Summary
Clinical non-instrumental evaluation plays an important role in the assessment of the dysphagic patient. This evaluation, called “ bedside examination” , aims to establish whether dysphagia is present, evaluating severity, determining the alterations which cause it, planning rehabilitation, testing outcome of treatment. The assessment takes into consideration anamnesis regarding the swallowing problem, evaluation of the anatomy and functionality, of sensitivity and the reflexes, of the swallowing apparatus. Finally, the oral feeding test is performed, which evaluates the oral and pharyngeal phases of swallowing. The examination performed in the neurologic patient is different from that performed in the patient submitted to ENT or maxillo-facial surgery.
Keywords: Deglutition, Dysphagia, Diagnosis, Bedside examination
Riassunto
L’ esame clinico non strumentale ha un importante ruolo nella valutazione del paziente disfagico. Tale valutazione, denominata “ bedside examination” , ha come scopi: stabilire se è presente disfagia, valutarne la severità , definire le alterazioni che la provocano, programmare la riabilitazione, valutare i risultati del trattamento. La valutazione prevede l’ anamnesi riguardante il problema di deglutizione, la valutazione dell’ anatomia e della funzionalità , della sensibilità e dei riflessi, dell’ apparato deglutitorio. Infine si esegue il test di alimentazione orale, che valuta le fasi orale e faringea della deglutizione. L’ esame del paziente neurologico è differente rispetto a quello eseguito nel paziente operato di chirurgia ORL o maxillo-facciale.
Clinical non-instrumental evaluation plays an important role in the assessment of the dysphagic patient 1–5. This evaluation, called “ bedside examination” 6, aims to:
establish whether dysphagia is present;
evaluate the severity;
determine the alterations which cause it;
plan rehabilitation;
test the outcome of treatment.
Dysphagic patients can be divided into two different groups:
neurologic patients 7 8, when dysphagia is caused by stroke, cranial trauma, degenerative neurologic diseases, neurosurgical treatment;
operated patients 9 10, when dysphagia is caused by alterations in the anatomical structures involved in swallowing, after ENT or maxillo-facial surgery.
The first step in the assessment is the anamnesis, which includes:
patient’ s generic data (age);
general conditions (nutritional situation, breathing functionality);
neurologic diagnosis (stable, recurrent or degenerative disease);
description of the surgical procedure on the upper digestive-airways, in the case of dysphagic patient after oncologic intervention of ENT or maxillo-facial surgery;
breathing condition;
vigilance level, neuropsychologic conditions (neurologic patient);
communicative level (neurologic patient);
feeding habit (preferences);
quality of phonation and speech articulation;
presence of hypersalivation;
duration of the meal;
social environment.
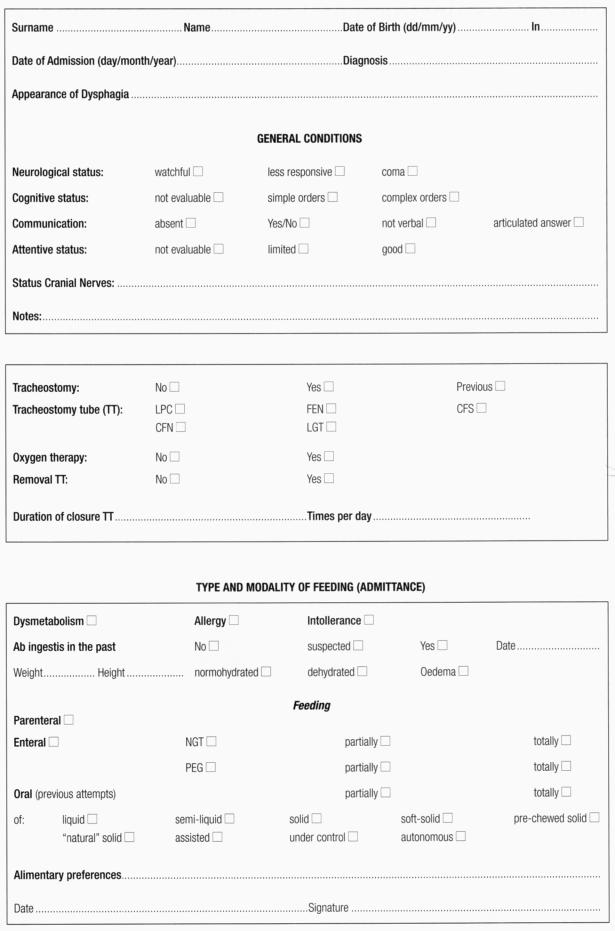
The schedule used for the detection of data regarding the patient’ s general conditions is shown in Table I.
