Summary
Fibrous histiocytoma is a benign tumour composed of a mixture of fibroblastic and histiocytic cells. Based on the location of this tumour, fibrous histiocytoma are usually divided into cutaneous types and those involving deep tissues. These lesions most often arise on the skin, but may rarely occur in soft deep tissues. The diagnosis of fibrous histiocytoma may be clinically difficult when the lesion is located in the deep tissues, and is frequently confirmed after local excision. The most important diagnostic distinction is the separation of this tumour from aggressive forms of fibrohistiocytic neoplasms, including dermatofibrosarcoma protuberans and malignant fibrous histiocytoma. A 19-year-old male presented with a painless swelling on the right cheek. Detailed clinical and laboratory examinations were performed. The lesion had been totally excised under local anaesthesia, and histopathology revealed a benign fibrous histiocytoma. The diagnosis, location, treatment and prognosis of fibrous histiocytoma are also discussed.
Keywords: Benign tumour, Cheek, Benign Fibrous Histiocytoma
Riassunto
Il fibroma istiocitario è un tumore benigno composto da fibroblasti e istiociti. In base alla sede di questo tumore, i fibromi istiocitari sono divisi solitamente nei tipi cutanei ed in quelli che coinvolgono i tessuti profondi. Queste lesioni si presentano spesso sulla cute, mentre possono riscontrarsi raramente nei tessuti molli profondi. La diagnosi clinica del fibroma istiocitario può essere difficile quando la lesione è situata in profondità e frequentemente se ne ha conferma solo dopo l’asportazione. La distinzione diagnostica più importante è la differenziazione di questo tumore dalle forme aggressive del tumore fibroistiocitario, compreso il dermatofibrosarcoma protuberans e l’istiocitoma fibroso maligno. Caso clinico: un paziente maschio di 19 anni si presenta con tumefazione non dolorosa alla guancia destra. Vengono effettuati gli esami di laboratorio e clinici. La lesione viene completamente asportata in anestesia locale. L’esame istologico ha rivelato un istiocitoma fibroso benigno. Sono discussi la diagnosi, la sede, il trattamento e la prognosi del fibroma istiocitario.
Introduction
Fibrous histiocytoma (FH) is a benign tumour composed of a mixture of fibroblastic and histiocytic cells. This tumour most frequently occurs in the dermis, but is also sporadically found in soft tissue and parenchymal organs. The benign FH usually originates in sun-exposed skin and in orbital tissues, whereas the occurrence of this lesion in deep soft tissues of the head and neck has rarely been reported. The term cutaneous FH is usually used to refer to all superficial tumours of skin regardless of appearance. Similar lesions involving subcutis or deep structures will only be referred as FH 1 2. These neoplasms should be differentiated from the malignant FH, which frequently has a rather aggressive malignant course 3 4.
In the present study, a case with subcutaneous FH on the cheek is described. From a thorough search of the literature, only 6 cases with subcutaneous benign FH of the head and neck area were found, only two of which located on the cheek 1 2 5 (Table I).
Table I. Review of literature of subcutaneous fibrous histiocytomas of head and neck.
| No. | Ref. | Site | Age yrs | Sex | Treatment | Follow-up,outcome |
| 1. | Fletcher, 1990 | Subcutaneous face | 45 | M | LE*X2 | †Re at 2 Y ‡NED after 8Y |
| 2. | Fletcher, 1990 | Intramuscular scalp | 31 | M | LE | 9 M, NED |
| 3. | Fletcher, 1990 | Subcutaneous scalp | 58 | F | LE | 10 M, NED |
| 4. | Fletcher, 1990 | Subcutaneous scalp | 10 | F | LE | **NA |
| 5. | Fletcher, 1990 | Subcutaneous cheek | 60 | M | LE | NA |
| 6. | Fletcher, 1990 | Intramuscular cheek | 56 | M | LE | NA |
| 7. | Our case | Subcutaneous cheek | 22 | M | LE | 4 Y, NED |
LE: Local excision;
Re: recurrence;
NED: no evidence of disease;
NA: information not available
Case report
A 19-year-old male presented in our ENT outpatient clinic, with an apparently painless swelling on the right cheek, complaining of a lesion that appeared 4 years previously. His past medical history was negative, apart from mild acne compatible with his age.
