Summary
The presence of multiple calculi in the major salivary glands is an uncommon finding. Sjögren’s syndrome is a chronic autoimmune disease characterized by lymphocyte-mediated destruction of the exocrine glands. The case is presented of a 49-year-old female with Sjögren’s syndrome found to have bilateral multiple sialolithiasis in the parenchyma of the parotid glands. The patient presented with a right sided painful inflamed swelling of the parotid region. Even though she had been diagnosed with primary Sjögren’s syndrome 3 years prior to admission, she did not report any previous episode of sialadenitis. Full blood count showed leukocytosis (white blood cells = 14,900/106L) with neutrophilia (75%). Radiological assessment included ultrasound and computed tomography scan of the parotids which demonstrated intra-parenchymal multiple calculi of both parotid glands and obstruction of the right Stensen’s duct. The patient was treated with intravenous antibiotics and anti-inflammatory drugs. On the second day of hospitalisation, she reported spontaneous extrusion of a calculus during massage of the gland, with immediate relief of symptoms. In patients with Sjögren’s syndrome and radiological findings of calculi in the major salivary glands, close observation is mandatory for better control of recurrent sialadenitis and early recognition of mucosa-associated lymphoid tissue lymphomas.
Keywords: Parotid gland, Sialolithiasis, Sjögren’s syndrome
Riassunto
La presenza di calcolosi multipla nelle ghiandole salivari maggiori non è frequente. La sindrome di Sjögren è un disordine autoimmune caratterizzato da distruzione cellulo-mediata delle ghiandole esocrine. Presentiamo il caso di una paziente di 49 anni con sindrome di Sjögren in cui si è osservata scialolitiasi bilaterale multipla delle ghiandole parotidi. La paziente si è presentata con gonfiore dolente della parotide destra. Nonostante la diagnosi di sindrome di Sjögren tre anni prima la paziente non aveva mai presentato episodi di scialoadenite. Gli esami di laboratorio hanno evidenziato una leucocitosi (14.500 WBC) con neutrofilia (75%) e le indagini radiologiche (esame ecografico e CT) hanno dimostrato la presenza di numerosi calcoli nel parenchima delle ghiandole parotidi, e l’ostruzione del dotto di Stenone destro. Antibiotici e farmaci anti-infiammatori sono stati somministrati per via endovenosa; al secondo giorno di ricovero, durante il massaggio manuale della ghiandola, si è verificata l’esplusione spontanea di un calcolo dalla ghiandola parotide destra, con immediato miglioramento dei sintomi. I pazienti affetti da sindrome di Sjögren e con reperti radiologici positivi per calcolosi delle ghiandole parotidi devono essere seguiti nel tempo, per meglio controllare possibili recidive di scialoadenite e poter effettuare la diagnosi precoce di un MALT linfoma, eventualmente associato.
Introduction
Sjögren’s syndrome is a chronic inflammatory disease of the exocrine glands that affects primarily females. It is clinically characterized by dry eyes (kerato-conjuctivitis sicca) and dry mouth (xerostomia). Histological findings include lymphocytic infiltration and destruction of the salivary and lacrimal glands 1 2. Primary Sjögren’s syndrome can cause serious parotid morbidity secondary to inflammation and infection. Furthermore, in some patients, Sjögren’s syndrome is associated with lithiasis of the major salivary glands 3. Although sialolithiasis occurs mainly in the submandibular gland (72-94%) 4, patients with Sjögren’s syndrome more frequently present with lithiasis of the parotid gland 4. Multiple salivary stones are rarely reported, and they potentially exist in higher frequency in patients with severe Sjögren’s syndrome 5.
Although no epidemiological data are available concerning the incidence of sialolithiasis in Sjögren’s syndrome, the presence of multiple calculi in the parotid glands is considered extremely rare 5 6.
Patients with Sjögren’s syndrome present a significant risk of developing mucosa-associated lymphoid tissue (MALT) lymphomas, often occurring as parotid masses 7, for which close follow-up is mandatory.
