Abstract
OBJECTIVES
To examine the association of stopping to rest during a 400 meter usual-pace walk test (400-MWT) with incident mobility disability in older persons with functional limitations.
DESIGN
Prospective cohort study
SETTING
Community-based
PARTICIPANTS
Four hundred twenty-four participants of the Lifestyle Intervention and Independence for Elders Pilot (LIFE-P) Study aged 70–89 years, having functional limitation (summary score =9 on the Short Physical Performance Battery (SPPB)), and being able to complete the 400-MWT within 15 minutes.
MEASUREMENTS
Rest stops during the 400-MWT were recorded. The onset of mobility disability, defined as being unable to complete the 400-MWT or taking more than 15 minutes to do so, was recorded at months 6 and 12.
RESULTS
Fifty-four (12.7%) participants rested during the 400-MWT at baseline, of whom 37.7% experienced mobility disability during follow-up versus 8.6% of those not stopping to rest. Performing any rest stop was strongly associated with incident mobility disability at follow-up (odds ratio (OR) = 5.4, 95% confidence interval (CI) = 2.7–10.9) after adjustment for age, gender, and clinic site. This association was diminished, but remained statistically significant, after further adjusting for SPPB and the time to complete the 400-MWT simultaneously (OR = 2.6, 95%CI = 1.2–5.9).
CONCLUSION
Stopping to rest during the 400-MWT is strongly associated with incident mobility disability in non-disabled older persons with functional limitations. Given the prognostic value, rest stops should be recorded as part of the standard assessment protocol for the 400-MWT.
Keywords: mobility disability, aging, physical performance test
INTRODUCTION
Losing functional independence is a major concern of older individuals.1 The 400-meter usual-pace walk test (400-MWT) is a highly reliable performance-based measure of mobility.2 Chang et al. have reported that the incidence of loss of ability to walk 400 meters was 33.9% over a 21-month follow-up period in a group aged 75–85 who had functional limitations.3 Time to complete the 400-MWT at baseline was the strongest predictor of subsequent loss of mobility. Furthermore, these investigators identified a potential threshold in the time to complete the 400-MWT at baseline of 7 minutes, at or above which the proportion of persons unable to complete the test at follow-up was substantially higher. Newman et al. showed that in non-disabled older persons each one minute increase in the time required to complete the 400-meter walk performed as quickly as possible was associated with a 52% increased risk of mobility disability (defined as two consecutive reports of severe difficulty or inability walking a quarter of a mile or climbing stairs).4
However, another factor that could predict the risk of mobility disability is the need to rest during the 400-MWT. This might provide important prognostic information and potentially be more important than, for example, the time to complete the test. The number of rest stops allowed during the 400-MWT is unlimited; however, to complete the test successfully rest stops longer than 60 seconds and sitting are not allowed.2 Rolland et al. reported a mean number of rest stops per person of 0.7 (SD 1.5) in a group of community-dwelling participants (n=60), aged 65 or older, who had self-reported difficulty in two or more of four functional domains. The need to rest during the 400-MWT may identify individuals who are at a high risk for developing mobility disability despite successfully completing the 400-MWT. To our knowledge, the clinical utility of needing to rest during the 400-MWT have not been previously evaluated, especially in relation to the onset of subsequent mobility disability.
The aim of the present study was to determine whether participants who stop to rest during the 400-MWT at baseline are more likely to develop mobility disability as compared with those who do not stop to rest during the baseline assessment.
