Abstract
Objectives. We developed a method to evaluate geographic and temporal variations in community-level obesity prevalence and used that method to identify communities in Massachusetts that should be considered high priority communities for obesity control.
Methods. We developed small-area estimation models to estimate community-level obesity prevalence among community-living adults 18 years or older. Individual-level data from the Behavioral Risk Factors Surveillance System from 1999 to 2005 were integrated with community-level data from the 2000 US Census. Small-area estimation models assessed the associations of obesity (body mass index ≥ 30 kg/m2) with individual- and community-level characteristics. A classification system based on level and precision of obesity prevalence estimates was then used to identify high-priority communities.
Results. Estimates of the prevalence of community-level obesity ranged from 9% to 38% in 2005 and increased in all communities from 1999 to 2005. Fewer than 7% of communities met the Healthy People 2010 objective of prevalence rates below 15%. The highest prevalence rates occurred in communities characterized by lower income, less education, and more blue-collar workers.
Conclusions. Similar to the rest of the nation, Massachusetts faces a great challenge in reaching the national obesity control objective. Targeting high-priority communities identified by small-area estimation may maximize use of limited resources.
Obesity, a major health concern in the United States,1 results in an estimated 240 000 premature deaths2–4 and medical costs of over $90 billion5,6 annually. An objective of Healthy People 2010 is to reduce the prevalence of adult obesity (body mass index [BMI] ≥ 30 kg/m2) to less than 15% nationwide.7 Numerous studies8–10 confirm that rates of obesity are rapidly rising in almost all sociodemographic groups. Recent national data11,12 suggest that obesity has reached an historical high, affecting 32% of the adult population.11
Obesity control is a complex process that requires approaches at all levels—federal, state, and community, as well as organizational, interpersonal, and individual.13,14 Control programs that address the specific needs of communities are likely to be more effective than are nonspecific programs planned at higher geopolitical levels such as county or state.15,16 Similar to the rest of the nation, Massachusetts encounters shortages of resources for obesity control. For effective use of limited resources, estimates of community-specific prevalence are needed to identify communities with the greatest needs. In addition, city and town public officials and community-based organizations increasingly ask the Massachusetts Department of Public Health for obesity prevalence data that are timely and community specific.
In Massachusetts, the Behavioral Risk Factor Surveillance System (BRFSS)17 is the only source of population-based data on the prevalence of obesity among residents 18 years or older. However, the current BRFSS does not provide prevalence data at the community level because most communities do not have adequate sample sizes for directly calculating prevalence with reasonable precision. Small-area estimation models can be adapted to overcome this limitation and provide community-level prevalence estimates.
Using the BRFSS data and small-area estimation models, we estimated and analyzed geographic variations and temporal trends in obesity prevalence in 398 communities (including 339 towns and small cities and 59 subdivisions of the 12 largest cities) in Massachusetts. To assist in the planning of statewide obesity control efforts, we developed a method for classifying communities into priority groups based on adult obesity prevalence estimates and the precision of these estimates.
METHODS
Small-area estimation models generate community-specific prevalence estimates by making use of (1) the associations of obesity with individual- and community-level characteristics, (2) data from multiple years and across geographic regions, and (3) community demographic characteristics. Our models used the following data for the years 1999 to 2005: (1) individual-level data on body weight, body height, and sociodemographic characteristics for adults residing in the communities under study, (2) community characteristics associated with obesity at least in part independently of individual-level characteristics (such as community-level per capita income), and (3) community composition by age, gender, race/ethnicity, marital status, education, and income. Community-level variables were categorized in the same way as their individual-level counterparts.
Individual-Level Data
Individual-level data were obtained from the Massachusetts BRFSS collected from 1999 through 2005. The BRFSS collects uniform data on preventive health practices and risk behaviors associated with chronic diseases, injuries, and infectious diseases in the adult population. Data are collected annually from a sample of community-dwelling adults 18 years or older through a random-digit-dialing telephone survey. For the period of this study (1999–2005), response rates calculated by the CASRO method18 ranged from 33% (in 2000) to 44% (in 2002). Factors relevant to this study included self-reported body weight and height and sociodemographic characteristics (such as age, gender, race/ethnicity, education, marital status, unemployment, and household income). Since 1999, respondents' residences have been recorded at both the town or city level and the 5-digit zip code level.
Definition of Obesity
In each survey year, interviewees reported their body weight (in pounds) and height (in feet and inches). Because self-reported weight and height are subject to social desirability biases that vary across gender, socioeconomic status, and racial/ethnic group,19–24 we developed a correction method to minimize self-report biases based on data from the Third National Health and Nutrition Examination Survey (NHANES III).25 This method included a set of gender- and race/ethnicity-specific linear regression models to correct for self-reported body weight and height (see appendix 1, available as a supplement to the online version of this article at http://www.ajph.org). The models accounted for respondents' age, marital status, education, and income. BMI values were calculated as corrected weight in kilograms divided by corrected height in meters squared.
Respondents were classified on the basis of their BMI values as either obese (corrected BMI ≥ 30 kg/m2; n = 11 651 [22.1%]) or not obese (corrected BMI < 30 kg/m2; n = 41 034 [77.9%]). The 3630 respondents (6.4%) whose BMI values could not be determined, and 14 respondents who had biologically implausible BMI values ( < 12 kg/m2 or > 70 kg/m2), were excluded.
Definition of Communities and Geographic Unit of Analysis
A person's community was defined as the town, city, or subdivision of a large city of residence.26 The city of Boston was divided into 17 communities according to neighborhood planning districts defined by the Boston Redevelopment Authority. The city of Worcester was divided into 8 subdivisions, each of which included 3 to 5 adjacent census tracts with comparable sociodemographic profiles. Other larger cities, including Brockton, Cambridge, Fall River, Lawrence, Lowell, Lynn, New Bedford, Newton, Quincy, and Springfield, were divided into subdivisions by similar methods. Two communities, the town of Monroe and Harbor Island in the city of Boston, were excluded because of inadequate sample size.