We present a case of a female patient with primary Sjögren’s disease and bilateral multiple calculi of the parotids who presented in our Hospital with her first episode of sialadenitis of the right parotid gland after a 3-year history of the disease.
Case Report
A 49-year-old female patient presented to the ENT emergency outpatient clinic of our Hospital, suffering from a painful inflammatory swelling on the right side of the face. Onset of the swelling was sudden and appeared during a mealtime. The patient had been diagnosed with primary Sjögren’s syndrome, 3 years before admission but did not report any previous episode of sialadenitis.
Upon physical examination, the right parotid region was diffusely swollen and painful to palpation. There was no cervical or other palpable lymphadenopathy. A purulent discharge was expelled from the right Stensen duct ostium during massaging of the gland.
The initial laboratory examinations consisted of blood tests and an ultrasound (US) examination of the parotid region. Full blood count demonstrated leukocytosis (WBC 14,500/106L), with neutrophilia (75%). Sonography revealed multiple hypoechoic areas, hyperechoic lines and spots (microliths) in both parotid glands. The right parotid gland was markedly enlarged in size due to oedema and the right Stensen’s duct was occluded by a sialolith (Fig. 1).
Fig. 1.
US examination of parotid glands revealing obstruction of hilum of right Stensen’s duct by a calculus (black arrow). Pa-renchymal heterogeneity with presence of hypoechoic areas (white arrows).
Since Sjögren’s syndrome is related to MALT lymphomas 7, and the US examination was inconclusive showing parenchymal heterogeneity of the parotids, a computed tomography (CT) scan was performed in order to exclude the presence of malignancy. CT scan confirmed the diagnosis of acute sialadenitis in the right parotid gland due to obstruction and revealed the presence of multiple sialoliths in both parotid glands (Fig. 2). Salivary gland involvement in Sjögren’s syndrome is usually confirmed by X-ray sialography 8. In our case, the diagnosis of Sjögren’s syndrome had already been made and sialography would have exposed the patient to ionized radiation without gaining any additional information.
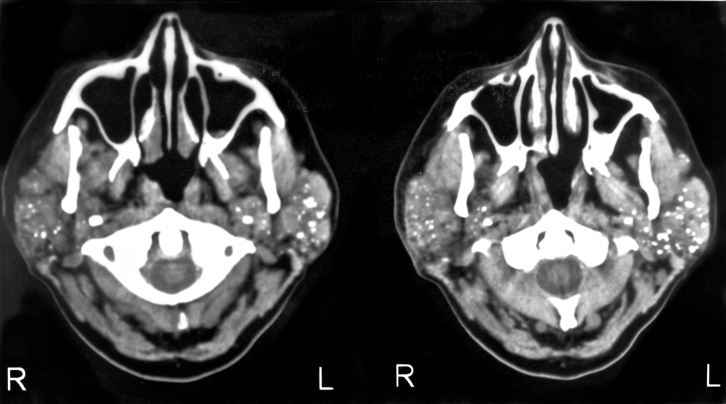
Fig. 2.
CT scan of parotid regions (two axial sections) showing multiple calculi in parenchyma of both parotid glands (superficial and deep lobe of glands).
The patient was hospitalized and treated with intravenous administration of antibiotics (amoxicillin with clavoulanic acid 1.2 g tid and metronidazole 500 mg bd) anti-inflammatory drugs, and massage of the right parotid area. On the second day of her hospital stay, the patient reported spontaneous extrusion of a calculus during massage of the gland with immediate relief of symptoms. The patient was discharged after 4 days of hospital stay, free of symptoms and in good general conditions. At follow-up, 6 months later, the patient did not report any further episodes of sialadenitis or parotid swelling in response to eating. The patient remains under observation with regular follow-up in the ENT outpatient clinic.
Discussion
Sjögren’s syndrome is associated with scarring and scattered inflammation of the salivary glands. Sialolithiasis is uncommon in Sjögren’s syndrome with limited documented epidemiological data 5 6 9.
