Abstract
The increased blood loss and resulting need for allogenic blood has been a major concern of one-stage bilateral total knee arthroplasty (TKA). One hundred eighteen consecutive patients donating either 2 units (87 patients) or 3 units (31 patients) of autologous blood prior to one-stage bilateral TKA were retrospectively evaluated to determine: (1) how many patients received allogenic transfusion; (2) what percentage of autologous blood was wasted; and (3) whether donating 2 or 3 units of autologous blood before surgery is more cost-effective. Fifteen patients in the 2-units donation group (17.2%) and one patient in the 3-units donation group (3.2%) required allogenic blood transfusions. In the 2-units group, 37.9% of the patients wasted 21.8% of predonated autologous blood, and in the 3-units group, 64.5% of the patients wasted 32.3% of predonated autologous blood. The estimated cost for patients donating 2 or 3 units of blood was $1,814.17 and $1,996.10, respectively. Donating 2 units of autologous blood is more cost-effective; however, patients donating 3 units of blood required less allogenic blood.
Keywords: autologous blood, cell saver, allogenic blood, transfusion, bilateral total knee arthroplasty
Introduction
The one-stage bilateral total knee arthroplasty (TKA) is still considered controversial for the treatment of bilateral knee arthritis. Some studies have reported increased risk of complications in one-stage bilateral knee arthroplasty [1–8]. Ritter et al. reported that one-stage bilateral TKA is associated with a minimal increase in morbidity and mortality [7]. Bullock et al. reported that complications were slightly raised in bilateral TKA versus unilateral TKA, whereas mortality rates were about the same [9]. The overall blood loss is higher in one-stage bilateral TKA than staged or unilateral TKA [10, 11].
In a recent retrospective study of 461 one-stage bilateral TKA patients, those donating 1 units of autologous blood required allogenic blood in 72% of cases; those donating 2 units of autologous blood required allogenic blood in 48% of cases; those donating 3 units of autologous blood required allogenic blood in 29% of cases; and those donating 4 units of autologous blood required allogenic blood in 27% of cases [12]. The study concluded that preoperative donation of autologous blood does not completely alleviate the need for allogenic blood transfusion after bilateral TKA. Based on a retrospective calculation, the authors suggested that the combination of a perioperative cell saver and 2 units of autologous blood would be the most cost-effective and efficient blood management tool to decrease the need for allogenic blood [12]. A perioperative cell saver has been routinely used at the authors’ institution for patients undergoing one-stage bilateral TKA.
The purpose of this study was to analyze the success of using a perioperative cell saver and predonation of autologous blood in avoiding the need for allogenic transfusion in patients undergoing single-stage bilateral TKA. Specific research aims included studying what percentage of patients require allogenic blood transfusion after donating either 2 or 3 units of autologous blood and what percentage of predonated autologous blood is wasted with either of the protocols. The third aim was to determine which of the two autologous donation protocols (2- or 3-unit predonation) is more cost-effective.
Materials and methods
A case-controlled, retrospective review of 118 one-stage bilateral TKA patients was conducted to observe the incidence of allogenic transfusion comparing two groups: one group that predonated 2 units of autologous blood and one group that predonated 3 units of autologous blood.
Between June 2004 and July 2006, 118 patients were operated on by 15 surgeons at the Hospital for Special Surgery (HSS). Forty-three males and 75 females participated with an average age at the time of the surgery of 64 years (range, 39–79 years). The average height was 169.1 cm (range, 149.9–193 cm), the average weight was 76.2 kg (range, 45.1–114 kg), and the average body mass index was 26.7 kg m−2 (range, 14.0–42.9 kg m−2). The study protocol was approved by the Institutional Review Board at the authors’ institution.
All patients had spinal epidural anesthesia prior to surgery. A pneumatic tourniquet was used routinely. The knees were replaced sequentially beginning with the more symptomatic knee in case the operation had to be discontinued after the first knee replacement. The OrthoPAT® (Transfusion Technologies Corporation, Natick, MA, USA) retransfusion device was connected to the intraoperative suction as soon as the tourniquet was released and was connected to the postoperative drains as soon as the capsule was closed. Warfarin, in combination with a pneumatic foot compression device, was used for thromboembolic prophylaxis in all patients. Continuous passive motion was started in the postoperative anesthesia care unit on the day of surgery.