The clinical examination revealed a mass about 3 x 4 cm on the right cheek, of skin colour and hard consistency, which was not attached to the subcutaneous tissue or to the skin. The lesion had been increasing slightly in size over the last 6 months. Small, painless, mobile lymph nodes, on the right submandibular triangle, were also palpable.
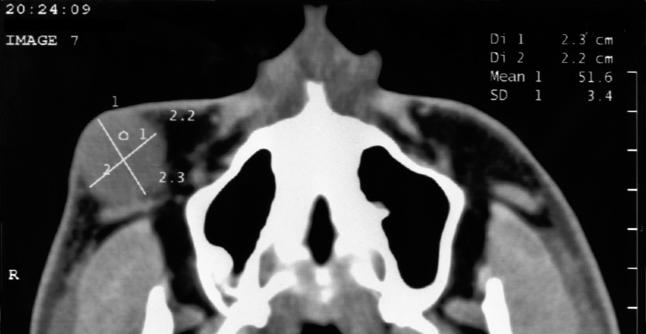
Full blood count, erythrocyte sedimentation rate, renal urea and creatinine, as well as, liver tests were all within normal limits. Echography and Doppler echography of the mass suggested a lesion of vascular origin. A computed tomography scan was performed with administration of intravenous contrast, which revealed a mass of soft tissue, the dimensions of which were 3 x 3.5 cm (Fig. 1). The lesion had well-defined borders, not infiltrating the surrounding tissues. These radiologic findings were not compatible with the diagnosis of a lymph node, but were rather indicative of a benign vascular lesion.
Fig. 1.
CT scan shows homogenous enhancement of mass on right cheek.
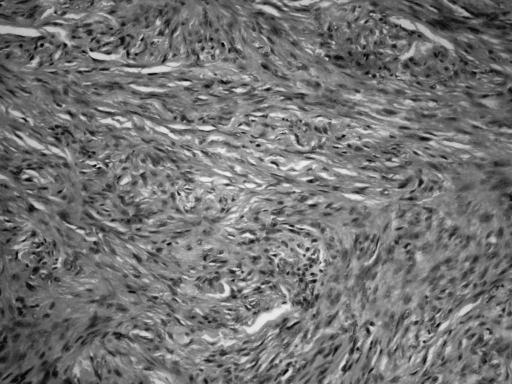
The lesion, of whitish colour and of fibroelastic consistency, had been totally excised under local anaesthesia. Pathology examination revealed a neoplasm of mesenchymal origin, rich in cells with morphology and immunohistochemical characters compatible with benign fibrous histiocytoma (Fig. 2). Immunohistochemical staining demonstrated positivity for CD68 (monoclonal, clonePG-M1 dilution 1:50, Dako) (Fig. 3A) and Vimentin (monoclonal, clone V9, dilution 1:50, Dako) (Fig. 3B), and negativity for smooth muscle actin (SMA) (monoclonal, clone 1A4, dilution 1:50, Dako) (Fig. 3C), S-100 protein (polyclonal, dilution 1:400, Dako) (Fig. 3D), CD34 (monoclonal, clone QBend 10 dilution 1:50, Dako) and factor XIIIa (polyclonal, dilution 1:200, Biocave). Microscopic and immunohistochemical examinations confirmed the diagnosis of benign fibrous histiocytoma. The patient is asymptomatic with no evidence of recurrent disease after a 4-year follow-up.
Fig. 2.
Irregularly arranged collagen fibres mixed with scattered proliferating fibroblasts (Histiocytoma, fibrous type), X200, H + E.
Fig. 3.