The presence of multiple, bilateral calculi in the parenchyma of the parotids in Sjögren’s syndrome patients, as seen in our case, is very rare with only a few reports appearing in the current literature 5 6. Shimizu et al. 5 reported that multiple microliths potentially exist in higher frequency in patients with severe Sjögren’s syndrome. However, in our case, the patient had a 3-year history of diagnosed Sjögren’s syndrome and did not report any previous episodes of sialadenitis and described her symptoms (xerostomia, kerato-conjuctivitis sicca) as mild.
The typical initial symptoms of patients with Sjögren’s syndrome are dry eyes and mouth. However, sialadenitis caused by atypical inflammation or obstruction of Stensen’s duct, due to a sialolith, is occasionally the first presentation of Sjögren’s syndrome 9. The mechanism of stone formation in Sjögren’s disease is not yet completely known. Reduced salivary flow and high concentration in saliva of calcium salts may be possible aetiologic factors 10. Calculi generally consist of a mixture of various calcium phosphates (hydroxyl-apatite, carbonate-apatite) together with an organic matrix 11. An initial organic nidus progressively grows by deposition of layers of organic and inorganic substances 11. A more inorganic calculus is more radio-opaque and can be more easily detected in plain X-rays. The use of US in the diagnostic work-up solved these problems as calculi > 2 mm can be identified, independently of their composition.
When assessing patients with parotid swelling, physical examination should always include palpation of the gland and simultaneous observation of salivary flow from Stensen’s duct ostium. Initial assessment must include US examination of the parotid glands. When US findings (parenchymal heterogeneity, multiple calcifications) cannot exclude the synchronous presence of a MALT lymphoma or pseudotumour of the parotid gland, a CT scan is required.
The risk of malignant lymphoma development in Sjögren’s syndrome patients, is approximately 44 times greater than that of the general population.
The significant risk of MALT lymphoma development 7–12 often presenting as parotid masses, justifies a very close monitoring of these patients.
The approach in complicated cases, presenting as sialadenitis, includes aggressive medical treatment with intravenous antibiotics, antinflammatory drugs and analgesia. Sialagogues (chewing gum, sour drops) are also used in the acute phase of a sialadenitis episode and the long-term management of Sjögren’s syndrome 13.
Some Authors have suggested hypercalcaemia as a causative factor of stone formation in an animal model 14. However, this has not yet been proven in humans and thus a preventive diet, regarding the calcium concentration does not exist in the current literature.
Surgical intervention, if required, consists of minimal invasive techniques, such as, stone removal with Dormia basket, under endoscopic (sialendoscopy) 15 or radiological (sialography) 16 guidance, and shock-wave lithotripsy under US guidance 17. However, the Dormia basket techniques are limited to removal of stones located in the duct up to the hilum of the gland but are not feasible for parenchymal stones. Another limitation of these techniques concerns the size of the stones, as only calculi with a diameter < 5 mm can be removed from the parotid ductal system 15. The treatment of choice, for parotid stones not responding to conservative treatment, is extra-corporeal shock-wave lithotripsy under sonographic control. This treatment can be carried out independently of the location, size and number of calculi and can be repeated if required. This method is reported to be effective, with patients stone-free in 50-60% and symptom-free in 80-90% 18. Albeit, although lithotripsy is a useful technique, there is the potential risk of parenchymal damage and fibrosis of the gland 18.
Parotidectomy should be considered as the last treatment option, in patients with multiple stones (> 3 stones) in the same gland, recurrent episodes of sialadenitis and after failure of minimal invasive techniques and shock-wave lithotripsy 18.