METHODS
Participants
The study participants were recruited from four sites (Dallas, Texas; Stanford, California; Pittsburgh, Pennsylvania; and Winston-Salem, North Carolina) to the Lifestyle Intervention and Independence for Elders Pilot (LIFE-P) Study, a randomized controlled pilot clinical trial evaluating the effect of physical activity on mobility disability. Participants were 424 community-dwelling older men and women between 70–89 years of age who had functional limitations (as described below), were able to complete the 400-MWT within 15 minutes without the use of an assistive device, and had a sedentary lifestyle (i.e., less than 20 minutes a week of regular physical activity during the past month). Potential participants were excluded if they had a Mini-Mental State Examination (MMSE) score5 less than 21 or had one or more of the following conditions: uncontrolled angina, Parkinson’s disease or cancer requiring treatment in the past three years. Details of the entry criteria and the recruitment process have been previously described.6,7
Main variables
The main independent variable was the need to rest during the baseline assessment of the 400-MWT,2 which was performed at usual pace. In the 400-MWT, any standing rest stop was allowed as long as it did not exceed 60 seconds. The number and duration of rest stops were recorded in intervals of <30 seconds and 30–60 seconds. Our main interest was whether any rest stop (yes/no) was associated with mobility disability. A secondary question was whether increased numbers of rest stops were associated with increased risk of mobility disability. Lastly, in sub-analyses, 15 or 45 seconds per rest were subtracted from the total walk time for rest stops of <30 seconds and 30–60 seconds, respectively.
The main outcome variable was the loss of ability to complete the 400-MWT within 15 minutes without sitting and without the use of an assistive device (including a cane) during a reassessment at either 6 or 12 months. Thus, mobility disability is defined as being unable to complete the 400-MWT within 15 minutes without sitting. If the 400-MWT could not be assessed at follow-up, the outcome was adjudicated by a committee of investigators masked to intervention group.8 Available information at follow-up was reviewed and mobility disability was determined to be present if any of the following were found: 1) the observation of a 4-meter walking speed below 0.4 meter/second at a home/clinic assessment, 2) the inability to walk across a room without assistance of another person or assistive device as evident from either observation or self/proxy-reports collected in person or by telephone, or 3) medical records documenting the participant being unable to walk such as when bed/wheelchair-bound. The mobility disability outcome was defined as indeterminate if information was insufficient to adjudicate the outcome.
Functional limitation is defined as having a SPPB score of 9 or below. The SPPB evaluates balance, gait, and strength.9,10 For balance, participants were asked to stand with their feet in side-by-side, semi-tandem, and tandem balance positions for 10 seconds each. Participants were then asked to walk a distance of four meters at their usual pace. The quickest time out of two trials was chosen for further analysis. Finally, participants were asked to rise from a chair five times as quickly as possible while keeping their arms folded over their chest. Details on scoring of the tests have been described previously.9,10 Briefly, the sum of sub-scores of the balance, walking, and chair-rise tests yields the total SPPB score, ranging from 0 to 12 (best function).
Baseline characteristics
Participant characteristics included age, gender, race, body mass index (BMI), and cognitive function, evaluated with the Mini-Mental State Examination (MMSE).5 Total number (maximum = 10) of clinical conditions was ascertained using the question “Has a doctor ever told you that you have…”: high blood pressure or hypertension; heart attack, coronary, or myocardial infarction; congestive heart failure; stroke or brain hemorrhage; cancer or a malignant tumor (excluding minor skin cancers); diabetes, sugar in the urine, or high blood sugar; broken or fractured hip; lower limb arthritis; cirrhosis or liver disease; and chronic lung disease (i.e., chronic bronchitis, COPD, asthma, or emphysema). The total number (maximum = 9) of symptoms (anxiety, fatigue, decreased appetite, insomnia, dizziness, muscle or joint stiffness, muscle strain or soreness, sprain (ankle or knee), foot pain) within the past 6 months was determined. Self-rated health status was assessed and participants reporting fair and poor health were distinguished from those reporting excellent, very good, or good health.
Participants were asked about the farthest distance walked at one time in the past two weeks without sitting to rest (less than ½ mile (0.4 km) versus others). Self-reported limitation in walking one mile was defined as “having difficulty in walking one mile”, and limitation in climbing stairs was defined as “having a lot of difficulty” with this task. Usual walking speed across 4 meters (m/sec) was assessed.
