Abstract
The authors evaluated the little-examined association between intelligence (IQ) and injury mortality and, for the first known time, explored the extent to which IQ might explain established socioeconomic inequalities in injury mortality. A nationwide cohort of 1,116,442 Swedish men who underwent IQ testing at about 18 years of age was followed for mortality experience for an average of 22.6 years. In age-adjusted analyses in which IQ scores were classified into 4 groups, relative to the highest scoring category, the hazard ratio in the lowest was elevated for all injury types: poisonings (hazard ratio (HR) = 5.82, 95% confidence interval (CI): 4.25, 7.97), fire (HR = 4.39, 95% CI: 2.51, 7.77), falls (HR = 3.17, 95% CI: 2.19, 4.59), drowning (HR = 3.16, 95% CI: 1.85, 5.39), and road injury (HR = 2.17, 95% CI: 1.91, 2.47). Dose-response effects across the full IQ range were evident (P-trend < 0.001). Control for potential covariates, including socioeconomic position, had little impact on these gradients. When socioeconomic disadvantage—indexed by parental and subject's own occupational social class—was the exposure of interest, IQ explained a sizable portion (19%–86%) of the relation with injury mortality. These findings suggest that IQ may have an important role both in the etiology of injuries and in explaining socioeconomic inequalities in injury mortality.
Keywords: cohort studies, intelligence, mortality, socioeconomic factors
Unintentional injury is a major public health problem: in most Western societies, including the United States, it is the leading cause of mortality among people less than 45 years of age (1–3). The burden of injury mortality in low- and middle-income countries is also rising rapidly as they undergo economic transition (4). While the toll incurred by injury mortality due to productive years of life lost is obviously considerable, disability due to injury also carries a major financial cost in terms of medical care and rehabilitation.
Despite its public health importance, much less is known about risk factors for injury than for common chronic diseases such as cardiovascular disease and cancer. In the few studies, socioeconomic disadvantage—indexed by having low income and a manual occupational social class—emerges as a strong predictor of fatal unintentional injury (5–7), although the potential mechanisms underlying this association are still unclear. Cognitive ability (also referred to as intelligence or IQ) is closely correlated with socioeconomic position such that people with a higher IQ tend to be more socioeconomically advantaged (8). Thus, IQ in its own right could be related to injury rates, as it is with total mortality (9, 10), cardiovascular disease (11, 12), and suicide (13, 14). It is also plausible that IQ could at least partially explain socioeconomic inequalities in injuries as it does for selected chronic disease outcomes (15, 16).
Several lines of research implicate IQ in the etiology of injuries, although, taken together, the evidence is not strong. First, persons with an intellectual disability have markedly higher rates of injury than the general population or cognitively normal controls (17, 18); however, whether risk of injury is related to intelligence across the full range of ability is unclear. Second, cross-sectional studies have shown that low mental ability is associated with motor vehicle injury (19, 20) and driving offenses (21, 22). However, given that head trauma, common, for instance, in motor vehicle injury, often leads to reduced cognitive function (23), a spurious negative mental ability–injury gradient may be generated by using this type of study design. Third, in prospective investigations of older people, cognitive ability is inversely related to specific types of injury, particularly falls (24), but reverse causality is again a problem here because comorbidity, prevalent in older people, may influence both cognition and risk of falls. To date, the best evidence for a relation between cognition and injuries comes from follow-up of children or young adult populations, where comorbidity is rare. In the few studies conducted, higher IQ scores confer protection against total (25) and cause-specific (26, 27) injury, including motor vehicle incidents and poisonings, although this observation is not universal (28).
With this paper, we add to this sparse and somewhat inconsistent literature by utilizing data from a cohort study of more than 1 million Swedish men that is well characterized for IQ in late adolescence, socioeconomic position, other covariates, and cause-specific injury mortality. Using this cohort, we previously showed an inverse relation between IQ and deaths from all causes, coronary heart disease, suicides, and all injuries combined (29). For the first known time, we now report on the link between IQ and mortality from a range of injury subtypes by utilizing extended follow-up of this cohort.
This cohort has several advantages compared with other studies. First, given that the sample size is 2 orders of magnitude greater than the next-largest study (26), we were able to estimate the strength of the association of IQ with cause-specific injury mortality with greater precision. In particular, we could examine whether there is evidence of a threshold rather than a dose-response relation, as some studies have suggested (26, 27). This large sample size also enabled us to examine the association between IQ and a wider range of injury subtypes than has previously been possible. Second, this data set contains information on obesity and blood pressure. Although both may be confounding variables in the IQ-injury gradient given their recently reported links with both exposure (30, 31) and outcome (32, 33), their role has yet to be considered. Third, in addition to exploring the relation between IQ and injury mortality rates, the present study permitted us to examine the extent to which IQ might explain well-established socioeconomic inequalities in injury mortality (5–7).
MATERIALS AND METHODS
Study participants and record linkage of registers
The record linkage methods used to generate this cohort study have been reported in detail elsewhere (14, 34–36). In brief, the cohort comprised all nonadopted men born in Sweden from 1950 to 1976 for whom both biologic parents could be identified in the Multi-Generation Register. Using unique personal identification numbers, we linked the Multi-Generation Register with the Military Service Conscription Register (for IQ and covariate data), the Cause of Death Register, Population and Housing Censuses records (1960, 1970, and 1990), and the Register of Education (1990–2001). Doing so resulted in 1,346,545 successful matches and a data set containing a range of physiological, social, psychological, and behavioral characteristics of the men involved (and their parents), together with ascertainment of vital status. Study approval was obtained from the Regional Ethics Committee, Stockholm.
Conscription examination
The Swedish military service conscription examination involves a structured, standard medical assessment of physical health, mental status, and cognitive function (herein called IQ). During the years covered by this study, this examination was required by law; only men of foreign citizenship or those with a severe disability were excused. This data set covers examinations from September 15, 1969, to December 31, 1994, after which the testing procedures used to measure IQ changed. Average age at examination was 18.3 years (range: 16–25).
IQ was measured by 4 written subtests representing logical, spatial, verbal, and technical abilities (37). All test scores, including a global IQ score derived from summing the results of the subtests, were standardized to give a Gaussian-distributed score between 1 and 9. Higher values indicate greater intellectual capacity. The logical test measures capacity to understand written instructions and apply them to solving a problem. Items from the spatial test depicted a plan drawing of an object in its preassembled, 2-dimensional state. Respondents were required to identify, from a series of drawings of fully assembled, 3-dimensional objects, which one it represented. The verbal test measures knowledge of synonyms. Respondents were required to determine which of 4 alternatives is the synonym for a given word. The technical test measures knowledge of chemistry and physics and implies assessment of a component of general knowledge.
Blood pressure, height, and weight were measured by medical personnel during the examination using standard protocols. Height and weight were used to compute body mass index with the usual formula: weight (kg)/height (m)2. We used height as a proxy for early-life circumstances. Although, of course, under a large degree of genetic control, stature is a widely used indicator of preadult suboptimal nutrition, socioeconomic adversity, and perhaps psychosocial stress (38, 39). Psychiatric illness at conscription was based on physician assessment of psychoses (International Classification of Diseases, Eighth Revision (ICD-8) and ICD-9 codes 290–299) and/or neuroses (ICD-8 and ICD-9 codes 300–316).