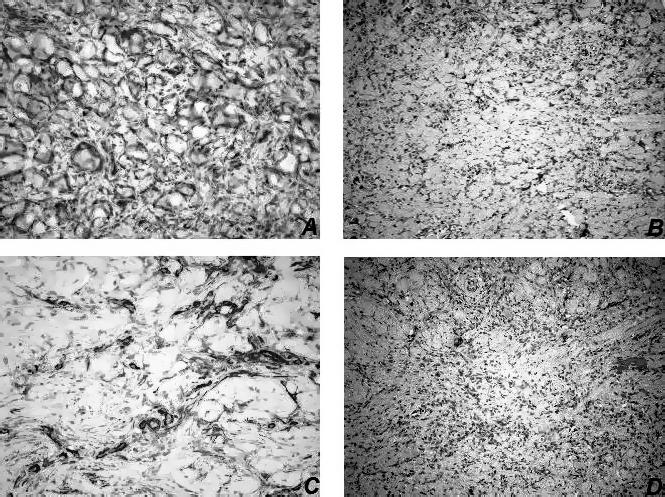
Immunohistochemical staining demonstrated positivity for CD68 (A) and Vimentin (B), and negativity for smooth muscle actin (SMA) (C) and S-100 (D).
Discussion
Benign FH was not known as a clinical entity before 1970 when, as a result of the development of immunohistochemical techniques and electronic microscopy, differential diagnosis became feasible 6 7.
The diagnosis of FH may be difficult clinically when the lesion is located in the deep tissues, and is frequently confirmed after local excision. Histopathologically, this tumour is a neoplasm of histiocytic origin and is composed of a biphasic cell population of histiocytes and fibroblasts 8. This accounts for the dual population of histiocytic and fibrous elements commonly seen in this tumour. According to other Authors, the histiocyte originates from an undifferentiated mesenchymal stem cell 9. In our case, immunohistochemistry was performed for differential diagnosis, showing similar features on microscopic examination. The positivity for CD68 and vimentin demonstrated that the lesion was composed of histiocytic cells and fibroblast-like cells on immunohistochemistry, and the negativity for SMA and S-100 could differentiate the lesion from leiomyosarcoma and neurogenic tumours 10.
The most important diagnostic distinction is the separation of this tumour from aggressive forms of fibrohistiocytic neoplasms, including dermatofibrosarcoma protuberans and malignant FH 11 12. As with benign FH, the diagnosis of malignant FH frequently relies upon immunohistochemistry and electron microscopy to differentiate it from other lesions.
Malignant FH is composed of malignant pleomorphic sarcomatous cells, bizarre giant cells, and frequent mitotic figures 13. Histologic features, unfortunately, play a minor role in predicting the biologic behaviour of these neoplasms. The presence of certain atypical histological features, including necrosis, marked cellular and mitotic activity, does not correlate well with clinical recurrence 3 11 14.
The difference between benign and malignant FH is usually obvious, because the latter is a pleomorphic, deeply situated tumour with numerous typical and atypical mitotic figures and prominent areas of haemorrhage and necrosis. Less obvious, however, is the difference between this tumour and the angiomatoid form of FH. The latter is a tumour occurring usually in childhood characterized by sheets of histiocytic cells interrupted by cystic areas of haemorrhage. These are surrounded by a dense cuff of lymphocytes and plasma cells, but hardly ever possess giant cells and xanthoma cells like the FH 11 14 15.
Like FH, dermatofibrosarcoma protuberans occurs in the dermis and subcutis, but is more apt to show extensive subcutaneous involvement than benign FH. It is also characterized by a more uniform cellular population and lacks giant cells, inflammatory cells, and xanthomatous elements. Its fascicles, composed of slender attenuated cells, are longer and arranged in a distinct storiform pattern, unlike the short curlicue fascicles of FH. Its margins are infiltrative in contrast to the well-defined margins of FH. Immunostaining also reveals distinct differences in the cellular composition of these tumours. Fibrous histiocytomas contain a significant population of factor XIIIa-positive cells, although it has been debated whether these cells represent a population of neoplastic cells or a peculiar infiltrate that accompanies the tumour. In contrast, dermatofibrosarcoma protuberans contains only scattered factor XIIIa-positive cells, but, in striking contrast to benign FH, it expresses CD34 in a significant portion of neoplastic cells. The combination of these two stains has proved to be highly reliable in distinguishing these two lesions, which often cause diagnostic problems, particularly when only a superficial biopsy specimen is available for assessment 12 14–16.