Self-efficacy in walking ability was evaluated after completing the 400-MWT, and high efficacy was defined as complete confidence (i.e., 10 on a 10-point scale) in being able to walk 5 laps at the same speed one week after initially completing the 400-MWT.11
Finally, intervention assignment (physical activity (PA) or successful aging (SA) intervention), which has previously been described in detail,6,8 was included to examine whether PA participation could decrease the impact of stopping to rest on incident mobility disability. In short, the PA intervention included walking and strength, flexibility and balance exercises. The intervention had three phases, passing from primarily supervised, group-based sessions to home-based exercise. Between four and five sessions per week were encouraged throughout the intervention period. The SA intervention comprised group-based sessions focusing on health education such as nutrition, medication use, and foot care and was employed to provide this control group attention in the study period. During the first 26 weeks participants had weekly sessions, followed by monthly sessions until the end of the study.
Statistical Analyses
Baseline characteristics of participants who stopped to rest (REST) during the 400-MWT and those who did not rest (NO-REST) were compared using un-paired Student t tests or Chi-square tests to examine group differences. Any variable that yielded a group difference with a p-value below 0.1 was used as a covariate for the subsequent logistic regression analyses which were used to assess the association of stopping to rest during the 400-MWT with mobility disability at either 6 or 12 month follow-up. The association of stopping to rest with mobility disability at follow-up was further examined in age-, sex- and clinic examination site-adjusted analyses stratified by selected baseline variables: age, gender, SPPB score, 400-MWT, and intervention group assignment. All statistical analyses were performed using SAS version 9.1 (SAS, Cary, NC) and a 5% two-tailed level of significance was applied.
RESULTS
At baseline, 54 (12.5%) participants stopped to rest during the 400-MWT. As shown in Table 1, participant’s mean age was 76.8 years (standard deviation (SD) = 4.2). Participants who stopped to rest were significantly more likely to be female, have higher BMI, lower extremity arthritis, and walking limitations than those who completed the 400-MWT at baseline without resting. Additionally, those who rested performed more poorly on the SPPB, were slower to complete both the 4 meter walk and 400-MWT as compared with those who did not rest. The percentage being confident in completing 5 laps of the 400-MWT at the same speed the following week was lower in those who rested than in those who did not rest (70% versus 90%). No differences were observed between the two groups in MMSE score, total number of clinical conditions or symptoms, self-rated health (Table 1). Fifty percent of both those who rested and those who did not rest were assigned to the physical activity intervention. Among 213 participants in the physical activity group 27 rested and among 211 in the successful aging 27 participants rested.
Table 1.
Baseline Characteristics of All Participants and by Rest Stopping Performance During the 400-Meter Walk Test.
| All participants (n=424) | REST (n=54) | NO-REST (n=370) | P-value | |
|---|---|---|---|---|
| Age, years | 76.8±4.2 | 77.6±3.8 | 76.6±4.3 | 0.09 |
