Abstract
Objective
To investigate the effectiveness of radiographic parameters on segmental instability in the lumbar spine using Kinetic magnetic resonance imaging (MRI).
Methods
Segmental motion, defined as excessive (more than 3 mm) translational motion from flexion to extension, was investigated in 309 subjects (927 segments) using Kinetic MRI. Radiographic parameters which can help indicate segmental instability include disc degeneration (DD), facet joint osteoarthritis (FJO), and ligament flavum hypertrophy (LFH). These three radiographic parameters were simultaneously evaluated, and the combinations corresponding to significant segmental instability at each level were determined.
Results
The overall incidence of segmental instability was 10.5% at L3-L4, 16.5% at L4-L5, and 7.3% at L5-S1. DD and LFH at L3-L4 and FJO and LFH at L4-L5 were individually associated with segmental instability (p<0.05). At L4-L5, the following combinations had a higher incidence of segmental instability (p<0.05) when compared to other segments : (1) Grade IV DD with grade 3 FJO, (2) Grade 2 or 3 FJO with the presence of LFH, and (3) Grade IV DD with the presence of LFH. At L5-S1, the group with Grade III disc and Grade 3 FJO had a higher incidence of segmental instability than the group with Grade I or II DD and Grade 1 FJO.
Conclusion
This study showed that the presences of either Grade IV DD or grade 3 FJO with LFH at L4-L5 were good indicators for segmental instability. Therefore, using these parameters simultaneously in patients with segmental instability would be useful for determining candidacy for surgical treatment.
Keywords: Segmental instability, Disc degeneration, Facet joint osteoarthritis, Hypertrophy of ligament flavum, MRI
INTRODUCTION
Lumbar segmental instability is thought to be a possible causative mechanism of underlying low back pain and sciatica6,15-18,20-22,25,28). It is often an important factor in determining surgical indications for spinal fusion in lumbar degenerative disc disease (DDD)8,11,16,17,21,25). Spinal fusion surgeries allow symptomatic patients with mechanically unstable lumbar segments to significantly improve their quality of life by ameliorating low back pain. The decision to perform an arthrodesis, in addition to decompressive surgery, for patients with lumbar DDD depends on the stability of the involved spinal segments25).
The diagnosis of segmental instability is commonly based on the radiographic finding of abnormal segmental motion. Radiographic studies may include plain radiographs, magnetic resonance imaging (MRI), computed tomography, and provocative discography1,3,4,10,16,17,20,22,25,27). Unfortunately, there is poor correlation between the presence of low back pain and imaging study findings in the general population16,17,21). Numerous studies have documented that a high percentage of asymptomatic patients have abnormal findings on imaging studies of the presence of DDD3,4,10,16,17,21,27). Consequently, the decision to undertake surgical management of DDD requires extensive radiographic analysis. The authors of this study wanted to find more reliable indicators for segmental instability using recently introduced imaging technology known as Kinetic MRI®. Kinetic MRI allows us to visualize dynamic segmental motion and to determine abnormal segmental motion10,26). The purpose of the present study is to investigate relationship of individual radiographic parameters and various combinations of radiographic parameters upon lumbar segmental instability using Kinetic MRI.
MATERIALS AND METHODS
Subject population
From July 2005 through August 2007, 309 patients with symptomatic back pain with/without radiculopathy were included in the study. All subjects underwent Kinetic MRI in flexion, neutral, and extension positions. There were 199 males and 110 females. The mean age was 42.1 (range 16-85). Each of the 927 lumbar segments was classified into two groups : a segmental instability group and a segmental non-instability group. The segmental instability group consisted of segments with excessive translational motion (more than 3 mm translation) and the segmental non-instability group consisted of segments without excessive translational motion (less than 3 mm translation).