The highest socioeconomic index of either parent was based on census assessments in the 1960s and 1970s (5 categories: nonmanual (high/intermediate), nonmanual (low), skilled, unskilled, and other). The men's highest achieved educational level (1990–2001) was based on 4 categories (<9 years of primary school, 9–10 years of primary school, full secondary school, and higher education). For men born before 1960, we used the Population and Housing Censuses records (1990) to ascertain their occupational social class, coded as parental social class described above.
For a subgroup of study participants conscripted between 1969 and 1970 only (n = 33,319), information was collected on smoking (>20, 11–20, 6–10, 1–5 cigarettes/day; nonsmoker) and alcohol consumption. Alcohol consumption was assessed by using responses to questions regarding frequency and average consumption of beer, wine, and strong spirits measured in grams per week.
Ascertainment of mortality
Deaths were categorized into all unintentional injuries (ICD-8 and ICD-9 codes E800–E949; ICD-10 codes V01–X59) and the main individual causes in this cohort: road injury (ICD-8 and ICD-9 codes E810–E829; ICD-10 codes V01–V80, V82, V89); poisoning (ICD-8 and ICD-9 codes E850–E869; ICD-10 codes X40–X49); falls (ICD-8 and ICD-9 codes E880–E888; ICD-10 codes W00–W19); fire (ICD-8 and ICD-9 codes E890–E899; ICD-10 codes X00–X09); and drowning (ICD-8 and ICD-9 code E910; ICD-10 codes W65–W74). “Other” injury deaths comprised deaths due to injuries other than the above types.
Statistical methods
Pearson correlation coefficients among the 4 IQ subtests were moderate to high (range: 0.48–0.70; P < 0.001). Preliminary analyses revealed that associations between each of the cognitive subtest scores and total injury mortality were similar, so here we report on the association between global cognitive test scores only (denoted hereafter as IQ) and mortality. Because of the smaller numbers of deaths from some types of injury, the 9-point total IQ scale was collapsed into 4 categories (1/2 = 1, 3/4 = 2, 5/6 = 3, 7–9 = 4). We also examined the relation of IQ with mortality risk by using a standard deviation (1.93 IQ “units”) decrease in the continuous 9-point version of the global IQ scale.
Having checked that the proportional hazards assumption was met, we used Cox proportional hazards models (40) to produce hazard ratios with 95% confidence intervals to summarize the association between IQ and mortality from all unintentional injury types and from individual types. These analyses were based on deaths that occurred from the date of conscription up to December 31, 2004. We controlled for age, early-life socioeconomic position (based on parental occupational social class and the subject's own height), body mass index, education, and systolic blood pressure. We then produced multiply adjusted models—with and without control for education—to evaluate the attenuating role of this close correlate of IQ. As in previous analyses of this cohort (29), we also controlled for both conscription testing center and birth year in the fully adjusted model. These analyses are based on 1,116,442 men for whom data were complete.
Finally, to examine the impact of IQ on the relation between socioeconomic position and mortality, we computed a hazard ratio for the age-adjusted socioeconomic position–mortality relation using parental and subject's own occupational social class as our indicator of socioeconomic position. We then added IQ to the model and compared the percentage attenuation in this hazard ratio with that seen in the age-adjusted analyses by using the same formula we have utilized previously (15): ([hazard ratioadjusted for age – 1] – [hazard ratioadjusted for age and IQ – 1]/[hazard ratioadjusted for age – 1]) × 100.
RESULTS
Table 1 shows the relations between IQ score and the study covariates. Because of the large sample size, all correlations were highly statistically significant but mostly of low magnitude. Men with higher IQ scores had greater educational attainment, were less likely to have parents in unskilled occupations or to be in unskilled occupations themselves in later life, and were taller than those who had lower scores. Men with a higher IQ tended to be slightly older at conscription, and they had a lower body mass index. There was little evidence of a consistent relation between IQ and blood pressure.
Table 1.
Relation of IQ Score With Study Covariates, Sweden, 1969–1994 (N = 1,116,442)
| IQ Score Category |
Correlation With IQ Scorea | ||||
| 1 (n = 103,869) | 2 (n = 274,278) | 3 (n = 446,847) | 4 (Highest) (n = 291,448) | ||
| Parent in an unskilled occupation in 1960–1970, no. (%) | 39,691 (38.2) | 88,503 (32.3) | 110,980 (24.8) | 48,803 (16.6) | −0.268 |
| Educational attainment <11 years, no. (%)b | 37,876 (36.9) | 60,470 (22.2) | 46,325 (10.5) | 10,662 (3.7) | 0.540 |
| Age at testing, mean (SD), years | 18.3 (0.60) | 18.2 (0.55) | 18.3 (0.55) | 18.4 (0.56) | 0.069 |
| Height, mean (SD), cm | 177.3 (6.66) | 178.4 (6.45) | 179.4 (6.38) | 180.4 (6.37) | 0.149 |
| BMI, mean (SD), kg/m2 | 21.9 (3.35) | 21.8 (2.98) | 21.6 (2.73) | 21.4 (2.50) | −0.063 |
| Systolic blood pressure, mean (SD), mm Hg | 128.6 (11.0) | 128.4 (10.9) | 128.5 (11.0) | 128.6 (11.0) | 0.003 |
| Diastolic blood pressure, mean (SD), mm Hg | 68.1 (10.2) | 67.6 (10.0) | 67.3 (9.97) | 67.6 (9.91) | −0.007 |
| In an unskilled occupation in 1990, no. (%)c | 36,616 (35.3) | 75,367 (27.5) | 85,275 (19.1) | 31,678 (10.9) | −0.201 |
Abbreviations: BMI, body mass index; SD, standard deviation.
P values for correlations ≤0.001. Correlations for occupational social class and education were calculated by using the full range of categories.
Based on a subgroup of 1,106,267 men for whom data on education were available.
Based on a subgroup of 1,104,880 men for whom data on own occupational social class were available.
Table 2 presents the relations between IQ and risk of death from all types of unintentional injury, plus the 2 most common causes of such deaths: road injury and poisoning. During a mean follow-up period of 22.6 years, there were 5,415 deaths from all unintentional injuries combined. Average age at censoring was 40.5 years (range: 17.5–54.0). As indicated previously, in an earlier follow-up of the present cohort we reported on the relation of IQ with all deaths due to injury (n = 3,954) alone (29). For the purposes of comparison with individual injury types, we report on this same association here based on a longer follow-up with more such deaths.
Table 2.