| Women, % | 69.1 | 81.5 | 67.3 | 0.04 |
| Race | 0.87 | |||
| White | 74.3 | 72.2 | 74.6 | |
| Black | 18.2 | 18.5 | 18.1 | |
| Other | 7.5 | 9.3 | 7.3 | |
| Geographical location | <0.01 | |||
| Dallas, TX | 24.3 | 9.3 | 26.5 | |
| Palo Alto, CA | 25.7 | 35.2 | 24.3 | |
| Pittsburgh, PA | 25.0 | 37.0 | 23.2 | |
| Winston-Salem, NC | 25.0 | 18.5 | 25.9 | |
| Body Mass Index, kg/m2 | 30.2±6.0 | 32.5±6.3 | 29.9±5.9 | <0.01 |
| MMSE, score | 27.3±2.3 | 27.2±2.3 | 27.3±2.3 | 0.66 |
| Total number of clinical conditions* | 1.7±1.1 | 1.9±1.3 | 1.6±1.1 | 0.17 |
| Hypertension, % | 69.3 | 74.1 | 68.6 | 0.41 |
| Myocardial infarction, % | 9.4 | 9.6 | 9.3 | 0.95 |
| Congestive heart failure, % | 5.8 | 9.3 | 5.3 | 0.24 |
| Stroke or brain hemorrhage, % | 4.8 | 3.7 | 4.9 | 0.70 |
| Cancer or a malignant tumor, % | 17.7 | 20.4 | 17.3 | 0.58 |
| Diabetes, % | 22.1 | 23.5 | 21.9 | 0.79 |
| Broken or fractured hip, % | 3.1 | 5.7 | 2.7 | .25 |
| Lower limb arthritis, % | 20.6 | 31.5 | 19.0 | .03 |
| Cirrhosis or liver disease, % | 2.6 | 5.6 | 2.2 | .15 |
| Chronic lung disease, % | 14.0 | 11.5 | 14.3 | .59 |
| Total number of symptoms* (last 6 months) | 3.1±1.9 | 2.9±1.9 | 3.1±1.9 | .38 |
| Self-rated health, fair and very poor, % | 20.3% | 22.2 | 20.0 | .70 |
| Less than 1/4 mile walked in previous 2 weeks, % | 53.0 | 68.5 | 50.7 | .01 |
| Limited in walking a mile, % | 53.9 | 83.3 | 49.4 | <.001 |
| Limited a lot in climbing stairs, % | 6.3 | 5.7 | 6.3 | .85 |
| Complete confidence in walking 5 laps, % | 87.2 | 70.4 | 89.7 | <.001 |
| SPPB, score | 7.5±1.4 | 6.8±1.5 | 7.6±1.4 | <.001 |
| 4 meter walk time, m/sec | 0.74±0.16 | 0.66±0.14 | 0.75±0.16 | <.001 |
| 400 meter walk time, minutes | 8.17±1.89 | 10.31±2.16 | 7.86±1.64 | <.001 |
| Randomized to Physical Activity Intervention, % | 50.2 | 50.0 | 50.3 | .93 |
Note: Continuous variables are reported as mean ± standard deviation. MMSE denotes Mini Mental State Examination; SPPB denotes Short Physical Performance Battery. REST and NO-REST denote groups of participants stopping to rest or not during the 400-meter walk test.
For details on included diseases and symptoms, see methods.
Four hundred seven participants were tested for mobility disability at least once during the follow-up and 372 were tested twice. Mobility disability could not be adjudicated for twelve surviving participants and two who died before follow-up. These participants were not systematically different at baseline from the participants with non-missing mobility disability outcome. The proportions of adjudicated failures and indeterminate outcomes and deaths in those who rested were not significantly different as compared with those who did not rest.
The percentage of participants failing the 400-MWT at follow-up was 37.7% in those who rested and 8.7% in those who did not rest. Among those who rested, there was no step-wise increase in the rate of failing the 400-MWT as a function of the number of rest stops (P = 0.77). In both groups, the percentage of participants failing the 400-MWT at follow-up was higher in those taking longer to complete the baseline 400-MWT. Those completing the baseline 400-MWT in less than 8 minutes had a low incidence of failing the 400-MWT at follow-up, and there were few among those stopping to rest who completed the walk this fast at baseline. In contrast, the percentage of failure in the group needing 10 or more minutes to complete the 400-MWT was 48% in those who rested as compared with 25% in those who did not rest.
