Summary
To assess whether locking-screw titanium plates (UniLOCK) and pedicled pectoralis major myocutaneous flaps are a valid alternative to complex reconstruction with bony free flaps in poor prognosis or poor performance status oncological patients with mandibular defects, a retrospective evaluation has been made of outcomes in 27 consecutive cases. No patient died peri-operatively. Mean operating time was 270 minutes. Post-operative course was uneventful in 14. Mean follow-up was 13 months with no loss to follow-up. Twelve patients are alive and well, 12 died from their malignancy, two from non-neoplastic causes, and one from second cancer. Plate exposure – the main problem with bridging plates – occurred in 6 (22%, 4 early, 2 late), 4 with symphyseal and 2 with postero-lateral defects: removal was necessary in 2; 2 died with the plate exposed, and 2 had successful re-coverage, increasing the final success rate from 78% to 85%. Most patients considered the aesthetic outcome acceptable, however all edentulous patients complained of unsatisfactory dental rehabilitation. From the acceptable success rate, it may be concluded that bridging plates represent a useful reconstruction method, provided they are well covered by viable muscular tissue. They should be offered to patients contraindicated for more invasive procedures or with limited functional needs, or poor prognosis.
Keywords: Head and neck cancer, Surgical treatment, Mandibular reconstruction, Pedicled flap, Bridging plate
Riassunto
Allo scopo di verificare se la placca locking-screw (UniLOCK), unitamente al lembo muscolo-cutaneo di gran pettorale, sia una valida alternativa alla complessa ricostruzione con lembi liberi ossei o composti per i difetti mandibolari in pazienti a cattiva prognosi o in condizioni generali compromesse, sono stati valutati retrospettivamente i risultati di tale tecnica in 27 casi consecutivi. La mortalità peri-operatoria è stata nulla. La durata media dell’intervento è stata di 270 min. Il decorso post-operatorio è stato normale in 14 casi. Il follow-up medio è di 13 mesi e nessun paziente è stato perso ai controlli. Dodici pazienti sono vivi e liberi da malattia, 12 sono morti per il tumore, 2 per cause non neoplastiche ed 1 per un secondo tumore. L’esposizione della placca si è verificata in 6 casi (pari al 22%, in 4 precocemente ed in 2 tardivamente): in 4 casi il difetto era anteriore ed in 2 era latero-posteriore. La rimozione della placca si è resa necessaria in 2 casi; 2 pazienti sono morti con la placca esposta, mentre nei rimanenti 2 è stato possibile coprire la placca con un intervento locale, portando così il tasso di successo finale da 78% a 85%. La maggior parte dei pazienti considera accettabile il risultato cosmetico, mentre i pazienti edentuli lamentano un’insoddisfacente riabilitazione dentale. L’accettabile tasso di successo ci permette di concludere che la placca costituisce un utile metodo di ricostruzione mandibolare, alla condizione che essa sia ricoperta da abbondante tessuto muscolare. Tale metodo ricostruttivo è adatto a pazienti non eligibili per procedure più invasive, o con limitate necessità funzionali, o con prognosi sfavorevole.
Introduction
Reconstructive surgery of the mandible is one of the most complex aspects of the treatment of head and neck malignancies. The mandible protects the upper airways, supports the lower dental arcade and associated soft tissue and tongue, and is crucially involved in the complex movements of swallowing, eating and speaking. The mandible also contributes essentially to the aesthetic integrity of the face. Segmental resection of the mandible and associated soft tissue results in loss of primary mandibular function, exacerbated by loss of teeth and occlusion. Reconstruction of the osseous continuity is not sufficient to restore function; it is also necessary to repair and restore the associated soft tissue. The gold standard in such cases is free flaps. However, the microsurgical procedures involved may be excessively long for patients at high surgical risk, and in some patients, the dental rehabilitation possibilities offered by a bony free flap may not be useful or required. Furthermore, the high cost of such surgery may not be justified in patients with advanced disease and poor prognosis, or poor performance status. In such cases, simpler mandibular reconstruction techniques may be used, provided there is a good possibility of restoring function, including masticatory function, and improving appearance, thereby improving quality of life.