Hazard Ratios for the Relation of IQ With Mortality From Unintentional Injury—All Combined, Road Injury, and Poisoning, Sweden, 1969–2004 (N = 1,116,442)
| IQ Score Category |
P-Trend | Per 1-SD Decrease in IQ |
||||||||
| 1 (n = 103,869) |
2 (n = 274,278) |
3 (n = 446,847) |
4 (Highest) (n = 291,448) | |||||||
| HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |||
| All unintentional injury | ||||||||||
| No. of deaths | 839 | 1,625 | 1,962 | 989 | ||||||
| Age adjusted | 2.34 | 2.13, 2.56 | 1.71 | 1.58, 1.86 | 1.32 | 1.22, 1.42 | 1.0 (ref) | <0.001 | 1.32 | 1.27, 1.35 |
| Age and early-life socioeconomic position adjusteda | 2.11 | 1.91, 2.32 | 1.59 | 1.46, 1.72 | 1.26 | 1.17, 1.36 | 1.0 | <0.001 | 1.28 | 1.24, 1.32 |
| Age and BMI adjusted | 2.31 | 2.11, 2.53 | 1.70 | 1.57, 1.84 | 1.31 | 1.22, 1.42 | 1.0 | <0.001 | 1.32 | 1.27, 1.35 |
| Age and systolic blood pressure adjusted | 2.34 | 2.13, 2.57 | 1.71 | 1.58, 1.86 | 1.32 | 1.22, 1.42 | 1.0 | <0.001 | 1.32 | 1.27, 1.35 |
| Age and education adjustedb | 1.52 | 1.34, 1.74 | 1.15 | 1.02, 1.29 | 1.02 | 0.91, 1.13 | 1.0 | <0.001 | 1.15 | 1.11, 1.20 |
| Age and later-life socioeconomic position adjustedc | 2.28 | 2.02, 2.59 | 1.73 | 1.55, 1.93 | 1.36 | 1.22, 1.51 | 1.0 | <0.001 | 1.15 | 1.13, 1.17 |
| Multiply adjustedd (without education) | 2.25 | 1.98, 2.56 | 1.68 | 1.51, 1.88 | 1.28 | 1.15, 1.43 | 1.0 | <0.001 | 1.31 | 1.26, 1.36 |
| Multiply adjusted (with education) | 1.18 | 1.03, 1.35 | 0.98 | 0.87, 1.10 | 0.90 | 0.81, 1.00 | 1.0 | <0.001 | 1.06 | 1.02, 1.11 |
| Road injury | ||||||||||
| No. of deaths | 411 | 879 | 1,062 | 524 | ||||||
| Age adjusted | 2.17 | 1.91, 2.47 | 1.76 | 1.58, 1.96 | 1.33 | 1.20, 1.48 | 1.0 | <0.001 | 1.29 | 1.25, 1.34 |
| Age and early-life socioeconomic position adjusted | 1.91 | 1.68, 2.19 | 1.60 | 1.43, 1.78 | 1.26 | 1.13, 1.40 | 1.0 | <0.001 | 1.24 | 1.20, 1.30 |
| Age and BMI adjusted | 2.14 | 1.88, 2.44 | 1.74 | 1.56, 1.94 | 1.33 | 1.19, 1.47 | 1.0 | <0.001 | 1.30 | 1.24, 1.34 |
| Age and systolic blood pressure adjusted | 2.18 | 1.91, 2.48 | 1.76 | 1.58, 1.96 | 1.33 | 1.20, 1.48 | 1.0 | <0.001 | 1.29 | 1.25, 1.34 |
| Age and education adjusted | 1.35 | 1.10, 1.65 | 1.13 | 0.96, 1.35 | 0.95 | 0.81, 1.12 | 1.0 | <0.001 | 1.11 | 1.04, 1.18 |
| Age and later-life socioeconomic position adjusted | 2.06 | 1.70, 2.49 | 1.74 | 1.48, 2.05 | 1.29 | 1.10, 1.51 | 1.0 | <0.001 | 1.13 | 1.10, 1.17 |
| Multiply adjusted (without education) | 2.06 | 1.69, 2.50 | 1.70 | 1.44, 2.01 | 1.21 | 1.03, 1.42 | 1.0 | <0.001 | 1.28 | 1.20, 1.35 |
| Multiply adjusted (with education) | 1.00 | 0.81, 1.23 | 0.93 | 0.78, 1.11 | 0.81 | 0.69, 0.96 | 1.0 | 0.008 | 1.01 | 0.94, 1.07 |
| Poisoning | ||||||||||
| No. of deaths | 122 | 185 | 167 | 57 | ||||||
| Age adjusted | 5.82 | 4.25, 7.97 | 3.35 | 2.49, 4.50 | 1.99 | 1.47, 2.69 | 1.0 | <0.001 | 1.79 | 1.64, 1.96 |
| Age and early-life socioeconomic position adjusted | 5.12 | 3.70, 7.09 | 3.08 | 2.27, 4.18 | 1.90 | 1.40, 2.58 | 1.0 | <0.001 | 1.73 | 1.58, 1.89 |
| Age and BMI adjusted | 5.78 | 4.22, 7.91 | 3.33 | 2.47, 4.48 | 1.98 | 1.47, 2.68 | 1.0 | <0.001 | 1.79 | 1.64, 1.96 |
| Age and systolic blood pressure adjusted | 5.87 | 4.28, 8.03 | 3.36 | 2.49, 4.52 | 1.99 | 1.48, 2.69 | 1.0 | <0.001 | 1.79 | 1.64, 1.96 |
| Age and education adjusted | 2.84 | 1.96, 4.10 | 1.71 | 1.21, 2.43 | 1.33 | 0.95, 1.88 | 1.0 | <0.001 | 1.35 | 1.22, 1.52 |
| Age and later-life socioeconomic position adjusted | 5.18 | 3.63, 7.38 | 3.25 | 2.32, 4.56 | 2.11 | 1.51, 2.96 | 1.0 | <0.001 | 1.30 | 1.24, 1.37 |
| Multiply adjusted (without education) | 4.87 | 3.37, 7.02 | 3.11 | 2.20, 4.39 | 2.01 | 1.43, 2.82 | 1.0 | <0.001 | 1.66 | 1.51, 1.84 |
| Multiply adjusted (with education) | 2.02 | 1.39, 2.95 | 1.46 | 1.02, 2.07 | 1.19 | 0.84, 1.69 | 1.0 | <0.001 | 1.31 | 1.18, 1.46 |
Abbreviations: BMI, body mass index; CI, confidence interval; HR, hazard ratio; ref, referent; SD, standard deviation.
Socioeconomic position in early life is indexed by parental occupational social class and the subject's height.
Based on a subgroup of 1,106,267 men for whom data on education were available (3,126 deaths from all injuries, 1,348 from road injury, and 961 from poisonings).
Based on a subgroup of 1,104,880 men for whom data on later-life occupational social class were available (3,151 deaths from all injuries, 1,367 from road injury, and 459 from poisonings).
Adjusted for age at testing, conscript testing center, birth year, parental social class, later-life social class, body mass index, height, and systolic blood pressure.