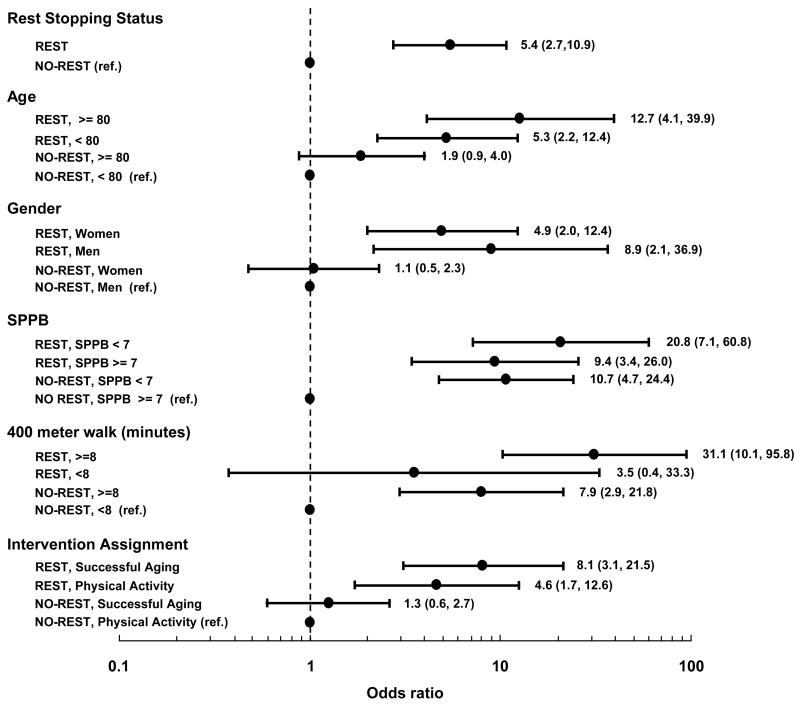
Adjusted for age, sex, and clinic site, the likelihood of mobility disability at follow-up was more than 5 times higher in those who rested as compared with those who did not rest (OR 5.4; CI 2.7–10.9). As shown in Figure 1, even when stratified by age, gender, SPPB, 400 meter walking time, and intervention assignment, those stopping to rest generally had an increased likelihood of failing the 400 meter walk at follow-up compared with those who did not. For example, those who rested and were less than 80 years or 80 years or older were 5.3 and 12.7 times more likely to develop mobility disability, respectively, than those who did not rest and were younger than 80 years old.
Figure 1.
Odds Ratios (95 % Confidence Intervals) for Mobility Disability at Follow-up According to Stratification by Rest Stop Status, Age, Gender, Performance in Short Physical Performance Battery (SPPB) and 400-Meter Walk, and Intervention Group Assignment. Note: The black circle and the horizontal lines correspond to odds ratio and 95% confidence interval. Adjusted for age, sex, and clinic examination site.
Separate analyses were performed in those who rested and those who did not rest to examine the possible protective effect of being assigned to the physical activity intervention as compared with the successful aging intervention (data not shown). In those who rested, being assigned to the intervention with physical activity was associated with a non-significant but substantial reduction in the likelihood of mobility disability (OR 0.3, CI 0.1–1.3) at follow-up. In those who did not rest, there was also a non-significant, but smaller reduction in the likelihood of mobility disability (OR 0.8; CI 0.4–1.7) associated with being assigned to the physical activity intervention.
Table 2 shows the association of rest stopping with subsequent mobility disability adjusting for age, gender, clinic site, 400 meter walking time, SPPB, self-reported one mile walking limitation, walking efficacy, lower limb arthritis and BMI. In general, adjustment for 400 meter walking time resulted in the largest reduction in the association. But even when simultaneously adjusting for SPPB and 400 meter walking time together with the variables in the first model there was still a 2-fold increased likelihood of mobility disability (Table 2, Model 4). When adjusting for all variables simultaneously, persons who rested at baseline were more than twice as likely to develop mobility disability, but this did not reach statistical significance (OR 2.1; CI 0.9–4.9, P = 0.09) (Table 2, Model 7). In analysis not shown, utilizing the 400 meter walking time subtracting the estimated time to do the rest stops did not substantially change the estimates. Lastly, entering intervention assignment did not affect the results.
Table 2.
Adjusted Association of Stopping to Rest with Mobility Disability at Follow-up.
