Abstract
Segmental bone defects of the tibia present a challenging problem, particularly when they are associated with soft tissue injuries or instability. Various techniques have been reported to treat bone loss in the tibia. This case report describes a patient with massive segmental bone loss associated with a soft tissue injury, which required a flap for coverage. The injury was treated with an ipsilateral fibular transport utilizing an Ilizarov/Taylor spatial frame. At one and a half year follow-up, the patient was able to walk without any support at home and wore a protective shell for outdoor activities. The outcome of this case study indicates that ipsilateral fibular transport using the Ilizarov method is a valuable technique for limb salvage reconstruction.
Keywords: fibular transport, segmental defect, Taylor spatial frame (TSF), vascularized graft, fibular hypertrophy, Ilizarov
Introduction
Various techniques have been used to treat large segmental tibial defects such as autogenous cortical bone grafts [1], tibiofibular synostosis, ipsilateral fibular graft [2–8], allograft reconstruction [9], vascularized free fibula transfer [10–12], and bone transport. Ipsilateral fibular transport [13–15] is a novel option in limb salvage surgery for patients with large tibial defects.
In 1904, Nichols [2] first presented the use of an ipsilateral fibular graft as a treatment for an infected tibia. The technique included partial dissection of muscle attachments and an osteotomy of the ipsilateral fibula, followed by medial mobilization using the intact attachments. Zahiri et al. [8] successfully used a modification of this method to treat chronic osteomylitis of the entire tibial shaft in nine children. They performed osteotomies at both metaphyses leaving the metaphyseal plates untouched. The two ends of the fibula were brought into the centers of the tibial metaphyseal stumps. Proximal fixation was achieved by locking the end of the fibula into the center of the metaphysis. Distally, an unthreaded Steinmann's pin was drilled from the heel through the calcaneum, talus, and tibial epiphysis into the medullary canal of the transferred fibula. Experiments on Macaca monkeys demonstrated that a vascularized pedicle graft of the shaft of the ipsilateral fibula could be fixed across a defect in the tibia and remain viable, even if isolated from the surrounding tissue [3, 5]. A large graft of ipsilateral fibula raised on a pedicle of peroneal tibial muscles, anterior tibial muscles, and the peroneal vessels, which are aligned and fixed with the tibia in its posterior long axis, could provide a sound mechanical and biological basis of union. However, open methods require large surgical dissections and skeletal stability could be difficult to accomplish [3, 4, 7, 13–15].
The ipsilateral and contralateral fibulae can be used to replace the missing segment using both vascularized [10] and nonvascularized grafts [16]. With vascularized grafts, specialized microvascular techniques are used to re-establish the blood supply. Free vascularized fibular grafting is a complex procedure that requires the expertise of a microvascular surgeon. Excellent results have been reported but complications of thrombosis, nonunion, and deformity have been reported [10]. In addition, complications related to the fibula harvest include hematoma, nerve injury, infection, and valgus deformity of the ankle [17, 18].
The Ilizarov method has been used to successfully transport bone and soft tissues longitudinally to treat tibial bone loss and at times to close an accompanying soft tissue defect [15, 19–24]. A less common application of the Ilizarov technique is transverse bone transport [13, 15, 25]. The frame allows for gradual transport of the fibula into the adjacent tibial defect site, precise proximal and distal alignment of the fibula, and compression at tibial contact sites. This is a minimally invasive technique which requires little surgical dissection.
We present a case report of a patient with massive segmental loss of tibia and an associated soft tissue injury treated with fibular transport utilizing the Ilizarov/Taylor spatial frame (TSF) (Memphis, TN, USA).
Case report
A 41-year-old patient (M.P.) involved in a motorcycle accident presented with a high energy right open tibia fracture with massive bone and soft tissue loss. The patient was initially treated with provisional external fixation and serial irrigation and debridement. The initial defect was 15 cm in length (Figs. 1a and 2a). He had a traumatic brain injury and a percutaneous endoscopic gastrostomy tube was placed for feeding purposes. A free muscle flap was performed early to obtain soft tissue coverage and avoid infection (Fig. 1b). Subsequently, he was referred to the Limb Lengthening and Deformity Service for reconstruction of the bone defect.