Bridging plates have been used extensively for this purpose 1 2, but have lost favour because of their high complication rates, including fracture and loosening of fixation, and, most importantly, plate exposure. More recent studies 3–6 have suggested solutions to some of these problems. In particular, plate exposure rates can be markedly reduced by covering the plate with a myocutaneous flap.
The purpose of this retrospective study was to evaluate outcomes of mandibular reconstruction with locking screw titanium plates (UniLOCK – Synthes, Solothurn, Switzerland) covered with a pedicled pectoralis major myocutaneous flap.
Patients and methods
Between December 2000 and August 2004, 27 patients, 18 male, 9 female, median age 64 years (range 29-85), with composite or extensive composite oromandibular defects underwent reconstruction with titanium plate and pedicled pectoralis major myocutaneous flap at the Department of Head and Neck Surgery of the Istituto Ortopedico Galeazzi, Milan, Italy. The Department was opened in October 2000.
Overall, 17 (63%) patients underwent immediate reconstruction after resection for tumour recurrence (3 had received radiotherapy alone, 7 surgery alone, and 7 surgery plus post-operative radiotherapy). Ten (37%) patients underwent immediate reconstruction after resection as first treatment for malignancy.
The series constitutes 46.6% of the 58 mandibular reconstructions performed on cancer patients over the same period, the other 31 patients were submitted to fibula free flap repair.
Sites of primary tumours are shown in Table I. Most patients (22/27) had squamous cell carcinoma and were classified according to the TNM system (UICC 6th ed, and AJCC) (Table II). The remaining 5 patients had basal cell carcinoma, salivary adenocarcinoma, ameloblastoma, liposarcoma and osteosarcoma.
Table I. Primary tumour sites in 27 patients undergoing mandibular reconstruction with titanium plate and pedicled pectoralis major myocutaneous flap.
| Site | No. cases |
| Gum | 8 |
| Oropharynx | 5 |
| Floor of mouth | 5 |
| Tongue | 3 |
| Mandible | 2 |
| Cheek | 1 |
| Parotid | 1 |
| Skin | 1 |
| Lip | 1 |
Table II. cTNM stage of 22 patients with squamous cell carcinoma of head and neck.
| T2 | T3 | T4 | Total | |
| N0 | 0 | 1 | 3 | 4 |
| N1 | 2 | 0 | 2 | 4 |
| N2b | 0 | 0 | 8 | 8 |
| Nx | 0 | 0 | 6 | 6 |
| Total | 2 | 1 | 19 | 22 |
Mandibular defects were classified according to the condyle, ramus, body, symphysis (CRBS) scoring system, and are shown in Table III. Most defects involved the angle, but symphyseal involvement was present in 10/27; in 6 cases, condyle resection was necessary.
Table III. Classification of mandibular defects according to CRBS scoring system.
| Defect | No. cases |
| Body, ramus | 14 |
| Symphysis, body, ramus | 2 |
| Body, symphysis, body | 2 |
| Body, ramus, condyle | 2 |
| Symphysis, body, ramus, condyle | 2 |
| Body, symphysis, body, ramus | 1 |
| Condyle ramus, body, symphysis, body | 1 |
| Ramus, body, symphysis, body, ramus | 1 |
| Symphysis, body | 1 |
| Ramus, condyle | 1 |
Soft tissue resection included the mobile tongue in 9 cases, floor of the mouth in 6, tonsillar fossa in 7, soft palate in 7, base of the tongue in 5, pterygo-palatine fossa in 4, and cervical skin in 10. In 4 cases, total laryngectomy was also necessary.
The bone defects were bridged with 2.4 mm thick titanium plates (UniLOCK). Pre-plating was performed whenever feasible, with at least 3 holes made and screws introduced on each side. In one patient, symphyseal wires instead of screws were used because of poor bone quality. When the defect included the condyle, an appropriate condyle-bearing plate was used, secured to the glenoid fossa by two non-resorbable sutures. In all cases, correct plate position was checked by Panorex.
The pectoralis major pedicled flap for soft tissue repair was prepared, whenever possible, while the resection was being performed (two-team approach). The muscle was always raised entirely, with the skin area as large as possible, compatible with primary wound closure, sometimes combined with releasing incisions. As a result, the muscular component exceeded that of the skin and the excess was wrapped around the plate.