Kinetic magnetic resonance imaging
MR imaging of the lumbar spine was performed using a 0.6 Tesla MRI scanner (Fonar Corp. Upright, Multi-Position™, New York, NY). The MR unit utilizes a vertical orientation of the two opposing magnet doughnuts, allowing scanning of the patient in an upright axially loaded position (Fig. 1). Images were obtained using a quad channel planar coil. An 18-inch gap between the magnets is present. T1-weighted sagittal spin echo images (repetition time 671 ms, echo time 17 ms, thickness 4.0 mm, field of view 30 cm, matrix 256×224, NEX 2) and T2-wighted fast spin echo images (repetition time 3,000 ms, echo time 140 ms, thickness 4.0 mm, field of view 30 cm, matrix 256×224, NEX 2, flip angle) were obtained.
Fig. 1.
The picture of Kinetic magnetic resonance imaging unit. Kinetic magnetic resonance imaging unit is configured with a top-open design and allows dynamic flexion and extension maneuvers of the spine.
MRI procedure
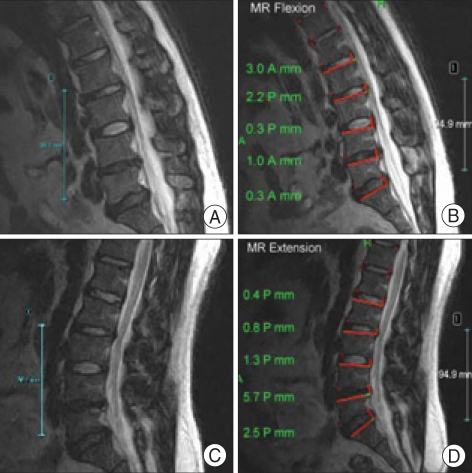
Patients were placed in the upright axially loaded neutral position (T1 and T2 weighted images) and upright axially loaded flexion and extension positions (T2 weighted fast spin echo images only). Segmental translational motion was measured at three levels (L3-L4, L4-L5, L5-S1). All measurements were recorded on a computer and all calculations were completed using MR Analyzer Software (TrueMRI Corporation, Bellflower, CA) (Fig. 2). Total segmental motion was determined to be the difference in displacement between flexion and extension. Segmental instability was defined as excessive segmental motion (more than 3 mm translation).
Fig. 2.
The measurement method of lumbar translational motion using magnetic resonance Analyzer Software. During positional change from flexion (A) to extension (C), all measurements are recorded on a computer software. Dynamic translational motion (4.7 mm) in L4-L5 level is calculated as the difference between flexion (1.0 mm) (B) and extension (5.7 mm) (D).
Radiographic paramater grading
For this study, three radiographic parameters including disc degeneration (DD), facet joint osteoarthritis (FJO), and ligament flavum hypertrophy (LFH) were used. Varying combinations of these parameters were analyzed in an attempt to find more reliable indications for segmental instability. Disc degeneration was classified into one of five grades using Pfirrmann's criteria24). Grade I corresponded to normal discs and Grade V corresponded to advanced degeneration. FJO was classified into 4 grades according to Fujiwara et al.'s method7). Grade 1 corresponded to normal facet joints; grade 2, 3, 4, to mild, moderate, severe facet joints degeneration, respectively. LFH was classified as being either negative or positive. Negative classification corresponded to having no ligamentum flavum hypertrophy, and positive classification indicated the presence of LFH. When the facet joint interspaces were not clearly visible upon the axial Kinetic MRI the images were regarded as having low image quality for assessing the facet joint and were excluded.
Data analysis
The incidence of segmental instability according to age and gender was analyzed using the Chi-square test and student t-test, respectively. Relationships between radiographic parameters and segmental instability at L3-L4, L4-L5 and L5-S1 were analyzed using the Chi-square test. The criterion for statistical significance was p<0.05.
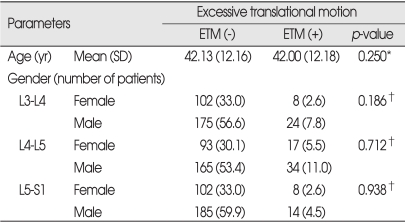
RESULTS
The incidence of segmental instability was 10.5% at L3-L4, 16.5% at L4-L5, and 7.3% at L5-S1. The incidence at L4-L5 was significantly higher than that at L3-L4 (p<0.05) and L5-S1 (p<0.01). Between the group with segmental instability and the segmental non-instability group, age and gender did not differ significantly (Table 1).
