Abstract
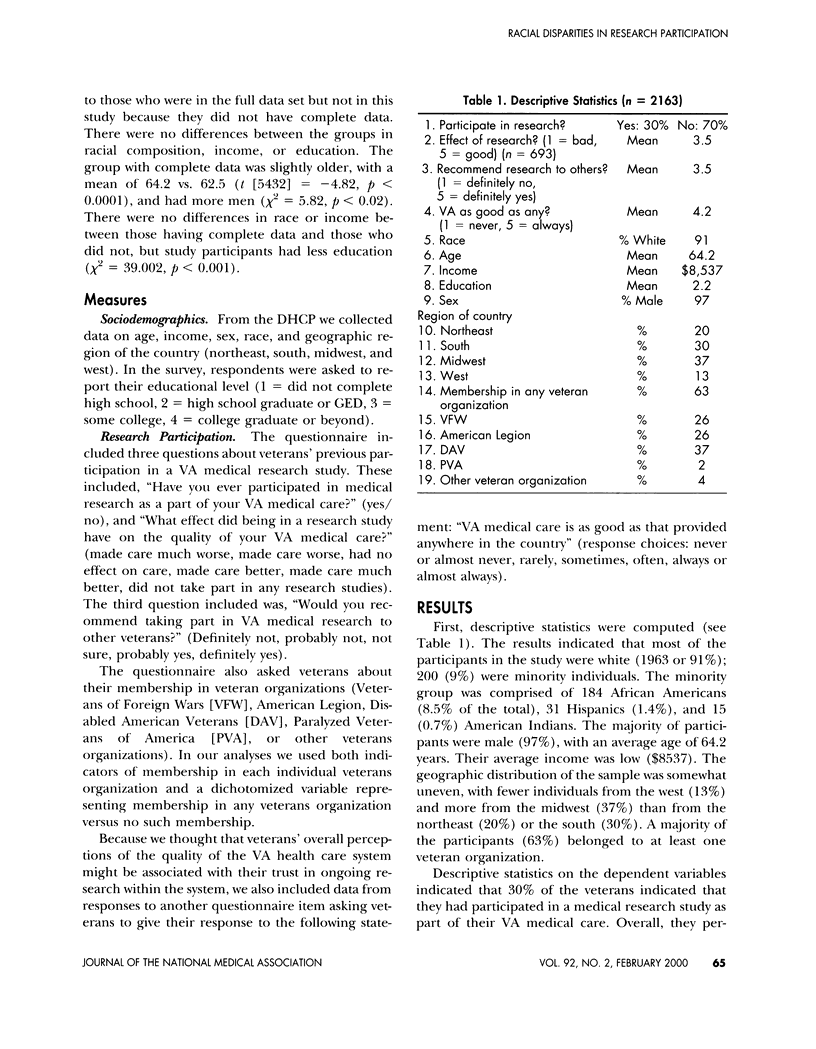
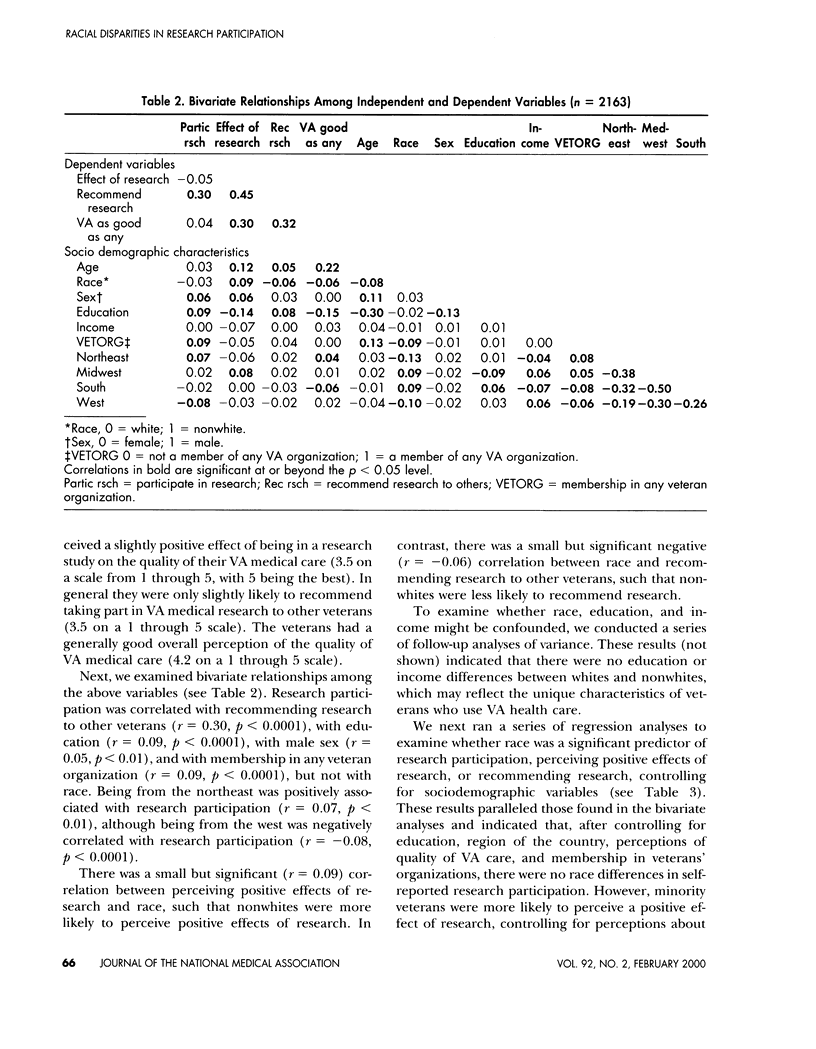
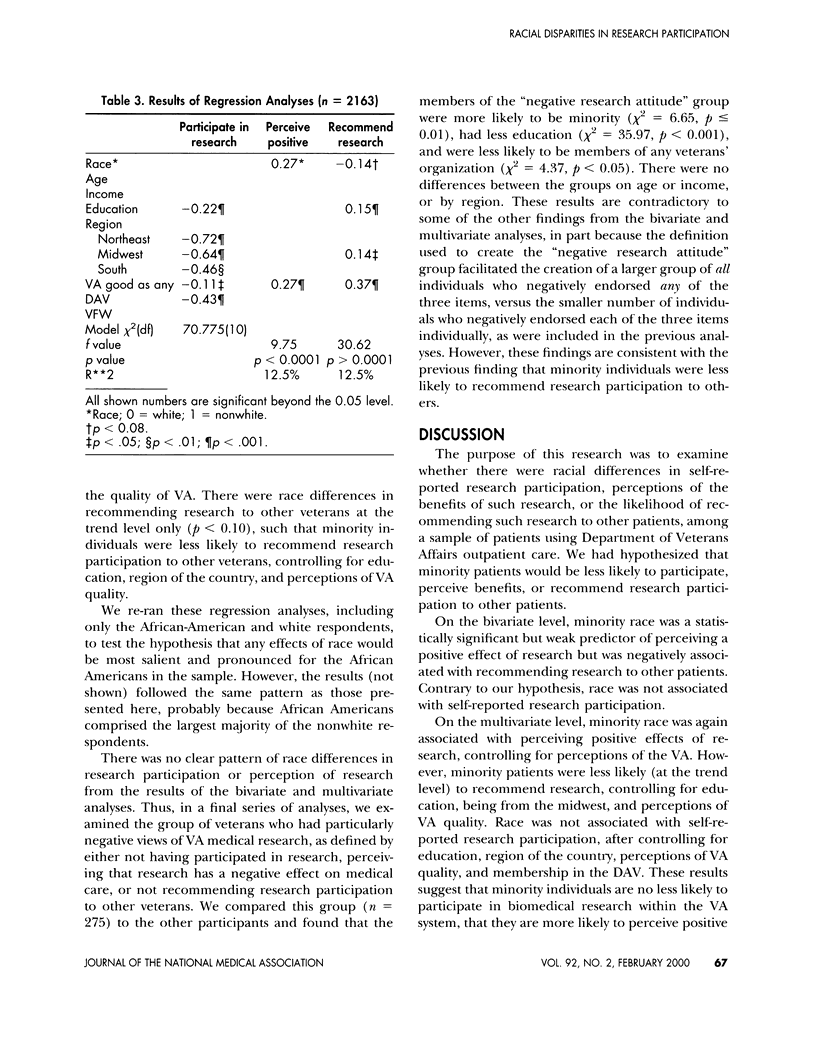
To determine whether minority patients were less likely to participate in biomedical research, perceive positive benefits from such participation, or to recommend research participation to other patients, an observational study was conducted. Sociodemographic and survey data were collected from 5436 users of Department of Veterans Affairs (VA) Ambulatory Care, which included questions about veterans' research participation and related attitudes. Bivariate and multivariate analyses were performed to determine if there were racial differences in the outcomes of interest, controlling for relevant sociodemographic factors. Bivariate and multivariate analyses indicated that there were no racial differences in self-reported research participation, but minority veterans were more likely to perceive a positive effect of research and less likely to recommend research to other veterans. However, subgroup analyses indicated that, of those veterans having negative attitudes about research, minority and less educated veterans were disproportionately represented. In the VA system, racial differences in research participation may dissipate because many sociodemographic factors are controlled. Although we did not observe consistent racial differences in research participation or attitudes, the fact that minority veterans were disproportionately represented among the group with the most negative attitudes about research suggests that further research is necessary to fully understand the racial dynamics of research participation in the VA.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ballard E. L., Nash F., Raiford K., Harrell L. E. Recruitment of black elderly for clinical research studies of dementia: the CERAD experience. Gerontologist. 1993 Aug;33(4):561–565. doi: 10.1093/geront/33.4.561. [DOI] [PubMed] [Google Scholar]
