Abstract
BACKGROUND:
Although an autoimmune mechanism has been postulated for myocarditis and acute-onset inflammatory dilated cardiomyopathy (DCM), immunomodulatory treatment strategies are still under investigation.
METHODS AND RESULTS:
The clinical data of six patients with acute inflammatory DCM referred for evaluation for possible heart transplantation were reviewed. All patients were admitted with acute congestive heart failure and severely impaired left ventricular (LV) function and were treated with high-dose (2 g/kg) intravenous immunoglobulin (IVIG). The diagnosis of acute inflammatory DCM was based on recent onset of congestive heart failure (New York Heart Association functional class III or IV) with severely depressed LV ejection fraction ([LVEF] 30% or lower) occurring shortly after viral-like illness. All patients had inflammation on endomyocardial biopsy or elevated cardiac enzymes, as well as a normal coronary angiogram. All patients were in New York Heart Association class I or II at the time of hospital discharge. The mean LVEF improved from 21.7±7.5% at baseline to 50.3±8.6% at discharge (P=0.005). Four patients had complete recovery (LVEF 50% or higher) and two patients had partial LV recovery. Patients were followed for a median 13.2 months (range two to 24 months) and had a mean LVEF of 53±6% (P not significant versus LVEF at discharge).
CONCLUSIONS:
Therapy with intravenous high-dose IVIG may be a potentially useful treatment in selected patients if given early in the course of acute fulminant inflammatory DCM. A randomized, prospective trial is warranted to prove the real benefit of IVIG in this patient population.
Keywords: Cardiomyopathies, Dilated cardiomyopathy, Heart failure, Intravenous immunoglobulins, Left ventricular dysfunction, Myocarditis
Abstract
HISTORIQUE :
Même si on postule qu’un mécanisme autoimmun déclenche la myocardite et la myocardiopathie dilatée (MCD) d’installation brutale, les stratégies de traitement immunomodulatoire sont toujours à l’étude
MÉTHODOLOGIE ET RÉSULTATS :
Les auteurs ont analysé les données cliniques de six patients atteints d’une MCD fulminante aiguë aiguillés en vue d’évaluer la possibilité d’une transplantation cardiaque. Au moment de l’hospitalisation, tous les patients souffraient d’insuffisance cardiaque congestive et d’une défaillance sévère de la fonction ventriculaire gauche (VG) et avaient été traités à l’aide de fortes doses (2 g/kg) d’immunoglobuline intraveineuse (IVIG). Le diagnostic de MCD aiguë se fondait sur la récente apparition d’une insuffisance cardiaque congestive (classification fonctionnelle III ou IV de la New York Heart Association) accompagnée d’une diminution marquée de la fraction d’éjection VG (FEVG 30 % ou moins) se manifestant peu après une maladie pseudovirale. Tous les patients présentaient une inflammation à la biopsie endomyocardique ou des enzymes cardiaques élevés ainsi qu’une coronarographie normale. Tous les patients étaient passés à la classification I ou II de la New York Heart Association au moment de leur congé de l’hôpital. La FEVG moyenne est passée de 21,7±7,5 % en début d’étude à 50,3±8,6 % au congé (P=0,005). Quatre patients se sont complètement rétablis (FEVG de 50 % ou plus) et deux patients ont profité d’un rétablissement VG partiel. Les patients ont été suivis pendant une période médiane de 13,2 mois (plage de deux à 24 mois) et avaient une FEVG moyenne de 53±6 % (P non significatif par rapport à la FEVG au congé).
CONCLUSIONS :
Un traitement à l’aide de fortes doses intraveineuses d’IVIG peut être utile chez des patients sélectionnés s’il est administré tôt dans l’évolution de la MCD fulminante aiguë. Un essai prospectif aléatoire s’impose pour démontrer les réels bienfaits de l’IVIG au sein de cette population de patients.