FH, based on the location, are usually divided into cutaneous types and those involving deep tissues 2 5. These lesions usually arise on the skin, but may very occasionally occur in soft deep tissues 1 6. Non-cutaneous benign FH represents approximately 1% of all benign FH lesions. This tumour has been associated with a previous trauma, sun exposure, and chronic infection, rather suggesting that it represents a reactive proliferation of benign cells. Benign FH of the non-cutaneous soft tissues of the head and neck most often develops as a painless mass with specific symptoms caused by interference with the normal anatomy and physiology of the area in which they arise 1 11.
Specific sites of involvement, on the head and neck region, described in the literature, include buccal mucosa, submandibular triangle, oral tongue, larynx, nasal cavity, mandible and supraclavicular fossa 1 5 6 11 17 18. Usually, these lesions appear very well circumscribed (often being encapsulated) and the cut surface is firm and pale to yellowish-brown in colour. There is no macroscopic evidence of necrosis but sometimes the lesions are focally cystic, presenting haemorrhage within. The maximum diameter has been reported to range from 2 to 12 cm 5. It is worthwhile pointing out that the majority of lesions had only been shelled out, a fact that almost certainly contributed to the high local recurrence rate 1. All lesions proved to be solitary, none being related to a joint. Clinically, most lesions presented as a painless, slowly growing mass, the pre-operative duration ranging from 3 to 12 months 5 6 11.
The ages of the patients emerging from a review of the literature varied from 1 to 70 years, while the patient described in this report was 19 years old. The male-to-female ratio in the literature review was 2.5:1 6. This tumour of the head and neck usually develops as a painless mass with specific symptoms caused by interference with the normal anatomy and physiology of the area in which they are found. The most commonly reported initial symptoms were nasal obstruction, epistaxis, dysphagia and dyspnoea. When the mass is located posteriorly in the oral cavity or tongue, patients may present dysphagia, dyspnoea, snoring, or a combination of these symptoms 6. Our patient presented a mass on the cheek, associated with swelling, without other symptoms.
Most lesions were treated by local excision without sacrificing structures that would cause major functional or cosmetic morbidity. Our patient was submitted to complete local excision with clear margins without any morbidity. These lesions have no metastatic potential and generally good prognosis. Of the cases with follow-up reported in the literature, only 2 (11%) out of 18 had a recurrence after a local excision 1 10. The reason for these recurrences is unknown, as is the adequacy of the margins of resection. If the surgical margins were reported to be free of tumour, local recurrences were uncommon. Radiation therapy and chemotherapy have no role in the management of benign FH 1 6.