Men with a lower IQ had an increased risk of dying from all unintentional injury: for a standard deviation decrease in IQ, the age-adjusted hazard ratio was 1.32 (95% confidence interval (CI): 1.27, 1.35). There was a gradient in risk across the range of IQ scores (P-trend < 0.001). Compared with those in the highest IQ category, men in the lowest-scoring IQ category had a death rate from unintentional injury more than twice as high: 2.34 (95% CI: 2.13, 2.56). When we adjusted separately for indicators of early-life socioeconomic position (height and parental social class), body mass index, and blood pressure, these effect estimates were unchanged. Adjustment for later-life occupational social class (available for a subgroup of men) had only a modest attenuating impact on the effect estimates. However, adding education (also available for a subgroup of the men) to the multivariable model led to marked attenuation of IQ-injury gradient. Following simultaneous control for all potential covariates, the hazard ratios per standard deviation decrease in IQ without and with adjustment for education were 1.31 (95% CI: 1.26, 1.36) and 1.06 (95% CI: 1.02, 1.11), respectively.
For deaths ascribed to road injury and poisoning, we again found an increase in risk with a decrease in IQ, with a particularly large effect for mortality due to poisoning. Thus, compared with those in the highest IQ category, men in the lowest category had a death rate from poisoning almost 6 times higher: the age-adjusted hazard ratio was 5.82 (95% CI: 4.25, 7.97). For a standard deviation decrease in IQ, the age-adjusted hazard ratios were 1.79 (95% CI: 1.64, 1.96) for death due to poisoning and 1.29 (95% CI: 1.25, 1.34) for death due to road injury. With the exception of education, these risk estimates changed little following individual adjustment for other covariates and in the multivariable model controlling simultaneously for all covariates except education. Further control for education effectively flattened the IQ–road injury relation: the hazard ratio for a standard deviation decrease in IQ was 1.01 (95% CI: 0.94, 1.07). In the analyses featuring poisoning as the outcome of interest, we also found marked attenuation after adding education to the multivariable model, although statistical significance at conventional levels was retained (hazard ratio (HR) = 1.31, 95% CI: 1.18, 1.46).
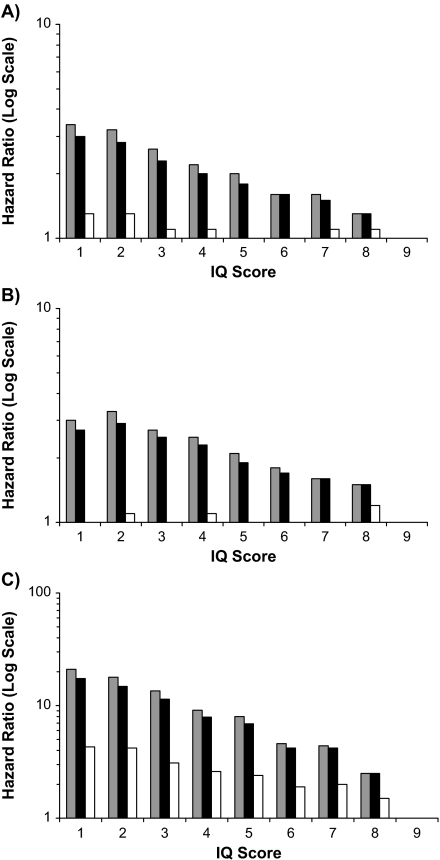
As indicated, because of a low number of deaths for less common injury types, we have presented the injury outcomes in relation to 4 categories of IQ. For the 3 most commonly occurring outcomes—all injuries combined, road injury, and poisonings—there were sufficient cases to conduct analyses across all 9 original IQ categories, depicted in Figure 1. These illustrations essentially confirm the results given in the tables: age-adjusted IQ-injury associations were incremental across the 9-point IQ range, and controlling for covariates had only a moderate impact, except in the case of education.
Figure 1.
IQ and selected injury mortality (N = 1,116,442), Sweden, 1969–2004. Gray bars, age adjustment; black bars, full adjustment (without education); white bars, full adjustment (with education). Referent: highest-scoring IQ group (category 9). A) All injuries (n = 5,415); B) road injury (n = 2,876); C) poisonings (n = 531).
Table 3 depicts the relation of IQ with death due to falls, fire, and drowning. These analyses revealed dose-response relations with IQ similar to those described above. Although, as previously, statistical significance was retained when education was added to the regression model, a nonlinear IQ-drowning association became apparent—the only departure from a dose-response gradient in these analyses. Risk of death from types of injury other than the above categories (n = 1,431) was more weakly related to IQ than in most of the other analyses (age-adjusted HR for a standard deviation decrease in IQ = 1.17, 95% CI: 1.11, 1.23), an association that was lost after multiple adjustment for covariates that included education (HR = 0.96, 95% CI: 0.89, 1.04) (results not shown but available from the corresponding author upon request).
Table 3.
Hazard Ratios for the Relation of IQ With Mortality From Unintentional Injury—Falls, Fire, and Drowning, Sweden, 1969–2004 (N = 1,116,442)
| IQ Score Category |
P-Trend | Per 1-SD Decrease in IQ |
||||||||
| 1 (n = 103,869) |
2 (n = 274,278) |
3 (n = 446,847) |
4 (Highest) (n = 291,448) | |||||||
| HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |||
| Falls | ||||||||||
| No. of deaths | 60 | 104 | 99 | 52 | ||||||
| Age adjusted | 3.17 | 2.19, 4.59 | 2.08 | 1.49, 2.91 | 1.29 | 0.92, 1.80 | 1.0 (ref) | <0.001 | 1.47 | 1.32, 1.64 |
| Age and early-life socioeconomic position adjusteda | 3.00 | 2.04, 4.42 | 2.00 | 1.42, 2.82 | 1.25 | 0.89, 1.76 | 1.0 | <0.001 | 1.46 | 1.30, 1.63 |
| Age and BMI adjusted | 3.11 | 2.14, 4.51 | 2.06 | 1.47, 2.87 | 1.28 | 0.91, 1.79 | 1.0 | <0.001 | 1.47 | 1.32, 1.64 |
| Age and systolic blood pressure adjusted | 3.18 | 2.19, 4.60 | 2.09 | 1.50, 2.91 | 1.29 | 0.92, 1.80 | 1.0 | <0.001 | 1.47 | 1.32, 1.64 |
| Age and education adjustedb | 2.32 | 1.40, 3.86 | 1.44 | 0.90, 2.30 | 1.01 | 0.64, 1.59 | 1.0 | <0.001 | 1.38 | 1.18, 1.61 |
| Age and later-life socioeconomic position adjustedc | 3.65 | 2.26, 5.89 | 2.27 | 1.46, 3.55 | 1.37 | 0.88, 2.15 | 1.0 | <0.001 | 1.26 | 1.17, 1.35 |