Recent-onset congestive heart failure (CHF) of nonischemic origin is mostly related to acute myocarditis or an idiopathic dilated cardiomyopathy (DCM) (1). Recently, a syndrome of inflammatory DCM has been described (2). Acute myocarditis is usually self-limited, but approximately one-half of patients continue to have significant left ventricular (LV) dysfunction, symptoms of CHF and a poor prognosis (3). Because an inflammatory process in the myocardium is a potentially reversible process, therapy to promote the recovery of LV function and improve the outcome of these patients should be aggressively sought. Limited success has been reported for treatment of acute myocarditis with corticosteroids and immunosuppressive drugs (4,5). Antiviral therapy is seldom used in clinical practice because the diagnosis of myocarditis is usually made weeks after acute viral infection, but it has been reported to have a positive effect in a murine Coxsackie virus myocarditis model in the acute viremic stage (6,7). To date, there have been few published reports of treatment with high-dose intravenous immunoglobulin (IVIG) therapy in patients with acute myocarditis and chronic DCM (8–14). The role of IVIG therapy, however, has not been clinically defined. In the present report, we describe six critically ill patients with an acute onset of heart failure due to fulminant inflammatory cardiomyopathy in whom high-dose IVIG treatment was followed by dramatic clinical improvement, including LV function recovery in each patient.
MATERIALS AND METHODS
The clinical and laboratory data of six critically ill patients with acute CHF and impaired LV function after a recent viral illness were reviewed. Each patient was referred for evaluation for possible heart transplantation (1998 to 2004) to the heart transplantation program at the Cedars-Sinai Medical Center (Los Angeles, USA). No other patients with acute fulminant inflammatory DCM were referred for heart transplantation over this time period. The study was approved by the institutional review board at the centre. LV ejection fraction (LVEF) was measured by two-dimensional echocardiography (15). A panel of tests was obtained to exclude systemic autoimmune disease, the presence of active infection and other specific reasons of acute cardiomyopathy. All patients had coronary angiography and right heart catheterization. An endomyocardial biopsy was obtained from four of the six patients.
Following baseline evaluation on conventional treatment for heart failure, IVIG (Gamunex 10%; Bayer Healthcare, Germany) was administered in a total dose of 2 g/kg of body weight. Three patients received 1 g/kg intravenously over 12 h on each of two successive days; two patients had 2 g/kg over 24 h and one patient was treated with a five-day course of 400 mg/kg per day.
Results are summarized as mean ± SD. Change in LVEF was assessed by paired t test. Change in New York Heart Association (NYHA) functional class was assessed by the Wilcoxon’s signed rank test. All significance tests were two-sided with a significance level of 0.05.
RESULTS
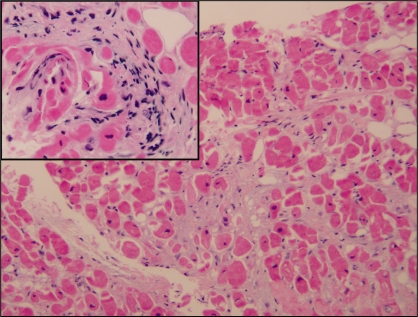
Six patients (three men; mean age 44±12 years) were admitted to the hospital shortly after a flu-like illness (range seven to 15 days) and presented with NYHA class III or IV symptoms. The clinical picture of the patients fulfilled four of the five criteria outlined by Reyes and Lerner (16) for the diagnosis of acute myocarditis. The clinical, laboratory hemodynamic and biopsy findings are shown in Table 1. Clinical examination revealed typical signs of left-sided heart failure in one patient and biventricular failure in the remaining five patients. Four patients had compromised hemodynamics on admission and received intravenous inotropic therapy; one was also on mechanical ventilatory support. Five of the six patients developed rhythm disturbances in the first 48 h: two had atrial fibrillation, two had ventricular tachycardia and one had complete atrioventricular block. The mean LVEF improved from 21.7±7.5% at baseline to 50.3±8.6% at discharge (P=0.005). Coronary angiography revealed no obstructive coronary artery disease. Of note, in two patients (cases 3 and 6), right heart catheterization was performed while the patients were receiving inotropic support. Histological analysis of endomyocardial biopsy samples identified definitive myocarditis using the Dallas criteria (17) in three patients and borderline myocarditis in one patient (Figure 1). No patient had evidence of amyloidosis, hemochromatosis or other noninflammatory infiltrative disease on endomyocardial biopsy.