The age and weight of the patient, the length of the procedure, the intraoperative, and total postoperative blood loss as well as the amount of blood reinfused after surgery were recorded. The amount of predonated autologous blood and the number of autologous and allogenic blood transfusions were documented. The postoperative hemoglobin levels during the first 7 days after surgery were recorded. A hemoglobin level of 8 mg/dL was considered an indication for transfusion in patients with an appropriate clinical picture (hypotension, tachycardia, weakness) of postoperative anemia not relieved by a fluid bolus.
Transfusion indications were individually reviewed and it was assumed that patients with a postoperative hemoglobin greater than 10.5 mg/dL at the time of discharge had received too many blood transfusions if they had no medical conditions justifying increased transfusion requirements, such as preexisting coronary artery disease or a history of myocardial infarction.
To analyze the cost-effectiveness of different approaches, we used the following data: 1 units of autologous blood or 1 units of allogenic blood costs $275 at the author’s institution. If blood is ordered for transfusion, an additional $150 is charged for the type and cross-match of each unit. A transfusion fee of $100 is charged for each transfusion. For the use of the postoperative cell saver system (OrthoPAT®, Transfusion Technologies Corporation), $684 is charged in addition to the $100 transfusion fee.
Student’s t test was used to compare costs and the need for allogenic blood. A p value of less than 0.05 was considered significant.
Results
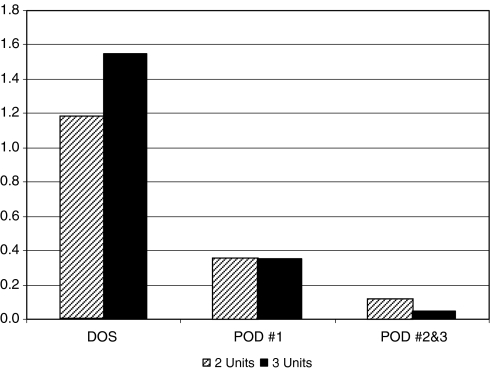
The average intraoperative blood loss was 407.2 mL (range, 150–1,000 mL) and the average postoperative blood loss was 1,697.6 mL (range, 215–5,810 mL). On average, patients received 548.2 mL (range, 50–2,050 mL) of blood from the OrthoPAT® retransfusion device. In one (0.8%) of the 118 patients utilizing the device, not enough blood was collected for reinfusion. There was no difference in preoperative hemoglobin (p = 0.405) and postoperative hemoglobin (p = 0.420) levels between patients who donated 2 or 3 units of blood. In the postoperative period, the patients received an average of 0.97 units of blood (range, 0–6 units; 1.7 units of autologous blood and 0.26 units of allogenic blood) (Fig. 1). Overall, 13.6% of the patients received allogenic blood.
Fig. 1.
The average number of autologous and allogenic blood transfusions for each protocol are displayed for the day of surgery (DOS), postoperative day 1 (POD #1), and postoperative days 2 and 3 (POD #2&3)
Patients that predonated 2 units of autologous blood required more units of allogenic blood than those that predonated 3 units (p = 0.047). Fifteen patients (17.2%) in the 2-units group and one patient (3.2%) in the 3-units group required allogenic blood transfusions (Table 1).
Table 1.
The table displays the preoperative and postoperative hemoglobin levels as well as autologous and allogenic blood transfusion requirements in patients donating 2 or 3 U of autologous blood
| Number of autologous blood donations (units) | Number of patients | Preoperative hemoglobin average (g/dL) | Postoperative hemoglobin average (g/dL) | Average number of autologous blood transfusions | Average number of allogenic blood transfusions | Average number of overall blood transfusions |
|---|---|---|---|---|---|---|
| 2 | 87 | 12.4 | 10.1 | 1.6 | 0.3 | 1.9 |
| 3 | 31 | 12.5 | 10.2 | 2.0 | 0.1 | 2.0 |
Patients in the 3-units group wasted a greater percentage of predonated autologous blood than those in the 2-units group. (p = 0.0003). In the 2-units group, 23 patients (37.9%) wasted 21.8% of predonated autologous blood, and in the 3-units group, 17 patients (64.5%) wasted 32.3% of predonated autologous blood (Table 2).