Community-Level Data
Community-level measures included sociodemographic indicators from the 2000 US Census, such as community compositions by gender, age group, household income, educational attainment, marital status, and employment. The data also included measures of (1) income and wealth (per capita income, percentage of population in poverty, median value of occupied housing units), (2) education (average years of education, percentage of degree holders), (3) occupation (percentage of blue- or white-collar job holders), (4) housing characteristics (vacancy rate, percentage of home ownership, density of housing units), (5) community stability (median tenure of residency, percentage of renters, percentage of single-parent families), and (6) mode (public transit, driving, walking, or cycling) and average time of commute from home to work.
Linking Community- and Individual-Level Data
Community-level 2000 US Census data27 were linked with individual-level BRFSS data through use of unique community identification codes. Relevant individual-level variables in BRFSS databases were classified to be similar to their counterparts in the 2000 Census. Thus, the community-level census data could be incorporated in the small-area estimations to account for the demographic compositions of the communities.
Statistical Modeling
We have previously described the statistical modeling approach.26 We adapted the small-area estimation model of Malec et al.28,29 to estimate community-level prevalence. Our model was a 2-level random-effects logistic regression model. First, it estimated the associations of respondents' obesity status with both individual- and community-level characteristics. Odds ratios for each predictor were calculated from the parameter estimates in the model. Second, community-level logit values were estimated on the basis of these estimated associations and the demographic compositions of the communities. Finally, community-level prevalences were then obtained on the basis of the estimated community-level logit values. (For model specifications, see appendix 2, available as a supplement to the online version of this article at http://www.ajph.org.)
Candidate predictors included individual- and community-level risk factors for obesity documented in the literature.30 Following the parsimonious principle, the final model was identified by a stepwise backward elimination procedure. A predictor was retained in the model if its regression coefficient was statistically significant (P < .10).
The final model included as fixed effects several individual-level characteristics, such as gender, age group, race/ethnicity, marital status, education level, employment status, and annual household income level. Gender and age group accounted for (1) the nonlinear relationship between obesity and age and (2) the strong interaction between gender and age in relation to obesity status. Missing household income levels (15%) were imputed with an ordinal logistic regression model accounting for personal attributes and community-level characteristics of residence. Missing values of other individual-level variables were imputed with either medians or means or the most frequent categories, as appropriate.
The final model also included selected community-level characteristics as fixed effects, such as median per capita income, percentage of blue-collar job holders, median tenure of residency, percentage of single-parent families, percentage of workers walking or biking to work, and percentage of vacant housing units. Most of these variables presented nonlinear associations with individuals' likelihood of being obese and thus were categorized either by quartiles or thresholds if thresholds were present.
Year of interview was included in the model to estimate the community-specific slopes of prevalence change over time. Additional town-level variations that could not be accounted for by the fixed effects and random slopes were modeled as random intercepts.
Using the model we have described and the data on the sociodemographic characteristics of the communities, we estimated the community-level logit values for obesity in a given year by replacing individual-level covariates with their community-level values according to Census 2000.27 We calculated the confidence intervals of the logit estimates using the variances of the random intercepts and random slopes. Community-level prevalence rates and associated confidence intervals were obtained by applying exponential transformation to the estimated logit values and their confidence intervals.
Priority Classification of Communities
To determine which communities should be targeted for obesity surveillance and control efforts, communities were classified into 8 categories on the basis of the level and the precision (defined as half the width of the 95% confidence interval) of the estimated prevalence of obesity. The 4 categories of obesity prevalence estimates were as follows: above 30% (near or above national average of 34%31), 25.1% to 30% (above state average of 24.5%), 15.1% to 25% (below state average but above the national goal in Healthy People 20107), and 15% or below (met the national goal). Precision was divided into 2 groups: acceptable ( ≤ 3%) and unacceptable ( > 3%). In addition, for a few communities (n = 7), data were insufficient for estimation.
All analyses were conducted with Stata MP 10.0 (StataCorp LP, College Station, TX). Prevalence estimates were then mapped with ESRI ArcGIS 9.2 (ESRI, Redlands, CA).
RESULTS
The final analytic sample across all study years included 52 019 respondents (92.3%) from 398 communities. Respondents with missing information on either BMI (6.5%) or town or city of residence (0.1%), along with pregnant women (1.1%), were excluded. Men composed 41% of the sample and women 59%; the mean age was 47 years. Using the direct estimation method of the BRFSS, we estimated the state-level prevalence of obesity in Massachusetts in 2005 as 24.5% (95% confidence interval = 23.1%, 25.8%).
Determinants of Individual-Level Obesity Status
Adjusted odds ratios for obesity for each individual- and community-level factor are presented in Table 1. Individual-level factors associated with higher probability of being obese included male gender, middle age (aged 45-74 years), Black race, Hispanic ethnicity, no college education, unemployment, and annual household income less than $25 000.
TABLE 1.