TABLE 1.
Clinical and laboratory findings
| Patient | Age (years), sex | Days* | NYHA- p | NYHA- d | S3 | Pulmonary edema | Hypotension (BP <90 mmHg) | Right-sided CHF | Troponin I*, μg/L | CK^p‡, U/L | ESR§, mm/h | CI, L/min/m2 | Biopsy (Dallas criteria) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 20, female | 14 | 4 | 1 | + | + | + | + | 3.0 | 250 | 60 | 2.7 | Definitive myocarditis |
| 2 | 51, female | 15 | 4 | 1 | + | + | + | + | 15 | – | 66 | 2.0 | Definitive myocarditis |
| 3 | 48, male | 7 | 3 | 1 | + | + | + | + | 10.9 | 489 | 29 | 3.2¶ | Definitive myocarditis |
| 4 | 39, male | 7 | 4 | 1 | + | – | + | – | 19 | – | 59 | – | Not performed |
| 5 | 61, female | 14 | 3 | 2 | + | + | + | + | – | 287 | 26 | 1.9 | Not performed |
| 6 | 47, male | 9 | 4 | 1 | + | + | – | + | 11 | – | 51 | 2.6¶ | Borderline myocarditis |
| Mean | 44 | 11 | 3.7 | 1.2** | NA | NA | NA | NA | 11.8 | 342 | 47.8 | 2.5 | NA |
| SD | 12 | 3.7 | 0.5 | 0.4 | NA | NA | NA | NA | 6 | 105 | 18.8 | 0.5 | NA |
*Indicates duration from the onset of symptoms to intravenous immunoglobulin administration;
†Troponin I normal range is less than 0.4 μg/L;
‡Creatine kinase (CK) normal range is less than 160 U/L;
§Erythrocyte sedimentation rate (ESR) normal range is less than 20 mm/h;
¶Patients receiving inotropic support;
**P=0.03 when comparing New York Heart Association on discharge (NYHA-d) and NYHA prior to treatment (NYHA-p). BP Blood pressure; CHF Congestive heart failure; CI Cardiac index; NA Not applicable; S3 Third heart sound gallop
Figure 1).
Endomyocardial biopsy demonstrating inflammatory changes. Hematoxylin and eosin-stained section revealed myocardial tissue with areas of fibre dropout and degeneration (original magnification ×200). Inset demonstrates interstitial inflammatory cells composed primarily of lymphocytes and plasma cells (original magnification ×400)
Antibodies against a panel of viruses (HIV, Coxsackie B, enteric cytopathic human orphan virus, Epstein-Barr, cytomegalovirus, herpes simplex 1 and 2, adenovirus, influenza, parvovirus) were negative in four patients. Two patients were positive for Coxsackie B. Antinuclear antibody was positive in a speckled pattern at a titre of 1:40 in two patients, and rheumatoid factor was positive in one patient.
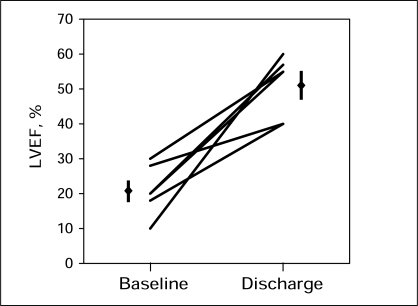
At a mean interval of 11±3.7 days after onset of symptoms, patients received IVIG (2 g/kg). All patients tolerated IVIG therapy without complications. As shown in Table 1, patients were discharged with a significant functional improvement of NYHA class. All patients demonstrated an improvement in LVEF on echocardiography at discharge (9.7±3.2 days) (Figure 2). Four patients had complete (LVEF 50% or higher) and two patients had partial LV recovery. Patients were followed for a median 13.2 months after therapy (range two to 24 months) and had a mean LVEF of 53±6% at follow-up (P not significant) compared with discharge. No patients required rehospitalization for CHF on follow-up.