- Blendon R. J., Aiken L. H., Freeman H. E., Corey C. R. Access to medical care for black and white Americans. A matter of continuing concern. JAMA. 1989 Jan 13;261(2):278–281. [PubMed] [Google Scholar]
- Escarce J. J., Epstein K. R., Colby D. C., Schwartz J. S. Racial differences in the elderly's use of medical procedures and diagnostic tests. Am J Public Health. 1993 Jul;83(7):948–954. doi: 10.2105/ajph.83.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gornick M. E., Eggers P. W., Reilly T. W., Mentnech R. M., Fitterman L. K., Kucken L. E., Vladeck B. C. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. 1996 Sep 12;335(11):791–799. doi: 10.1056/NEJM199609123351106. [DOI] [PubMed] [Google Scholar]
- Kazis L. E., Miller D. R., Clark J., Skinner K., Lee A., Rogers W., Spiro A., 3rd, Payne S., Fincke G., Selim A. Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med. 1998 Mar 23;158(6):626–632. doi: 10.1001/archinte.158.6.626. [DOI] [PubMed] [Google Scholar]
- Kindig D. A., Yan G. Physician supply in rural areas with large minority populations. Health Aff (Millwood) 1993 Summer;12(2):177–184. doi: 10.1377/hlthaff.12.2.177. [DOI] [PubMed] [Google Scholar]
- Krieger N., Rowley D. L., Herman A. A., Avery B., Phillips M. T. Racism, sexism, and social class: implications for studies of health, disease, and well-being. Am J Prev Med. 1993 Nov-Dec;9(6 Suppl):82–122. [PubMed] [Google Scholar]
