried out. It is also well known that in patients who present with only otological symptoms, the size of the tumour cannot be conjectured a priori and, in particular, the extent of the hearing loss (in turn, a determining factor in interpreting ABR alterations) can not be correlated with the size of the tumour 4.
All ABR recordings (FP and T groups) were performed in our Hospital by means of Medelec Sensor equipment, stimulating with non-filtered alternate polarity clicks, lasting 0.1 msec, in trains of 2048 stimuli, with 20 PPS cadence and 120 dB SPL intensity, with ipsi- and contra-lateral recording.
The MRI scans were carried out in various centres, as our series included patients followed on an outpatient basis and/or referred from other centres. However, the brain, in general, and the acoustic nerve, in particular, were always examined, using paramagnetic contrast medium, except in patients with suspected or confirmed allergy to metals.
Results
In the 130 patients in the FP group, with ABR alterations but without MRI evidence of organic disorders (in particular neuromas of cn VIII), and in the 50 patients in the T group (due to the presence, at MRI, of a tumour of cn VIII) the distribution of the ABR alterations indicated above was as showed in Table I.
Table I.
| FP group (130) | T group (50) | |
| Type 1: Complete absence of response not justified by extent of hearing loss | 2 (1.5%) | 9 (18%) |
| Type 2: Presence of only wave I | 1 (0.7%) | 7 (14%) |
| Type 3: Increase in wave V absolute latency with normal I-V interpeak latency | 36 (27.6%) | 1 (2%) |
| Type 4: Increase in wave V latency, sole component | 37 (28.4%) | 10 (20%) |
| Type 5: Increase in wave V absolute latency and I-V interpeak latency | 54 (41.5%) | 23 (46%) |
A complete response pattern (I-V pattern) was recorded in 90 cases in the FP group (69%) and in 24 cases in the T group (48%), while wave V was recorded in 127 cases in the FP group (97%) and in 34 cases in the T group (68%).
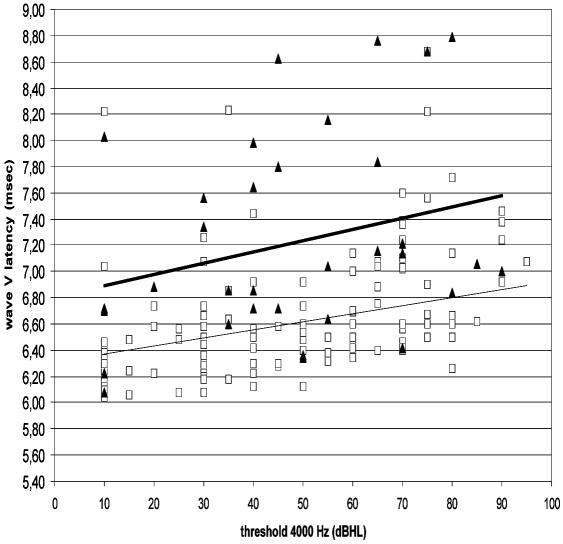
The relationships existing between wave V latency and the audiometric threshold at 4000 Hz were evaluated, for both groups of patients, by calculating the linear regression (Fig. 1).
Fig. 1.
Correlation between wave V latency and hearing threshold at 4000 Hz in cases of acoustic neuroma (T) and in false positives (FP).
It is worthwhile stressing the casual finding, at MRI, of two cases of intracanal neuroma in the opposite ear to that suspected of harbouring a retrocochlear lesion and without a pathological ABR (thus not included in the T group): if the total of 204 MRIs evaluated (130 FP group + 50 T group + 24 performed exclusively for slight and isolated morphological abnormalities) is taken into consideration, the incidence of intra-canalicular neuromas found by chance was therefore 0.09%.
Discussion and conclusions
A series of considerations can be made with regard to the results obtained.
First of all, comparison of the two groups showed that the “major” ABR alterations (types 1 and 2) were significantly more frequent in the T group than in the FP group: in actual fact, the complete absence of a response despite a sufficient hearing threshold or the presence of wave I only indicates a high probability of a neuroma rather than a false positive. This can naturally be explained by the intense neural conduction disorders often produced by an expansive disease.
The type 3 alteration indicates the coexistence of a normal parameter (the I-V interval) and an altered parameter (wave V absolute latency): this situation was seen almost exclusively in the group of false positives, but this finding in a case of neuroma of cn VIII (with an incidence of 2%) is not easy to interpret.
As far as concerns the other types of alterations, the comparison between the two groups did not offer elements that can be clearly interpreted.
In particular, the increase in the I-V interval (type 5), considered one of the most reliable diagnostic criteria, presented an almost identical percentage in the two groups: the finding of this alteration, at least as far as our series is concerned, does not, therefore, indicate a high probability of diagnosing a cn VIII neuroma.
The observation of only wave V with increased latency values (type 4) also has a similar incidence in the two groups and does not appear to have any particular predictive value.
It is, therefore, evident that the finding (within certain limits) of an increase in wave V latency or in the I-V interval does not, in general, have any particular predictive value in the diagnosis of an acoustic neuroma. These findings are not very comforting in terms of an improvement in the diagnostic performance of ABRs with regard to the specificity of the alterations.