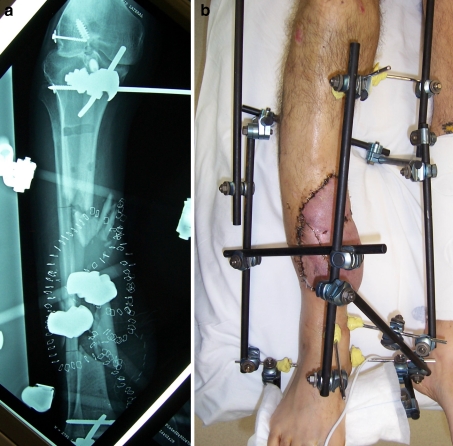
Fig. 1.
a This is an anteroposterior (AP) radiograph prior to the application of the Taylor spatial frame (TSF) showing the initial bony defect in a provisional external fixator. b This preop picture of the patient shows the leg in a provisional external fixator after a free muscle flap was placed to cover the soft tissue defect
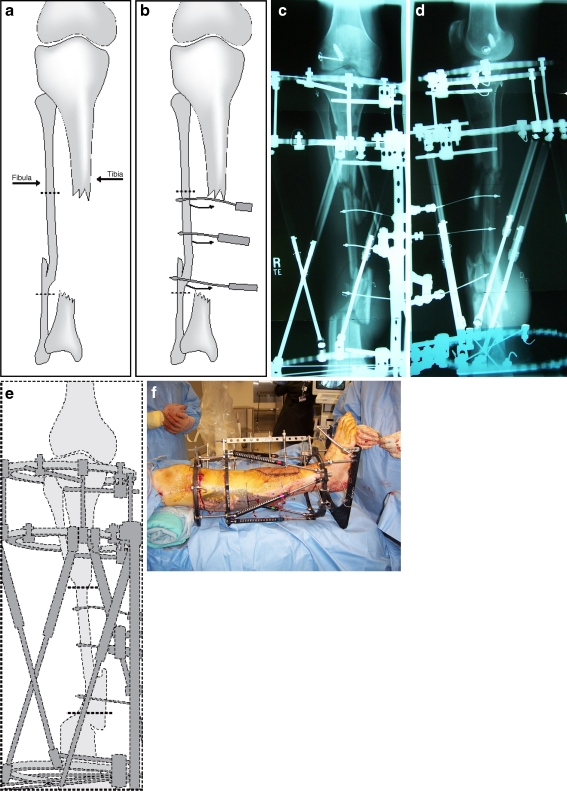
Fig. 2.
a This is an illustration of the 15-cm tibial defect. b A diagrammatic representation of the fibular transport shows the level of the fibular osteotomy and the direction of the fibular transport using three olive fibular pulling wires. c, d The AP/lateral X-ray views of the leg were taken after the application of the two-ring frame and the fibular osteotomies. Note the three fibular wires aiming from posterolateral to anteromedial direction. e This is a diagrammatic representation of the fibular transport in the Ilizarov/TSF with three pulling olive wires. f This picture, taken in the operating room, is of the patient's leg after the application of Ilizarov/TSF2
A month after his accident, he underwent an application of an Ilizarov/TSF along with a two level fibular osteotomy for bone transport. A two-ring frame connected with TSF struts was applied to the leg. This spanned the bone defect and stabilized the proximal and distal bone segments in line with each other. This allowed control of the proximal and distal segments on either side of the defect. A long Ilizarov plate was then connected to the frame anteromedially in preparation for the fibular transport. A two level osteotomy of the fibula was planned at the level of the tibial defect. Three pulling olive wires were placed through the fibula aiming from the posterolateral to the anteromedial (Fig. 2b). The tails of the olive wires were cut at the level of the bead and the olives were positioned against the fibula. These wires were set up as pulling wires and were attached to the anteromedial plate via three short slotted rods that had the capacity to pull all three of these olive wires. The position of these wires was such that it would pull the fibula from the posterolateral position in an anteromedial direction into the tibial defect (Fig. 2a–f).