| Multiply adjustedd (without education) | 3.40 | 2.08, 5.56 | 2.14 | 1.36, 3.37 | 1.30 | 0.83, 2.04 | 1.0 | <0.001 | 1.53 | 1.32, 1.77 |
| Multiply adjusted (with education) | 1.85 | 1.10, 3.12 | 1.30 | 0.81, 2.09 | 0.93 | 0.59, 1.48 | 1.0 | 0.008 | 1.29 | 1.10, 1.52 |
| Fire | ||||||||||
| No. of deaths | 33 | 62 | 57 | 20 | ||||||
| Age adjusted | 4.39 | 2.51, 7.77 | 3.22 | 1.95, 5.33 | 1.90 | 1.14, 3.17 | 1.0 | <0.001 | 1.69 | 1.46, 1.97 |
| Age and early-life socioeconomic position adjusted | 3.96 | 2.22, 7.04 | 2.96 | 1.77, 4.96 | 1.80 | 1.08, 3.17 | 1.0 | <0.001 | 1.65 | 1.41, 1.94 |
| Age and BMI adjusted | 4.39 | 2.51, 7.68 | 3.22 | 1.95, 5.33 | 1.90 | 1.14, 3.17 | 1.0 | <0.001 | 1.69 | 1.46, 1.97 |
| Age and systolic blood pressure adjusted | 4.41 | 2.52, 7.70 | 3.22 | 1.95, 5.33 | 1.90 | 1.14, 3.17 | 1.0 | <0.001 | 1.70 | 1.46, 1.97 |
| Age and education adjusted | 2.64 | 1.21, 5.74 | 1.86 | 0.91, 3.80 | 1.38 | 0.69, 2.79 | 1.0 | 0.049 | 1.50 | 1.20, 1.87 |
| Age and later-life socioeconomic position adjusted | 4.68 | 2.25, 9.73 | 3.22 | 1.63, 6.38 | 2.01 | 1.02, 3.99 | 1.0 | <0.001 | 1.33 | 1.20, 1.47 |
| Multiply adjusted (without education) | 4.66 | 2.11, 9.43 | 3.03 | 1.52, 6.06 | 1.88 | 0.95, 3.74 | 1.0 | <0.001 | 1.74 | 1.42, 2.14 |
| Multiply adjusted (with education) | 2.07 | 0.94, 4.56 | 1.62 | 0.78, 3.33 | 1.25 | 0.62, 2.54 | 1.0 | 0.217 | 1.41 | 1.13, 1.77 |
| Drowning | ||||||||||
| No. of deaths | 29 | 27 | 52 | 25 | ||||||
| Age adjusted | 3.16 | 1.85, 5.39 | 1.12 | 0.65, 1.93 | 1.44 | 0.89, 2.31 | 1.0 | <0.001 | 1.36 | 1.15, 1.61 |
| Age and early-life socioeconomic position adjusted | 2.73 | 1.56, 4.76 | 1.01 | 0.58, 1.76 | 1.34 | 0.83, 2.18 | 1.0 | <0.001 | 1.31 | 1.10, 1.56 |
| Age and BMI adjusted | 3.18 | 1.86, 5.44 | 1.13 | 0.65, 1.94 | 1.44 | 0.90, 2.32 | 1.0 | <0.001 | 1.37 | 1.16, 1.62 |
| Age and systolic blood pressure adjusted | 3.17 | 1.86, 5.42 | 1.12 | 0.65, 1.93 | 1.44 | 0.89. 2.32 | 1.0 | <0.001 | 1.36 | 1.15, 1.61 |
| Age and education adjusted | 1.96 | 1.08, 3.55 | 0.70 | 0.39, 1.26 | 1.06 | 0.64, 1.74 | 1.0 | 0.002 | 1.18 | 0.97, 1.44 |
| Age and later-life socioeconomic position adjusted | 2.24 | 1.29, 3.89 | 0.89 | 0.51, 1.56 | 1.27 | 0.78, 2.05 | 1.0 | 0.003 | 1.11 | 1.02, 1.22 |
| Multiply adjusted (without education) | 2.21 | 1.85, 3.91 | 0.88 | 0.50, 1.55 | 1.20 | 0.74, 1.95 | 1.0 | <0.001 | 1.23 | 1.03, 1.47 |
| Multiply adjusted (with education) | 1.55 | 0.33, 1.08 | 0.59 | 0.33, 1.08 | 0.92 | 0.56, 1.52 | 1.0 | 0.006 | 1.06 | 0.87, 1.30 |
Abbreviations: BMI, body mass index; CI, confidence interval; HR, hazard ratio; ref, referent; SD, standard deviation.
Socioeconomic position in early life is indexed by parental occupational social class and the subject's height.
Based on a subgroup of 1,106,267 men for whom data on education were available (209 deaths from falls, 106 from fires, and 132 from drownings).
Based on a subgroup of 1,104,880 men for whom data on later-life occupational social class were available (208 deaths from falls, 109 from fires, and 132 from drownings).
Adjusted for age at testing, conscript testing center, birth year, parental social class, later-life social class, body mass index, height, and systolic blood pressure.
When we used the alcohol consumption data available for a subgroup of the study participants (n = 33,319) in which there were 190 deaths due to injury, we found an age-adjusted inverse association between IQ and all injuries combined (HRper 1 standard deviation decrease in IQ = 1.44, 95% CI: 1.26, 1.65). This result was essentially unchanged when alcohol consumption was added to the model (HR = 1.41, 95% CI: 1.23, 1.62). Similar observations were made when road injury was the mortality endpoint (80 deaths). There were too few deaths from other injury types for separate analysis. We also adjusted for smoking as a marker of risk-taking behavior, and the hazard ratios again changed little.
In the original sample (N = 1,116,442), 66,224 men were diagnosed with a psychiatric illness at conscription. Although IQ was inversely associated with psychiatric illness (odds ratioper 1 standard deviation decrease in IQ = 1.84, 95% CI: 1.82, 1.85), adding this variable to the age-adjusted model had very little impact on the magnitude of the relation between IQ and any of the injury outcomes under investigation. The largest attenuation was seen for risk of death from poisonings, for which, after further adjustment for psychiatric illness, the age-adjusted hazard ratio for mortality per standard deviation decrease in IQ fell only from 1.79 (95% CI: 1.64, 1.96) to 1.64 (95% CI: 1.52, 1.80). In the case of other types of accidents and all accidents combined, adjustment for psychiatric illness attenuated the hazard ratio by, at most, 3%.
Finally, we examined the extent to which IQ “explained” socioeconomic inequalities in injuries, that is, the degree to which it accounted for the relative change in risk of parental and own occupational social class with injury mortality. For brevity in this paper, we show the age-adjusted relation for 3 selected injury mortality outcomes with socioeconomic position, before and after control for IQ (Table 4). As expected, socioeconomic disadvantage was related to an elevated rate of deaths due to road injury, poisonings, and all injuries combined. Controlling for IQ led to marked attenuation of these gradients such that the percentage reduction in the hazard ratio ranged between 19% and 86%.
Table 4.