Table I.
Schedule for general conditions of dysphagic patient.
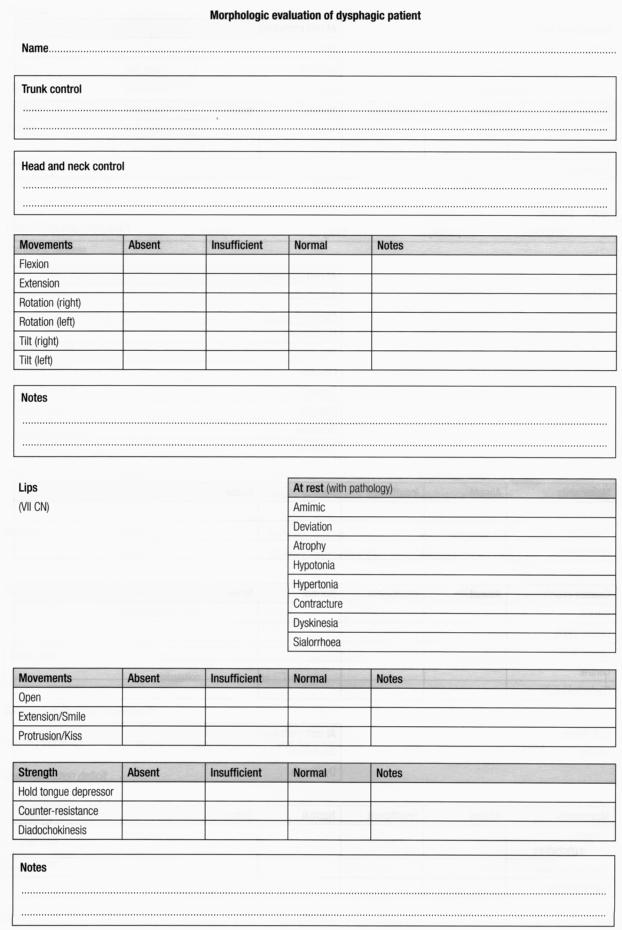
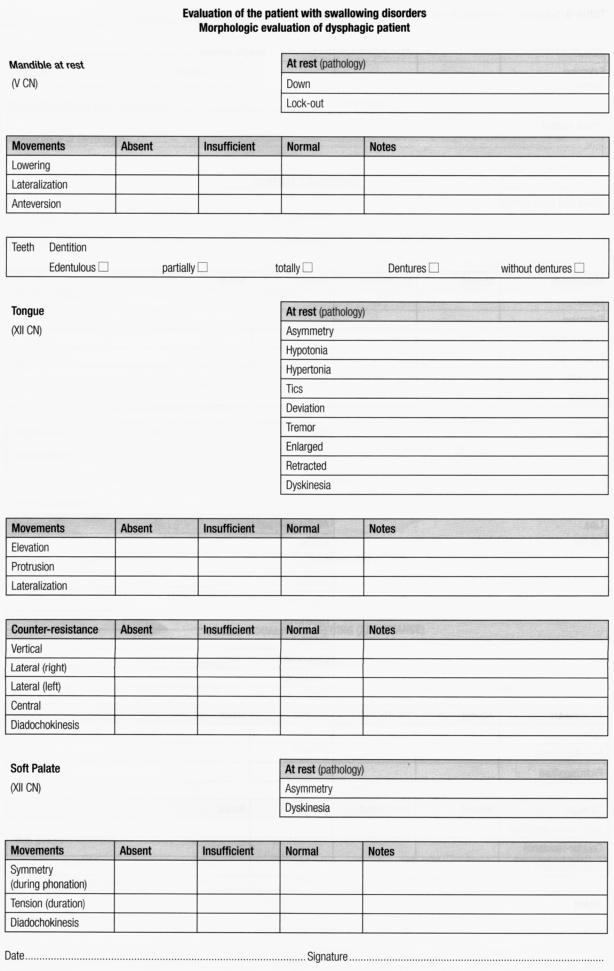
The next step concerns the morphodynamic evaluation (Table II) regarding:
Table II.