As stated above, evaluation of wave V absolute latency represents one of the most widely adopted parameters, even in the presence of a measurable I-V interval.
Various methods proposed in the literature to establish whether an increase in wave V latency depends exclusively on hearing loss or, instead, on a retro-cochlear disorder have been previously reported.
Albeit, if one considers the relationships that exist between wave V latency and the audiometric threshold (4 KHz) in the two groups of patients (127 FP and 34 T with detectable wave V), it is evident that, at the same level of hearing loss, the cases of tumour tend to present higher wave V latency than the false negatives, but, at the same time, there is a dispersion and overlapping of values, thus making any attempt to make a clear distinction between the two groups impossible (Fig. 1).
In other words, regardless of the diagnostic criterion used to evaluate wave V latency, it appears impossible to reduce the number of false positives without increasing (further and unacceptably) the number of false negatives.
Likewise, it is obvious that the interpretation of an ABR must not be based on one evaluation parameter alone.
It has, however, already been pointed out that the formulas for correcting wave V latency in relation to the degree of hearing loss are not completely reliable 7 just as the intrinsic diagnostic potentiality of this method has been criticised 3.
The finding of a high percentage of “false positives” and the by no means negligible incidence of “false negatives” show, however, that with the diagnostic criteria currently used it is not possible, in a certain number of cases, to distinguish between a cochlear and a retro-cochlear alteration, or at least a retro-cochlear alteration dependent upon expansive lesions or other disorders that can be detected with MRI.
The real incidence of acoustic neuromas in the event of unilateral (or asymmetrical) perceptive hearing loss was recently estimated at 2.1% 19, while their casual finding in patients studied for others reasons occurs in 1-0.07% of cases 20 21. On the other hand, as far as sudden hearing loss is concerned, the finding of an acoustic neuroma varies considerably in the different series, being generally low (0.8-5%), but with peaks of 30-47.5% 22–24.
Considering the overall data obtained, it is, therefore, logical to expect that a very large number of MRI scans (probably more than 90%) performed for first instance diagnostic investigation of unilateral hearing loss will be negative. This represents the main criticism of MRI by those who have to limit health spending and manage the waiting lists for this examination.
The characteristics of our study (retrospective evaluation of cases that all, in some way, had an altered electrophysiological response) do not allow us to substantially contribute to the data already available on the sensitivity and specificity of ABRs.
Calculation of these indicators does, in fact, presume that even cases with a normal ABR or not suspected of having a retro-cochlear lesion should be submitted to MRI in order both to identify false negatives (as regards sensitivity) and confirm true negatives (as regards specificity). Furthermore, in order to obtain realistic estimates (given the substantially low incidence of acoustic neuromas in a population with sensorineural hearing loss) it would be necessary to study systematically, and in sequence, a vast series of cases with ABR and MRI in order to include a sufficient number of neuromas of various sizes, a fundamental aspect for the sensitivity of the method. It has, in fact, already been pointed out 6 that the diagnostic performance of ABRs has always been calculated on selected populations with cerebellopontine angle tumours.
In conclusion, data in the literature and our findings confirm that the study of brainstem evoked hearing potentials in otoneurological diagnosis is hindered by a high percentage of false positives which apparently, based on current knowledge, cannot be reduced. If we then add the substantial number of false negatives and the fact that this method has very limited applications in cases of severe hearing loss, it is quite reasonable to question, as other Authors have done 3, the true usefulness of ABRs in otoneurological diagnosis.
However, the need to limit health costs and the difficulty in accessing MRI support the use of ABRs which, nonetheless, may possibly lead to postponement of the neuroradiological examination and also avoid a certain number of tests in patients considered clinically to have a low risk of neuroma, in subjects who cannot access MRI (or alternatively CT with contrast medium) and in cases in which the general clinical situation, in any case, is a contraindication for non strictly indispensable neurosurgery.