Multivariable Adjusted Odds Ratios (ORs) of Individual- and Community-Level Factors for Obesity: Massachusetts, 1999–2005
| OR (95% CI) | |
| Individual-level factors | |
| Interview year (1999–2005) | 1.37 (1.30, 1.45) |
| Women, age, y | |
| 18–24 (Ref) | 1.00 |
| 25–34 | 1.49 (1.28, 1.73) |
| 35–44 | 1.93 (1.67, 2.24) |
| 45–54 | 2.57 (2.22, 2.97) |
| 55–64 | 3.01 (2.59, 3.51) |
| 65–74 | 2.63 (2.23, 3.09) |
| ≥ 75 | 1.72 (1.45, 2.05) |
| Men,a age, y | |
| 18–24 | 0.98 (0.83, 1.16) |
| 25–34 | 1.93 (1.67, 2.24) |
| 35–44 | 2.48 (2.14, 2.88) |
| 45–54 | 2.97 (2.55, 3.45) |
| 55–64 | 3.58 (3.06, 4.19) |
| 65–74 | 2.70 (2.27, 3.21) |
| ≥ 75 | 1.56 (1.29, 1.90) |
| Race/ethnicity | |
| Non-Hispanic White (Ref) | 1.00 |
| Non-Hispanic Black | 1.62 (1.47, 1.78) |
| Hispanic | 1.23 (1.14, 1.34) |
| Other | 0.66 (0.57, 0.76) |
| Marital status | |
| Other (Ref) | 1.00 |
| Divorced or widowed | 0.95 (0.90, 1.00) |
| Education | |
| College graduate (Ref) | 1.00 |
| Some college | 1.39 (1.31, 1.48) |
| High school graduate | 1.36 (1.28, 1.44) |
| Less than high school graduate | 1.52 (1.39, 1.66) |
| Employment status | |
| Employed (Ref) | 1.00 |
| Unemployed | 1.11 (1.01, 1.22) |
| Student (enrolled in school) | 0.71 (0.60, 0.84) |
| Not in labor force | 1.15 (1.08, 1.22) |
| Household income, $ | |
| < 15 000 | 1.46 (1.33, 1.61) |
| 15 000–24 999 | 1.26 (1.16, 1.37) |
| 25 000–49 999 | 1.09 (1.02, 1.16) |
| 50 000–74 999 | 1.15 (1.07, 1.24) |
| ≥ 75 000 (Ref) | 1.00 |
| Community-level factors | |
| Average per capita income, $ | |
| < 20 000 | 1.35 (1.13, 1.60) |
| 20 000–24 999 | 1.33 (1.17, 1.51) |
| 25 000–34 999 | 1.20 (1.07, 1.34) |
| ≥ 35 000 (Ref) | 1.00 |
| % of blue-collar workersb | 1.08 (1.03, 1.13) |
| % of workers walking or biking to workc | 0.93 (0.87, 0.99) |
| % of single-parent familiesd | 1.06 (1.03, 1.09) |
| Median tenure of residency, y | |
| < 5 (Ref) | 1.00 (Ref) |
| ≥ 5 | 1.10 (1.00, 1.20) |
| Housing units vacant | |
| < 5% (Ref) | 1.00 |
| ≥ 5% | 0.91 (0.83, 1.00) |
Note. CI = confidence interval. Estimates were made with a mixed-effects logistic model that included all variables, with an estimated coefficient constant of 3.203 (95% CI = 3.442, 2.963) and a standard deviation of random intercept of 0.0898 (95% CI = 0.0610, 0.1321). In the likelihood ratio test for random effects, χ21 = 11.52; P < .001.
Reference category is women aged 18–25 years.
OR for every 10% increase in percentage of blue-collar workers.
OR for every 10% increase in percentage of workers walking or biking to work.
OR for every 10% increase in percentage of single-parent families.
Independent of individual-level variables, community-level predictors of obesity included lower per capita income, higher percentage of blue-collar workers, lower vacancy rate for housing units ( < 5 % ), longer median tenure of residency ( ≥ 5 years ), higher percentage of single-parent families, and lower percentage of workers walking or biking to work.
Community-Level Prevalence Estimation and Precision
We calculated community-level prevalences using the estimated associations in Table 1 and the estimation procedures described in the “Methods” section. In 2005, community-level prevalence estimates ranged from less than 10% to 38%. Nearly all communities ( > 93%) failed to meet the national goal of obesity prevalence below 15%.
Table 2 lists the 20 communities with the highest and lowest estimates of obesity prevalence and their key sociodemographic characteristics. Compared with the communities with the lowest estimated prevalences, communities with the highest estimated prevalences had one third the per capita income, one third the median value of occupied housing units, twice the proportion of blue-collar job holders, 2.5 times the proportion of single-parent families, and one third the proportion of adults 25 years or older with a college degree. All of the 20 communities with the highest estimated prevalences were located in poor urban communities, whereas those with the lowest estimated prevalences included both urban and rural communities but were of higher socioeconomic status or consisted of a predominantly college-educated population.
TABLE 2.
