Abstract
A 31-year-old man presented with dull headache and memory disturbance lasting for one week. Computed tomographic scans revealed acute hydrocephalus. The cerebrospinal fluid contained 53 leukocytes/mm3, with a mononuclear preponderance and no erythrocytes. Magnetic resonance imaging revealed hydrocephalus and leptomeningeal enhancement. Magnetic resonance angiography and digital subtraction angiography showed supraclinoid occlusion of the right internal carotid artery, which resembled unilateral moyamoya disease. Neuroendoscopic biopsy of a lesion in the septum pellucidum revealed noncaseating granulomas, which was consistent with sarcoidosis. The patient was successfully managed with intravenous methylprednisolone and ventriculoperitoneal shunting. To our knowledge, this is the first case of moyamoya-like vasculopathy associated with neurosarcoidosis.
Keywords: Moyamoya disease, Neurosarcoidosis, Hydrocephalus
INTRODUCTION
Sarcoidosis is a systemic disease of unknown etiology that can only be diagnosed with certainty by histological analysis10). Approximately 5% of patients with sarcoidosis show neurological involvement8,10). Although pathologic studies have shown clear evidence of granulomatous involvement of cerebral vessels in sarcoidosis, ischemic events related to neurosarcoid vasculitis are limited to a few case reports2,3,7,12). In addition, large cerebral artery involvement in sarcoidosis is extremely rare2,3,7,9,12). To our knowledge, only two cases of moyamoya-like vascular abnormality in pulmonary sarcoidosis have been previously reported9,12). This is the first case of moyamoya-like vasculopathy associated with neurosarcoidosis to be published in the literature.
CASE REPORT
A 31-year-old man was admitted to our hospital due to headache and memory disturbance. On initial examination, he was confused and disoriented in time and space. He had suffered from a dull headache in the bifrontal areas without nausea or vomiting for one week, and he continued to show signs of psychomotor slowing, apathy, and forgetfulness. Neither he nor his family members had a significant medical history. The patient was afebrile, and the results of a physical examination were unremarkable. His short-term memory was impaired, and he had difficulty paying attention. The results of a routine complete blood count, serum biochemistry profiles and autoimmune antibody screening were normal.
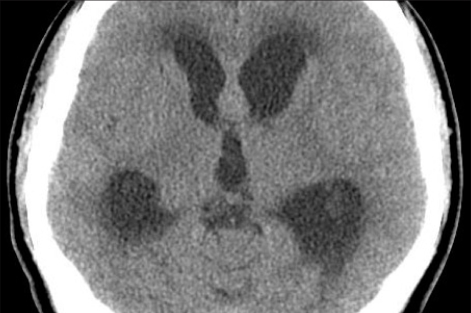
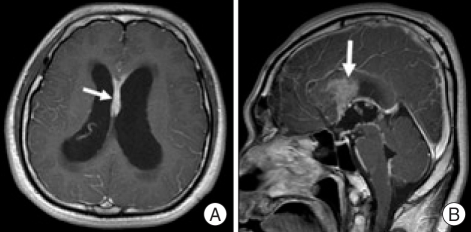
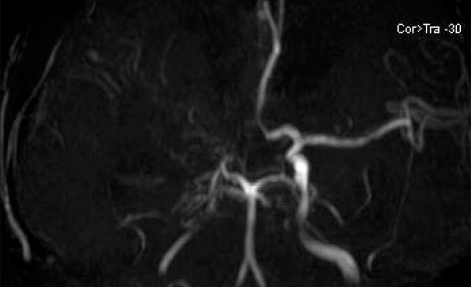
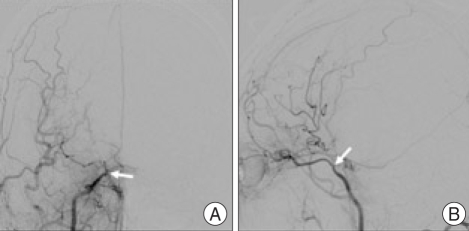
A cranial computed tomography scan showed acute hydrocephalus with periventricular interstitial edema (Fig. 1). The cerebrospinal fluid (CSF) contained 53 leukocytes/mm3, with a mononuclear preponderance and no erythrocytes. However, the level of CSF protein was increased to 2.64 g/L, while that of glucose was normal. Cultures for bacteria, fungi, and Mycobacterium tuberculosis in the CSF were negative, as were the results of polymerase chain reaction for herpes simplex virus. Chest X-ray and CT scan showed bilateral hilar and mediastinal lymphadenopathy. Magnetic resonance imaging of the brain revealed hydrocephalus and an enhancing septumpellucidum, infundibulum, and aqueduct including the leptomeninges, and these findings were consistent with meningoencephalitis (Fig. 2). Magnetic resonance angiography showed supraclinoid occlusion of the right internal carotid artery (ICA) and absence of the right anterior and middle cerebral arteries (Fig. 3). Digital subtraction cerebral angiography demonstrated occlusion of the terminal portion of the right ICA (Fig. 4). There were little definite basal moyamoya vessels. Collateral circulation was provided by the vertebrobasilar system through the posterior communicating artery and by the left ICA through the anterior communicating artery. Brain SPECT imaging revealed normal brain perfusion with normal vascular reserve.