Next, a 1-in. skin incision was made at the proximal margin of the fibula, where the proximal osteotomy was planned. Dissection was carried down between the lateral and posterior compartments, and using a microsaggital saw, an oblique osteotomy of the fibula was made. The osteotomy was completed with an osteotome. Similarly, at the distal end of the defect, a 1-in. incision was made. Dissection was carried down to the fibula, and using a microsagittal saw, an oblique osteotomy was made. The osteotomy was completed with an osteotome. The osteotomies were not displaced. The wounds were irrigated and closed. The fibula transport was started 10 days postoperatively utilizing the principles of distraction osteogenesis.
Twelve weeks after the application of the frame and the fibular transport, the frame was modified to optimize contact between the tibia and the transported fibula (Fig. 3a,b). The modified frame improved stability and allowed for axial compression between the tibia and the transported fibula. Bone grafting with Op-1 (Stryker, Kalamazoo, MI, USA) was used to promote healing. Four wires were placed into the transported fibula and the adjacent bone. These included a posteromedial olive wire, which was braced medially in order to bring a posteromedial tibial fragment into the alignment, a wire on the distal aspect of the fibular transport and then two opposing olive wires on the proximal main segment of the fibular transport. Two additional rings were placed as rings #3 and #4 of a five-ring construct moving from proximal to distal. All rings were connected with three or four Ilizarov rod connections. Once the rings were in place, the four wires were attached to the rings, and an arched olive wire technique was used to optimize the position, opposition, and compression of the bone. The frame fit the leg well, and the position of the fibular graft remained satisfactory. The alignment was assessed in coronal and sagittal planes using fluoroscopy. The fibular transport wires were removed. An ultrasound bone stimulator (Exogen, Smith & Nephew, Memphis, TN, USA) was used to enhance bone healing.
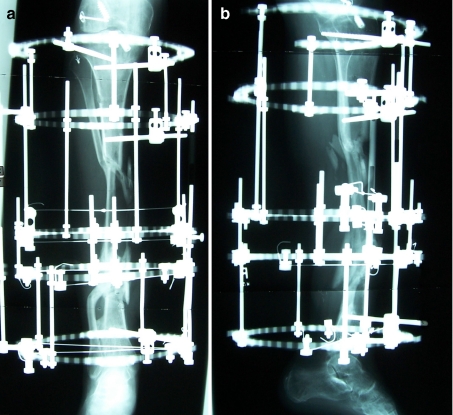
Fig. 3.
a The AP view of the patient's leg shows the Ilizarov/TSF after a modification and application of additional rings. b This is a lateral view of the patient's leg after frame modification
Two weeks later at the first follow-up visit, the overall anteroposterior alignment was normal, but the lateral view showed mild procurvatum. There was a limb length discrepancy of 2.2 cm (Fig. 4). Five weeks following frame modification, a follow-up office visit revealed the graft to be in a satisfactory position. Six months following frame modification, the intermediate and middle rings were removed leaving one proximal and one distal ring connected with the rods. This was done to dynamize the fibula.
Fig. 4.

The 51-in. long X-ray shows leg length and alignment
At 8 months following surgery, the bone showed good alignment and progression of healing (Fig. 5a,b). The frame was further dynamized at this juncture by loosening the connection at the proximal two connection points (Fig. 5c,d). This was done to load the fibula and encourage hypertrophy. Full weight bearing was permitted after dynamization. A superficial pin track infection was noted at 9 months. It resolved with oral antibiotic therapy. The frame was removed 1 year and 10 days following the initial application. The patient was placed in a short leg cast for 2 weeks, and upon cast removal, was able to tolerate full weight bearing (Fig. 6a–c).
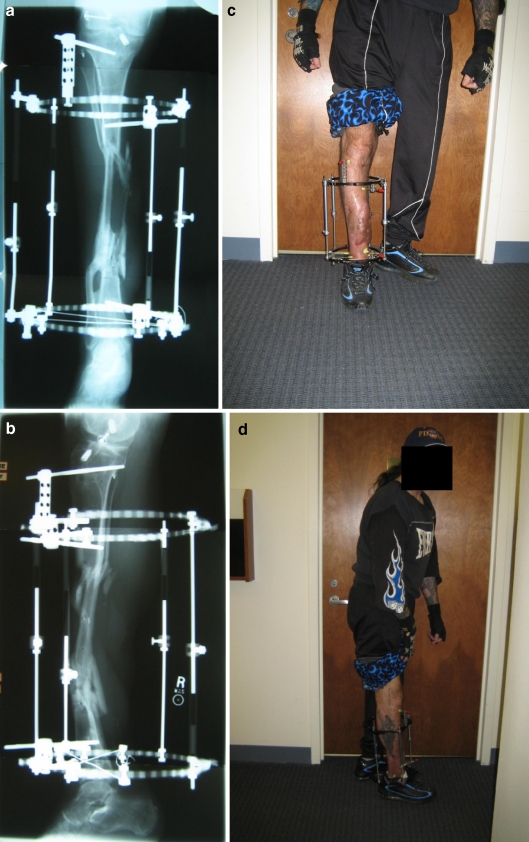
Fig. 5.