The muscle was wrapped around the plate from either a lingual or buccal direction, depending on the type of defect to be repaired, so as to achieve less compression on the pedicle. The aim was always to roll the flap around the plate to cover it completely or at least cover the surfaces most subject to frictional forces (body and symphysis intra-orally, angle extra-orally). In 10 cases, the cutaneous paddle was divided into two parts to allow repair of peri-mandibular or cervical skin.
Overall, 15 patients received post-operative radiotherapy, usually because of advanced disease stage; doses were in the range 16-70 Gy.
The Kaplan-Meier method was used to estimate plate success and survival probabilities, employing the WinStat for Excel package (R. Fitch Software, Staufen, Germany).
Results
Post-operative results
No patient died during the peri-operative period. Average operating time was 270 minutes (range 180-390). Post-operative course was uneventful in 14 patients. Intra-oral dehiscence without plate exposure occurred in four patients, orocutaneous fistula in three, and partial flap necrosis in two, all healed spontaneously. Medical complications were one case of pneumonia and one case of acute myocardial infarction. One patient required emergency surgery for a severe cervical haematoma.
Early plate exposure occurred in 4 patients (14.8%), in 3 cases intra-orally. Unfavourable conditions were suspected to have been responsible in 2 of these: one had synchronous lymphoma and all sutures, including those at the donor site completely dehisced; the other developed severe staphylococcal infection on the seventh post-operative day, leading to progressive and complete lysis of the flap despite prompt and aggressive antibiotic treatment. Plate removal was necessary in 2 of these exposure cases (patient with lymphoma and patient with extra-oral exposure). In the other 2, the plate was left temporarily exposed; one of these – a patient who developed post-operative acute myocardial infarction – underwent a second successful plate coverage after radiotherapy had also exposed the plate extra-orally; the other patient died of distant metastases before a second procedure could be attempted.
On discharge, 25 patients were able to eat a normal or a soft diet. The other 2 patients were discharged with a feeding tube in place due, in both cases, to 10th cranial nerve palsy and labial incompetence. Plate exposure did not compromise ability to eat more or less normally.
Longer term results
Mean follow-up was 13 months (range 1-32). No patients were lost to follow-up. Late plate exposure occurred in two patients. In one, the plate became exposed intra-orally following post-operative radiotherapy; secondary coverage was not possible because metachronous lung cancer was diagnosed and the patient died shortly after. The other patient developed minimal plate exposure at the symphyseal wire osteosynthesis 23 months after treatment: the plate was successfully re-covered after the wires had been replaced and the soft tissue sutured under local anaesthesia.
Overall results
Plate exposure occurred in 6 patients (22%; 4 early, 2 late): the plate had to be removed in 2, 2 died with the plate exposed, and 2 had successful re-coverage, increasing the final success rate from 78% to 85%. Plate exposure occurred in 4/10 (40%) patients with a symphyseal bridge, and in 2/17 (12%) patients with posterolateral defects. Of the 15/27 patients who received post-operative radiotherapy, plate exposure occurred in 4, but in only one was a direct relationship between radiotherapy and exposure likely, as the other 3 patients developed exposure before the commencement of radiotherapy, one of whom required plate removal. In the patient, whose plate became exposed (intraorally) following radiotherapy, second coverage was not attempted because of metachronous lung cancer.
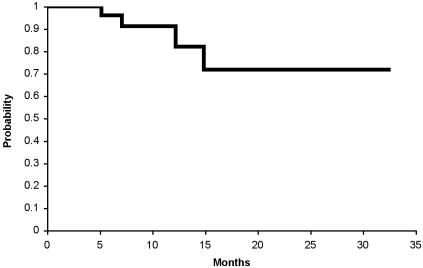
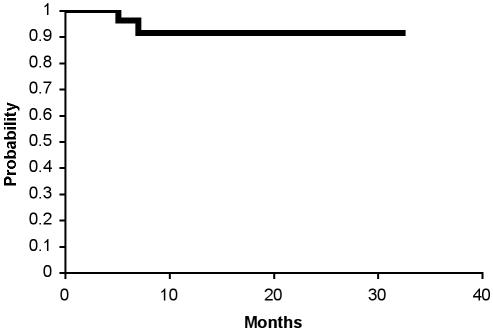
The survival curve for patients with a functioning and covered plate is shown in Figure 1. The survival curve for patients with a functioning plate, irrespective of whether exposed, is shown in Figure 2. No cases of plate fracture or screw loosening occurred.
