Abstract
Background
The aim was to investigate whether multivariate coefficients of serum cholesterol in the prediction of coronary heart disease (CHD) deaths were similar across different cultures in a long term follow-up.
Design
Thirteen cohorts for a total of 10,157 men aged 40–59 years at entry were enrolled in seven countries (USA, Finland, the Netherlands, Italy, Serbia, Greece, Japan), repeatedly examined and followed up for 40 years.
Methods
Serum cholesterol measured at baseline, and then on repeated occasions, was studied, using multivariate models, in relation to the occurrence of CHD deaths during a 40-year follow-up.
Results
Homogeneity of multivariate serum cholesterol coefficients was found considering cholesterol levels at baseline, as average of up to 3 measurements during the first 10 years, as average of up to 6 measurements in 35 years, using the time dependent technique with up to 3 measurements in 10 years, and with up to 6 measurement in 35 years.
Conclusions
The strength of the association between serum cholesterol and CHD death, appears homogeneous across different cultures characterized by different levels of serum cholesterol and different absolute risk of CHD death.
Keywords: coronary heart disease, serum cholesterol, population studies, prediction
INTRODUCTION
During decades of cardiovascular epidemiology, many studies have identified the strong association of serum cholesterol with coronary heart disease (CHD).
An open question is whether the predictive power of this risk factor is similar in different populations characterized by different levels of serum cholesterol and different incidence or death rates from CHD.
A classic review was published in 1990, suggesting that the multivariate coefficients of the major risk factors were relatively similar across different studies [1]. Similar strength of risk factor coefficients across different populations was found by Inter-Heart Study [2]. More recently a metanalysis run by the Prospective Studies Collaboration reported contrasting findings [3].
Within the Seven Countries Study of Cardiovascular Diseases the relationship of baseline serum cholesterol levels with CHD events was characterized by similar coefficients, when comparing different cultures along different lengths of follow-up. [4].
Presently, 40-year mortality data are available for 13 cohorts in seven countries, for men originally aged 40–59 years. The purpose of this analysis is to establish whether the predictive power of serum cholesterol is similar across different cultures characterized by different rates from CHD deaths, in a long follow-up period.
MATERIAL AND METHODS
The Seven Countries Study (SCS) entry surveys were conducted between 1957 and 1964, on 12,763 men aged 40–59 in 16 cohorts of seven countries. Baseline data were collected in the late 1950s and early 1960s, before the era of the Helsinki Declaration. Subsequently, oral informed consent was obtained in collecting follow-up data.
This analysis is restricted to 13 cohorts where the follow-up for mortality and causes of death could be extended for 40 years. Cohorts were located in the USA (1), Finland (2), the Netherlands (1), Italy (2), Serbia (3), Greece (2), Japan (2). Their characteristics were described elsewhere [4].
Overall initial participation rate was greater than 90%, with several cohorts reaching close to 100 % [4].
The following risk factors, measured at entry examination, were considered for this analysis:
- age, in years, rounded-off to the nearest birthday;
- smoking habits expressed as prevalence of current smokers;
- systolic blood pressure, in mmHg, following the technique described by the WHO Cardiovascular Survey Methods Manual [5];
- serum cholesterol, in mmol/l, measured on casual blood samples using the method described by Anderson and Keys [6].
Subsequent re-examination on survivors was conducted in most cohorts after 5, 10, 25, 30, and 35 years. The schedule of examinations varied by cohort. In particular, for all 7 countries, measurements were made at entry, and at 5 and 10 year follow-up. However, in the US Railroad cohort the 10-year examination was not run, and in the two Japanese cohorts the 5-year examination was not performed. For the two Finnish cohorts, the Dutch cohort, and the two Italian cohorts, field examinations were also run at years 25, 30, and 35. For the three Serbian cohorts, repeated measurements were available at years 25 and 35, while for the Crete cohort in Greece, repeated measurements were available at year 30.
Starting at year 25 of follow-up cholesterol measurements were no longer centralized, but all laboratories were under quality control with international agencies.