Table 1.
Age and gender between two groups according to presence of excessive translational motion
*Student t-test, †χ2test. ETM (+) indicates group 'with excessive translational motion'. ETM(-) indicates group 'without excessive translational motion'. ETM : excessive translational motion. SD : standard deviation
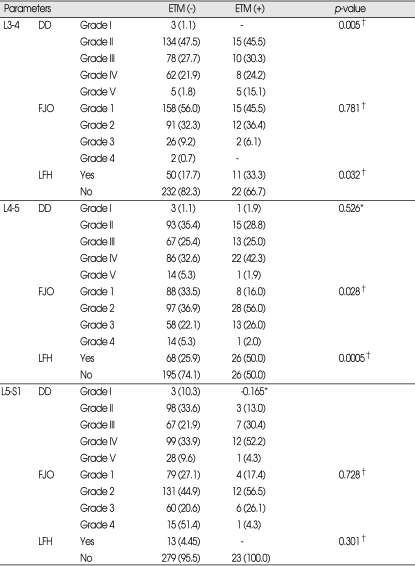
Individual parameters of DD, FJO, and LFH
At L3-L4, DD and LFH individually were significantly correlated with segmental instability (p<0.05) (Table 2). Additionally, at L4-5, FJO and LFH individually were significantly associated with segmental instability (p<0.05). At L5-S1, no individual parameter exhibited a significant effect upon the incidence of segmental instability.
Table 2.
Relationships between radiographic parameters and excessive translational motion
The values are numbers. ETM (+) indicates group 'with excessive trans-lational motion'. ETM (-) indicates group 'without excessive translational motion'. *Fisher' exact test. †χ2 test. DD : disc degeneration, FJO : facet joint osteoarthritis, LFH : ligament flavum hypertrophy
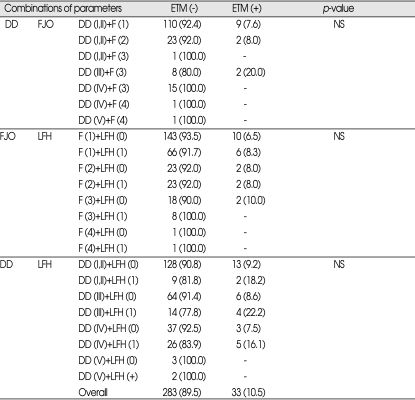
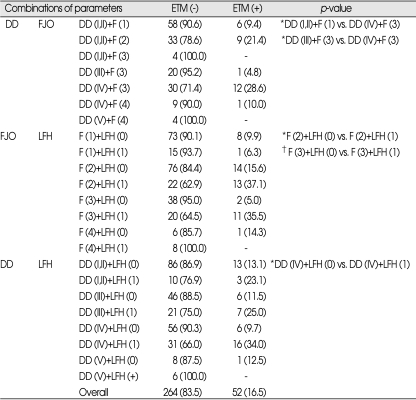
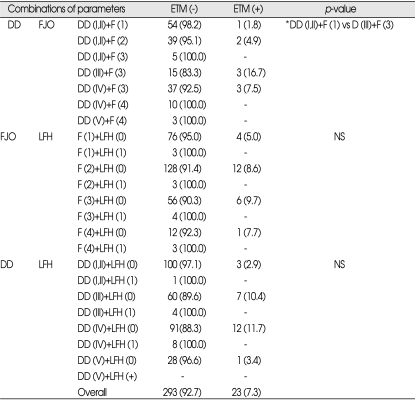
Combination of parameters of DD, FJO, and LFH
At L3-L4, no combinations of radiographic parameters had a significant association with the incidence of segmental instabilty (Table 3). However, three combinations of radiographic parameters at L4-L5 exhibited a strong associations with the incidence of segmental instabilty (Table 4). At L5-S1, the segments with Grade III discs and grade 3 facet joints had a higer incidence of segmental instabilty than those with normal or mild discs and normal facet joints (p<0.05) (Table 5).