| Variable | Model 1 | Model 2 | Model 3 | Model 4 | Model 5* | Model 6* | Model 7* |
|---|---|---|---|---|---|---|---|
| Rest Stop Status | |||||||
| REST | 5.4 (2.7, 10.9) | 2.5 (1.1, 5.5) | 4.3 (2.1, 9.0) | 2.6 (1.2, 5.9) | 3.7 (1.8, 7.7) | 5.0 (2.5, 10.1) | 2.1 (0.9, 4.9) |
| NO-REST (Ref) | |||||||
| 400-meter walking time, minutes | 1.5 (1.3, 1.8) | 1.4 (1.1, 1.6) | 1.3 (1.1, 1.6) | ||||
| SPPB, score | 0.6 (0.5, 0.7) | 0.7 (0.5, 0.8) | 0.7 (0.5, 0.9) | ||||
| Limited in walking a mile | |||||||
| Missing (n=64) | 2.9 (0.8, 10.2) | 1.7 (0.4, 6.6) | |||||
| Limited a lot | 5.7 (2.1, 15.3) | 3.6 (1.3, 10.4) | |||||
| Not limited (Ref) | |||||||
| Walking efficacy 5 laps | 0.4 (0.2, 0.8) | 0.5 (0.2, 1.0) | |||||
| Lower limb arthritis | 0.9 (0.4, 2.0) | 1.2 (0.5, 2.6) | |||||
| BMI | 1.0 (1.0, 1.1) | 1.0 (1.0, 1.1) | |||||
Note: Results are presented as odds ratios (95% confidence interval). Association of stopping to rest with mobility disability is in the full model (Model 7) adjusted for age, sex, clinic site, 400-meter walking time, Short Physical Performance Battery (SPPB) score, limitation in walking 1 mile, self-efficacy in walking 5 laps of the 400 meter walk (100 m), lower limb arthritis and Body Mass Index (BMI). Separate models are adjusted as follows: 1. Age, sex, clinic site (individual estimates for these not shown any of the models). 2. Model 1 + 400-meter walking time. 3. Model 1 + SPPB. 4. Model 2 + SPPB. 5. Model 1 + limited in walking 1 mile and walking efficacy 5 laps. 6. Model 1 + lower limb arthritis and BMI. 7. Full model. REST and NO-REST denote groups of participants stopping to rest or not during the 400-meter walk test. SPPB denotes Short Physical Performance Battery.
Measures of walking efficacy and lower limb arthritis each had one missing participant (see Table 1) who were excluded from the models.
DISCUSSION
The present study evaluated the association between stopping to rest during the 400-MWT and incident mobility disability in older persons with functional limitations. The primary finding of this analysis was that persons stopping to rest during a 400-MWT were more likely to develop future mobility disability. The association between stopping to rest and incident mobility disability was diminished, but remained statistically significant, after simultaneous adjustment for SPPB and the time to complete the 400-MWT. Simultaneously adjustment for all variables under study resulted in loss of statistical significance but this may result from having a small number of at risk persons and small number of events. No gradient between the number of rest stops and increased probability of mobility disability was observed.
This study demonstrated a strong association between rest stops and mobility disability, but the mechanisms underlying this association are not known. It is conceivable that stopping to rest is simply a characteristic of more physically impaired older persons who are on the brink of mobility disability. Interestingly, while those who rested had poorer physical functioning as compared with those who did not rest, there was no significant difference with regard to cognitive function, total number of diseases, total number of symptoms, and self-rated health.
On average, those who rested were 2.45 minutes slower in performing the 400-MWT as compared with those who did not rest. We evaluated whether the time actually spent stopping to rest biased the analyses of association between stopping to rest and mobility disability by subtracting time for each rest stop from the time to complete the 400-MWT but the results were essentially unchanged.
Self-efficacy in walking ability was significantly lower in those who rested as compared with those who did not rest. Participants were asked about their level of confidence in being able to walk 5 laps at the same speed as in the just finished 400-MWT one week later. Self-efficacy theory would predict that successful completion of the 400-MWT would increase one’s confidence in their ability to successfully complete the walk in the near future.12 However, stopping to rest during the 400-MWT reduced self-efficacy to the point that those who rested thought more negatively of future success in completing an even shorter distance of 100 meters (5 laps). It is likely that those who rested were more fatigued than those who did not rest, which may have reduced their confidence in their ability to complete a future walk. Focht and colleagues reported that fatigue was negatively associated with self-efficacy after acute physical exercise.13
Participation in physical activity reduced the risk of mobility disability non-significantly by 70% in those who rested and 20% in those who did not rest. Despite being non-significant, this reduction may be a true effect, as the main study was not powered to determine the effect of physical activity on mobility disability.6,8 Although speculative, the observed 70% reduction in risk of mobility disability in the physical activity group compared with the successful aging group among those who rested might partly be due to improved lower extremity function and a concomitant increased self-efficacy in the walking task.8,14
Some limitations of the study should be considered when interpreting the present results. The extent to which performing rest stops is a symptom of peripheral artery disease is not known because data to identify this condition was not collected.15,16 Assessing in depth why the rest stop was performed would have been helpful. However, reasons to completely discontinue the walk test at any time during the follow-up were assessed and 12 of a total of 75 reported leg pain, indicating that leg pain is an important factor for mobility disability, as has been observed previously.17 The most frequently stated reason for completely stopping the walk was shortness of breath (n=15). The definition of mobility disability, as assessed using an objective measurement of walking 400 meter, has been used previously 3,6 but is unlike definitions of mobility disability based on self-reported ability to perform given tasks. 4,18 Differences in definitions should be considered when interpreting these results.