Fig. 1.
Non-enhanced computed tomogra-phy image showing enlarged ventricles with interstitial edema, consistent with acute hydrocephalus.
Fig. 2.
Gadolinium-enhanced axial (A) and sagittal (B) magnetic resonance images show hydrocephalus and thickened enhancing lesions in the septum pellucidum (arrows).
Fig. 3.
Magnetic resonance angiography showing supraclinoid occlusion of the right internal carotid artery as well as the absence of the right anterior and middle cerebral arteries.
Fig. 4.
Anteroposterior (A) and lateral view (B) of right internal carotid artery angiography demonstrates occlusion distal to the ophthalmic artery origin of the right internal carotid artery (arrows).
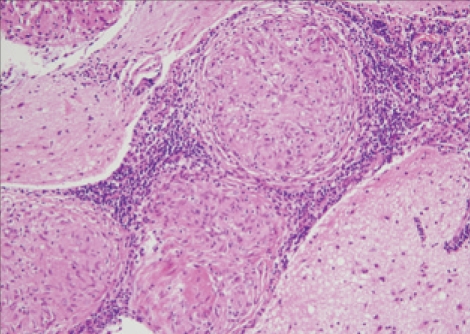
Neuroendoscopic biopsy of the lesion in the septum pellucidum revealed non-caseating granulomas, which was consistent with sarcoidosis (Fig. 5). The patient's neurological status was markedly improved following intravenous methylprednisolone and ventriculoperitoneal shunting.
Fig. 5.
Biopsy specimen shows noncaseating granulomas (H & E, × 400).
DISCUSSION
Sarcoidosis is an idiopathic systemic disease that is histologically characterized by the formation of a noncaseating granuloma10). The disease affects all parts of the body, especially the lungs and lymph nodes10). Central nervous system involvement is common in postmortem series, with approximately one-fourth of patients with systemic disease showing histologic evidence of central nervous system involvement10). Symptomatic central nervous system involvement in living patients is less common, occurring in only about 5% of cases8,10).
The diagnosis of definite neurosarcoidosis is confirmed by biopsy results showing noncaseating granulomas in the absence of organisms or other potential causes. In many cases, biopsy is not possible or desirable due to the site of involvement10).
Neurosarcoidosis most often presents with cranial palsies, predominantly affecting the optic and facial nerves, reflecting its predilection for the base of the brain. Hypothalamic and pituitary involvement is also common, as is the development of lesions in the spinal cord, cerebellum, hemispheres, and peripheral nerves as the disease progress2,3,11).
Hydrocephalus is another uncommon clinical feature and was involved in 6% of patients with neurosarcoidosis in a prospective study6). Both obstructive and communicating hydrocephalus occur with neurosarcoidosis, and the main cause of hydrocephalus is granulomatous meningitis, as seen in present case1,6). Secondary hydrocephalus following meningitis, ventriculitis, or hemorrhage may be complicated by septum formation in the ventricular system1,6). Although loculated hydrocephalus is often treated by placement of an additional shunt, multiple shunt placement is complicated and often results in shunt malfunction6). Recent advances in neuroendoscopic procedures now allow various techniques, such as third ventriculostomy, fenestration of the septum pellucidum or intraventricular septation, aqueductal plasty, and plasty of the foramen of Monro6). Although we identified that the right foramen of Monro was occluded with membranous tissue, the following plasty of the foramen Monro or fenestration of the septum pellucidum was not performed using the endoscope because the purpose of surgery was to establish tissue diagnosis. Although loculated hydrocephalus has been difficult or impossible with normal shunt placement, intravenous methylprednisolone and ventriculoperitoneal shunting markedly improved his neurological status in our case.
Although cerebral vasculitis is a well-known pathologic component of neurosarcoidosis, stroke in patients with neurosarcoidosis appears to be rare and has been limited to a few case reports2-5,7,12). These neuropathologic studies characteristically show granulomatous meningitis predominantly involving the basal meninges, with frequent parenchymal and occasional ependymal involvement. Parenchymal granulomas tend to invade the cerebral substrate along the Virchow-Robin spaces and are distributed perivascularly. In addition, granulomatous invasion of the blood vessel walls is frequent, with vasculitic disruption of the media and internal elastic lamina causing stenosis or occlusion. Several cases have shown that granulomatous vessel stenosis or occlusion is sometimes clearly associated with small cerebral infarcts3). In many instances, small perforating and medium-sized arteries were primarily affected, resulting in small, asymptomatic cerebral infarctions9). In addition, large cerebral artery involvement in sarcoidosis is extremely rare2,3,7,9,12). Unfortunately, the pathologic examination for the cerebral vessel was not possible because of surgical risk for the invasive procedure. Considering the relatively young age and the lack of any vascular risk factors, atherosclerosis is an unlikely cause of ICA occlusion in our patient. Although a simple coexistance of sarcoidosis and unilateral moyamoya disease was not completely ruled out in our patient, our case suggests that sarcoidosis may be related to large vessel involvement in the pattern of moyamoya vasculopathy.