Characteristics of the Massachusetts Communities With the 20 Highest and Lowest Obesity Prevalence Rates: Behavioral Risk Factor Surveillance System, 2005
| Ranka | Community (5-digit zip codes) | Priority Classb | Obesity Prevalence, % | Per Capita Income, $1000 | Median Value of Housing Units, $10 000 | Jobless Rate, % | Blue-Collar Workers, % | College Graduates, % | Families With Single Parent, % | Rural Population, % |
| Communities with the 20 highest obesity prevalence rates | ||||||||||
| 389 | Mattapan, Boston | 1 | 36.8 | 16.5 | 14.4 | 8.9 | 35.4 | 21.6 | 37.4 | 0 |
| 388 | Roxbury, Boston | 1 | 36.0 | 12.9 | 15.5 | 11.3 | 37.8 | 15.7 | 46.2 | 0 |
| 387 | New Bedford (02746) | 1 | 33.1 | 11.0 | 7.0 | 11.9 | 66.6 | 7.9 | 30.7 | 0 |
| 386 | South Dorchester | 1 | 32.8 | 17.9 | 17.3 | 7.2 | 38.3 | 24.4 | 33.3 | 0 |
| 385 | Springfield (01109) | 1 | 32.5 | 13.3 | 7.7 | 10.0 | 46.8 | 15.4 | 36.9 | 0 |
| 384 | Springfield (01104, 01151) | 1 | 31.3 | 14.4 | 8.0 | 7.5 | 53.6 | 14.6 | 27.3 | 0 |
| 383 | Fall River (02724) | 1 | 30.6 | 14.4 | 12.6 | 7.4 | 60.7 | 11.6 | 21.3 | 0 |
| 382 | Brockton (02301) | 1 | 30.4 | 17.7 | 12.1 | 6.0 | 54.3 | 17.4 | 25.3 | 0 |
| 381 | Fall River (02721) | 1 | 30.3 | 15.0 | 11.7 | 7.3 | 63.9 | 11.4 | 22.2 | 0 |
| 380 | New Bedford (02745) | 1 | 30.2 | 18.8 | 11.4 | 6.1 | 57.2 | 18.7 | 19.6 | 1 |
| 379 | Springfield (01103, 01105, 01107) | 1 | 30.0 | 11.2 | 12.8 | 14.2 | 48.9 | 14.8 | 35.1 | 0 |
| 378 | Lawrence (01843) | 4 | 29.9 | 16.9 | 11.4 | 6.1 | 59.2 | 17.7 | 29.0 | 0 |
| 377 | Taunton | 3 | 29.7 | 19.9 | 14.6 | 4.3 | 57.8 | 21.4 | 17.7 | 5.6 |
| 376 | Brockton (02302) | 3 | 29.5 | 16.9 | 13.2 | 7.5 | 54.6 | 21.1 | 26.2 | 0 |
| 375 | Hyde Park, Boston | 4 | 29.2 | 18.7 | 17.1 | 5.4 | 36.3 | 28.3 | 25.1 | 0 |
| 374 | Springfield (01119, 01129) | 4 | 29.2 | 15.2 | 8.7 | 8.5 | 48.7 | 20.2 | 29.0 | 0 |
| 373 | Revere | 3 | 29.2 | 19.7 | 16.8 | 5.9 | 52.0 | 18.9 | 19.2 | 0 |
| 372 | Fall River (02723) | 3 | 29.2 | 15.3 | 13.7 | 7.6 | 61.0 | 13.2 | 21.1 | 0 |
| 371 | Lynn (01905) | 3 | 29.1 | 15.9 | 12.7 | 6.7 | 55.1 | 16.8 | 26.8 | 0 |
| 370 | Lawrence (01840) | 3 | 29.1 | 10.2 | 13.0 | 15.7 | 60.5 | 10.2 | 26.9 | 0 |
| Average | 16.0 | 12.6 | 7.8 | 53.5 | 17.4 | 26.0 | 0.4 | |||
| Communities with the 20 lowest obesity prevalence ratesc | ||||||||||
| 1 | Cambridge (02138) | 8 | 7.7 | 35.9 | 60.5 | 6.8 | 15.4 | 61.0 | 8.4 | 0 |
| 2 | Back Bay/Beacon Hill, Boston | 8 | 8.7 | 31.1 | 29.5 | 9.3 | 24.8 | 49.0 | 5.1 | 0 |
| 3 | Central, Boston | 8 | 8.7 | 57.2 | 54.2 | 5.9 | 24.1 | 67.6 | 5.3 | 0 |
| 4 | Fenway/Kenmore, Boston | 8 | 10.2 | 12.6 | 22.6 | 14.7 | 31.6 | 30.1 | 13.9 | 0 |
| 5 | Amherst | 8 | 10.5 | 17.4 | 17.7 | 8.2 | 27.5 | 37.6 | 13.2 | 4.1 |
| 6 | Brookline | 8 | 10.6 | 44.3 | 60.0 | 3.5 | 19.8 | 76.1 | 9.4 | 0 |
| 7 | Cambridge (02139, 02142) | 8 | 11.4 | 27.1 | 31.1 | 6.4 | 21.6 | 62.0 | 13.8 | 0 |
| 8 | Wellesley | 8 | 12.1 | 52.9 | 54.8 | 3.5 | 21.7 | 66.4 | 8.9 | 0 |
| 9 | Williamstown | 8 | 12.3 | 26.0 | 16.8 | 6.3 | 27.4 | 42.0 | 10.2 | 21.9 |
| 10 | Wenham | 8 | 12.6 | 36.8 | 36.3 | 30.7 | 33.5 | 42.0 | 7.9 | 15.4 |
| 11 | Newton (02459, 02467) | 8 | 12.6 | 46.1 | 53.6 | 3.8 | 24.1 | 63.0 | 8.3 | 0 |
| 12 | Cambridge (02140) | 8 | 13.1 | 35.0 | 39.4 | 3.3 | 23.8 | 63.1 | 14.9 | 0 |
| 13 | Weston | 8 | 13.7 | 79.6 | 73.9 | 1.7 | 24.8 | 72.5 | 7.4 | 0 |
| 14 | Newton (02458) | 8 | 13.8 | 44.3 | 43.8 | 2.5 | 27.6 | 65.3 | 11.9 | 0 |
| 15 | Lincoln | 8 | 13.9 | 49.1 | 59.0 | 1.5 | 25.4 | 72.8 | 7.5 | 22.6 |
| 16 | Allston/Brighton | 8 | 14.0 | 22.5 | 22.0 | 4.1 | 32.4 | 55.1 | 10.4 | 0 |
| 17 | Newton (02461, 02464, 02468) | 8 | 14.0 | 51.9 | 45.3 | 2.2 | 21.7 | 75.1 | 11.1 | 0 |
| 18 | Newton (02462, 02466) | 8 | 14.0 | 39.2 | 38.5 | 5.3 | 24.8 | 62.3 | 11.0 | 0 |
| 19 | Charlestown, Boston | 8 | 14.5 | 38.9 | 41.5 | 4.4 | 27.4 | 53.5 | 17.5 | 0 |
| 20 | Newton (02460, 02465) | 8 | 14.7 | 45.4 | 40.6 | 1.8 | 27.2 | 66.4 | 10.8 | 0 |
| Average | 39.4 | 42.1 | 6.5 | 25.2 | 58.8 | 10.3 | 3.4 | |||
Rank goes from 1 (the lowest obesity prevalence) to 389 (the highest) and excludes communities with insufficient data.