In conclusion, stopping to rest when performing the 400-MWT at usual speed is strongly associated with future incident mobility disability in non-disabled older persons with functional limitations. A better understanding of why people stop to rest when tested on the 400-MWT might lead to improved interventions to prevent mobility disability.
Acknowledgments
Financial Disclosure: This study was supported by a Cooperative Agreement with the National Institute on Aging, UO1 AG022376, and in part by the Intramural Research Program, National Institute on Aging, NIH. Dr. Gill is the recipient of a Midcareer Investigator Award in Patient-Oriented Research (K24AG021507) from the National Institute on Aging. Studenski was supported by grants AG024827 and AG023641.
| Elements of Financial/Personal Conflicts | Sonja Vestergaard | Kushang V. Patel | Michael P. Walkup | Marco Pahor | ||||
|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | X | X | X | X | ||||
| Grants/Funds | X | X | X | X | ||||
| Honoraria | X | X | X | X | ||||
| Speaker Forum | X | X | X | X | ||||
| Consultant | X | X | X | X | ||||
| Stocks | X | X | X | X | ||||
| Royalties | X | X | X | X | ||||
| Expert Testimony | X | X | X | X | ||||
| Board Member | X | X | X | X | ||||
| Patents | X | X | X | X | ||||
| Personal Relationship | X | X | X | X | ||||
| Elements of Financial/Personal Conflicts | Anthony P. Marsh | Mark A. Espeland | Stephanie Studenski | Thomas M. Gill | ||||
| Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | X | X | X | X | ||||
| Grants/Funds | X | X | X | X | ||||
| Honoraria | X | X | X | X | ||||
| Speaker Forum | X | X | X | X | ||||
| Consultant | X | X | X | X | ||||
| Stocks | X | X | X | X | ||||
| Royalties | X | X | X | X | ||||
| Expert Testimony | X | X | X | X | ||||
| Board Member | X | X | X | X | ||||
| Patents | X | X | X | X | ||||
| Personal Relationship | X | X | X | X | ||||
| Elements of Financial/Personal Conflicts | Timothy Church, | Jack M. Guralnik | ||||||
| Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | X | X | ||||||
| Grants/Funds | X | X | ||||||
| Honoraria | X | X | ||||||
| Speaker Forum | X | X | ||||||
| Consultant | X | X | ||||||
| Stocks | X | X | ||||||
| Royalties | X | X | ||||||
| Expert Testimony | X | X | ||||||
| Board Member | X | X | ||||||
| Patents | X | X | ||||||
| Personal Relationship | X | X | ||||||
Dr. Studenski is a consultant for Merck and Co., Glaxo Smith Kline, Asubio and Eli Lilly and Co.
Footnotes
Author Contributions: Sonja Vestergaard: study concept and design, analysis and interpretation of data, preparation of the manuscript. Kushang V. Patel: analysis and interpretation of data, preparation of manuscript. Michael P. Walkup: analysis of data, preparation of manuscript. Marco Pahor, Anthony P. Marsh, Mark A. Espeland, Stephanie Studenski, Thomas M. Gill, Timothy Church: acquisition of participants and data, interpretation of data, preparation of manuscript. Jack M. Guralnik: study concept and design, acquisition of participants and data, interpretation of data, preparation of the manuscript.