Figure 2).
Left ventricular ejection fraction (LVEF) by echocardiography at baseline and at discharge in study patients. The mean ± SD LVEF was 21.7±7.5% before treatment and 50.3±8.6% at discharge (P=0.005)
DISCUSSION
According to the current World Health Organization classification of cardiomyopathies (2), a new entity, ‘inflammatory cardiomyopathy’, is defined as an inflammatory heart muscle disease associated with cardiac dysfunction.
Viruses are an important cause of myocarditis. Enterovirus and adenovirus have been confirmed as being cardiotropic for myocarditis (18). A direct cytopathic effect and the immune response to the virus are the two main pathways in the viral pathogenesis of myocarditis (19). There is a potential clinical application for antiviral therapy (interferon) when the virus persists in the myocardium (6).
Myocarditis can be diagnosed by clinical, histological and immunohistochemical criteria. Clinical features of myocarditis are variable, including recent CHF, arrhythmias, syncope and sudden death. The disease is often self-limited, and it is thought that the majority of these cases have a favourable prognosis. However, a report (3) evaluating the long-term prognosis of patients with biopsy-proven myocarditis showed a reduced five-year survival in this population. The wide spectrum of symptoms and LV dysfunction, ranging from asymptomatic status to fulminant disease, may be the reason why the prevalence of myocarditis is underestimated and the outcome of the disease is still poorly characterized. McCarthy et al (20) showed that most patients with fulminant myocardidis survived, but other reports (21,22) described very high mortality in a pediatric population with fulminant myocarditis. Recently, LV recovery has been reported in 33% of patients with acute myocarditis who required ventricular assist device implantation as a bridge to heart transplantation (23).
Endomyocardial biopsy using the Dallas criteria remains the standard tool for the diagnosis of myocarditis (17). The major limitation of endomyocardial biopsy is the low sensitivity due to sampling error in the presence of focal disease (5). Recently, immunohistological evaluation has been introduced to improve the diagnostic accuracy of endomyocardial biopsy (24).
At present, anti-inflammatory therapies for myocarditis remain an option in addition to conventional heart failure medication. However, most controlled trials have failed to prove the efficacy of therapy with corticosteroids, azathioprine or cyclosporine. Parrillo et al (4) studied 102 patients with DCM and showed an improvement in both LVEF and treadmill exercise duration with prednisone therapy in a subgroup of reactive patients. In a multicentre trial of 111 patients, Mason et al (5) evaluated the efficacy of immunosuppressive therapy with prednisone with either cyclosporine or azathioprine, but no significant difference was seen in LVEF or survival between those treated and not treated with immunosuppressive therapy. A recent study by Wojnicz et al (25) demonstrated a long-term benefit from three months of immunosuppressive therapy in selected patients with inflammatory DCM and human leukocyte antigen upregulation on biopsy.
Recently, treatment with high-dose IVIG has been introduced for patients with myocarditis, recent-onset DCM and peripartum cardiomyopathy (8,10–14,26,27). The immunomodulatory effects of IVIG are multifactorial: neutralization of pathogens, reduction of inflammatory cytokines and antiviral effects. Preliminary data from several clinical reports (8,11–14,27) with limited numbers of patients indicate that high-dose IVIG may be beneficial in patients with myocarditis and acute cardiomyopathy. Drucker et al (27) have reported on 21 children with presumed acute myocarditis treated with high-dose IVIG, which resulted in recovery of LV function and better survival. McNamara et al (8) performed an open trial of 10 adults with NYHA class III or IV heart failure, LVEF lower than 40% and symptoms of less than six months in duration, all of whom were treated with high-dose IVIG 2 g/kg. Significant improvement in LVEF was found in nine patients at 12-month follow-up. Whereas an increase in LVEF after treatment with IVIG was reported in nonrandomized trials on recent-onset DCM, the randomized trial with single administration of 2 g/kg IVIG failed to confirm a significant improvement in LVEF or functional capacity in patients treated with IVIG (10). The inclusion criteria were LVEF lower than 40%, an evaluation consistent with either myocarditis or idiopathic DCM, and onset of symptoms less than six months. Limitations of the latter study were that cellular inflammation was seen in a minority of patients, a clinical course compatible with acute myocarditis after a recent viral illness was not described in all cases and immunohistological evaluation was not performed to identify patients with myocardial inflammation. Thus, the present study addressed the efficacy of IVIG treatment in recent-onset DCM, but not the efficacy in patients with acute inflammatory DCM. A few case reports have suggested the beneficial effect of IVIG in patients with myocarditis and confirmed parvovirus and Coxsackie virus infection (11,12). Recently, Kishimoto et al (13) found improvement in LV function at follow-up in patients with myocarditis and acute DCM with reduction of cytokines shortly after IVIG treatment.