For an explanation of priority classes, see the “Results” section.
These communities met, or nearly met, the Healthy People 2010 objective of obesity prevalence rates below 15%.
The margins of error (or precisions) of prevalence estimates for the year 2005 ranged from 1.5% to 3.5%, with 63% of the communities having margins of error less than 3.0%.
All communities experienced substantial increases in obesity prevalence from 1999 to 2005. The rate of increase was similar for all communities (likelihood ratio test: P > .70). The odds ratios of change in obesity over any 5-year period ranged from 1.34 to 1.39.
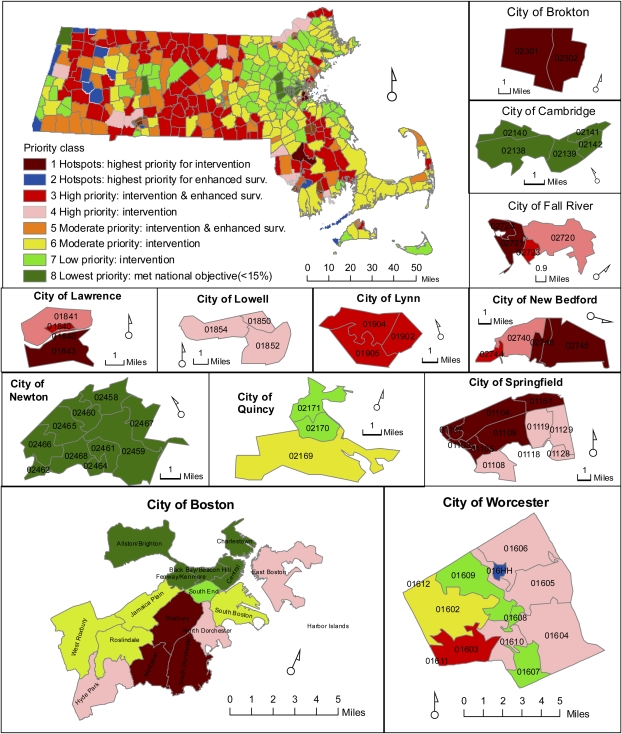
Priority Classification of Communities
The communities were then classified into 8 priority classes:
Class 1. Definite hotspots: communities with obesity prevalence estimates near or above the national average ( ≥ 30%) and of good precision ( ≤ 3.0%). These communities should be a high priority for intervention; we classified 11 communities as definite hotspot communities.
Class 2. Insufficient data: communities with no or insufficient data. These communities are of the highest priority for enhanced surveillance; we classified 7 communities as having insufficient data.
Class 3. High priority: communities with (1) prevalence estimates above the state average ( ≥ 25%) but below the national average (30%) and (2) of limited precision ( > 3%). These communities should be a high priority for both intervention and enhanced surveillance; we classified 85 communities as class 3 high priority communities.
Class 4. High priority: communities with (1) prevalence estimates above the state average ( ≥ 25%) but below the national average (30%) and (2) of good precision ( ≤ 3%). These communities should be a high priority for intervention; we classified 30 communities as class 4 high priority communities.
Class 5. Moderate priority: communities with (1) prevalence estimates above 20% but below the state average ( < 25%) and (2) of limited precision ( > 3%). These communities should be a priority for both intervention and enhanced surveillance; we classified 51 communities as class 5 moderate priority communities.
Class 6. Moderate priority: communities with (1) prevalence estimates above 20% but below the state average ( < 25%) and (2) of good precision ( ≤ 3%). These communities should be a moderate priority for intervention; we identified 113 communities as class 6 moderate priority communities.
Class 7. Lower priority: communities with (1) prevalence estimates above the national objective (15%) but below 20% and (2) of good precision ( ≤ 3%). These communities should be a lower priority for intervention; we classified 73 communities as class 7 lower priority communities.
Class 8. Lowest priority: communities with (1) prevalence estimates that are lower than the national objective ( < 15%) and (2) of good precision ( ≤ 3%). These communities require continued surveillance and should maintain their obesity control efforts; we classified 26 communities as lowest priority communities.