Sponsor’s Role: The granting institutions named above did not interfere in any way with the design, methods, participants’ recruitment, data collection, or analysis and preparation of the manuscript.
References
- 1.Salkeld G, Cameron ID, Cumming RG, et al. Quality of life related to fear of falling and hip fracture in older women: a time trade off study. BMJ. 2000;320:341–346. doi: 10.1136/bmj.320.7231.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rolland YM, Cesari M, Miller ME, et al. Reliability of the 400-m usual-pace walk test as an assessment of mobility limitation in older adults. J Am Geriatr Soc. 2004;52:972–976. doi: 10.1111/j.1532-5415.2004.52267.x. [DOI] [PubMed] [Google Scholar]
- 3.Chang M, Cohen-Mansfield J, Ferrucci L, et al. Incidence of loss of ability to walk 400 meters in a functionally limited older population. J Am Geriatr Soc. 2004;52:2094–2098. doi: 10.1111/j.1532-5415.2004.52570.x. [DOI] [PubMed] [Google Scholar]
- 4.Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295:2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- 5.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 6.Rejeski WJ, Fielding RA, Blair SN, et al. The lifestyle interventions and independence for elders (LIFE) pilot study: Design and methods. Contemp Clin Trials. 2005;26:141–154. doi: 10.1016/j.cct.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Katula JA, Kritchevsky SB, Guralnik JM, et al. Lifestyle Interventions and Independence for Elders pilot study: recruitment and baseline characteristics. J Am Geriatr Soc. 2007;55:674–683. doi: 10.1111/j.1532-5415.2007.01136.x. [DOI] [PubMed] [Google Scholar]
- 8.The LIFE Study Investigators. Effects of a Physical Activity Intervention on Measures of Physical Performance: Results of the Lifestyle Interventions and Independence for Elders Pilot (LIFE-P) Study. J Gerontol A Biol Sci Med Sci. 2006;61:1157–1165. doi: 10.1093/gerona/61.11.1157. [DOI] [PubMed] [Google Scholar]
- 9.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 10.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–M231. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 11.Rejeski WJ, Brawley LR, Ambrosius WT, et al. Older adults with chronic disease: benefits of group-mediated counseling in the promotion of physically active lifestyles. Health Psychol. 2003;22:414–423. doi: 10.1037/0278-6133.22.4.414. [DOI] [PubMed] [Google Scholar]
- 12.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 13.Focht BC, Knapp DJ, Gavin TP, et al. Affective and self-efficacy responses to acute aerobic exercise in sedentary older and younger adults. J Aging Phys Act. 2007;15:123–138. doi: 10.1123/japa.15.2.123. [DOI] [PubMed] [Google Scholar]
- 14.Rejeski WJ, King AC, Katula JA, et al. Physical activity in prefrail older adults: confidence and satisfaction related to physical function. J Gerontol B Psychol Sci Soc Sci. 2008;63:19–26. doi: 10.1093/geronb/63.1.p19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gardner AW, Montgomery PS, Afaq A. Exercise performance in patients with peripheral arterial disease who have different types of exertional leg pain. J Vasc Surg. 2007;46:79–86. doi: 10.1016/j.jvs.2007.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McDermott MM, Hoff F, Ferrucci L, et al. Lower extremity ischemia, calf skeletal muscle characteristics, and functional impairment in peripheral arterial disease. J Am Geriatr Soc. 2007;55:400–406. doi: 10.1111/j.1532-5415.2007.01092.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McDermott MM, Greenland P, Liu K, et al. Leg symptoms in peripheral arterial disease: associated clinical characteristics and functional impairment. JAMA. 2001;286:1599–1606. doi: 10.1001/jama.286.13.1599. [DOI] [PubMed] [Google Scholar]
- 18.Shumway-Cook A, Patla A, Stewart AL, et al. Assessing environmentally determined mobility disability: Self-report versus observed community mobility. Journal of the American Geriatrics Society. 2005;53:700–704. doi: 10.1111/j.1532-5415.2005.53222.x. [DOI] [PubMed] [Google Scholar]