Fig. 1.
Probability of living with functioning covered plate.
Fig. 2.
Probability of maintaining plate (covered or exposed).
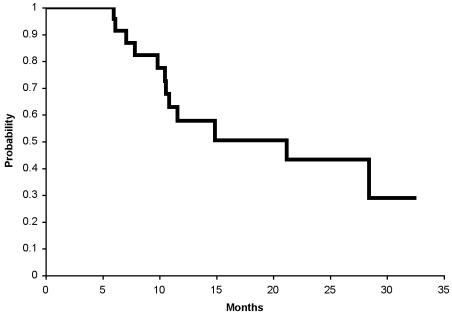
Twelve patients are alive and well, 12 have died from their mandibular malignancy, 2 from non-neoplastic causes, and one from a second cancer. Cause-specific survival is shown in Figure 3.
Fig. 3.
Cause-specific survival.
Discussion
The aims of mandibular reconstruction are to restore function, including dental function, and improve appearance, resulting in improvement of patient quality of life. In the present series, instead of using the gold standard of reconstruction with a bony free flap and soft tissue restoration, we used a titanium plate and pedicled pectoralis major flap. Justifications for this approach were relative or absolute surgical risk, poor prognosis, and patient needs. Our current policy is to try to tailor the surgical approach to the patient, after involving him/her in the decision-making process.
Plate exposure is a major concern in alloplastic mandibular reconstructions. Early plate exposure has been related to wound breakdown following infection or soft tissue necrosis. Late exposure is considered a consequence of long-term friction between the plate and soft tissues. Sixty years ago Byars 7 realised that the key to metal retention and absence of exposure was the presence of a substantial, well-vascularized soft tissue covering to the plate. The pectoralis major myocutaneous flap is considered the workhorse of head and neck reconstruction in view of its versatility, reliability and ease of use 8. Muscle tissue is considered particularly resistant to infection and plate-exerted pressure 5. The pectoralis major myocutaneous flap unites the advantages of simple technique and reliability, with minimal morbidity. Some Authors 9 recommend plate coverage with a free flap. However, this option unites the disadvantages of foreign body introduction with a long and complex operation, and is at odds with the indications for plate usage. In cases where the pectoralis major flap does not have sufficient volume or area to repair a large soft tissue defect alternatives are the larger latissimus dorsi and the bulkier rectus abdominis free flaps 6.
Our exposure rate of 22% is in line with most published experience although figures in the range 0%-46% have been reported 3–6 10–17. Our success rate, in terms of unexposed plates, was 78%; using Boyd et al.’s 18 criterion of no need for plate removal, the success rate was 85%. Most exposures (4/6) in our series occurred early. At least two exposures were not related to the type of reconstruction, since complete wound dehiscence and severe staphylococcal infection would have compromised any repair. We had a similar staphylococcal-related failure recently in a patient who had received a rectus abdominis free flap. Staphylococcal infections rarely complicate head and neck surgery, but are common in the orthopaedic environment and our Department is located in an orthopaedic hospital.
Re-coverage of early intra-oral exposure in one patient was delayed because of acute myocardial infarction; this patient then developed external exposure after radiotherapy. Following a course of hyperbaric oxygen, a minor procedure successfully re-covered the plate both intra-orally and extra-orally.
A patient who developed intra-oral exposure after radiotherapy was initially considered unfit for a free flap procedure due to hyperhomocystinuria. His plate became exposed after partial flap necrosis during radiotherapy. Completing the adjuvant treatment was considered more important than plate coverage, but soon after lung cancer was diagnosed, and re-coverage was not attempted.
A patient with mandibular involvement from parotid cancer, developed extra-oral plate exposure at the level of the condyle and the plate had to be removed; we neglected to consider possible use of the temporalis muscle flap in a salvage procedure.