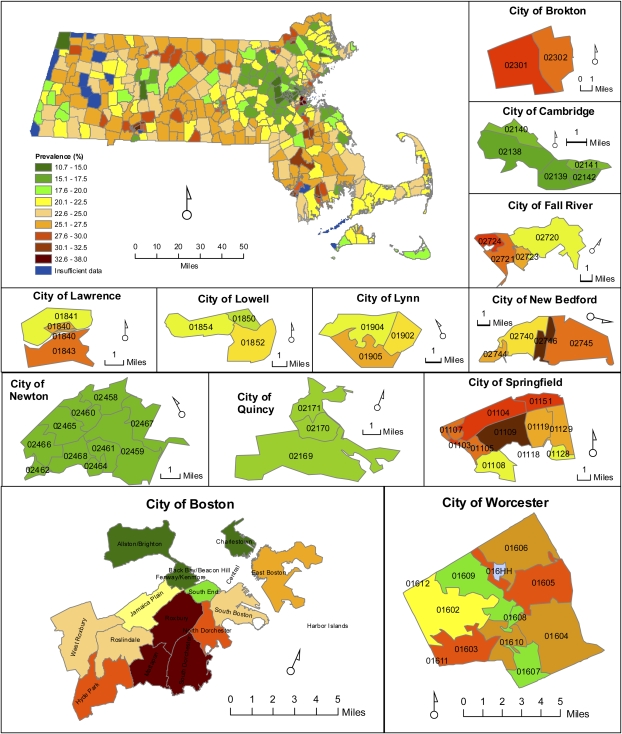
Mapping of Prevalence and Priority Classification of Communities
Obesity prevalence estimates of each community in Massachusetts for 2005 are shown in Figure 1. Geographic disparities in obesity prevalence are evident, with high prevalence occurring in socioeconomically disadvantaged communities, especially poor urban communities. These communities are characterized by low income, lack of white-collar and professional job opportunities, and a higher level of social disorganization (e.g., a higher proportion of families with single parents, shorter tenure of residency). The geographic disparity is largely, but not entirely, explained by the high correlation between obesity prevalence and community-level per capita income (Spearman rank correlation = −0.841; P < .001).
FIGURE 1.
Community-level prevalence of obesity: Massachusetts, 2005.
The priority classifications of communities are illustrated in Figure 2, which shows which communities are of high priority for intervention, for enhanced surveillance, or for both, and which communities have met the national objective of reducing obesity prevalence to below 15% of the population.
FIGURE 2.
Priority classes of communities and recommended actions for obesity control: Massachusetts, 2005.
DISCUSSION
Using Massachusetts BRFSS data, we employed a small-area estimation approach to analyze geographic variations and temporal trends in community-level prevalence of obesity. This approach largely overcomes the problem of small sample size that generally occurs when trying to estimate community-level prevalence. This analysis, along with our previous study on community-level prevalence of cigarette smoking,26 demonstrates the application of small-area estimation methods in public health planning at the community level using existing health surveillance systems.
Previous studies have assessed the association of neighborhood-level effects and individual obesity status using various definitions of community, such as census tract,32,33 5-digit US zip code,34,35 county,36,37 and metropolitan statistical area.38 These studies are important because they also can be used for public health planning. In Massachusetts, the lowest level of government is the town or city. However, to our knowledge, no previous study has examined whether associations between obesity and community-level factors exist at the town or city level, nor have attempts been made to explore how such associations can be applied to improve prevalence estimation at this level and assist in policymaking and evaluation.
Although the prevalence of obesity in Massachusetts is among the lowest in the United States, few communities meet the Healthy People 2010 goal of reducing obesity prevalence to below 15%.7 In all communities in Massachusetts, obesity prevalence increased between 1999 and 2005. Our results imply that, as in other states, the obesity epidemic overwhelms current statewide prevention and control efforts in Massachusetts. The immediate need for strengthening obesity control efforts in all communities challenges Massachusetts to allocate more resources and make efficient use of them for obesity control. Although control efforts should be increased in all communities, highest priority should be given to socioeconomically disadvantaged communities with high prevalence of obesity. Our results provide much-needed data for policymakers and stakeholders in a state with scarce resources for their efforts to address the obesity epidemic.
The rapidly increasing obesity prevalence found in this study is consistent with national and state-specific trends.11,12 The rate of change in obesity prevalence showed little variation among communities in Massachusetts. It remains to be understood why temporal trends varied little but prevalences varied greatly among communities.
The individual- and community-level determinants of obesity observed in this study are consistent with those documented by others.35,39 It is interesting that obesity and cigarette-smoking prevalence share some, but not all, individual-level risk factors, including male gender, lower education, and lower household income. The association between age and obesity peaks during middle age (55–64 years) and is higher among men than among women; however, smoking prevalence progressively decreases with age. Blacks and Hispanics are the most likely to be obese but are less likely to smoke. Members of other minority groups are least likely to be obese or smokers. Living alone is associated with a higher risk of being a smoker but is only weakly associated with obesity.
Similarly, obesity and cigarette-smoking prevalence share some, but not all, community-level determinants.26 Low community per capita income is associated with obesity and even more strongly with smoking. A higher percentage of blue-collar workers predicts obesity better than does smoking. High vacancy rates of occupied housing units predict both obesity and smoking. Median time traveling from home to work, tenure of residency, and percentage of families with a single parent are associated with obesity but not cigarette smoking. Racial diversity and the percentage of the population living in an urban area are associated with smoking but not obesity.
Limitations
This analysis has several limitations as well as strengths. The BRFSS, similar to other telephone surveys, has relatively low response rates and undercoverage of cell-phone—only households.40 In addition, response rates differ among sociodemographic groups. To address this issue, small-area models take into account the demographic characteristics of the small-area populations, whereas conventional direct-estimation methods use poststratification41 or calibration42 weights. The models for correcting self-report bias in body weight and height may reduce, but not completely remove, the biases. About 6.5% of respondents in our study had unknown BMI values; our analysis shows that rates of missing BMI values were higher among women, middle-aged persons, and those with less than a college education. Because single instead of multiple imputations for missing covariate values were used in this analysis, the precision of the prevalence estimates is probably overstated. Our priority classification scheme was based on prevalence estimates and their precision. Other indicators such as prevalence of being at risk for overweight could also be incorporated. When we conducted the analysis collapsing obese and overweight categories (data not shown) into 1 category, however, the community priority classifications were almost identical.