- McBean A. M., Gornick M. Differences by race in the rates of procedures performed in hospitals for Medicare beneficiaries. Health Care Financ Rev. 1994 Summer;15(4):77–90. [PMC free article] [PubMed] [Google Scholar]
- Rosenheck R., Fontana A., Cottrol C. Effect of clinician-veteran racial pairing in the treatment of posttraumatic stress disorder. Am J Psychiatry. 1995 Apr;152(4):555–563. doi: 10.1176/ajp.152.4.555. [DOI] [PubMed] [Google Scholar]
- Simberkoff M. S., Hartigan P. M., Hamilton J. D., Day P. L., Diamond G. R., Dickinson G. M., Drusano G. L., Egorin M. J., George W. L., Gordin F. M. Long-term follow-up of symptomatic HIV-infected patients originally randomized to early versus later zidovudine treatment; report of a Veterans Affairs Cooperative Study. VA Cooperative Study Group on AIDS Treatment. J Acquir Immune Defic Syndr Hum Retrovirol. 1996 Feb 1;11(2):142–150. doi: 10.1097/00042560-199602010-00005. [DOI] [PubMed] [Google Scholar]
- Thomas S. B., Quinn S. C. The Tuskegee Syphilis Study, 1932 to 1972: implications for HIV education and AIDS risk education programs in the black community. Am J Public Health. 1991 Nov;81(11):1498–1505. doi: 10.2105/ajph.81.11.1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson N. J., Kizer K. W. The VA health care system: an unrecognized national safety net. Health Aff (Millwood) 1997 Jul-Aug;16(4):200–204. doi: 10.1377/hlthaff.16.4.200. [DOI] [PubMed] [Google Scholar]
- Wolinsky F. D., Coe R. M., Mosely R. R., 2nd, Homan S. M. Veterans' and nonveterans' use of health services. A comparative analysis. Med Care. 1985 Dec;23(12):1358–1371. doi: 10.1097/00005650-198512000-00005. [DOI] [PubMed] [Google Scholar]
- el-Sadr W., Capps L. The challenge of minority recruitment in clinical trials for AIDS. JAMA. 1992 Feb 19;267(7):954–957. [PubMed] [Google Scholar]