Table 2.
The preoperative donation of 2 units of autologous blood increases the need for allogenic blood but decreases the percentage of unused autologous blood and overall cost of blood management in patients undergoing one-stage bilateral TKA
| Number of autologous blood donations (units) | Number of patients | Percentage of patients receiving allogenic blood (%) | Unused predonated autologous blood (%) | Patients with unused autologous blood (%) | Patients with cell saver (%) | Cost per Patient (US dollars) |
|---|---|---|---|---|---|---|
| 2 | 87 | 17.2 | 21.8 | 37.9 | 100 | 1,814.17 |
| 3 | 31 | 3.2 | 32.3 | 64.5 | 100 | 1,996.10 |
The average cost of blood management was higher for patients that donated 3 units of autologous blood compared to those that donated 2 units (p = 0.021). The average cost was $1,996.10 in the 3-units group compared to $1,814.17 in the 2-units group.
Discussion
One-stage bilateral TKA is associated with a high perioperative blood loss and need for perioperative blood transfusions [6, 10, 11]. The current case-controlled retrospective study evaluated whether predonation of either 2 or 3 units of autologous blood would decrease the need for allogenic blood transfusion without increasing the percentage of wasted predonated autologous blood and blood management costs.
The current study is limited by its retrospective nature. Transfusion guidelines were not strictly enforced at the authors’ institution, and therefore, the number of transfusions had to be retrospectively corrected in patients who were overtransfused. Another shortcoming is the use of historical controls. The decision to predonate 2 or 3 units of blood is based on surgeon preference.
Total blood loss and transfusion requirements are major concerns after one-stage bilateral TKA [5]. The total blood loss after bilateral TKA is more than double than during unilateral TKA [13]. One-stage bilateral TKA is also associated with increased postoperative transfusion rates [14]. Bottner and coworkers previously reported that donation of autologous blood alone did not reduce the use of allogenic blood to below 25% in one-stage bilateral TKA and recommended predonation of 2 units of autologous blood in combination with a perioperative cell saver [12].
Breakwell and coworkers recently reported that drainage blood reinfusion in bilateral TKA was “a safe and effective method of reducing allogenic blood requirements” [15]. In their study, an average of 1,000 mL of blood was drained and filtered using the Stryker CBCII ConstaVac, reducing average allogenic blood use from 6.3 to 3.8 units [15]. Bottner and coworkers calculated the impact of a cell saver on the need for allogenic blood. It was calculated that the combination of a cell saver with predonation of 2 units of autologous blood would reduce the need for allogenic blood to approximately 8% [12]. In clinical studies, the reduced need for allogenic blood has been less predictable [16]. Implementing a cell saver in combination with an average of 1.68 units of predonated autologous blood (range, 0–3 units) in patients undergoing one-stage bilateral TKA reduced the need of allogenic blood to 17% [16]. This is similar to the data in the current study for patients that predonated 2 units of autologous blood.
Previous studies, in agreement with the findings of this report, suggest that the percentage of wasted autologous blood increases with the number of predonated units of autologous blood [12] Patients donating 1, 2, 3, or 4 units of autologous blood wasted 1%, 5%, 19%, and 23% of predonated autologous blood, respectively [12]. Similar results were observed in the current study and explained that a protocol involving predonation of 2 units of autologous blood is more cost-effective than a protocol involving predonation of 3 units of autologous blood.
Based on the study results, either the use of 2 units predonated autologous blood in combination with a perioperative cell saver or 3 units predonated autologous blood in combination with perioperative cell saver can be recommended. Whether 64% of the patients should donate a third unit of blood to help prevent allogenic blood transfusion in 14% of patients should be individually discussed with the patient.
Acknowledgments
The authors wish to thank the following surgeons for including their patients in this study: David W. Altchek, MD; Mathias P. Bostrom, MD; Frank A. Cordasco, MD, MS; Charles N. Cornell, MD; Mark P. Figgie, MD; Steven B. Haas, MD; Stephen J. O’Brien, MD, MBA; Douglas E. Padgett, MD; Thomas P. Sculco, MD; Edwin P. Su, MD; Geoffrey H. Westrich, MD; and Russell Windsor, MD, PC.