Mortality data through the 40th anniversary after baseline examination were collected systematically by periodic visits to the areas. Causes of death were adjudicated by a single reviewer (AM) exploiting information from the official death certificate, the medical history collected from interviewing physicians, relatives of the dead persons and other witnesses, and from abstracts of hospital and other medical records. After 10 years of follow-up in the US Railroad cohort, after 15 years in the Finnish cohorts, and 25 years in the Italian, Greek and Japanese cohorts, only death certificates were made available for the majority of cases. Overall, cases with death certificate only were 49%.
Causes of death were coded using the 8th Revision of the WHO-ICD [7]. In case of multiple causes contributing to death, priority was given, in order, to accidents, cancer in advanced stages, coronary heart disease, stroke, and then other conditions. The definition of CHD death was based on operative criteria, i.e. ICD codes 410–414 plus cases of sudden (coronary) death (ICD code 795) validated by the coexistence of a second or third code corresponding to CHD, i.e. 410–414 and considering other medical information when available.
Small losses to follow-up were recorded in the US, Japanese, Dutch and Serbian cohorts, but they were minimal considering the man years of observation.
Statistical Methods
Subjects with an entry diagnosis of CHD were excluded from the analysis. CHD criteria were based on a combination of history and ECG findings following the Seven Countries internal rules [4]. Deaths other than coronary were treated as censored. Cohorts of the same country were pooled.
Five types of analyses were run:
- analysis of 7 countries with entry examination for serum cholesterol;
- analysis of 7 countries with up to 3 averaged measurements of serum cholesterol, in 10 years;
- analysis of 7 countries, with up to 3 time dependent measurements of serum cholesterol in 10 years (updating to the most recent value whenever a new cholesterol value became available);
- analysis of 5 countries (Greece being represented only by Crete), with up to 6 averaged measurements of serum cholesterol in 35 years;
- analysis of 5 countries (Greece being represented only by Crete), with up to 6 time dependent measurements of serum cholesterol.
Each of the above models were computed also for the pool of all countries, with the addition of dummy variables identifying the several countries (Finland as reference).
The Cox proportional hazards model [8] has been employed for the estimate of coefficients for serum cholesterol, with entry levels of age, systolic blood pressure and smoking habits as possible confounders. Plots of Schoenfeld residuals on time were produced to test the proportionality of hazard.
The coefficients of serum cholesterol obtained by models in the single countries were compared to each other using a test of heterogeneity [9], separately for the various models.
Within each country, a test of heterogeneity [9] was made to compare coefficients produced in the several models.
Possible differences in the predictive power of serum cholesterol were also tested producing models that included all the single countries, with the addition of dummy variables for their identification and interaction terms cholesterol-country.
Curves describing the relationship of serum cholesterol levels with CHD deaths were derived for each country for a man aged 50, the specific background cumulative hazard and the specific cholesterol coefficient. The extremes of the curves were truncated at levels roughly corresponding to the country-specific 10th and 90th percentile of the proper cholesterol distribution.
RESULTS
Overall CHD death rates
Large differences in CHD death rates were found across cultures (Table 1), as repeatedly shown in previous analyses for shorter follow-up periods [4]. The highest rates were located in Northern America and Northern Europe, the lowest in Southern Europe and Japan, with the exception of Serbia that can be assigned to Eastern Europe and shows rates comparable to those of Northern Europe. All-cause death rates followed a slightly different pattern. Average base-line serum cholesterol levels were largely different across countries, again as shown repeatedly in the past [4].
Table 1.