Hazard Ratios for the Relation of Indicators of Socioeconomic Position With Mortality From Unintentional Injury—All Combined, Road Injury, and Poisoning, Sweden, 1969–2004
| Type of Injury Mortality and Indicator of Socioeconomic Position | No. of Deaths | No. of Subjects | Adjusted for Age |
Adjusted for Age and IQ |
% Changea | ||
| HR | 95% CI | HR | 95% CI | ||||
| All | |||||||
| Parental social class | |||||||
| Manual | 3,771 | 740,452 | 1.32 | 1.25, 1.40 | 1.16 | 1.09, 1.23 | −50 |
| Nonmanual | 1,522 | 375,990 | 1.0 (ref) | 1.0 | |||
| Own social class | |||||||
| Manual | 2,580 | 818,668 | 2.91 | 2.63, 3.20 | 2.50 | 2.26, 2.77 | −21 |
| Nonmanual | 467 | 286,311 | 1.0 | 1.0 | |||
| Road injury | |||||||
| Parental social class | |||||||
| Manual | 785 | 375,990 | 1.39 | 1.28, 1.51 | 1.24 | 1.14, 1.34 | −38 |
| Nonmanual | 2,091 | 740,452 | 1.0 | 1.0 | |||
| Own social class | |||||||
| Manual | 1,173 | 818,668 | 2.84 | 2.44, 3.31 | 2.49 | 2.13, 2.92 | −19 |
| Nonmanual | 194 | 286,311 | 1.0 | 1.0 | |||
| Poisoning | |||||||
| Parental social class | |||||||
| Manual | 383 | 375,990 | 1.44 | 1.18, 1.74 | 1.06 | 0.87, 1.29 | −86 |
| Nonmanual | 148 | 740,452 | 1.0 | 1.0 | |||
| Own social class | |||||||
| Manual | 413 | 818,668 | 5.29 | 3.90, 7.18 | 3.78 | 2.76, 5.17 | −35 |
| Nonmanual | 46 | 286,311 | 1.0 | 1.0 | |||
Abbreviations: CI, confidence interval; HR, hazard ratio; ref, referent.
Percentage change in hazard ratio in age-adjusted analyses compared with hazard ratio in age- and IQ-adjusted analyses.
DISCUSSION
In this study of more than 1 million men, we found an apparent protective effect of higher IQ against risk of death from unintentional injury overall, and, in descending order of magnitude, from each of the 5 most common causes of injury deaths in this cohort (poisoning, fire, falls, drowning, and road injury). Of these different endpoints, road injury is most likely to have been caused by a second party, which may have weakened its association with IQ.
While the magnitude of the IQ-injury associations varied, in all cases the associations were strong, generally incremental across the range of IQ scores, and independent of early- and later-life socioeconomic disadvantage. That these gradients were of a dose-response nature—an elevated risk of injury mortality was not, for instance, apparent for only those men with below-average IQ performance; rather, it was found across the full IQ range—strongly implies that our results were not due to existing mental disability.
In all of these analyses, adding education to the multivariable model led to pronounced attenuation of the IQ-injuries relation, although rarely was the association lost. In this data set, as in others (41), education and IQ were positively correlated (r = 0.54; P < 0.001). Indeed, this finding is universal (8). The causal direction of the association is a moot point. Therefore, inclusion of education in our models is questionable; it is likely that higher educational credentials are, to a substantial extent, the outcome of higher IQ (41).
We found that the extent to which the socioeconomic position–injury mortality association was explained by IQ differed according to the indicator of adversity and outcome under consideration, although it was substantial. A similar observation was made previously when chronic diseases—coronary heart disease, long-term limiting illness, minor psychiatric morbidity—were the outcomes of interest (15, 16).
Plausible mechanisms
Several mechanisms may underlie these associations. First, higher IQ may be associated with more favorable levels of health behaviors, such as binge drinking (42), smoking (43–45), physical activity, and diet (46). The former particularly may have a role in the etiology of injury, although controlling for alcohol consumption in a subgroup of the present cohort had no impact. Socioeconomic position, a correlate of IQ, is positively related to ownership (47) and use of (48, 49) protective devices such as motorcycle and push-bike helmets and car seatbelts. We are, however, unaware of any studies directly examining the relation of their use with cognitive ability. Second, poor perceptual abilities, such as below-average information processing speed, has been advanced as a risk factor for road injury (23). Persons with higher scores on standard mental ability tests have faster processing speed (50). A third possibility is that lower-IQ-scoring persons may be more likely to work and live in less safe environments (51), where exposure to risk of road injury, falls, and fire might be more frequent. In controlling for occupational social class, we may have failed to fully capture these contextual effects. Fourth, lower IQ has been linked to poorer “health literacy” (52). Such an impairment may lead to a misunderstanding of warning labels on drugs and household products, thus increasing the risk of poisoning. Finally, perception of the risk of a given activity—fast driving, swimming in unknown waters or in unsafe conditions—may be more acute in the more intelligent.
Study strengths and limitations
The strengths of this study lie in its size and the availability of a range of data on covariates. However, this study also has some limitations. First, selection bias would occur in the present study if the IQ-mortality gradients differed markedly between persons included in the analyses and those excluded. In the present study, approximately one-quarter of the original study sample was dropped from the analytical sample because of missing data. Their characteristics, where available, were compared with those who were retained. Differences between the groups in terms of IQ and covariates were not marked (results not shown but available from the corresponding author upon request). Furthermore, of the 294,128 men excluded from our principal analyses, 36,654 had data on IQ, among whom 177 deaths from all injuries combined occurred. In age-adjusted analyses, the IQ–total injury mortality relation for the excluded men (hazard ratioper 1 standard deviation advantage in IQ = 1.51, 95% CI: 1.31, 1.74) did not differ greatly from that seen in the analytical sample (HR = 1.32, 95% CI: 1.27, 1.35), suggesting that selection bias is not a major concern. Second, the present analyses were confined to men; we are unsure whether these results can also be extrapolated to women.
In conclusion, in the largest and best characterized study to date known to examine the association, IQ was inversely related to mortality due to road injury, poisonings, falls, fire, and drowning. Tests of the existence of such associations in underresearched groups, such as women and ethnic minorities, are required. There was also a suggestion that IQ partially explained socioeconomic inequalities in injury mortality. Given that general learning and reasoning ability are captured by IQ tests, it may be that individual cognition levels should be considered more carefully when preparing injury prevention campaigns.
Acknowledgments
Author affiliations: MRC Social and Public Health Sciences Unit, University of Glasgow, Glasgow, United Kingdom (G. David Batty); Centre for Cognitive Ageing and Cognitive Epidemiology, Department of Psychology, University of Edinburgh, Edinburgh, United Kingdom (G. David Batty, Ian J. Deary); MRC Epidemiology Resource Centre, University of Southampton, Southampton, United Kingdom (Catharine R. Gale); and Department of Public Health Sciences, Karolinska Institute, Stockholm, Sweden (Per Tynelius, Finn Rasmussen).
The Medical Research Council (MRC) Social and Public Health Sciences Unit receives funding from the UK MRC and the Chief Scientist Office at the Scottish Government Health Directorates. The Centre for Cognitive Ageing and Cognitive Epidemiology is supported by the Biotechnology and Biological Sciences Research Council, the Engineering and Physical Sciences Research Council, the Economic and Social Research Council, the MRC, and the University of Edinburgh as part of the cross-council Lifelong Health and Wellbeing initiative. G. David Batty is a UK Wellcome Trust Fellow (WBS U.1300.00.006.00012.01).