References
- 1.Bielamowicz S, Dauer MS, Chang B, Zimmerman MC. Non-cutaneous benign fibrous histiocytoma of the head and neck. Otolaryngol Head Neck 1995;113:140-6. [DOI] [PubMed] [Google Scholar]
- 2.Batsakis JG. Fibrous lesions of the head and neck: Benign, malignant and indeterminate. In: Batsakis JG, editor. Tumours of the head and neck. 2nd edn. Baltimore, MD: Williams & Wilkins; 1979. p. 252-79. [Google Scholar]
- 3.Sullivan BO, Audel N, Catton CN, Gullane PJ. Soft tissue and bone sarcomas of the head and neck. In: Harrison LB, Sessions RB, Hong WK, editors. Head and Neck Cancer. 2nd edn. Philadelphia, PA: Lippincott Williams & Wilkins; 2004. p. 786-823. [Google Scholar]
- 4.Femiano F, Scully C, Laino G, Battista G. Benign fibrous histiocytoma of the cheek: CD 68-KP1 positivity. Oral Oncol 2001;37:673-5. [DOI] [PubMed] [Google Scholar]
- 5.Fletcher CD. Benign fibrous histiocytoma of subcutaneous and deep soft tissue: a clinicopathologic analysis of 21 cases. Am J Surg Pathol 1990;14:801-9. [PubMed] [Google Scholar]
- 6.Hong KH, Kim YK, Park JK. Benign fibrous histiocytoma of the floor of the mouth. Otolaryngol Head Neck Surg 1999;121:330-3. [DOI] [PubMed] [Google Scholar]
- 7.Kamino H, Salcedo E. Histopathologic and immunohistochemical diagnosis of benign and malignant fibrous and fibrohistiocytic tumours of the skin. Dermatol Clin 1999;17:487-505. [DOI] [PubMed] [Google Scholar]
- 8.Calonje E, Mentzel T, Fletcher CD. Cellular benign fibrous histiocytoma. Clinicopathologic analysis of 74 cases of a distinctive variant of cutaneous fibrous histiocytoma with frequent recurrence. Am J Surg Pathol 1994;18:668-76. [PubMed] [Google Scholar]
- 9.Wilk M, Zelger BG, Nilles M, Zelger B. The value of immunohistochemistry in atypical cutaneous fibrous histiocytoma. Am J Dermatopathol 2004;26:367-71. [DOI] [PubMed] [Google Scholar]
- 10.Fletcher CD, Gustafson P, Rydholm A, Willen H, Akerman M. Clinicopathologic re-evaluation of 100 malignant fibrous histiocytomas: prognostic relevance of subclassification. J Clin Oncol 2001;19:3045-50. [DOI] [PubMed] [Google Scholar]
- 11.Blitzer A, Lawson W, Zak FG, Biller HF, Som ML. Clinical-pathological determinants in prognosis of fibrous histiocytoma of the head and neck. Laryngoscope 1981;91:2053-70. [DOI] [PubMed] [Google Scholar]
- 12.Chen TC, Kuo T, Chan HL. Dermatofibroma is a clonal proliferative disease. J Cutan Pathol 2000;27:36-9. [DOI] [PubMed] [Google Scholar]
- 13.Billings SD, Folpe AL. Cutaneous and subcutaneous fibrohistiocytic tumours of intermediate malignancy: an update. Am J Dermatopathol 2004;26:141-55. [DOI] [PubMed] [Google Scholar]
- 14.Mentzel T, Kutzner H, Rutten A, Hugel H. Benign fibrous histiocytoma (dermatofibroma) of the face: clinicopathologic and immunohistochemical study of 34 cases associated with an aggressive clinical course. Am J Dermatopathol 2001;23:419-26. [DOI] [PubMed] [Google Scholar]
- 15.Van Laer C, Hamans E, Neetens I, Van Marck E, Van Oosterom A, Van de Heyning P. Benign fibrous histiocytoma of the larynx: presentation of a case and review of the literature. J Laryngol Otol 1996;110:474-7. [DOI] [PubMed] [Google Scholar]
- 16.Enzinger FM, Weiss SW. Benign fibrohistiocytic tumours. In: Enzinger FM, Weiss SW, editors. Soft Tissue Tumours. St Louis: Mosby; 1995. p. 293-303. [Google Scholar]
- 17.Shrier DA, Wang AR, Patel U, Monajati A, Chess P, Numaguchi Y. Benign fibrous histiocytoma of the nasal cavity in a newborn: MR and CT findings. Am J Neuroradiol 1998;19:1166-8. [PMC free article] [PubMed] [Google Scholar]
- 18.Heo MS, Cho HJ, Kwon KJ, Lee SS, Choi SC. Benign fibrous histiocytoma in the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;97:276-80. [DOI] [PubMed] [Google Scholar]