In the only case with late extra-oral exposure, which occurred after 23 months at the site one of the symphyseal wires, exposure was probably due to wire-induced decubitus.
Plate exposure intra-orally did not appear to cause major discomfort 19. The exposed plate behaved like an endosseous implant, and careful attention to oral hygiene was effective in preventing inflammation and infection.
Fracture at the mandibular reconstruction plate is around 5-16% in published series 6 10 20–23. Fracture did not occur in our series, probably in relation to the biomechanical properties of the UniLOCK system 23 we have been using since the Department was opened in October 2000. There is evidence that if a bridging plate is not replaced by bone, fracture will occur sooner or later. If this is the case, then late failure (≥ 24 months) due to fatigue fracture is a problem of lack of bone regeneration 23. Screw loosening may also lead to failure. Yi et al. 24 found that screw loosening is more likely when small numbers of screws are used to fix plates bridging large defects, and the consequent stress on individual screws is high. The empirical rule that emerges is that the larger the defect the more screws are needed. We found radiographic signs of osteolysis around screws in 4 patients, without consequences on plate stability and performance so far.
Patients were asked their oral opinions regarding outcomes. Most considered the aesthetic outcome acceptable. However, all (3 pre- and 10 post-operatively) edentulous patients complained of unsatisfactory dental rehabilitation; few were able to wear total dentures comfortably, even with application of adhesive paste. In edentulous patients suitable for prosthetic implant in the native mandible, the option was refused. Our opinion is that most of the dental problems arose because of lack of compliance with hyperbaric oxygen therapy prior to insertion of endo-osseous implants, prescribed in all irradiated patients.
A bony flap was offered to 5 low-risk long-term survivors but was refused in all cases. There is no doubt that reconstruction with a plate limits possibilities for dental rehabilitation, since only bone reconstruction provides a suitable base for the implantation of permanent prostheses. However, this limit appears to be of minor importance in patients candidate for plate reconstruction. Most edentulous patients appear to have little interest in long-term and expensive dental procedures, although the placement of a limited number of permanent implants would probably improve denture retention. Catania et al. 1 designed customised plates with incorporated dental fixtures, but did not report long-term results. Gullane et al. 4 suggested manufacturing similar plates and this possibility is currently being evaluated in our Department. Partially dentate patients generally considered that well-fitted removable prostheses were acceptable.
Some Authors 11 25 consider that the plate complication rate is unacceptably high and reject plates as a mandibular reconstruction option. Others consider that plates are only suitable for lateral defects 6 8 13 18 25. In particular, Schusterman et al. 13 found that the success rate was much lower for anterior compared to lateral defects, irrespective of how well covered the plate was; they did not, however. offer any explanation for this finding. Boyd et al. 18 suggested that disconnection of all mouth-opening muscles, denervation of lower lip musculature and lower lip ptosis were mainly responsible for plate failure in the anterior region. In our series, worst results (40% with plate exposure) were obtained when the symphysis was bridged, although this figure is slightly better than that reported in most other studies 8 13 14 18. Note also that in none of these cases did plate removal prove necessary.
Radiotherapy is believed to have a negative effect on the success rate of mandibular reconstruction with plates 15 26, although data from the present study do not support this opinion. However, since irradiation damage becomes more evident with time, longer follow-up might be necessary to reveal a relationship between success and irradiation.
Kiyokawa et al. 5 recently published results of a series of 7 mandibular reconstructions using a metal plate and pectoralis major myocutaneous flap, all of which were successful. The Authors stressed that covering the plate completely by wrapping muscle around it was the key to success. If this is the case, the relatively poor results of Wei et al. 11 might to be due to the lack of a muscular component in the antero-lateral thigh flap used for covering the plate. However, Cordeiro and Hidalgo’s experience 9 suggests different conclusions: all their reconstructions that covered the plate with a forearm free flap were successful, whereas the failure rate was 44% when they used a pectoralis major myocutaneous flap.
Two-year cause-specific survival was 43% in our series but fell to 28% at 32 months. These disappointing outcomes are in line with other published experience on patients with the advanced disease and confirm that prognosis must be taken into account in reconstruction decisions. Head et al. 12 suggested that many poor-prognosis patients do not survive long enough to experience delayed hardware-related complications, and, in such cases, reconstruction with a bridging plate becomes highly attractive, provided quality of life is improved in the short term.