Conflict of interest: none declared.
Glossary
Abbreviations
- CI
confidence interval
- HR
hazard ratio
- ICD-8
International Classification of Diseases, Eighth Revision (ICD-9 and ICD-10 defined similarly)
References
- 1.Segui-Gomez M, MacKenzie EJ. Measuring the public health impact of injuries. Epidemiol Rev. 2003;25:3–19. doi: 10.1093/epirev/mxg007. [DOI] [PubMed] [Google Scholar]
- 2.Australian Institute for Health and Welfare. Australia's Health 2000. 8th Biennial Health Report. Canberra: Australia: Australian Institute for Health and Welfare; 2002. (AIHW Cat No AUS 25) [Google Scholar]
- 3.Peden M, McGee K, Sharma G. The Injury Chartbook: A Graphical Overview of the Global Burden of Injuries. Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 4.Ameratunga S, Hijar M, Norton R. Road-traffic injuries: confronting disparities to address a global-health problem. Lancet. 2006;367(9521):1533–1540. doi: 10.1016/S0140-6736(06)68654-6. [DOI] [PubMed] [Google Scholar]
- 5.Cubbin C, LeClere FB, Smith GS. Socioeconomic status and injury mortality: individual and neighbourhood determinants. J Epidemiol Community Health. 2000;54(7):517–524. doi: 10.1136/jech.54.7.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cubbin C, LeClere FB, Smith GS. Socioeconomic status and the occurrence of fatal and nonfatal injury in the United States. Am J Public Health. 2000;90(1):70–77. doi: 10.2105/ajph.90.1.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lawlor DA, Sterne JA, Tynelius P, et al. Association of childhood socioeconomic position with cause-specific mortality in a prospective record linkage study of 1,839,384 individuals. Am J Epidemiol. 2006;164(9):907–915. doi: 10.1093/aje/kwj319. [DOI] [PubMed] [Google Scholar]
- 8.Neisser U, Boodoo G, Bouchard T, Jr, et al. Intelligence: knowns and unknowns. Am Psychol. 1996;51:77–101. [Google Scholar]
- 9.Batty GD, Gale CR, Mortensen LH, et al. Pre-morbid intelligence, the metabolic syndrome and mortality: the Vietnam Experience Study. Diabetologia. 2008;51(3):436–443. doi: 10.1007/s00125-007-0908-5. [DOI] [PubMed] [Google Scholar]
- 10.Batty GD, Shipley MJ, Mortensen L, et al. IQ in late adolescence/early adulthood, risk factors in middle-age, and later all-cause mortality in men: the Vietnam Experience Study. J Epidemiol Community Health. 2008;62(6):522–531. doi: 10.1136/jech.2007.064881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Batty GD, Mortensen L, Gale CR, et al. Is low IQ related to risk of death by homicide? Testing an hypothesis using data from the Vietnam Experience Study. Psychiatry Res. 2008;161(1):112–115. doi: 10.1016/j.psychres.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Batty GD, Mortensen EL, Nybo Andersen AM, et al. Childhood intelligence in relation to adult coronary heart disease and stroke risk: evidence from a Danish birth cohort study. Paediatr Perinat Epidemiol. 2005;19(6):452–459. doi: 10.1111/j.1365-3016.2005.00671.x. [DOI] [PubMed] [Google Scholar]
- 13.Andersson L, Allebeck P, Gustafsson JE, et al. Association of IQ scores and school achievement with suicide in a 40-year follow-up of a Swedish cohort. Acta Psychiatr Scand. 2008;118(2):99–105. doi: 10.1111/j.1600-0447.2008.01171.x. [DOI] [PubMed] [Google Scholar]
- 14.Gunnell D, Magnusson PK, Rasmussen F. Low intelligence test scores in 18 year old men and risk of suicide: cohort study. BMJ. 2005;330(7484):167. doi: 10.1136/bmj.38310.473565.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Batty GD, Der G, MacIntyre S, et al. Does IQ explain socioeconomic inequalities in health? Evidence from a population based cohort study in the west of Scotland. BMJ. 2006;332(7541):580–584. doi: 10.1136/bmj.38723.660637.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh-Manoux A, Ferrie JE, Lynch JW, et al. The role of cognitive ability (intelligence) in explaining the association between socioeconomic position and health: evidence from the Whitehall II prospective cohort study. Am J Epidemiol. 2005;161(9):831–839. doi: 10.1093/aje/kwi109. [DOI] [PubMed] [Google Scholar]
- 17.Sherrard J, Tonge BJ, Ozanne-Smith J. Injury in young people with intellectual disability: descriptive epidemiology. Inj Prev. 2001;7(1):56–61. doi: 10.1136/ip.7.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dunne RG, Asher KN, Rivara FP. Injuries in young people with developmental disabilities: comparative investigation from the 1988 National Health Interview Survey. Ment Retard. 1993;31(2):83–88. [PubMed] [Google Scholar]
- 19.O'Toole BI. Intelligence and behaviour and motor vehicle accident mortality. Accid Anal Prev. 1990;22(3):211–221. doi: 10.1016/0001-4575(90)90013-b. [DOI] [PubMed] [Google Scholar]
- 20.Smith DI, Kirkham RW. Relationship between intelligence and driving record. Accid Anal Prev. 1982;14:439–442. [Google Scholar]
- 21.Conger JJ, Miller WC, Rainey RV. Effects of driver education: the role of motivation, intelligence, social class and exposure. Traffic Saf Res Rev. 1966;10:2–13. [Google Scholar]
- 22.Harrington D. The Young Driver Follow-up Study: An Evaluation of the Role of Human Factors in the First Four Years of Driving. Sacramento, CA: Department of Motor Vehicles; 1971. (Report 38) [Google Scholar]
- 23.Hills BL. Vision, visibility, and perception in driving. Perception. 1980;9(2):183–216. doi: 10.1068/p090183. [DOI] [PubMed] [Google Scholar]
- 24.Anstey KJ, von Sanden C, Luszcz MA. An 8-year prospective study of the relationship between cognitive performance and falling in very old adults. J Am Geriatr Soc. 2006;54(8):1169–1176. doi: 10.1111/j.1532-5415.2006.00813.x. [DOI] [PubMed] [Google Scholar]
- 25.Hemmingsson T, Melin B, Allebeck P, et al. The association between cognitive ability measured at ages 18–20 and mortality during 30 years of follow-up—a prospective observational study among Swedish males born 1949–51. Int J Epidemiol. 2006;35(3):665–670. doi: 10.1093/ije/dyi321. [DOI] [PubMed] [Google Scholar]
- 26.Osler M, Andersen AM, Laursen B, et al. Cognitive function in childhood and early adulthood and injuries later in life: the Metropolit 1953 male birth cohort. Int J Epidemiol. 2007;36(1):212–219. doi: 10.1093/ije/dyl261. [DOI] [PubMed] [Google Scholar]
