Summary
Intramuscular haemangiomas are uncommon, benign tumours frequently arising in the trunk and extremities. When they appear in the head and neck, the most frequent sites are the trapezius and the masseter muscles, rarely other sites. The case is reported of an intramuscular haemangioma with an unusual location in the orbital part of the orbicularis oculi muscle of a 54-year-old female. Clinical, radiological and histological findings as well as the treatment approach are discussed.
Keywords: Head and neck neoplasm, Muscular tumour, Orbit, Intramuscular haemangioma, Orbicularis oculi muscle
Riassunto
L’emangioma intramuscolare è un raro tumore benigno il quale si sviluppa di solito nel tronco e agli arti. Quando questo compare nella testa e nel collo la sede più frequente è rappresentata dai muscoli trapezio e massetere, mentre è raro in altre regioni. Riportiamo un caso di emangioma intramuscolare nella parte orbitaria del muscolo orbicolare dell’occhio in una paziente di 54 anni. Vengono discussi l’approccio terapeutico, i risultati chirurgici, clinici, radiologici e istologici.
Introduction
Intramuscular haemangiomas (IMH) are uncommon tumours of the head and neck region. Haemangiomas frequently appear in infancy, but mainly in cutaneous and mucosal surfaces, with less than 1% appearing in the muscles of the trunk and extremities. When IMH are located in the head and neck region the most common sites are the masseter and the trapezius muscles, although cases of sternocleidomastoid, temporalis and orbital muscle involvement have been reported.
We report on a case of an IMH with an unusual localization, focusing on the related problems in differential diagnosis, treatment and follow-up.
Case report
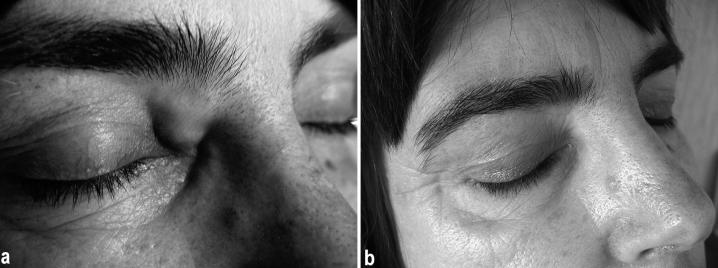
A 54-year-old, otherwise healthy, white, female presented in the ENT Outpatient Department with a painless, non-compressible, colourless, gradually enlarging mass in the right upper eyelid, lateral to the medial canthus (Fig. 1a). The lesion had first appeared 15 years previously, showing a slight but gradual increase in size causing marked discomfort to the patient due to the continuous palpebral movements. She had the first computed tomography (CT) scan in 1997 which revealed a soft tissue tumour in the right orbit but no intervention was decided at that time.
Fig. 1.
A gradually enlarging mass in right upper eyelid, lateral to medial canthus (a). Two years later no recurrence has been noted, with perfect aesthetic result (b).
When the patient presented to us, the lesion had markedly increased, causing functional compromise and cosmetic deformity, since eyelid movement was noticeably restricted. The clinical findings were confirmed by a second CT scan (Fig. 2) which revealed an increase in dimensions.
Fig. 2.
Axial CT scan showing soft tissue tumour in right orbicularis oculi muscle of orbit.
Surgical excision was performed through a Lynch excision. The tumour was removed en bloc. Because of its poorly encapsulated nature and the abundant intra-operative bleeding, dissection was relatively difficult. The mass was excised together with a margin of the normal surrounding muscle to make sure that no part of the tumour had been left in situ.
A lobulated tissue block measuring 16 mm x 40 mm x 70 mm was excised. When sectioned, it was bluish and haemorrhagic.
Histological evaluation revealed a benign vascular tumour consisting of dilated blood vessels, variable in size. The final diagnosis was intramuscular cavernous haemangioma (Fig. 3).
Fig. 3.
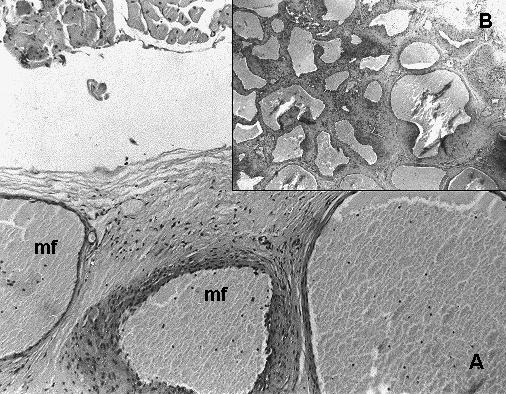
Intramuscular haemangioma showing dilated blood-filled vascular spaces with muscle fibres (mf). (A: HE X 400, B: HE X 100).