UniLOCK system plates are of pure titanium – a material, the biomechanical properties and biocompatibility of which, are well established. Like other systems, the screws penetrate to the bone cortex and lock to the plate, forming a solid unit. Loading forces are transmitted from bone to plate via the screws, reducing bone damage due to bone-plate friction, and increasing stability. This rigid fixation technique combines the properties of external fixation and internal osteosynthesis, reducing the need for perfect plate modelling and resulting in more favourable outcomes in irradiated bone. Gellrich et al. 23 found that the UniLOCK system provided slightly better results than the THORP system.
To conclude, the results of the present experience indicate that bridging mandibular defects with load-bearing plates is a useful reconstruction method, provided the plate is adequately covered by viable tissue, preferably of a muscular nature. Our 78% success rate, rising to 85% according to the criterion of no need for plate removal, is in line with the 75-80% success rate in the literature, and shows that the method is acceptably reliable. We, therefore, affirm that this option should be offered to patients contraindicated for more invasive procedures, with limited functional needs, or poor prognosis. Symphyseal region repair was associated with the highest failure rate, prompting the consideration that bone transplant might be a better option in such cases. Although every patient should receive the best available treatment, the most expensive treatment is not necessarily the best in all cases.
References
- 1.Catania VC, Cislaghi E, Molinari R. Nuovi orientamenti nella sostituzione protesica della mandibola dopo resezione o disarticolazione. Tumori 1973;59:137-50. [DOI] [PubMed] [Google Scholar]
- 2.Spiessl B. New concepts in maxillofacial bone surgery. Berlin and New York: Springer-Verlag; 1976. p. 156-66. [Google Scholar]
- 3.Raveh J, Stich H, Stutter F. The use of titanium-coated hollow screw and reconstruction plate system in bridging of lower jaw defects. J Oral Max-Fac Surg 1984;42:281-94. [DOI] [PubMed] [Google Scholar]
- 4.Gullane PJ, Havas TE, Holmes HH. Mandibular reconstruction with metal plate and myocutaneous flap. Aust NZ J Surg 1986;56:701-6. [DOI] [PubMed] [Google Scholar]
- 5.Kiyokawa K, Tai Y, Inoue Y, Yanaga H, Rikimaru H, Mori K, et al. Reliable, minimally invasive oromandibular reconstruction using metal plate rolled with pectoralis major myocutaneous flap. J Craniofacial Surg 2001;12:326-36. [DOI] [PubMed] [Google Scholar]
- 6.Poli T, Ferrari S, Bianchi B, Sesenna E. Primary oromandibular reconstruction using free flaps and Thorp plates in cancer patients: a 5-year experience. Head Neck 2003;25:15-23. [DOI] [PubMed] [Google Scholar]
- 7.Byars LT. Subperiosteal mandibular resection with internal bar fixation. Plast Reconstr Surg 1946;1:236. [DOI] [PubMed] [Google Scholar]
- 8.Ijsselstein CB, Hovius SE, ten Have BL, Wijthoff SJ, Sonneveld GJ, Meeuwis CA, et al. Is the pectoralis myocutaneous flap in intraoral and oropharyngeal reconstruction outdated? Am J Surg 1996;172:259-62. [DOI] [PubMed] [Google Scholar]
- 9.Cordeiro PG, Hidalgo DA. Soft tissue coverage of mandibular reconstruction plates. Head Neck 1994;16:112-5. [DOI] [PubMed] [Google Scholar]
- 10.Blackwell KE, Lacombe V. The bridging lateral mandibular reconstruction plate revisited. Arch Otolaryngol Head Neck Surg 1999;125:988-93. [DOI] [PubMed] [Google Scholar]