Table 3.
Combinations of radiographic parameters at L3-L4
The values are numbers. ( )=percentage. ETM (+) indicates group 'with excessive translational motion'. ETM (-) indicates group 'without excessive translational motion'. DD : disc degeneration, FJO : facet joint osteoarthritis, LFH : ligament flavum hypertrophy, NS : not significant
Table 4.
Combinations of radiographic parameters at L4-L5
The values are numbers. ( )=percentage. ETM (+) indicates group 'with excessive translational motion'. ETM (-) indicates group 'without excessive translational motion'.*p<0.05, †p<0.01. DD : disc degeneration, FJO : facet joint osteoarthritis, LFH : ligament flavum hypertrophy
Table 5.
Combinations of radiographic parameters at L5-S1
The values are numbers. ( )=percentage. ETM (+) indicates group 'with excessive translational motion'. ETM (-) indicates group 'without excessive translational motion'. *p<0.05, DD : disc degeneration, FJO : facet joint osteoarthritis, LFH : ligament flavum hypertrophy, NS : not significant
At L4-L5, the segments with grade 2/3 facet joints and the presence of ligament flavum hypertrophy had a high incidence of segmental instabilty. In addition, the segments with Grade IV discs and grade 3 facet joints had a significantly higher incidence of segmental instabilty than segments with normal discs and facet joints and segments with Grade III discs and grade 3 facet joints (p<0.05). The segments with grade 2 or 3 facet joints with ligament flavum hypertrophy at L4-L5 had a significantly higher incidence of segmental instabilty than those with grade 2 or 3 facet joints without ligament flavum hypertrophy. In addition, the segments with Grade IV discs and ligament flavum hypertrophy had a significantly higher incidence of segmental instabilty than those with Grade IV discs without ligament flavum hypertrophy (p<0.05).
DISCUSSION
The lumbar spinal segment exists as a functional unit in which the intervertebral disc and facet joints function together to provide stability. With intervertebral disc degeneration, facet degeneration leads to abnormal movement i.e. segmental instability2,6,12,17). Progressive degeneration in lumbar spine structures induces loss of water from the nucleus pulposus, which severely impairs its ability to fulfill intended functions. Furthermore, this leads to a loss of disc height and pretension in the ligaments, creating a mechanically unstable environment characterized by abnormal segmental motion patterns28). In this study, intervertebral discs, facet joints, and ligament flavum were chosen as the main parameters for evaluating segmental instability. We thought that analysis of these parameters may have great potential for better identifying segmental instability2,12).
Many studies have described the association between lumbar DDD and segmental instability15-17,21,22,25). Various occupational backgrounds and genetic predispositions have been shown to lead to lumbar DDD. Lumbar DDD is reported to be more common in patients with low back pain than in asymptomatic subjects29). Disc herniation, lack of sports activities, and night work shifts are significant risk factors for the deterioration associated with disc degeneration5). The concept of segmental instability as a cause of back pain has been gradually accepted6,15,17,18,20,21). Disc degeneration can be the initial painful process associated with back pain17). Many discographic studies have reported that a tear of the annulus fibrosus is sometimes painful. The recognition that discs cause low back pain and that degenerative discs lead to abnormal movement suggested the concept that abnormal movement causes pain21).
A lumbar motion segment is considered unstable when it exhibits abnormal movement. The common features associated with biomechanical descriptions of instability include increased mobility, abnormal spinal motion, and/or decreased stiffness of the functional spinal unit27). Movement associated with instability in patients with lumbar DDD is either abnormal in quality (abnormal coupling patterns) or in quantity (abnormal increase of movement)21). Radiolographic findings suggest that in lumbar DDD patients segmental instability includes loss of disc height, traction spurs, facet arthrosis, scoliosis, spondylolysis, and spondylolisthesis16,19). Additionally, in patients with lumbar DDD, hypertrophied arthritis of the facet joints has been shown to result in segmental instability31).