References
- 1.Bloch KJ, Buchanan WW, Bunium JJ. Sjögren’s syndrome: a clinical and serological study of sixty-two cases. Medicine 1965;44:187-273. [PubMed] [Google Scholar]
- 2.Moutsopoulos HM. Sjögren’s syndrome: autoimmune eprithelitis. Clin Immunol Immunopathol 1994;72:162-5. [DOI] [PubMed] [Google Scholar]
- 3.Lustmann J, Regev E, Melamed Y. Sialolithiasis. A survey on 245 patients and a review of the literature. Int J Oral Maxillofac Surg 1990;19:135-8. [DOI] [PubMed] [Google Scholar]
- 4.Zenk J, Gottwald F, Bozzato A, Iro H. Speichelsteine der Glandula submandibularis. HNO 2005;53:243-9. [DOI] [PubMed] [Google Scholar]
- 5.Shimizu M, Yoshiura K, Nakayama E, Kanda S, Nakamura S, Ohyama Y, et al. Multiple sialolithiasis in the parotid gland with Sjögren’s syndrome and its sonographic findings – Report of three cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:85-92. [DOI] [PubMed] [Google Scholar]
- 6.Wickramasinghe A, Howarth A, Drage N. Multiple bilateral parotid sialoliths in a patient with mucosa-associated lymphoid tissue lymphoma (MALT lymphoma) of the salivary glands. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:496-8. [DOI] [PubMed] [Google Scholar]
- 7.Voulgarelis M, Dafni UG, Isenberg DA, Moutsopoulos HM, and Members of the European Concerted action on SS: Jonsson R, Haga H-J, et al. Malignant lymphoma in primary Sjögren’s syndrome – A multicenter retrospective clinical trial by the European Concerted action on Sjögren’s syndrome. Arthritis Reum 1999;42:1765-72. [DOI] [PubMed] [Google Scholar]
- 8.Hisao T, Yoshimi O, Munetaka M, Yasuaki K, Hajime Y, Kotaro H, et al. MR Sialography in patients with Sjögren’s syndrome. Am J Neuroradiol 1998;19:1199-203. [PMC free article] [PubMed] [Google Scholar]
- 9.Nahlieli O, London D, Zagury A, Eliav E. Combined approach to impacted parotid stones. J Oral Maxillofac Surg 2002;60:1418-23. [DOI] [PubMed] [Google Scholar]
- 10.Epivatianos A, Harrison JD. The presence of microcalculi in normal human submandibular and parotid salivary glands. Arch Oral Biol 1989;34:261-5. [DOI] [PubMed] [Google Scholar]
- 11.Andretta M, Tregnaghi A, Prosenikliev V, Staffieri A. Current opinions in sialolithiasis diagnosis and treatment. Acta Otorhinolaryngologica Italica 2005;25:145-9. [PMC free article] [PubMed] [Google Scholar]
- 12.Kassan SS, Thomas TL, Moutsopoulos HM, Hoover R, Kimberly RP, Budman DR. Increase of lymphoma in sicca syndrome. Ann Intern Med 1978;89:888-92. [DOI] [PubMed] [Google Scholar]
- 13.Rauch S, Gorlin RJ. Diseases of the salivary glands. In: Gorlin RJ, Goldman HM, editors. Oral pathology. St Louis: Mosby; 1970. p. 962. [Google Scholar]
- 14.Westhofen M, Schafer H, Seifert G. Calcium redistribution, calcification and stone formation in the parotid gland during experimental stimulation and hypercalcaemia. Cytochemical and X-ray microanalytical investigations. Virchows Arch A Pathol Anat Histopathol 1984;402:425-38. [DOI] [PubMed] [Google Scholar]
- 15.Nahlieli O, Shacham R, Bar T, Eliav E. Endoscopic mechanical retrieval of sialoliths. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:396-402. [DOI] [PubMed] [Google Scholar]
- 16.Drage NA, Brown JE, Escudier MP, McGurk M. Interventional radiology in the removal of salivary calculi. Radiology 2000;214:139-42. [DOI] [PubMed] [Google Scholar]
- 17.Ottaviani F, Cappacio P, Campi M, Ottaviani A. Extracorporeal electromagnetic shock-wave lithotripsy for salivary gland stones. Laryngoscope 1996;106:761-4. [DOI] [PubMed] [Google Scholar]
- 18.Iro H, Schneider Th, Fodra C, Waitz G, Nitsche N, Heinritz HH, et al. Shockwave lithotripsy of salivary duct stones. Lancet 1992;339:1333-6. [DOI] [PubMed] [Google Scholar]