Similar to the small-area estimation model for smoking prevalence,26 the model for obesity prevalence in Massachusetts could be improved in future research by addressing issues related to the uneven distribution of town- or city-specific sample sizes, spatial correlations, probability weighting, and multiple imputations for missing values. The wide variations in town- or city-specific sample sizes could be reduced by increasing sample sizes in rural and smaller communities in the central and western part of the state or by combining adjacent communities that have comparable socioeconomic profiles. More-complex models could be developed to incorporate temporal and spatial correlations among the community-level random effects. Future research will develop new weighting methods that reflect the sampling scheme and demographic composition of the communities under analysis.
In this analysis, we did not include variables related to the physical environment, such as density of grocery stores, businesses, and civic services; proximity to grocery stores, restaurants, and places for exercise; characteristics of transportation systems; and land use patterns. Although these characteristics have been associated with obesity in recent studies, our initial analysis suggests that their relationships with obesity are probably complex and nonlinear (data not shown). With careful delineation and conceptualization, inclusion of these variables may improve the small-area estimation models.
Reliable community-specific prevalence estimates obtained from small-area estimation models make it possible for state and local stakeholders to take into account the community-specific burden of obesity. Several programs of the Massachusetts Department of Public Health have used such estimates to develop obesity control programs that better target communities in need, make efficient use of limited state resources, and comply with federal requirements for allocating funds to vulnerable populations. For instance, we have begun to examine resources for physical activity and accessibility to healthful foods in high-priority communities, using publicly available community auditing tools.43–47 Thus, small-area estimation methods for community-level prevalence will probably play a critical role in future obesity control in Massachusetts and elsewhere.
Acknowledgments
We thank the Massachusetts Behavioral Risk Factor Surveillance System and Division of Health Promotion and Disease Prevention, Massachusetts Department of Public Health, for providing survey and administrative data. The analysis methods and several components of the community-level data were developed by a study supported by the National Institute of Environmental Health Sciences (grant 1R21ES014195).
Human Participant Protection
This study was approved by the University of Massachusetts Medical School institutional review board.
References
- 1.Vastag B. Obesity is now on everyone's plate. JAMA 2004;291(10):1186–1188 [DOI] [PubMed] [Google Scholar]
- 2.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA 2004;291:1238–1245 [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA 2005;293(15):1861–1867 [DOI] [PubMed] [Google Scholar]
- 4.Mark DH. Deaths attributable to obesity. JAMA 2005;293(15):1918–1919 [DOI] [PubMed] [Google Scholar]
- 5.Colditz GA. Economic costs of obesity and inactivity. Med Sci Sports Exerc 1999;31(11 suppl):S663–S667 [DOI] [PubMed] [Google Scholar]
- 6.Manson JE, Skerrett PJ, Greenland P, VanItallie TB. The escalating pandemics of obesity and sedentary lifestyle. A call to action for clinicians. Arch Intern Med 2004;164(3):249–258 [DOI] [PubMed] [Google Scholar]
- 7.Healthy People 2010: Understanding and Improving Health. Washington, DC: US Dept of Health and Human Services; 2000 [Google Scholar]
- 8.Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 2003;289(1):76–79 [DOI] [PubMed] [Google Scholar]
- 9.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA 2001;286(10):1195–1200 [DOI] [PubMed] [Google Scholar]
- 10.Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP. The spread of the obesity epidemic in the United States, 1991–1998. JAMA 1999;282(16):1519–1522 [DOI] [PubMed] [Google Scholar]
- 11.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006;295(13):1549–1555 [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention State-specific prevalence of obesity among adults—United States, 2005. MMWR Morb Mortal Wkly Rep 2006;55(36):985–988 [PubMed] [Google Scholar]
- 13.The Massachusetts Partnership for Healthy Weight Health of Massachusetts: A Coordinated Response to Overweight and Obesity 2005. Boston: Massachusetts Dept of Public Health; 2005 [Google Scholar]
- 14.Willett WC, Domolky S. Strategic Plan for the Prevention and Control of Overweight and Obesity in New England: The New England Coalition for Health Promotion and Disease Prevention. Providence, RI: New England Coalition for Health Promotion and Disease Prevention; 2003 [Google Scholar]
- 15.Yancey AK, Kumanyika SK, Ponce NA, et al. Population-based interventions engaging communities of color in healthy eating and active living: a review. Prev Chronic Dis 2004;1:A09. [PMC free article] [PubMed] [Google Scholar]
- 16.Economos CD, Irish-Hauser S. Community interventions: a brief overview and their application to the obesity epidemic. J Law Med Ethics 2007;35(1):131–137 [DOI] [PubMed] [Google Scholar]
- 17.A Profile of Health Among Massachusetts Adults, 2005—Results From the Behavioral Risk Factor Surveillance System. Boston: Center for Health Information, Statistics, Research and Evaluation, Massachusetts Dept of Public Health; 2006 [Google Scholar]
- 18.White AA. Response rate calculation in RDD telephone health surveys: current practices. Washington, DC: American Statistical Association; 1984:277–282 [Google Scholar]
- 19.Bostrom G, Diderichsen F. Socioeconomic differentials in misclassification of height, weight and body mass index based on questionnaire data. Int J Epidemiol 1997;26(4):860–866 [DOI] [PubMed] [Google Scholar]
- 20.Villanueva EV. The validity of self-reported weight in US adults: a population based cross-sectional study. BMC Public Health 2001;1:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gillum RF, Sempos CT. Ethnic variation in validity of classification of overweight and obesity using self-reported weight and height in American women and men: the Third National Health and Nutrition Examination Survey. Nutr J 2005;4:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nyholm M, Gullberg B, Merlo J, Lundqvist-Persson C, Rastam L, Lindblad U. The validity of obesity based on self-reported weight and height: implications for population studies. Obesity (Silver Spring) 2007;15(1):197–208 [DOI] [PubMed] [Google Scholar]
- 23.Ezzati M, Martin H, Skjold S, Vander Hoorn S, Murray CJ. Trends in national and state-level obesity in the USA after correction for self-report bias: analysis of health surveys. J R Soc Med 2006;99(5):250–257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yun S, Zhu BP, Black W, Brownson RC. A comparison of national estimates of obesity prevalence from the behavioral risk factor surveillance system and the National Health and Nutrition Examination Survey. Int J Obes (Lond) 2006;30(1):164–170 [DOI] [PubMed] [Google Scholar]
- 25.National Health and Nutrition Examination Survey Data Hyattsville, MD: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 1988–1994. Available at: http://www.cdc.gov/nchs/about/major/nhanes/nh3rrm.htm#ag. Accessed September 9, 2008 [Google Scholar]
- 26.Li W, Land T, Zhang Z, Keithly L, Kelsey JL. A method for identifying high-priority communities for tobacco control efforts in Massachusetts. Am J Public Health 2009;99:470–479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Census. 2000 Available at: http://www.census.gov/main/www/cen2000.html. Accessed September 22, 2008.