- 27.Lawlor DA, Clark H, Leon DA. Associations between childhood intelligence and hospital admissions for unintentional injuries in adulthood: the Aberdeen Children of the 1950s cohort study. Am J Public Health. 2007;97(2):291–297. doi: 10.2105/AJPH.2005.080168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Batty GD, Deary IJ, Schoon I, et al. Childhood mental ability in relation to cause-specific accidents in adulthood: the 1970 British Cohort Study. QJM. 2007;100(7):405–414. doi: 10.1093/qjmed/hcm039. [DOI] [PubMed] [Google Scholar]
- 29.Batty GD, Modig-Wennerstad K, Davey Smith G, et al. IQ in early adulthood and mortality by middle age: cohort study of 1 million Swedish men. Epidemiology. 2009;20(1):100–109. doi: 10.1097/EDE.0b013e31818ba076. [DOI] [PubMed] [Google Scholar]
- 30.Starr JM, Taylor MD, Hart CL, et al. Childhood mental ability and blood pressure at midlife: linking the Scottish Mental Survey 1932 and the Midspan studies. J Hypertens. 2004;22(5):893–897. doi: 10.1097/00004872-200405000-00009. [DOI] [PubMed] [Google Scholar]
- 31.Chandola T, Deary IJ, Blane D, et al. Childhood IQ in relation to obesity and weight gain in adult life: the National Child Development (1958) Study. Int J Obes (Lond) 2006;30(9):1422–1432. doi: 10.1038/sj.ijo.0803279. [DOI] [PubMed] [Google Scholar]
- 32.Terry PD, Abramson JL, Neaton JD. Blood pressure and risk of death from external causes among men screened for the Multiple Risk Factor Intervention Trial. Am J Epidemiol. 2007;165(3):294–301. doi: 10.1093/aje/kwk014. [DOI] [PubMed] [Google Scholar]
- 33.Whitlock G, Norton R, Clark T, et al. Is body mass index a risk factor for motor vehicle driver injury? A cohort study with prospective and retrospective outcomes. Int J Epidemiol. 2003;32(1):147–149. doi: 10.1093/ije/dyg022. [DOI] [PubMed] [Google Scholar]
- 34.Batty GD, Deary IJ, Tengstrom A, et al. IQ in early adulthood and later risk of death by homicide: cohort study of 1 million men. Br J Psychiatry. 2008;193(6):461–465. doi: 10.1192/bjp.bp.107.037424. [DOI] [PubMed] [Google Scholar]
- 35.Batty GD, Modig Wennerstad K, Davey Smith G, et al. IQ in early adulthood and later cancer risk: cohort study of one million Swedish men. Ann Oncol. 2007;18(1):21–28. doi: 10.1093/annonc/mdl473. [DOI] [PubMed] [Google Scholar]
- 36.Silventoinen K, Modig-Wennerstad K, Tynelius P, et al. Association between intelligence and coronary heart disease mortality: a population-based cohort study of 682 361 Swedish men. Eur J Cardiovasc Prev Rehabil. 2007;14(4):555–560. doi: 10.1097/HJR.0b013e328014672e. [DOI] [PubMed] [Google Scholar]
- 37.David AS, Malmberg A, Brandt L, et al. IQ and risk for schizophrenia: a population-based cohort study. Psychol Med. 1997;27(6):1311–1323. doi: 10.1017/s0033291797005680. [DOI] [PubMed] [Google Scholar]
- 38.Gunnell D. Can adult anthropometry be used as a ‘biomarker’ for prenatal and childhood exposures? Int J Epidemiol. 2002;31(2):390–394. [PubMed] [Google Scholar]
- 39.Langenberg C, Shipley MJ, Batty GD, et al. Adult socioeconomic position and the association between height and coronary heart disease mortality: findings from 33 years of follow-up in the Whitehall study. Am J Public Health. 2005;95(4):628–632. doi: 10.2105/2004.046219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cox DR. Regression models and life-tables (with discussion) J R Stat Soc (B) 1972;34:187–220. [Google Scholar]
- 41.Deary IJ, Strand S, Smith P, et al. Intelligence and educational achievement. Intelligence. 2007;35:13–21. [Google Scholar]
- 42.Batty GD, Deary IJ, MacIntyre S. Childhood IQ and life course socioeconomic position in relation to alcohol induced hangovers in adulthood: the Aberdeen children of the 1950s study. J Epidemiol Community Health. 2006;60(10):872–874. doi: 10.1136/jech.2005.045039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Taylor MD, Hart CL, Davey Smith G, et al. Childhood mental ability and smoking cessation in adulthood: prospective observational study linking the Scottish Mental Survey 1932 and the Midspan studies. J Epidemiol Community Health. 2003;57(6):464–465. doi: 10.1136/jech.57.6.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Batty GD, Deary IJ, MacIntyre S. Childhood IQ in relation to risk factors for premature mortality in middle-aged persons: the Aberdeen Children of the 1950s study. J Epidemiol Community Health. 2007;61(3):241–247. doi: 10.1136/jech.2006.048215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Batty GD, Deary IJ, Schoon I, et al. Mental ability across childhood in relation to risk factors for premature mortality in adult life: the 1970 British Cohort Study. J Epidemiol Community Health. 2007;61(11):997–1003. doi: 10.1136/jech.2006.054494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Batty GD, Deary IJ, Schoon I, et al. Childhood mental ability in relation to food intake and physical activity in adulthood: the 1970 British Cohort Study [electronic article] Pediatrics. 2007;119(1):e38–e45. doi: 10.1542/peds.2006-1831. [DOI] [PubMed] [Google Scholar]
- 47.Kendrick D, Royal S. Inequalities in cycle helmet use: cross sectional survey in schools in deprived areas of Nottingham. Arch Dis Child. 2003;88(10):876–880. doi: 10.1136/adc.88.10.876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Khan I, Khan A, Aziz F, et al. Factors associated with helmet use among motorcycle users in Karachi, Pakistan. Acad Emerg Med. 2008;15(4):384–387. doi: 10.1111/j.1553-2712.2008.00049.x. [DOI] [PubMed] [Google Scholar]
- 49.Knight KK, Fielding JE, Goetzel RZ. Correlates of motor-vehicle safety behaviors in working populations. J Occup Med. 1991;33(6):705–710. doi: 10.1097/00043764-199106000-00011. [DOI] [PubMed] [Google Scholar]
- 50.Deary IJ, Der G, Ford G. Reaction times and intelligence differences: a population-based cohort study. Intelligence. 2001;29:389–399. [Google Scholar]
- 51.Whalley LJ, Deary IJ. Longitudinal cohort study of childhood IQ and survival up to age 76. BMJ. 2001;322(7290):1–5. doi: 10.1136/bmj.322.7290.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gottfredson LS. Intelligence: is it the epidemiologists’ elusive “fundamental cause” of social class inequalities in health? J Pers Soc Psychol. 2004;86(1):174–199. doi: 10.1037/0022-3514.86.1.174. [DOI] [PubMed] [Google Scholar]