The post-operative period was uncomplicated and after a 2-year follow-up, no recurrence has been noted, with perfect aesthetic results (Fig. 1b).
Discussion
Haemangiomas and vascular malformations are benign lesions of blood vessels 1. To date, many different terms and classifications have been suggested for these types of lesions. Recently, the literature has used the classification scheme suggested by Mulliken and Glowacki (1982), who employ the histological and clinical picture of the lesion as primary criteria for classification 2. Haemangiomas and vascular malformations can be localized exclusively in the skin, or they may appear in deeper tissues and involve the skin, thus being visible and easily recognized as soon as they appear. Occasionally, these lesions may be localized in extremely deep tissues and remain undiagnosed for years, especially if they do not produce any clinical symptoms. The most common sites of deep haemangiomas are in the muscle, liver and bone 1. IMH is a rare tumour, accounting for less than 1% of the total number of haemangiomas.
IMH was first reported by Liston in 1843. Additional descriptions in different anatomical areas have been made during the subsequent decade 3. These lesions are non-encapsulated benign neoplasms composed of differently sized vascular channels, sometimes with calcifications, and admixed with variable amounts of adipose, fibrous and myx-oid tissues 3 4.
Allen and Enzinger have described the histological characteristics of IMH 5. In their report, haemangiomas were sub-classified into small-vessel (capillary type), large vessel (cavernous type); and mixed types. However, the histological appearance of the lesion is variable. The vascular spaces differ from normal blood vessels in that there are no demonstrable walls. The spaces communicate freely with each other, giving a honeycomb appearance. There may be evidence of degeneration of muscle fibres. Usually there is minimal evidence of inflammation. Fibrous proliferation may be minimal or marked and is related to the clinical consistency of the tumour. Other variable findings include thrombosis or sclerosis of the vessels, and occasional phleboliths 4 6.
IMH has controversial origins, and congenital, traumatic and hormonal theories have been proposed to explain its aetiology. The congenital nature of these tumours is supported by Authors that observed a high incidence during the first years of life or even at birth 3. Others have suggested that it develops after repeated mechanical injuries of malformed tissue 3 7. Wolf et al. speculated a possible hormonal role in the growth of IMH, although no specific data were available to clearly demonstrate such a hypothesis 8.
About 14% of IMH develop in the head and neck region. The most common site of formation of an IMH in this region is the masseter muscle (36% of cases). Other muscles commonly involved are the trapezius (12%), sternocleidomastoid (10%) and temporalis (8%) 9.
To our knowledge, this is the first report of an IMH in the orbicularis oculi muscle of the orbit. Vascular lesions affecting the extra-ocular muscles are rare, the most common being carotid cavernous fistula. The major cause of extra-ocular muscle enlargement is dysthyroid ophthalmopathy 10–12.
IMH often remains undiagnosed pre-operatively, as in our case, but its nature may be suggested by magnetic resonance imaging (MRI), where the tumour often appear as a sharply demarcated, bright, intramuscular lesion in T2 weighted images, but not in T1 weighted images. This is due to the stagnant blood in the larger vessels 14. Linear areas, iso-intensive to fat and muscle, are often observed in the lesions representing fibro-fatty septae between vessels. Radiological distinction between the different types of IMH is not usually possible. IMH is poorly defined by CT 14 15 and X-ray control often does not help. Ultrasound and angiography are very useful 7.
Taking a biopsy from such tumours, in order to obtain histological proof, is often not very easy. In fact, when biopsy becomes essential, measures must be taken to prevent a haemorrhage.
The therapeutic approach to such lesions is difficult and often with poor results. Open surgical excision, including an adequate rim of surrounding healthy tissue, is the treatment of choice for the management of such lesions, although local recurrences ranging from 9 to 28% have been described 3, even after wide resection of a cuff of normal muscle around the tumour. Sclerotherapy, cryotherapy and radiation treatment may be followed by regression of the mass with relief of pain and compression symptoms. These conservative approaches, alone or in combination with partial surgical resections, are always indicated in the case of lesions massively involving organs (i.e., the tongue), the extensive or complete surgical removal of which could encompass an unjustified post-operative morbidity. Nevertheless, such treatments should be considered merely palliative options 3 16 17.
No cases of spontaneous regression or malignant transformation of these lesions have been reported 3 16–18. In our case, the natural history of the tumour was characteristic, with a slow growth over the past 15 years. A surgical excision was performed, that including an adequate rim of surrounding healthy tissue. Two years after surgery, there have been no signs of recurrence.
In conclusion, head and neck IMH is a rare, unencapsulated vascular neoplasm characterized by painless and slow growth, presenting difficulties in correct pre-operative diagnosis and treatment planning. The recurrence rate is high even after wide surgical excision, due to its microscopically infiltrative pattern of diffusion into the surrounding muscular tissue along planes of least resistance.