Age adjusted death rates in the pooled cohorts within each of the in the seven countries. Data refer to subjects used for the analysis, free from CHD at entry and from missing data.
| Men aged 40–59 years followed up 40 years | |||||
|---|---|---|---|---|---|
| Country | Denominator | CHD fatal events | CHD death rate per 1000 in 40 years and standard error( ) | All-cause death rate per 1000 in 40 years and standard error ( ) | Average serum cholesterol at entry mmol/L and standard deviation ( ) |
| United States | 2426 | 620 | 259 ( 9) | 836 (7) | 6.19 (1.17) |
| Finland | 1603 | 498 | 310 (12) | 896 (8) | 6.73 (1.34) |
| Netherlands | 851 | 180 | 221 (15) | 879 (11) | 6.08 (1.16) |
| Italy | 1654 | 210 | 125 (8) | 840 (9) | 5.21 (1.06) |
| Serbia | 1541 | 299 | 197 (10) | 887 (8) | 4.66 (1.08) |
| Greece | 1170 | 71 | 44 (6) | 814 (11) | 5.31 (1.12) |
| Japan | 912 | 34 | 37 (6) | 821 (13) | 4.26 (0.89) |
Predictive Models
In Table 2, multivariate coefficients of serum cholesterol are reported for each country (and for their pool) and for the five combinations of serum cholesterol measurements, as derived from the corresponding models predicting CHD deaths in 40 years. All coefficients were statistically significant except those of Japan. In general, the magnitude of coefficients was larger for the average of 2–3 cholesterol measurements compared to a single measurement, and even more for the average of 4 to 6 measurements. Models following the time dependent technique did not provide larger coefficients for cholesterol compared to those using the average serum cholesterol levels in multiple measurements. Within each model, tests of heterogeneity across countries were never statistically significant suggesting a relative homogeneity of coefficients.
Table 2.
Multivariate coefficients of serum cholesterol in different countries in the prediction of CHD deaths among middle aged men with a follow-up of 40 years. Models consider one or more measurements of serum cholesterol. Estimates are adjusted for age, systolic blood pressure and smoking habits.
Hazard ratio for 1 mmol/L difference.
| Coefficient | s.e. | T | Hazard ratio | 95% c.l. | ||
|---|---|---|---|---|---|---|
| Baseline cholesterol | ||||||
| United States | 0.1983 | 0.0325 | 6.10 | 1.22 | 1.14 | 1.30 |
| Finland | 0.1567 | 0.0336 | 4.66 | 1.17 | 1.09 | 1.25 |
| Netherlands | 0.1909 | 0.0612 | 3.12 | 1.21 | 1.07 | 1.36 |
| Italy | 0.2679 | 0.0619 | 4.33 | 1.31 | 1.16 | 1.48 |
| Serbia | 0.2248 | 0.0497 | 4.52 | 1.25 | 1.14 | 1.38 |
| Greece | 0.3132 | 0.0958 | 3.27 | 1.37 | 1.13 | 1.65 |
| Japan | −0.1510 | 0.1994 | −0.76 | 0.86 | 0.58 | 1.27 |
| All countries | 0.1983 | 0.0185 | 10.72 | 1.33 | 1.18 | 1.26 |
| Test of heterogeneity across countries: p 0.2691 (coefficient for all countries not considered) | ||||||
| Average of up to 3 Cholesterol measurements | ||||||
| United States | 0.2380 | 0.0365 | 6.51 | 1.27 | 1.18 | 1.36 |
| Finland | 0.2012 | 0.0379 | 5.31 | 1.22 | 1.14 | 1.32 |
| Netherlands | 0.1728 | 0.0705 | 2.45 | 1.19 | 1.04 | 1.36 |