Numerous criteria for defining segmental instability have been developed. The frequently accepted definition of segmental instability was defined by Panjabi and it defines segmental instability as "the loss of the ability of the spine under physiologic loads to maintain its patterns of displacement so there is no initial or additional neurologic deficit, no major deformity, and no incapacitating pain"30). Additionally, recurrent, acute episodes of low back pain produced by mechanical stresses have been considered indicative of instability13). The generally accepted opinion is that surgical intervention is necessary for patients with lumbar DDD exhibiting segmental instability through neurologic deficit related to spinal stenosis, and confirmatory imaging studies showing anterior translation greater than 3 mm and sagittal rotation greater than 10°17). Degenerative lumbar spondylolisthesis has been shown to be an important indication for surgery and can be visualized predominately in the sagittal plane. Radiological findings in the sagittal plane have been considered important factors of instability. Even if segmental range of motion, translational movement, or other angular measurements are useful parameters for the assessment of segmental instability, most studies have reported that unstable segments are typically described as having increased translational movement in the antero-posterior direction27). For this reason, the authors chose translational motion greater than 3 mm in the sagittal plane to represent radiographic segmental instability.
Segmental instability was often difficult to accurately measure using image studies16,17,20,25). In 1944, Knutsson et al.14) examined lateral flexion-extension radiographs of the lumbar spine to test segmental instability. Because of its simplicity, low expense, and pervasive availability, functional flexion-extension radiography is the most thoroughly studied and the most widely used imaging method for diagnosis of lumbar intervertebral instability17). The accuracy of functional flexion-extension radiographic data is questionable due to the lack of routinely applicable reference standards for defining intervertebral instability. Furthermore this technique is characterized by poor measurement reproducibility and a lack of appropriate ways for measuring displacement17). A slight variation in patient positioning or in the direction of the X-ray beam may result in a 10%-15% variation in the range of vertebral displacement17).
Other imaging studies regarding segmental instability have utilized bi-planar radiographs, stereophotogrammetric methods, conventional MRI, cineradiography, video-fluoroscophy, and roentgen stereophotogrammetric technique20,27). Each of these methods has been reported as useful means for evaluating lumbar spinal instability25). In recent years, the development of MRI has stimulated remarkable advances in the diagnosis of lumbar DDD. Conventional MRI scanners have been limited to obtaining images of patients in prone and supine positions20). Additionally, conventional MRI does not have the ability to portray dynamic segmental motion. It also lacks the ability to image patients in weight bearing positions, which are optimum for accurately determining motion3). However, recently Kinetic MRI technology has been introduced which allows patients to be imaged in various weight bearing positions. Kinetic MRI is an outstanding tool for dynamic detection of segmental instability10). It is capable of imaging patients in neutral, flexion, and extension upright, weight bearing positions. Therefore it is a promising medium for investigating conditions considered to lead to spinal instability20). It was used for this study to accurately detect lumbar segmental motion.
In general, radiographic imaging is used to predict segmental instability20). However, there are many questions regarding the ability of radiographic findings to accurately depict segmental instability. Abnormal segmental motion is not always representative of unstable segments9). Sometimes excessive mobility observed upon imaging studies can be transient. Iguchi et al.9) showed that a higher rate of patients with excessive movement in translation and angulation was observed in the younger age groups of teens and patients in their 20s. This study hypothesized that the younger patients who exhibited hypermobile segments without disc degeneration were transient symptomatic patients with normal spinal structures. Sometimes, especially in younger patients, transiently increased segmental motion is not an indication for spinal fusion. In the early stage of disc degeneration and facet joint osteoarthritis the frequency of excessive angular motion increased and this frequency decreased in late stages of disc degeneration and facet joint osteoarthritis. Additionally, in old age, unstable functional units exhibiting radiographic instability tended to become stable13,23).
We believe that the current criteria used for identifying segmental instability using simple flexion and extension radiographic images, while somewhat applicable, need to be improved. The authors believe that if each of the parameters that exhibit significant spinal stability were taken into consideration simultaneously, it could be better approximate clinical segmental instability. Thus, the authors hypothesized that functional units exhibiting radiographic instability in more than two parameters would constitute reliable indications of segmental instability. The authors first investigated the association between three individual parameters (disc degeneration, facet joint osteoarthritis, and ligament flavum hypertrophy) and segmental instability. Next all three parameters were simultaneously taken into consideration to elucidate their effect upon segmental instability.