A positive effect on LV function and clinical outcome has been reported in patients with both chronic ischemic and nonischemic DCM (9). The ongoing double-blind, randomized, placebo-controlled, three-armed European Study on the Epidemiology and Treatment of Cardiac Inflammatory Disease (ESETCID) (28) with prednisolone and azathioprine, high- and intermediate-dose IVIG will be able to provide clear information regarding the efficacy of immunomodulatory therapies in inflammatory cardiomyopathy.
The present report described six critically ill patients with a dramatic picture of acute onset of severe heart failure and impaired LV function following a recent viral illness, with an elevated sedimentation rate, increased myocardial enzymes, and no evidence of coronary artery disease or other systemic disease. There was evidence of inflammation in all patients on endomyocardial biopsy and/or an increase of cardiac enzymes. In the present series of adult patients, the presentation and hospital course were consistent with acute fulminant inflammatory DCM, and IVIG was administered within two weeks from the onset of symptoms. After treatment with high-dose IVIG, improvement in functional class and LV function was observed, suggesting that the IVIG treatment was beneficial.
Limitations
The present descriptive report has several limitations. It is only a retrospective review of all patients with acute fulminant inflammatory DCM who have been referred for heart transplantation to our heart transplant program. The small number of patients can be explained by the fact that only a minority of patients with acute inflammatory cardiomyopathy develop circulatory instability and do not respond to the conventional therapy, and are consequently referred for heart transplantation. The rarity of such a fulminant course of myocarditis, which requires heart transplantation in adults, has recently been supported by Simon et al (23). Although there was no control group in our study and it is difficult to unequivocally demonstrate that the dramatic response is a result of only immunomodulatory treatment, we suggest that in selected critically ill patients who present with a typical clinical picture in an early course of acute myocarditis or acute inflammatory DCM, treatment with high-dose IVIG may be tried before heart transplantation is considered. No definitive conclusions regarding the beneficial effect of IVIG can be drawn until double-blind, placebo-controlled studies of IVIG in the population with acute inflammatory DCM are confirmed.
Footnotes
FINANCIAL SUPPORT: This work was supported, in part, by a grant from the Rav-Noy Foundation and the Save-A-Heart Foundation, Cedars-Sinai Medical Center, Los Angeles, California, USA.