References
- 1.Thornton ARD. An evaluation of the application of auditory brain stem response to the detection of VIIIth nerve tumours. In: Filipo R, Barbara M, editors. Acoustic Neuroma: trends and controversies. The Hague: Kugler Publications; 1999. p. 37-52. [Google Scholar]
- 2.Don M, Masuda A, Nelson R, Brackmann D. Successful detection of small acoustic tumors using the stacked derived-band auditory brain stem response amplitude. Am J Otol 1997;18:608-21. [PubMed] [Google Scholar]
- 3.Wilson DF, Talbot JM, Mills M. A critical appraisal of the role of auditory brain stem response and magnetic resonance imaging in acoustic neuroma diagnosis. Am J Otol 1997;18:673-81. [PubMed] [Google Scholar]
- 4.Quaranta A, Zini C. Il neurinoma dell’acustico: reperti clinico-funzionali, risultati e complicanze chirurgiche. Acta Otorhinolaryngol Ital 2001;S68:1-20. [PubMed] [Google Scholar]
- 5.Rupa V, Job A, George M, Rajashekar V. Cost/effective initial screening for vestibular schwannoma: auditory brain stem response or magnetic resonance imaging? Otolaryngol Head Neck Surg 2003;128:823-8. [DOI] [PubMed] [Google Scholar]
- 6.Prosser S, Turrini M. Strategia audiometrica nella diagnostica differenziale cocleare/retrococleare. In: Grandori F, Martini A, editors. Potenziali evocati uditivi: basi teoriche ed applicazioni cliniche. Padova: Piccin Nuova Libraria SpA; 1995. p. 255-62. [Google Scholar]
- 7.Josey AF. Le risposte uditive evocate tronco-encefaliche nella topodiagnosi di lesione. In: Katz J, editor. Trattato di Audiologia Clinica. Edizione italiana a cura di Martini A. Padova: Piccin Nuova Libraria SpA; 1994. p. 487-500. [Google Scholar]
- 8.Starr A, Achor J. Auditory brainstem response in neurological disease. Arch Neurol 1975;32:761-8. [DOI] [PubMed] [Google Scholar]
- 9.Stockard JJ, Rossiter WS. Clinical and pathological correlates of brainstem auditory response abnormalities. Neurology 1977;27:316-25. [DOI] [PubMed] [Google Scholar]
- 10.Selters W, Brackman D. Acoustic tumour detection with brain stem electric response audiometry. Arch Otolaryngol 1977;103:181-7. [DOI] [PubMed] [Google Scholar]
- 11.Prosser S, Arslan E, Conti G, Michelini S. Evaluation of the monoaurally evoked brainstem response in the diagnosis of sensorineural hearing loss. Scand Audiol 1983;12:103-6. [DOI] [PubMed] [Google Scholar]
- 12.Prosser S, Arslan E. Prediction of auditory brainstem response wave V latency as a diagnostic tool in diagnosis of sensorineural hearing loss. Audiology 1987;26:179-87. [PubMed] [Google Scholar]
- 13.Montaguti M, Zanetti MA, Zacchini T. La valutazione della latenza dell’onda V nella diagnosi differenziale delle ipoacusie neurosensoriali. Audiologia Italiana 1986;III:20-4. [Google Scholar]
- 14.Rosenhamer H. The auditory evoked brain stem electric response (ABR) in cochlear hearing loss. Scand Audiol 1981;S13:83-93. [PubMed] [Google Scholar]
- 15.Terkildsen K, Osterhammel I, Thomsen J. The ABR and MLR in patients with acoustic neuromas. Scand Audiol 1981;S13:103-7. [PubMed] [Google Scholar]
- 16.Quaranta A, Scaringi A, Quaranta N. Auditory brain stem responses, otoacoustic emissions and efferent acoustic reflexes in ears with vestibular schwannoma. VS121 – IVth Int. Conf. on Vestibular Schwannoma and others CPA lesions. Cambridge, 13-17 July 2003. [Google Scholar]
- 17.Skinner LJ, Piccirillo E, Agarwal M, Falcioni M, Sanna M. A retrospective correlation of ABR and magnetic resonance imaging for acoustic neuromas/vestibular schwannomas. VS046 – IVth Int. Conf. on vestibular schwannoma and others CPA lesions. Cambridge, 13-17 July 2003. [Google Scholar]
- 18.Prosser S, Martini A. ABR in rapporto all’audiogramma (ipoacusia da lesione periferica). In: Grandori F, Martini A, editors. Potenziali evocati uditivi: basi teoriche ed applicazioni cliniche. Padova: Piccin Nuova Libraria SpA; 1995. p. 173-6. [Google Scholar]
- 19.Urben SL, Benninger MS, Gibbens ND. Asymmetric sensorineural hearing loss in a community-based population. Otolaryngol Head Neck Surg 1999;120:809-14. [DOI] [PubMed] [Google Scholar]
- 20.Selesnick SH, Deora M, Drotman M, Heier LA. Incidental discovery of acoustic neuromas. Otolaryngol Head Neck Surg 1999;120:815-8. [DOI] [PubMed] [Google Scholar]
- 21.Anderson TD, Loevner LA, Bigelow DC, Mirza N. Prevalence of unsuspected acoustic neuroma found by magnetic resonance imaging. Otolaryngol Head Neck Surg 2000;122:643-6. [DOI] [PubMed] [Google Scholar]
- 22.Chaimoff M, Nageris BI, Sulkes J, Spitzer T, Kalmanovitz M. Sudden hearing loss as presenting symptom of acoustic neuroma. Am J Otolaryngol 1999;20:157-60. [DOI] [PubMed] [Google Scholar]
- 23.Saunders JE, Luxford WM, Devgan KK, Fetterman BL. Sudden hearing loss in acoustic neuroma patients. Otolaryngol Head Neck Surg 1995;113:23-31. [DOI] [PubMed] [Google Scholar]
- 24.Fitzgerald DC, Mark AS. Sudden hearing loss: frequency of abnormal findings on contrast enhanced MR studies. Am J Neuroradiol 1988;19:1433-6. [PMC free article] [PubMed] [Google Scholar]