- 11.Wei FC, Celik N, Yang WG, Chen IH, Chang YM, Chen HC. Complications after reconstruction by plate and soft-tissue free flap in composite mandibular defects and secondary salvage reconstruction with osteocutaneous flap. Plast Reconstr Surg 2003;112:37-42. [DOI] [PubMed] [Google Scholar]
- 12.Head C, Alam D, Sercarz JA, Lee JT, Rawnsley JD, Berke GS, et al. Microvascular flap reconstruction of the mandible: a comparison of bone grafts and bridging plates for restoration of mandibular continuity. Otolaryngol Head Neck Surg 2003;129:48-54. [DOI] [PubMed] [Google Scholar]
- 13.Schusterman MA, Reece GP, Kroll SS, Weldon ME. Use of the AO plate for immediate mandibular reconstruction in cancer patients. Plast Reconstr Surg 1991;88:588-93. [DOI] [PubMed] [Google Scholar]
- 14.Coustal B, Michelet V, Pinsolle J, Siberchicot F, Caix PH, Michelet F. Résultats de l’utilisation des plaques de reconstruction mandibulaire en titane. Rev Stomatol Chir Maxillofac 1994;95:274-7. [PubMed] [Google Scholar]
- 15.Spencer KR, Sizeland A, Taylor GI, Wiesenfeld D. The use of titanium mandibular plates in patients with oral cancer. Int J Oral Maxillofac Surg 1999;28:288-90. [PubMed] [Google Scholar]
- 16.Lopez R, Dekeister C, Sleiman Z, Paoli JR. Mandibular reconstruction using the titanium functionally dynamic bridging plate system: a retrospective study of 34 cases. J Oral Maxillofac Surg 2004;62:421-6. [DOI] [PubMed] [Google Scholar]
- 17.Lindqvist C, Soderholm AL, Laine P, Paatsama J. Rigid reconstruction plate for immediate reconstruction following mandibular resection for malignant tumours. J Oral Maxillofac Surg 1992;50:1158-63. [DOI] [PubMed] [Google Scholar]
- 18.Boyd JB, Mulholland RS, Davidson J, Gullane PJ, Rotstein LE, Brown DH, et al. The free flap and plate in oromandibular reconstruction: long-term review and indications. Plastic Reconstr Surg 1995;95:1018-28. [DOI] [PubMed] [Google Scholar]
- 19.Pinsolle J, Demeaux H, Phan E, Coustal B, Siberchicot F, Michelet FX. Plaques de reconstruction mandibulaire en titane et radiothérapie. Ann Chir Plast Esthet 1993;38:163-6. [PubMed] [Google Scholar]
- 20.Shibahara T, Noma H, Furuya Y, Takaki R. Fracture of mandibular reconstruction plates used after tumour resection. J Oral Maxillofac Surg 2002;60:182-5. [DOI] [PubMed] [Google Scholar]
- 21.Vuillemin T, Raveh J, Sutter F. Mandibular reconstruction with the titanium hollow screw reconstruction plate (THORP) System: evaluation of 62 cases. Plast Reconstr Surg 1988;82:804-14. [DOI] [PubMed] [Google Scholar]
- 22.Klotch D, Gal T, Gal R. Assessment of plate for mandibular reconstruction: has changing technology made a difference? Otolaryngol Head Neck Surg 1999;121:388-92. [DOI] [PubMed] [Google Scholar]
- 23.Gellrich NC, Suarez-Cunqueiro MM, Otero-Cepeda XL, Schön R, Schmelzeisen R, Gutwald R. Comparative study of locking plates in mandibular reconstruction after ablative tumour surgery: THORP vs. UniLOCK system. J Oral Maxillofac Surg 2004;62:186-93. [DOI] [PubMed] [Google Scholar]
- 24.Yi Z, Jian-Gou Z, Guang-Yan Y, Ling L, Fu-Yun Z, Guo-Cheng Z. Reconstruction plates to bridge mandibular defects: a clinical and experimental investigation in biomechanical aspects. Int J Oral Maxillofac Surg 1999;28:445-50. [PubMed] [Google Scholar]
- 25.Cordeiro PG, Hidalgo DA. Conceptual considerations in mandibular reconstruction. Clin Plast Surg 1995;22:61-9. [PubMed] [Google Scholar]
- 26.Ueyama Y, Naitoh R, Yamagata A, Matsumura T. Analysis of reconstruction of mandibular defects using single stainless steel A-O reconstruction plates. J Oral Maxillofac Surg 1996;54:858-62. [DOI] [PubMed] [Google Scholar]