Cerebral angiogram findings in patients with sarcoidosis have been rarely positive, even in those with symptomatic stroke3). To our knowledge, there have only been two reported cases of moyamoya-like vasculopathy associated with sarcoidosis9,12). These two patients were diagnosed with pulmonary sarcoidosis without any clinical or radiological evidence of neurosarcoidosis. Unlike our case, these patients had bilateral ICA occlusion at the terminal portion and imaging evidence of cerebral infarcts. Although large cerebral artery involvement was unilateral in our case, this is the first report of moyamoya-like vasculopathy associated with neurosarcoidosis confirmed by biopsy.
CONCLUSION
A case of moyamoya-like vasculopathy associated with neurosarcoidosis is presented with its clinical features and a review of the literature.
References
- 1.Benzagmout M, Boujraf S, Góngora-Rivera F, Bresson D, Van-Effenterre R. Neurosarcoidosis which manifested as acute hydrocephalus : diagnosis and treatment. Intern Med. 2007;46:1601–1604. doi: 10.2169/internalmedicine.46.0126. [DOI] [PubMed] [Google Scholar]
- 2.Brisman JL, Hinduja A, McKinney JS, Gerhardstein B. Successful emergent angioplasty of neurosarcoid vasculitis presenting with strokes. Surg Neurol. 2006;66:402–404. doi: 10.1016/j.surneu.2006.02.048. [DOI] [PubMed] [Google Scholar]
- 3.Brown MM, Thompson AJ, Wedzicha JA, Swash M. Sarcoidosis presenting with stroke. Stroke. 1989;20:400–405. doi: 10.1161/01.str.20.3.400. [DOI] [PubMed] [Google Scholar]
- 4.Das SK, Sinha I, Kundu TN, Sanyal K, Santosh V, Shankar SK. Two cases of neurosarcoidosis presenting as peripheral neuropathy and stroke in young. J Assoc Physicians India. 1998;46:479–481. [PubMed] [Google Scholar]
- 5.Duffey P, Bates D. Transient focal neurological deficit in sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 1997;14:171–172. [PubMed] [Google Scholar]
- 6.Hamada H, Hayashi N, Kurimoto M, Umemura K, Hirashima Y, Endo S. Isolated third and fourth ventricles associated with neurosarcoidosis successfully treated by neuroendoscopy--case report. Neurol Med Chir (Tokyo) 2004;44:435–443. doi: 10.2176/nmc.44.435. [DOI] [PubMed] [Google Scholar]
- 7.Hodge MH, Williams RL, Fukui MB. Neurosarcoidosis presenting as acute infarction on diffusion-weighted MR imaging : summary of radiologic findings. AJNR Am J Neuroradiol. 2007;28:84–86. [PMC free article] [PubMed] [Google Scholar]
- 8.Johns CJ, Michele TM. The clinical management of sarcoidosis : a 50-year experience at the Johns Hopkins Hospital. Medicine (Baltimore) 1999;78:65–111. doi: 10.1097/00005792-199903000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Kim JS, No YJ. Moyamoya-like vascular abnormality in pulmonary sarcoidosis. Cerebrovasc Dis. 2006;22:71–73. doi: 10.1159/000092924. [DOI] [PubMed] [Google Scholar]
- 10.Smith JK, Matheus MG, Castillo M. Imaging manifestations of neurosarcoidosis. AJR Am J Roentgenol. 2004;182:289–295. doi: 10.2214/ajr.182.2.1820289. [DOI] [PubMed] [Google Scholar]
- 11.Stern BJ, Krumholz A, Johns C, Scott P, Nissim J. Sarcoidosis and its neurological manifestations. Arch Neurol. 1985;42:909–917. doi: 10.1001/archneur.1985.04060080095022. [DOI] [PubMed] [Google Scholar]
- 12.Takenaka K, Ito M, Kumagai M, Yamakawa H, Sugimoto Y, Yamakawa H, et al. Moyamoya disease associated with pulmonary sarcoidosis--case report. Neurol Med Chir (Tokyo) 1998;38:566–568. doi: 10.2176/nmc.38.566. [DOI] [PubMed] [Google Scholar]