- 28.Malec D, Sedransk J, Moriarity CL, LeClere FB. Small area inference for binary variables in the National Health Interview Survey. J Am Stat Assoc 1997;92(439):815–826 [Google Scholar]
- 29.Malec D, Davis WW, Cao X. Model-based small area estimates of overweight prevalence using sample selection adjustment. Stat Med 1999;18(23):3189–3200 [DOI] [PubMed] [Google Scholar]
- 30.Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev 2007;29:6–28 [DOI] [PubMed] [Google Scholar]
- 31.Ogden C, Carroll M, McDowell M, Flegal K. Obesity Among Adults in the United States—No Change Since 2003–2004. Hyattsville, MD: National Center for Health Statistics; 2007 [PubMed] [Google Scholar]
- 32.Rundle A, Roux AV, Free LM, Miller D, Neckerman KM, Weiss CC. The urban built environment and obesity in New York City: a multilevel analysis. Am J Health Promot 2007;21(4 suppl):326–334 [DOI] [PubMed] [Google Scholar]
- 33.Schlundt DG, Hargreaves MK, McClellan L. Geographic clustering of obesity, diabetes, and hypertension in Nashville, Tennessee. J Ambul Care Manage 2006;29(2):125–132 [DOI] [PubMed] [Google Scholar]
- 34.Lopez RP. Neighborhood risk factors for obesity. Obesity (Silver Spring) 2007;15(8):2111–2119 [DOI] [PubMed] [Google Scholar]
- 35.Drewnowski A, Rehm CD, Solet D. Disparities in obesity rates: analysis by ZIP code area. Soc Sci Med 2007;65:2458–2463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim D, Subramanian SV, Gortmaker SL, Kawachi I. US state- and county-level social capital in relation to obesity and physical inactivity: a multilevel, multivariable analysis. Soc Sci Med 2006;63(4):1045–1059 [DOI] [PubMed] [Google Scholar]
- 37.Ewing R, Schmid T, Killingsworth R, Zlot A, Raudenbush S. Relationship between urban sprawl and physical activity, obesity, and morbidity. Am J Health Promot 2003;18(1):47–57 [DOI] [PubMed] [Google Scholar]
- 38.Ford ES, Mokdad AH, Giles WH, Galuska DA, Serdula MK. Geographic variation in the prevalence of obesity, diabetes, and obesity-related behaviors. Obes Res 2005;13(1):118–122 [DOI] [PubMed] [Google Scholar]
- 39.Holtgrave DR, Crosby R. Is social capital a protective factor against obesity and diabetes? Findings from an exploratory study. Ann Epidemiol 2006;16(5):406–408 [DOI] [PubMed] [Google Scholar]
- 40.Delnevo CD, Gundersen DA, Hagman BT. Declining estimated prevalence of alcohol drinking and smoking among young adults nationally: artifacts of sample undercoverage? Am J Epidemiol 2008;167(1):15–19 [DOI] [PubMed] [Google Scholar]
- 41.Behavioral Risk Factor Surveillance System (BRFSS) Technical Information and Survey Data: 2005 BRFSS Overview. Atlanta, GA: Centers for Disease Control and Prevention; 2005 [Google Scholar]
- 42.Särndal C-E, Lundström S. Estimation in Surveys With Nonresponse. Hoboken, NJ: Wiley; 2005 [Google Scholar]
- 43.Brownson RC, Hoehner CM, Brennan LK, Cook RA, Elliot MB, McMullen KM. Reliability of two instruments for auditing the environment for physical activity. J Phys Act Health 2004;1:191–208 [Google Scholar]
- 44.Hoehner CM, Ivy A, Ramirez LK, Handy S, Brownson RC. Active neighborhood checklist: a user-friendly and reliable tool for assessing activity friendliness. Am J Health Promot 2007;21(6):534–537 [DOI] [PubMed] [Google Scholar]
- 45.Bedimo-Rung A, Gustat J, Tompkins BJ, Rice J, Thomson J. Development of a direct observation instrument to measure environmental characteristics of parks for physical activity. J Phys Act Health 2006;3(suppl 1):S176–S189 [DOI] [PubMed] [Google Scholar]
- 46.Glanz K, Sallis JF, Saelens BE, Frank LD. Nutrition Environment Measures Survey in stores (NEMS-S): development and evaluation. Am J Prev Med 2007;32(4):282–289 [DOI] [PubMed] [Google Scholar]
- 47.Saelens BE, Glanz K, Sallis JF, Frank LD. Nutrition Environment Measures Study in restaurants (NEMS-R): development and evaluation. Am J Prev Med 2007;32(4):273–281 [DOI] [PubMed] [Google Scholar]