Schedule for morphologic evaluation of dysphagic patient (after Schindler 1, modified).
lips (opening, closing, kissing, cheek sufflating);
tongue (motility, protrusion and backwards pushing);
jaw;
soft palate (cheek sufflating, vocalize with an /a/);
larynx (morphology and movements of the vocal folds, glottic closure, elevation of the larynx);
muscular control of the head.
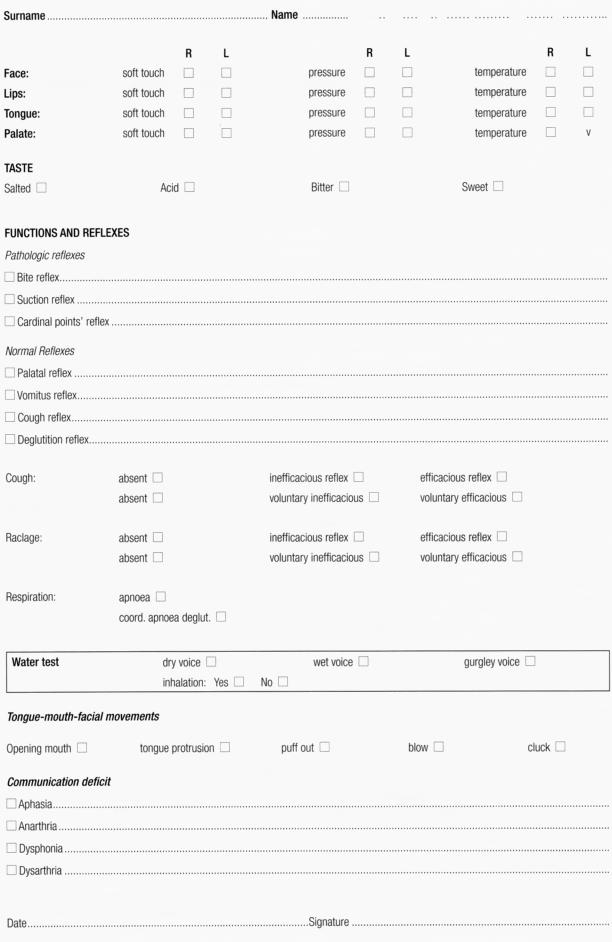
Sensitivity is then evaluated (Table III) of the peribuccal zone (superficial and deep), the lips, the mouth, the tongue and the soft palate (superficial, deep and thermic) and reflexes are evaluated (especially in neurologic patients):
Table III.
Schedule for evaluation of sensitivity and reflexes in dysphagic patient.
normal (gag reflex, cough reflex);
pathologic (bite, cardinal points, suction, swallowing);
water test 11, which is very useful and practical; it evaluates the characteristics of the voice after drinking some water. A dry, humid or gurgling voice may be present and it is possible to evaluate whether a cough caused by inhalation is present.
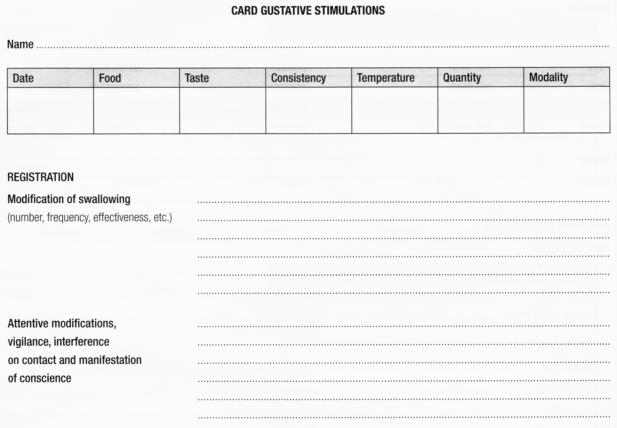
Gustative function with specific stimulations is evaluated (Table IV).
Table IV.
Schedule for evaluation of gustative stimulations in dysphagic patient.