Nevertheless, surgical resection, well beyond the gross limits of the tumour, is generally considered the most appropriate therapeutic strategy, other options being mostly palliative. Long-term clinical and radiological follow-up is strongly recommended in order to ensure timely diagnosis and treatment of eventual recurrences.
References
- 1.Shpitzer T, Noyek AM, Witterick I, Kassel T, Ichise M, Gullane P, et al. Noncutaneous cavernous hemangiomas of the head and neck. Am J Otolaryngol 1997;18:367-74. [DOI] [PubMed] [Google Scholar]
- 2.Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg 1982;69:412-22. [DOI] [PubMed] [Google Scholar]
- 3.Giudice M, Piazza C, Bolzoni A, Peretti G. Head and neck intramuscular haemangioma: report of two cases with unusual localization. Eur Arch Otorhinolaryngol 2003;260:498-501. [DOI] [PubMed] [Google Scholar]
- 4.Hessel AC, Vora N, Kountakis SE, Chang CY. Vascular lesion of the masseter presenting with phlebolith. Otolaryngol Head Neck Surg 1999;120:545-8. [PubMed] [Google Scholar]
- 5.Allen PW, Enzinger FM. Haemangioma of skeletal muscle: an analysis of 89 cases. Cancer 1972;29:8-22. [DOI] [PubMed] [Google Scholar]
- 6.Zhan FH, Jian XC, Shen ZH. Giant hemangioma of the sternocleidomastoid muscle: report of a case. J Oral Maxillofac Surg 1997;55:190-3. [DOI] [PubMed] [Google Scholar]
- 7.Clement WA, Graham I, Ablett M, Rawlings D, Dempster JH. Intramuscular hemangioma of the posterior belly of the digastric muscle failing to highlight on magnetic resonance imaging. Ann Otol Rhinol Laryngol 2002;111:1050-3. [DOI] [PubMed] [Google Scholar]
- 8.Wolf GT, Daniel F, Krause CJ, Kaufman RS. Intramuscular haemangioma of head and neck. Laryngoscope 1985;95:210-3. [DOI] [PubMed] [Google Scholar]
- 9.Makeieff M, Maurice N, Mondain M, Crampette L, Guerrier B. Intramuscular hemangioma of posterior neck muscles. Eur Arch Otorhinolaryngol 2001;258:28-30. [DOI] [PubMed] [Google Scholar]
- 10.Christensen SR, Børgesen SE, Heegaard S, Prause JU. Orbital intramuscular haemangioma. Acta Ophthalmol Scand 2002;80:336-9. [DOI] [PubMed] [Google Scholar]
- 11.Shields JA, Bakewell B, Augsburger JJ, Flanagan JC. Classification and incidence of space-occupying lesions of the orbit. A survey of 645 biopsies. Arch Ophthalmol 1984;102:1606-11. [DOI] [PubMed] [Google Scholar]
- 12.Lacey B, Chang W, Rootman J. Nonthyroid causes of extraocular muscle disease. Surv Ophthalmol 1999;44:187-213. [DOI] [PubMed] [Google Scholar]
- 13.Lopez-Cedrun JL, Fernandez JU, Baltanas JM, Lopez Garcia JA. Haemangioma of the temporalis muscle: a case report and review of the literature. J Oral Maxillofac Surg 1996;54:1130-2. [DOI] [PubMed] [Google Scholar]
- 14.Cohen EK, Kressel HY, Perosio T, Burk DL Jr, Dalinka MK, Kanal E, et al. MR imaging of soft-tissue haemangiomas: correlation with pathological findings. Am J Roentgenol 1988;150:1079-81. [DOI] [PubMed] [Google Scholar]
- 15.Buetow PC, Kransdorf MJ, Moser RP, Jelinek JS, Berrey BH. Radiologic appearance of intramuscular haemangioma with emphasis on MR Imaging. Am J Roentgenol 1990;154:563-7. [DOI] [PubMed] [Google Scholar]
- 16.Stofman GM, Reiter D, Feldman MD. Invasive intramuscular haemangioma of the head and neck. Ear Nose Throat J 1989;68:612-5. [PubMed] [Google Scholar]
- 17.Odabasi AO, Metin KK, Mutlu C, Basak S, Erpek G. Intramuscular hemangioma of the masseter muscle. Eur Arch Otorhinolaryngol 1999;256:366-9. [DOI] [PubMed] [Google Scholar]
- 18.Osada K, Yoshihara T, Itoh M. Intramasseter hemangiomas: a case report. J Otolaryngol 2000;29:166-9. [PubMed] [Google Scholar]