| Italy | 0.3190 | 0.0681 | 4.69 | 1.38 | 1.20 | 1.57 |
| Serbia | 0.2661 | 0.0501 | 5.31 | 1.30 | 1.18 | 1.44 |
| Greece | 0.3278 | 0.0962 | 3.40 | 1.39 | 1.15 | 1.68 |
| Japan | 0.1044 | 0.2344 | 0.46 | 1.11 | 0.70 | 1.76 |
| All countries | 0.2414 | 0.0204 | 11.86 | 1.27 | 1.22 | 1.32 |
| Test of heterogeneity across countries: p 0.5802 (coefficient for all countries not considered) | ||||||
| Average of up to 6 cholesterol measurements | ||||||
| United States | n.a. | n.a. | n.a. | n.a. | n.a. | |
| Finland | 0.3829 | 0.0405 | 9.45 | 1.47 | 1.35 | 1.59 |
| Netherlands | 0.2661 | 0.0746 | 3.57 | 1.30 | 1.13 | 1.51 |
| Italy | 0.3231 | 0.0699 | 4.62 | 1.38 | 1.20 | 1.58 |
| Serbia | 0.2959 | 0.0529 | 5.60 | 1.34 | 1.21 | 1.49 |
| Greece (Crete) | 0.3915 | 0.1675 | 2.34 | 1.48 | 1.06 | 2.05 |
| Japan | n.a. | n.a. | n.a. | n.a. | n.a. | |
| All countries | 0.3417 | 0.0268 | 12.75 | 1.41 | 1.34 | 1.48 |
| Test of heterogeneity across countries: p 0.8168 (coefficient for all countries not considered) | ||||||
| Time dependent based on up to 3 measurements | ||||||
| United States | 0.2090 | 0.0345 | 6.06 | 1.23 | 1.15 | 1.32 |
| Finland | 0.1503 | 0.0331 | 4.54 | 1.16 | 1.09 | 1.24 |
| Netherlands | 0.1385 | 0.0654 | 2.12 | 1.15 | 1.01 | 1.31 |
| Italy | 0.2510 | 0.0555 | 4.52 | 1.29 | 1.15 | 1.43 |
| Serbia | 0.2438 | 0.0425 | 5.74 | 1.28 | 1,17 | 1.39 |
| Greece | 0.2498 | 0.0848 | 2.95 | 1.28 | 1.52 | 2.95 |
| Japan | −0.1534 | 0.1949 | −0.79 | 0.86 | 0.59 | 1.26 |
| All countries | 0.1976 | 0.0181 | 10.92 | 1.22 | 1.18 | 1.26 |
| Test of heterogeneity across countries: p 0.1922 (coefficient for all countries not considered) | ||||||
| Time dependent based on up to 6 measurements | ||||||
| United States | n.a. | n.a. | n.a. | n.a. | ||
| Finland | 0.3921 | 0.0310 | 12.66 | 1.48 | 1.39 | 1.57 |
| Netherlands | 0.2974 | 0.0581 | 5.12 | 1.35 | 1.20 | 1.51 |
| Italy | 0.2937 | 0.0558 | 5.26 | 1.34 | 1.20 | 1.50 |
| Serbia | 0.2995 | 0.0460 | 6.51 | 1.35 | 1.23 | 1.48 |
| Greece (Crete) | 0.2900 | 0.1430 | 2.03 | 1.34 | 1.01 | 1.77 |
| Japan | n.a. | n.a. | n.a. | n.a. | ||
| All countries | 0.3448 | 0.0211 | 16.36 | 1.41 | 1.35 | 1.47 |
| Test of heterogeneity across countries: p 0.2932 (coefficient for all countries not considered) | ||||||
Test of heterogeneity for different models within each country: all non significant except for Finland (p<0.001)
None of tests of heterogeneity comparing coefficients of different models within each country was significant, except for Finland.
A test of heterogeneity comparing models computed on the pool of countries proved to be statistically significant (p <0.001), suggesting that the different combinations of cholesterol measurements produced different coefficient, usually larger for the average of up to 6 measurements and for the time dependent approach, again with up to 6 measurements.
Plots of the Schoenfeld residual on time did no show significant trends except for slight negative trends in Greece and Japan.