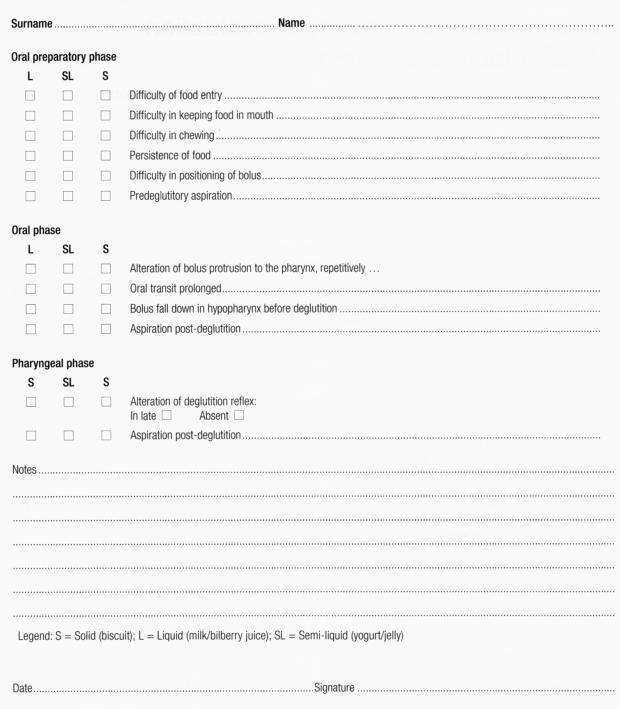
Finally, the oral feeding test is performed (Table V) which evaluates the oral phases of swallowing (suction and chewing) and the pharyngeal phase of swallowing, using liquids (thin pipe, spoon, glass) semi-liquids, semi-solids.
Table V.
Schedule for oral feeding test in dysphagic patient.
The assessment is different in the neurologic patient compared to the operated patient. In the former, we perform a scrupulous examination of motricity and reflexes and an evaluation is made of coordination, communicative possibilities and collaboration ability.
In patients submitted to ENT or maxillo-facial surgery, an evaluation is made of the outcome of the surgical treatment on “ oral-pharyngeal-oesophageal pulsive pump” function which is moved by the tongue, the pharynx and the oesophagus, which squeezes the bolus from the mouth to the stomach, crossing five unidirectional valves: lips, velum-pharyngeal sphincter, larynx; superior oesophageal sphincter, inferior oesophageal sphincter.
References
- 1.Schindler O. Manuale operativo di fisiopatologia della deglutizione. Torino: Ed. Omega; 1990. [Google Scholar]
- 2.Schindler O, Ruoppolo G, Schindler A. Deglutologia. Torino: Ed. Omega; 2001. [Google Scholar]
- 3.Ruoppolo G, Amitrano A, Virdia P, Romualdi P. Semeiotica generale. In: Schindler O, Ruoppolo G, Schindler A, editors. Deglutologia, Torino: Ed. Omega; 2001. p. 97-109. [Google Scholar]
- 4.Schindler O, Raimondo S. Linee guida sulla gestione del paziente disfagico adulto in foniatria e logopedia. Torino: Consensus Conference, 29 gennaio 2007. Acta Phoniatrica Latina 2007;29:5-31. [Google Scholar]
- 5.Logemann JA. Evaluation and treatment of swallowing disorders. San Diego: College-Hill Press; 1983. [Google Scholar]
- 6.Lim SH, Lieu PK, Phua SY, Seshadri R, Uenketasubramanian N, Lee SH, et al. Accuracy of bedside clinical methods compared with fiberoptic endoscopic examination of swallowing (FEES) in determining the risk of aspiration in acute stroke patients. Dysphagia 2001;16:1-6. [DOI] [PubMed] [Google Scholar]
- 7.Logemann JA. Dysphagia: evaluation and treatment. Folia Phoniatr Logop 1995;47:140-64. [DOI] [PubMed] [Google Scholar]
- 8.Rago R, Perino C. La riabilitazione nei trauma cranio encefalico nell’ adulto. Milano: Ed. Ghedini; 1981. [Google Scholar]
- 9.Piemonte M. Fisiopatologia della deglutizione. (Relazione Ufficiale XIV Giornate Italiane di Otoneurologia. Senigallia, 18 aprile 1997). Milano: Formenti Ed.; 1997. [Google Scholar]
- 10.Unnia L. Trattamento logopedico del paziente disfagico adulto. Torino: Ed. Omega; 1995. [Google Scholar]
- 11.De Pippo KL, Holas MA, Reding MJ. Validation of the 3-oz water swallow test for aspiration following stroke. Arch Neurol 1992;49:1259-61. [DOI] [PubMed] [Google Scholar]