Our results demonstrate that individually, disc degeneration at L3-L4, facet joint degeneration at L4-L5, and LFH at L3-L4 and L4-L5 were significantly associated with radiographic segmental instability. After combining all three parameters no significant association was discovered at L3-L4 and L5-S1. However, at L4-L5, a significant relationship with segmental instability was discovered when all three parameters were taken into consideration at once. Segments with Grade IV degenerative discs and grade 3 facet joint osteoarthrits had more frequent segmental instability compared to segments with Grade III degenerative discs and grade 3 facet joint osteoarthritis. Additionally, at L4-L5, segments with grade 3 arthritic facet joints and the presence of ligament flavum hypertrophy exhibited segmental instability more frequently than segments with grade 3 arthritic facet joints lacking the presence of ligament flavum hypertrophy. Finally, Grade IV degenerative discs with the presence of ligament flavum hypertrophy also exhibited segmental instability more frequently than segments with Grade IV degenerative discs lacking the presence of ligament flavum hypertrophy. These findings indicate that a delicate combination of three radiographic parameters may constitute an improved criteria for accurately identifying segmental instability on Kinetic MRI. These results support that symptomatic disc degeneration, facet joint osteoarthritis and the presence/absence of ligament flavum hypertrophy can be taken into consideration in order to identify significantly unstable segments requiring surgical intervention
Even though various imaging techniques are widely used to investigate segmental instability, radiographic data alone cannot replace clinical evaluation and criteria when it comes to determining segmental instability. Radiographic criteria for segmental instability does not completely explain the entire concept of segmental instability due to limitations regarding measurements, discrepancies between radiographic and clinical findings, and the short-term existence of an unstable phase in younger patients. Even if a patient exhibits radiographic instability, they do not always demonstrate clinical symptoms of instability3,15,16,27). Radiographic instability is based solely on image findings and does not take into consideration patients symptoms. There is a relatively high incidence of abnormal findings on images belonging to asymptomatic individuals3). Initially obtaining MRI analysis of the spine to determine if anything is wrong can be the beginning of a dangerous thought process. For this reason we cannot definitively conclude that patients with radiographic findings of instability actually have instability.
Even if radiographic findings exhibiting segmental instability are not definitive evidence of clinical instability, according to this study the authors believe that symptomatic high grades of disc degeneration and facet joint osteoarthritis in addition to the presence of ligament flavum hypertrophy when is combined with translational abnormal movement can be good indications for surgical treatment, such as spinal fusion, for patients with lumbar DDD. This is not to say that pre-surgical evaluations are unnecessary. Prior to the decision for surgical treatment, all patients should have a thorough history taken relating to any spinal complaints, a physical examination followed by a working diagnosis and directed imaging studies. Our results simply allow segmental instability to be more accurately identified in symptomatic patients using information regarding disc degeneration, facet joint osteoarthritis, and the presence/absence of ligament hypertrophy.
CONCLUSION
The authors have shown that simultaneously taking into consideration three radiographic parameters constitutes an effective method for identifying segmental instability. Our results show that at L4-L5, segments with Grade IV degenerative discs with grade 3 arthritic facet joints, grade 3 arthritic facet joints with the presence of ligamentum flavum hypertrophy, and Grade IV degenerative discs with the presence of ligamentum flavum hypertrophy all exhibited higher incidences of segmental instability when compared to other groups. Therefore, using these parameters simultaneously in patients with lumbar DDD would be useful for determining candidacy for surgical treatment.