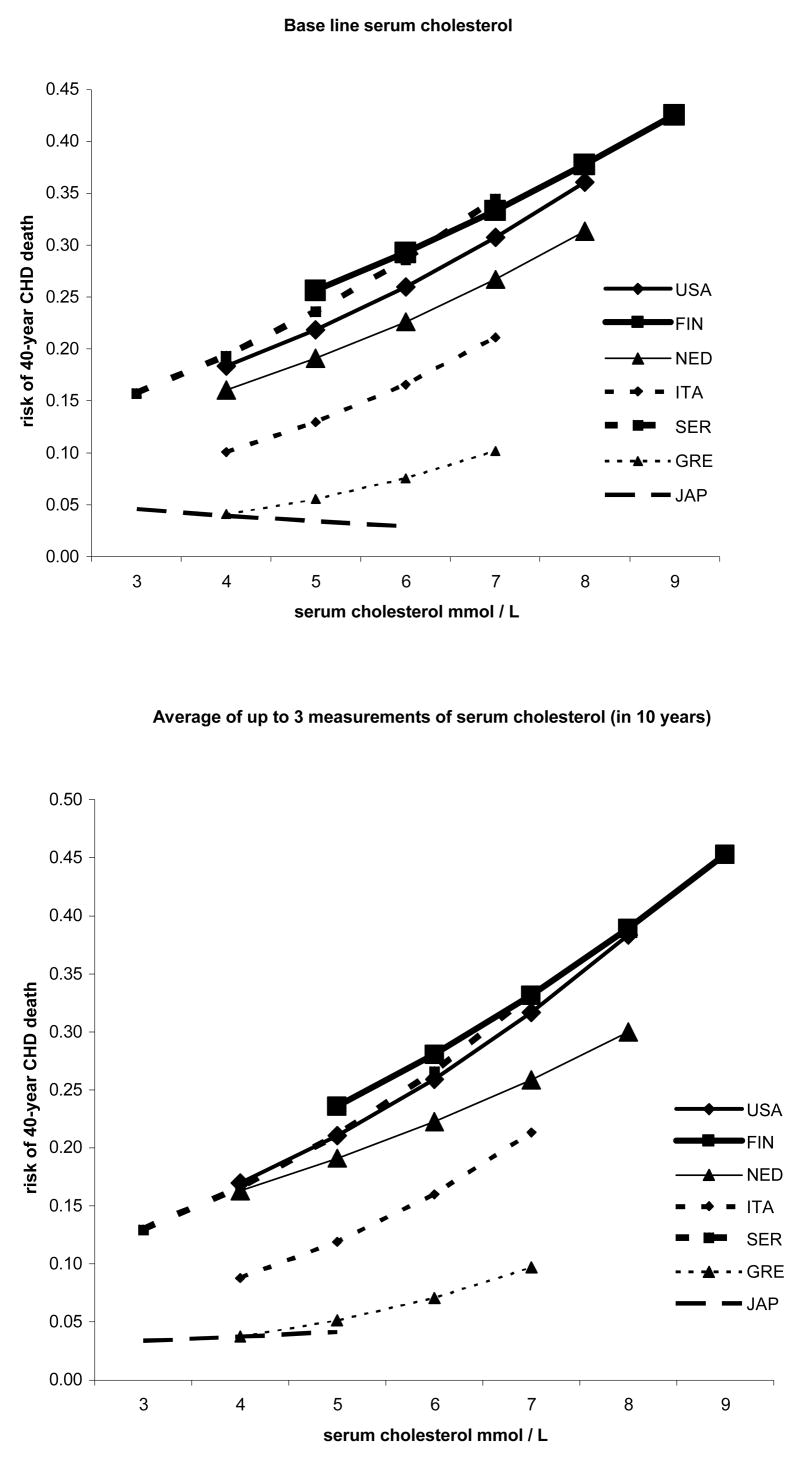
Figure 1 provides examples of the relationship of serum cholesterol with CHD mortality in 40 years, when cholesterol measurement was taken at entry only, and up to 3 times. In general curves were almost parallel across different countries.
Figure 1.
Relationship of serum cholesterol at entry examination and as average of up to 3 measurements in 10 years, with CHD death risk among middle aged men in 7 countries during 40 years of follow-up.
USA: United States of America; FIN: Finland; NED: the Netherlands; ITA: Italy; SER: Serbia; GRE: Greece; JAP: Japan
Five multivariate models were solved for the pool of all countries, that included interaction terms between serum cholesterol and countries. The interaction terms cholesterol-country produced non significant coefficients in all models except one (Serbia, time dependent model with up to 6 measurements).