REFERENCES
- 1.Michels VV, Moll PP, Miller FA, et al. The frequency of familial dilated cardiomyopathy in a series of patients with idiopathic dilated cardiomyopathy. N Engl J Med. 1992;326:77–82. doi: 10.1056/NEJM199201093260201. [DOI] [PubMed] [Google Scholar]
- 2.Richardson P, McKenna W, Bristow M, et al. Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the Definition and Classification of cardiomyopathies. Circulation. 1996;93:841–2. doi: 10.1161/01.cir.93.5.841. [DOI] [PubMed] [Google Scholar]
- 3.Grogan M, Redfield MM, Bailey KR, et al. Long-term outcome of patients with biopsy-proved myocarditis: Comparison with idiopathic dilated cardiomyopathy. J Am Coll Cardiol. 1995;26:80–4. doi: 10.1016/0735-1097(95)00148-s. [DOI] [PubMed] [Google Scholar]
- 4.Parrillo JE, Cunnion RE, Epstein SE, et al. A prospective, randomized, controlled trial of prednisone for dilated cardiomyopathy. N Engl J Med. 1989;321:1061–68. doi: 10.1056/NEJM198910193211601. [DOI] [PubMed] [Google Scholar]
- 5.Mason JW, O’Connell JB, Herskowitz A, et al. A clinical trial of immunosuppressive therapy for myocarditis. The Myocarditis Treatment Trial Investigators. N Engl J Med. 1995;333:269–75. doi: 10.1056/NEJM199508033330501. [DOI] [PubMed] [Google Scholar]
- 6.Kühl U, Pauschinger M, Schwimmbeck PL, et al. Interferon-beta treatment eliminates cardiotropic viruses and improves left ventricular function in patients with myocardial persistence of viral genomes and left ventricular dysfunction. Circulation. 2003;107:2793–8. doi: 10.1161/01.CIR.0000072766.67150.51. [DOI] [PubMed] [Google Scholar]
- 7.Takada H, Kishimoto C, Hiraoka Y. Therapy with immunoglobulin suppresses myocarditis in a murine coxsackievirus B3 model. Antiviral and anti-inflammatory effects. Circulation. 1995;92:1604–11. doi: 10.1161/01.cir.92.6.1604. [DOI] [PubMed] [Google Scholar]
- 8.McNamara DM, Rosenblum WD, Janosko KM, et al. Intravenous immune globulin in the therapy of myocarditis and acute cardiomyopathy. Circulation. 1997;95:2476–8. doi: 10.1161/01.cir.95.11.2476. [DOI] [PubMed] [Google Scholar]
- 9.Gullestad L, Aass H, Fjeld JG, et al. Immunomodulating therapy with intravenous immunoglobulin in patients with chronic heart failure. Circulation. 2001;103:220–5. doi: 10.1161/01.cir.103.2.220. [DOI] [PubMed] [Google Scholar]
- 10.McNamara DM, Holubkov R, Starling RC, et al. Controlled trial of intravenous immune globulin in recent-onset dilated cardiomyopathy. Circulation. 2001;103:2254–9. doi: 10.1161/01.cir.103.18.2254. [DOI] [PubMed] [Google Scholar]
- 11.Tedeschi A, Airaghi L, Giannini S, Ciceri L, Massari FM. High-dose intravenous immunoglobulin in the treatment of acute myocarditis. A case report and review of the literature. J Intern Med. 2002;251:169–73. doi: 10.1046/j.1365-2796.2002.00929.x. [DOI] [PubMed] [Google Scholar]
- 12.Stouffer GA, Sheahan RG, Lenihan DJ, Patel P, Lenihan DJ. The current status of immune modulating therapy for myocarditis: A case of acute parvovirus myocarditis treated with intravenous immunoglobulin. Am J Med Sci. 2003;326:369–74. doi: 10.1097/00000441-200312000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Kishimoto C, Shioji K, Kinoshita M, et al. Treatment of acute inflammatory cardiomyopathy with intravenous immunoglobulin ameliorates left ventricular function associated with suppression of inflammatory cytokines and decreased oxidative stress. Int J Cardiol. 2003;91:173–8. doi: 10.1016/s0167-5273(03)00002-0. [DOI] [PubMed] [Google Scholar]