Conflict of interest statement No financial support was received. None of the investigators have a conflict of interest related to the topic of the publication.
Footnotes
Ethical Board Review statement: Institutional Review Board Approval IRB 25053
Level of evidence: level III: retrospective, case-controlled study
References
- 1.Dorr LD, Udomkiat P, Szenohradszky J, Chorn R, Raya J, Udomkiat P, Szenohradszky J, Chorn R, Raya J (2002) Intraoperative monitoring for safety of bilateral total knee replacement. Clin Orthop Relat Res 396:142–151 [DOI] [PubMed]
- 2.Kim YH (2001) Incidence of fat embolism syndrome after cemented or cementless bilateral simultaneous and unilateral total knee arthroplasty. J Arthroplasty 16(6):730–739 [DOI] [PubMed]
- 3.Leonard L, Williamson DM, Ivory JP, Jennison C (2003) An evaluation of the safety and efficacy of simultaneous bilateral total knee arthroplasty. J Arthroplasty 18(8):972–978 [DOI] [PubMed]
- 4.Lombardi AV, Mallory TH, Fada RA, Hartman JF, Capps SG, Kefauver CA, Dodds K, Adams JB (2001) Simultaneous bilateral total knee arthroplasties: who decides? Clin Orthop Relat Res 392:319–329 [DOI] [PubMed]
- 5.Lynch NM, Trousdale RT, Ilstrup DM (1997) Complications after concomitant bilateral total knee arthroplasty in elderly patients. Mayo Clin Proc 72:799–805 [DOI] [PubMed]
- 6.Pavone V, Johnson T, Saulog PS, Sculco TP, Boettner F (2004) Perioperative morbidity in bilateral one-stage total knee replacements. Clin Orthop Relat Res 421:155–161 [DOI] [PubMed]
- 7.Ritter MA, Harty LD, Davis KE, Meding JB, Berend M (2003) Simultaneous bilateral, staged bilateral, and unilateral total knee arthroplasty. A survival analysis. J Bone Joint Surg Am 85:1532–1537 [DOI] [PubMed]
- 8.Ritter MA, Harty LD (2004) Debate: simultaneous bilateral knee replacements: the outcomes justify its use. Clin Orthop Relat Res(428):84–86 [DOI] [PubMed]
- 9.Bullock DP, Sporer SM, Shirreffs TG Jr (2003) Comparison of simultaneous bilateral with unilateral total knee arthroplasty in terms of perioperative complications. J Bone Joint Surg Am 85-A(10):1981–1986 [DOI] [PubMed]
- 10.Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB (1999) An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am 81(1):2–10 [DOI] [PubMed]
- 11.Bould M, Freeman BJ, Pullyblank A, Newman JH (1998) Blood loss in sequential bilateral total knee arthroplasty. J Arthroplasty 13(1):77–79 [DOI] [PubMed]
- 12.Bottner F, Pavone V, Johnson T, Heitkemper S, Sculco TP (2003) Blood management after bilateral total knee arthroplasty. Clin Orthop Relat Res 410:254–261 [DOI] [PubMed]
- 13.Boettner F, Sculco TP (2004) Letters to the editor: blood management after bilateral total knee arthroplasties. Clin Orthop Relat Res 422:270–284 15187867
- 14.Etchason J, Petz L, Keeler E, Calhoun L, Kleinman S, Snider C, Fink A, Brook R (1995) The cost effectiveness of preoperative autologous blood donations. N Engl J Med 332:719–724 [DOI] [PubMed]
- 15.Breakwell LM, Getty CJ, Dobson P (2000) The efficacy of autologous blood transfusion in bilateral total knee arthroplasty. Knee 7(3):145–147, Jul [DOI] [PubMed]
- 16.Lane GJ, Hozack WJ, Shah S, Rothman RH, Booth RE, Eng K, Smith P (1997) Simultaneous bilateral versus unilateral total knee arthroplasty. Outcomes analysis. Clin Orthop 345:106–112 [PubMed]