References
- 1.Abbott JH, McCane B, Herbison P, Moginie G, Chapple C, Hogarty T. Lumbar segmental instability : a criterion-related validity study of manual therapy assessment. BMC Musculoskelet Disord. 2005;6:56. doi: 10.1186/1471-2474-6-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berne D, Goubier JN, Lemoine J, Saillant G. The aging of the spine : natural evolution. Eur J Orthop Surg Traumatol. 1999;9:125–133. [Google Scholar]
- 3.Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. J Bone Joint Surg AM. 1990;72:403–408. [PubMed] [Google Scholar]
- 4.Edmondston SJ, Song S, Bricknell RV, Davies PA, Fersum K, Humphries P, et al. MRI evaluation of lumbar spine flexion and extension in asymptomatic individuals. Man Ther. 2000;5:158–164. doi: 10.1054/math.2000.0356. [DOI] [PubMed] [Google Scholar]
- 5.Elfering A, Semmer N, Birkhofer D, Zanetti M, Hodler J, Boos N. Risk factors for lumbar disc degeneration. Spine. 2002;27:125–134. doi: 10.1097/00007632-200201150-00002. [DOI] [PubMed] [Google Scholar]
- 6.Fujiwara A, Tamai K, An HS, Kurihashi T, Lim TH, Yoshida H, et al. The relationship between disc degeneration, facet joint osteoarthritis, and stability of the degenerative lumbar spine. J Spinal Disord. 2000;13:444–450. doi: 10.1097/00002517-200010000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Fujiwara A, Tamai K, Yamato M, An HS, Yoshida H, Saotome K, et al. The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine : an MRI study. Eur Spine J. 1999;8:396–401. doi: 10.1007/s005860050193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haughton VM, Lim TH, An H. Intervertebral disk appearance correlated with stiffness of lumbar spinal motion segments. AJNR Am J Neuroradiol. 1999;2:1161–1165. [PMC free article] [PubMed] [Google Scholar]
- 9.Iguchi T, Kanemura A, Kasahara K, Kurihara A, Doita M, Yoshiya S. Age distribution of three radiologic factors for lumbar instability : probable aging process of the instability with disc degeneration. Spine. 2003;28:2628–2633. doi: 10.1097/01.BRS.0000097162.80495.66. [DOI] [PubMed] [Google Scholar]
- 10.Jinkins JR, Dworkin JS, Green CA, Greenhalgh JF, Gianni M, Gelbien M, et al. Upright, weight-bearing, dynamic-kinetic magnetic resonance imaging of the spine-review of the first clinical results. J HK Coll Radiol. 2003;6:55–74. [Google Scholar]
- 11.Kanayama M, Hashimoto T, Shigenobu K, Oha F, Ishida T, Yamane S. Intraoperative biomechanical assessment of lumbar spinal instability : validation of radiographic parameters indicating anterior column support in lumbar spinal fusion. Spine. 2003;28:2368–2672. doi: 10.1097/01.BRS.0000085357.24025.27. [DOI] [PubMed] [Google Scholar]
- 12.Kim KA, Wang MY. MRI-based morphological predictors of SPECT positive facet arthropathy in patients with axial back pain. Neurosurgery. 2006;58:147–156. doi: 10.1227/01.NEU.0000219956.58725.6F. [DOI] [PubMed] [Google Scholar]
- 13.Kirkaldy-Willis WH, Farfan HF. Instability of the lumbar spine. Clin Orthop Relat Res. 1982;165:110–123. [PubMed] [Google Scholar]
- 14.Knutsson F. The instability associated with disc degeneration in the lumbar spine. Acta Radiol. 1944;25:593–609. [Google Scholar]
- 15.Kotilainen E. Long-term outcome of patients suffering from clinical instability after microsurgical treatment of lumbar disc herniation. Acta Neurochir(Wien) 1998;140:120–125. doi: 10.1007/s007010050072. [DOI] [PubMed] [Google Scholar]
- 16.Kotilainen E, Heinänen J, Gullichsen E, Koivunen T, Aro HT. Spondylodesis in the treatment of segmental instability of the lumbar spine with special reference to clinically verified instability. Acta Neurochir(Wien) 1997;139:629–635. doi: 10.1007/BF01411998. [DOI] [PubMed] [Google Scholar]