- 14.Takeda Y, Yasuda S, Miyazaki S, Daikoku S, Nakatani S, Nonogi H. High-dose immunoglobulin G therapy for fulminant myocarditis. Jpn Circ J. 1998;62:871–2. doi: 10.1253/jcj.62.871. [DOI] [PubMed] [Google Scholar]
- 15.Naik MM, Diamond GA, Pai T, Soffer A, Siegel RJ. Correspondence of left ventricular ejection fraction determinations from two-dimensional echocardiography, radionuclide angiography and contrast cineangiography. J Am Coll Cardiol. 1995;25:937–42. doi: 10.1016/0735-1097(94)00506-L. [DOI] [PubMed] [Google Scholar]
- 16.Reyes MP, Lerner AM. Coxsackievirus myocarditis – with special reference to acute and chronic effects. Prog Cardiovasc Dis. 1985;27:373–94. doi: 10.1016/0033-0620(85)90001-5. [DOI] [PubMed] [Google Scholar]
- 17.Aretz HT, Billingham ME, Edwards WD, et al. Myocarditis. A histopathologic definition and classification. Am J Cardiovasc Pathol. 1987;1:3–14. [PubMed] [Google Scholar]
- 18.Why HJ, Meany BT, Richardson PJ, et al. Clinical and prognostic significance of detection of enteroviral RNA in the myocardium of patients with myocarditis or dilated cardiomyopathy. Circulation. 1994;89:2582–9. doi: 10.1161/01.cir.89.6.2582. [DOI] [PubMed] [Google Scholar]
- 19.Pauschinger M, Bowles NE, Fuentes-Garcia FJ, et al. Detection of adenoviral genome in the myocardium of adult patients with idiopathic left ventricular dysfunction. Circulation. 1999;99:1348–54. doi: 10.1161/01.cir.99.10.1348. [DOI] [PubMed] [Google Scholar]
- 20.McCarthy RE, III, Boehmer JP, Hruban RH, et al. Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. N Engl J Med. 2000;342:690–5. doi: 10.1056/NEJM200003093421003. [DOI] [PubMed] [Google Scholar]
- 21.Meyer T, Grumbach IM, Kreuzer H, Morguet AJ. Giant cell myocarditis due to coxsackie B2 virus infection. Cardiology. 1997;88:296–9. doi: 10.1159/000177346. [DOI] [PubMed] [Google Scholar]
- 22.Lee CH, Tsai WC, Hsu CH, Liu PY, Lin LJ, Chen JH. Predictive factors of a fulminant course in acute myocarditis. Int J Cardiol. 2006;109:142–5. doi: 10.1016/j.ijcard.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 23.Simon MA, Kormos RL, Murali S, et al. Myocardial recovery using ventricular assist devices: Prevalence, clinical characteristics, and outcomes. Circulation. 2005;112(Suppl):I32–6. doi: 10.1161/CIRCULATIONAHA.104.524124. [DOI] [PubMed] [Google Scholar]
- 24.Chander S, Talwar KK, Chopra P. Immunohistochemical characterisation and quantitative evaluation of lymphomononuclear cells in dilated cardiomyopathy –an endomyocardial biopsy study. Indian Heart J. 1995;47:360–4. [PubMed] [Google Scholar]
- 25.Wojnicz R, Nowalany-Kozielska E, Wojciechowska C, et al. Randomized, placebocontrolled study for immunosuppressive treatment of inflammatory dilated cardiomyopathy: Two-year follow-up results. Circulation. 2001;104:39–45. doi: 10.1161/01.cir.104.1.39. [DOI] [PubMed] [Google Scholar]
- 26.Bozkurt B, Villaneuva FS, Holubkov R, et al. Intravenous immune globulin in the therapy of peripartum cardiomyopathy. J Am Coll Cardiol. 1999;34:177–80. doi: 10.1016/s0735-1097(99)00161-8. [DOI] [PubMed] [Google Scholar]
- 27.Drucker NA, Colan SD, Lewis AB, et al. Gamma-globulin treatment of acute myocarditis in the pediatric population. Circulation. 1994;89:252–7. doi: 10.1161/01.cir.89.1.252. [DOI] [PubMed] [Google Scholar]
- 28.Maisch B, Richter A, Sandmöller A, Portig I, Pankuweit S, BMBF-Heart Failure Network Inflammatory dilated cardiomyopathy (DCMI) Herz. 2005;30:535–44. doi: 10.1007/s00059-005-2730-5. [DOI] [PubMed] [Google Scholar]