DISCUSSION
All findings described above point to the same conclusion, that is, a substantial homogeneity of multivariate cholesterol coefficients across different cultures, or at least an absence of statistically significant heterogeneity. In other words it seems that a general biological rule regulates the association of serum cholesterol levels with the occurrence of fatal CHD events. The consequence is that, in all the considered cultures, the same increase in CHD death risk is expected for a given increase in serum cholesterol level. The partial exception of the Japanese cohorts might be interpreted in relation with the small numbers involved in the denominator and in the event rates. In fact, the relationship of serum cholesterol to CHD mortality was found positive and strong in the Eastern Asian populations examined in a recent meta-analysis that included also a Japanese component [3].
In general, a single measurement of serum cholesterol made at entry examination is less predictive than other combinations, such as the average of up to 3, or up to 6 measurements, or the use of the time dependent approach where the latest available measurement is considered. The simple approach using the average of multiple measurements takes into account the effect of changes in cholesterol levels during the long follow-up period, beyond the measurement errors and the effect of regression towards the mean.
However, there is little difference between models using baseline cholesterol only and time dependent models using up to three measurements since in the latter models most of the follow-up and a large majority of the events took place when the single 3rd cholesterol measurement is used alone. The benefit from using the average of cholesterol measurements is obvious since it reflect somehow the time of exposure. The similarity of the six measurement’s average model and the time dependent models suggests that it is the long-term (tens of years) cholesterol rather than the immediate (less than 5 years) cholesterol value that matters. An alternative explanation is that they are the same persons who had a high cholesterol and the same persons who had low cholesterol throughout the follow-up period, in which case the two models becomes similar.
The average cholesterol levels have been changing during the follow-up with different directions and magnitudes across the various countries, as documented elsewhere [4].
In general is seems that more measurements of the same countries do change the coefficients and that the change is consistent among the countries. although these improvements are not statistically significant (except in the pooled analysis).
The curves describing the relation of serum cholesterol with the risk of CHD death clearly show that, although being almost parallel, more or less large gaps do exist among them. This means that the absolute risk of fatal CHD can be largely different among countries although the relative risk for the same difference in serum cholesterol is the same. In fact, CHD death rates for Italy, Greece and Japan were definitely lower than those of the other countries, ecologically explained by large differences in dietary habits [4].
Limitation of this analysis are the use of slightly heterogeneous methodologies, such as the biochemical methods of cholesterol measurements at different times, the discrepancies in the number of available measurements across countries, and the fact that only half of the causes of deaths were validated by sources of information other than the death certificate.
Another problem is the treatment of those who died early using more than one cholesterol measurement. The fact is that the average cholesterol was intended as the best estimate of the time exposure. Those who died early had, consequently, fewer measurements to contribute to the average.
Again, caution should be expressed in comparing coefficients belonging to the same country and derived from different combinations of cholesterol measurements since they could be highly correlated one each other. On the other hand, we can relay only of the magnitude of the coefficients that represents they predictive power.
Moreover the validity of the proportional hazards assumption was confirmed although not in all models. This is also in line with previous Seven Countries analyses where, in a follow-up of 35 years, the partitioned approach showed that baseline cholesterol measurement kept a strong predictive power in successive quinquennia for at least the first 30 years [10]. This confirms that the concept of cholesterol/life years, corresponding to the time lag theory proposed for the French paradox [11], is an explanation for the long term predictive power of older measurements.
The suggestion that multivariate coefficients of risk factors and serum cholesterol in particular are similar in different cultures was given by a review of several studies made in 1990 [1]. However, caution was expressed since different studies may use different methodologies, thus impairing the value of the comparison.