- 17.Leone A, Guglielmi G, Cassar-Pullicino VN, Bonomo L. Lumbar intervertebral instability : a review. Radiology. 2007;245:62–77. doi: 10.1148/radiol.2451051359. [DOI] [PubMed] [Google Scholar]
- 18.Louis R. Spinal stability as defined by the three-column spine concept. Anat Clin. 1985;7:33–42. doi: 10.1007/BF01654627. [DOI] [PubMed] [Google Scholar]
- 19.Macnab I. The traction spur. An indicator of segmental instability. J Bone Joint Surg Am. 1971;53:663–670. [PubMed] [Google Scholar]
- 20.McGregor AH, Anderton L, Gedroyc WM, Johnson J, Hughes SP. The use of interventional open MRI to assess the kinematics of the lumbar spine in patients with spondylolisthesis. Spine. 2002;27:1582–1586. doi: 10.1097/00007632-200207150-00019. [DOI] [PubMed] [Google Scholar]
- 21.Mulholland RC. The myth of lumbar instability : the importance of abnormal loading as a cause of low back pain. Eur Spine J. 2008;17:619–625. doi: 10.1007/s00586-008-0612-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murata M, Morio Y, Kuranobu K. Lumbar disc degeneration and segmental instability : a comparison of magnetic resonance images and plain radiographs of patients with low back pain. Arch Orthop Trauma Surg. 1994;113:297–301. doi: 10.1007/BF00426175. [DOI] [PubMed] [Google Scholar]
- 23.Paajanen H, Tertti M. Association of incipient disc degeneration and instability in spondylolisthesis. A magnetic resonance and flexion-extension radiographic study of 20-year-old low back pain patients. Arch Orthop Trauma Surg. 1991;111:16–19. doi: 10.1007/BF00390186. [DOI] [PubMed] [Google Scholar]
- 24.Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 2001;26:1873–1878. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 25.Rihn JA, Lee JY, Khan M, Ulibarri JA, Tannoury C, Donaldson WF, et al. Does lumbar facet fluid detected on magnetic resonance imaging correlate with radiographic instability in patients with degenerative lumbar disease? Spine. 2007;32:1555–1560. doi: 10.1097/BRS.0b013e318067dc55. [DOI] [PubMed] [Google Scholar]
- 26.Siddiqui M, Karadimas E, Nicol M, Smith FW, Wardlaw D. Effects of X-stop device on sagittal lumbar spine kinematics in spinal stenosis. J Spinal Disord Tech. 2006;19:328–333. doi: 10.1097/01.bsd.0000211297.52260.d5. [DOI] [PubMed] [Google Scholar]
- 27.Takayanagi K, Takahashi K, Yamagata M, Moriya H, Kitahara H, Tamaki T. Using cineradiography for continuous dynamic-motion analysis of the lumbar spine. Spine. 2001;26:1858–1865. doi: 10.1097/00007632-200109010-00008. [DOI] [PubMed] [Google Scholar]
- 28.Tsantrizos A, Ito K, Aebi M, Steffen T. Internal strains in healthy and degenerated lumbar intervertebral discs. Spine. 2005;30:2129–2137. doi: 10.1097/01.brs.0000181052.56604.30. [DOI] [PubMed] [Google Scholar]
- 29.Waris E, Eskelin M, Hermunen H, Kiviluoto O, Paajanen H. Disc degeneration in low back pain. A 17-year follow-up study using magnetic resonance imaging. Spine. 2007;32:681–684. doi: 10.1097/01.brs.0000257523.38337.96. [DOI] [PubMed] [Google Scholar]
- 30.White AA, 3rd, Panjabi MM. The basic kinematics of the human spine. Spine. 1978;3:12–20. doi: 10.1097/00007632-197803000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Würgler-hauri CC, Kalbarczyk A, Wiesli M, Landolt H, Fandino J. Dynamic neutralization of the lumbar spine after microsurgical decompression in acquired lumbar spinal stenosis and segmental instability. Spine. 2008;33:E66–E72. doi: 10.1097/BRS.0b013e31816245c0. [DOI] [PubMed] [Google Scholar]