a, b The AP/lateral views of the leg show progression of healing and alignment of the fibular transport. This is a dynamized frame. c, d Pictures of the patient standing and full weight bearing after frame modification and dynamization
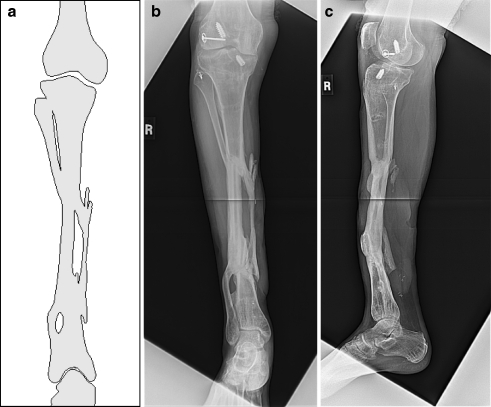
Fig. 6.
a A diagrammatic representation of the healed fibular transport is shown after removal of the frame. b, c AP/lateral X-ray views of the healed fibular transport are shown after removal of frame
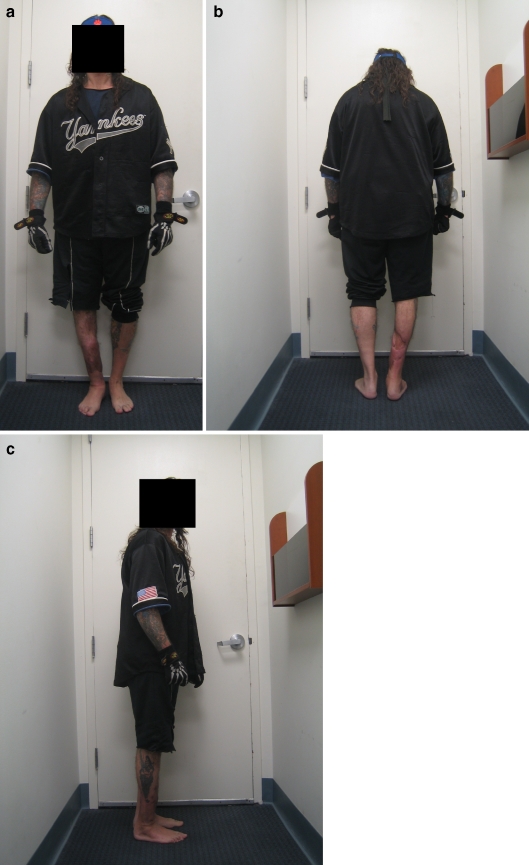
The patient continued to improve, and at the one and a half year follow-up visit, the patient showed a well healed fibula transport. This was assessed by clinical and radiographic measures. The patient continues to walk without any support in his home, and he wears a protective shell for outdoor activities. M.P. tolerates full weight bearing (Fig. 7a–c).
Fig. 7.
a–c These photographs display front, back, and side views of the patient standing without support. He is full weight bearing at this one and a half year follow-up
Discussion
A large segmental defect of the tibia is a difficult problem to treat [2–8, 10, 13, 15, 24]. These patients will often present with other traumatic injuries, and treatment options become limited if soft tissue defects are combined with segmental bone loss. Various methods to fill segmental bone defects such as microsurgical transport of vascularized bone, e.g., rib, iliac crest, fibula, and allograft reconstruction, have also been employed. A below knee amputation is a reasonable alternative solution. However, it is not preferable, particularly in patients who have a normal foot and ankle and do not require vascular repair [26]. Each of these methods is effective depending on the circumstances. They have drawbacks including the possibility of donor site morbidity, deep infection [13], peroneal nerve injury [1], and ankle instability on the contralateral previously unaffected limb. They may be at a high risk of failure [1, 9, 10] as infection, rejection, fracture, and nonunion all have been described with these techniques. A limb salvage reconstruction was chosen with understanding that an amputation could be performed if this failed.