More recently the Inter –Heart, an international metacentre study on risk factors and myocardial infarction, showed that across different groups of countries the predictive power of several risk factors were similar [2]. This was a case-control with possible inherent bias, and the comparison across countries was made for the ratio of apoB/apoA1 ratio which is only a proxi of cholesterol. Moreover a specific test on possible heterogeneity of coefficient was not provided.
Two other international studies showed similar multivariate coefficients for serum cholesterol across different countries or groups of countries [12,13]
A recent meta-analysis of cholesterol and vascular diseases considered the problem of heterogeneity in different countries and studies [3]. Heterogeneity of the association between cholesterol and CHD death was found when considering the 61 studies contributing to the meta-analysis, and this was confirmed even after the exclusion of some outliers based on several criteria. However, heterogeneity was not found when studies were grouped by large geographical entities, such as Europe, USA plus Australia, and East Asia. Probably these conflicting findings are attributable to different methodologies and approaches that could not be taken into proper account in the meta-analytical procedure.
In conclusion long term data from the Seven Countries Study suggest the existence of substantial homogeneity, across different cultures, in the relationship between cholesterol levels and the risk of fatal CHD despite differences in absolute risk. This means that relative risk for a given difference in serum cholesterol level is similar across cultures. Differences in absolute risks for CHD death is bound not only to cholesterol, but also to other risk factors and cultural differences.
Acknowledgments
The Authors acknowledge the late Prof Ancel Keys who was the founder and leader of the Seven Countries Study and to the principal investigators in the various countries.
Medrisk co, Rome, provided partial financial help for this analysis.
Footnotes
Conflicts of interest: NONE
BIBLIOGRAPHY
- 1.Chambless L, Dobson AJ, Patterson CC, Raines B. On the use of a logistic risk score in predicting risk of coronary hart disease. Stat Med. 1990;9:385–396. doi: 10.1002/sim.4780090410. [DOI] [PubMed] [Google Scholar]
- 2.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 3.Prospective Studies Collaboration. Blood cholesterol and vascular mortality by age, sex and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55000 vascular deaths. Lancet. 2007;370:1829–1839. doi: 10.1016/S0140-6736(07)61778-4. [DOI] [PubMed] [Google Scholar]
- 4.Kromhout D, Menotti A, Blackburn H. Diet, lifestyle and risk factors in the Seven Countries Study. Norwell Ma, USA and Dordrecht, NL: 2002. Prevention of coronary heart disease; pp. 1–267. [Google Scholar]
- 5.Rose G, Blackburn H. Cardiovascular survey methods. Geneva: World Health Organization; 1968. [PubMed] [Google Scholar]
- 6.Anderson JT, Keys A. Cholesterol in serum and lipoprotein fractions: its measurement and stability. Clin Chem. 1956;2:145–159. [PubMed] [Google Scholar]
- 7.International Classification of Diseases and Causes of Death, 8th Revision. Geneva: World Health Organization; 1965. [Google Scholar]
- 8.Cox DR. Regression models and life tables. J Roy Stat Soc. 1972;B43:185–220. [Google Scholar]
- 9.Dyer AR. A method for combining results from several epidemiological studies. Stat Med. 1986;5:303–317. doi: 10.1002/sim.4780050403. [DOI] [PubMed] [Google Scholar]
- 10.Menotti A, Lanti M, Kromhout D, Kafatos A, Nedeljkovic S, Nissinen A. Short and long term association of a single serum cholesterol measurement in middle-aged men in prediction of fatal coronary and other cardiovascular events: a cross-cultural comparison through Europe. Eur J Epidemiol. 2005;20:597–604. doi: 10.1007/s10654-005-7918-8. [DOI] [PubMed] [Google Scholar]
- 11.Law M, Wald N. Why heart disease mortality is low in France: the time lag explanation. BMJ. 1999;318:1471–1480. doi: 10.1136/bmj.318.7196.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.ERICA Research Group. Prediction of coronary heart disease in Europe. The 2nd report of the WHO-ERICA Project. Eur Heart J. 1991;12:291–297. [PubMed] [Google Scholar]
- 13.Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular diseases in Europe: the SCORE project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]