In 1877, Albert [6] first proposed the use of the fibula as a substitute for the tibia. He obtained fusion between the fibula and the femur in a patient with congenital absence of the proximal tibia. Since then, the fibula has been used as a substitute for a missing segment of tibia or to reinforce a weakened section. The major advantage of a perfused transplant is to retain the biological potential of living bone. This gives a shorter time for consolidation, increases potential for remodeling, confers greater resistance to infection, and has better long-term mechanical properties [3–6, 23]. Furthermore, in contrast to an allograft, it has no immunogenicity [5, 9]. The fibula is a straight cortical bone and is long enough to bridge most defects. While it normally carries only one sixth of the static loading of the leg [7], the fibula will undergo hypertrophy [5, 6, 10, 13, 16] when it is subjected to greater loading stresses. This was our rationale for maintaining the patient in a dynamized frame for an extended period of time. This allowed remodeling of the tibia–fibula docking sites and fibula hypertrophy while protecting the fibula from fracture.
Ilizarov described two methods [13, 25] for treating large defects with his fine wire fixator. In the first method, the fibular segment is translated medially, creating a proximal and distal, side-to-side tibiofibular synostosis. This is the method that we used. In the second method, the fibula is split longitudinally and transverse distraction osteogenesis is performed. This technique is complex and no mention is made of the clinical results. Ipsilateral fibular bone transport using an Ilizarov/TSF is a successful approach to safely and effectively fill a tibial defect [3, 5, 7, 13, 15, 25]. It has the advantage of a vascularized fibular graft but does not require large dissection; there is no need for microvascular surgery, and there is no donor site morbidity. A tibia–fibula synostosis and bony healing is achieved at both ends of the defect.
The Ilizarov/TSF allows for stability and longitudinal compression without internal fixation [13, 14, 19, 21]. Furthermore, operative dissection of the fibula is minimal, and the bone remains well vascularized as both sources of blood supply are neither defined nor dissected [22–24]. Muscle attachments are maintained without dissection and the overlying free flap remains undisturbed. The fibular segment is central and is held by the tibial remnants in a mechanically advantageous position in the line of the axis of the tibia. Weight bearing can begin almost immediately after surgery, and the proximal and distal joints are mobilized satisfactorily. Further, limb lengthening may be carried out through a separate corticotomy of either the proximal or distal tibial remnant. However, this procedure has its limitations. It requires a suitable length of uninjured fibula to be available in the same leg, and although this may be present in most tumor cases, it is not always the case in trauma-related injuries.
Acknowledgment
The authors would like to thank Craig Fryman, BS (Research Coordinator).
References
- 1.Enneking WF, Eady JL, Burchardt H (1980) Autogenous cortical bone grafts in the reconstruction of segmental skeletal defects. J Bone Joint Surg Am 62:1039–1058 [PubMed]
- 2.Huntington TW (1905) Case of bone transference. Use of a segment of fibula to supply a defect in the tibia. Ann Surg 41:249–251 [DOI] [PMC free article] [PubMed]
- 3.Chacha PB, Ahmed M, Daruwalla JS (1981) Vascular pedicle graft of the ipsilateral fibula for non-union of the tibia with a large defect: an experimental and clinical study. J Bone Joint Surg Br 63:244–253 [DOI] [PubMed]
- 4.Agiza AR (1981) Treatment of tibial osteomyelitic defects and infected pseudarthroses by the Huntington fibular transference operation. J Bone Joint Surg Am 63:814–819 [PubMed]
- 5.Shapiro MS, Endrizzi DP, Cannon RM et al (1993) Treatment of tibial defects and nonunions using ipsilateral vascularized fibular transposition. Clin Orthop Relat Res 296:207–212 [PubMed]
- 6.Hertel R, Pisan M, Jakob RP (1995) Use of the ipsilateral vascularised fibula for tibial reconstruction. J Bone Joint Surg Br 77:914–919 [PubMed]
- 7.Date AS, Solanki SB, Badhe NP et al (1996) Management of gap non-union of tibia by tibialisation of ipsilateral vascular fibula. J Postgrad Med 42:109 [PubMed]
- 8.Zahiri CA, Zahiri H, Tehrany F (1997) Limb salvage in advanced chronic osteomyelitis in children. Int Orthop 21:249–252 [DOI] [PMC free article] [PubMed]
- 9.Mankin HJ, Hornicek FJ, Raskin KA (2005) Infection in massive bone allografts. Clin Orthop Relat Res 432:210–216 [DOI] [PubMed]
- 10.Wood MB (2007) Free vascularized fibular grafting—25 years' experience: tips, techniques and pearls. Orthop Clin North Am 38:1–12 [DOI] [PubMed]
- 11.Carr AJ, Macdonald DA, Waterhouse N (1988) The blood supply of the osteocutaneous free fibular graft. J Bone Joint Surg Br 70:319–321 [DOI] [PubMed]
- 12.Mozzafarian K, Lascombes P, Dautel G (2008) Vascular basis of free transfer of proximal epiphysis and diaphysis of fibula: an anatomical study. Arch Orthop Trauma Surg (in press) [DOI] [PubMed]
- 13.Atkins RM, Madhaven P, Sudhaker J et al (1999) Ipsilateral vascularized fibular transport for massive defects of the tibia. J Bone Joint Surg Br 81:1035–1040 [DOI] [PubMed]
- 14.Goren D, Sapir O, Stern A et al (2005) Ipsilateral fibular transfer for a large tibial defect caused by a gunshot injury. Mil Med 170:418–421 [DOI] [PubMed]
- 15.Catagni MA, Ottaviani G, Camagni M (2007) Treatment of massive tibial bone loss due to chronic draining osteomyelitis: fibula transport using the Ilizarov frame. Orthopedics 30:608–611 [DOI] [PubMed]
- 16.May JW, Jupiter JB, Weiland AJ et al (1989) Current concepts review clinical classification of post-traumatic tibial osteomyelitis. J Bone Joint Surg Am 71:1422–1428 [PubMed]
- 17.Minami A, Kasashima T, Iwasaki N et al (2000) Vascularized fibular grafts—an experience of 102 patients. J Bone Joint Surg Br 82-B:1022–1025 [DOI] [PubMed]
- 18.Pederson WC, Person DW (2007) Long bone reconstruction with vascularized bone grafts. Orthop Clin North Am 38:23–35 [DOI] [PubMed]
- 19.Mullen JE, Rozbruch SR, Blyakher A et al (2004) Ilizarov method for wound closure and bony union of an open grade IIIB tibia fracture. Case Rep Clin Pract Rev 5:70–75
- 20.Shane JN, Helfet DL, Rozbruch SR (2006) Temporary intentional leg shortening and deformation to facilitate wound closure using the Ilizarov/Taylor spatial frame. J Orthop Trauma 20:419–424 [DOI] [PubMed]
- 21.Rozbruch SR, Adam M, Weitzman BA et al (2006) Simultaneous treatment of tibial bone and soft-tissue defects with the Ilizarov method. J Orthop Trauma 20:197–205 [DOI] [PubMed]
- 22.Rozbruch SR, Pugsley JS, Fragomen AT et al (2008) Repair of tibial nonunions and bone defects with the Taylor spatial frame. J Orthop Trauma 22:88–95 [DOI] [PubMed]
- 23.Cattaneo R, Catagni M, Johnson EE (1992) The treatment of infected nonunions and segmental defects of the tibia by the methods of Ilizarov. Clin Orthop Relat Res 280:143–152 [PubMed]
- 24.Sen C, Kocaoglu M, Eralp L et al (2004) Bifocal compression–distraction in the acute treatment of grade III open tibial fractures with bone and soft-tissues: a report of cases. J Orthop Trauma 18:150–157 [DOI] [PubMed]
- 25.Ilizarov GA (1992) Pseudoarthroses and defects of long tubular bones: treatment of marked defects. In: Ilizarov GA (ed) Transosseous osteosynthesis. Springer, Berlin, pp 478–479
- 26.Lange RH (1989) Limb reconstruction versus amputation decision making in massive lower extremity trauma. Clin Orthop Relat Res 243:92–99 [PubMed]