Abstract
Treatment of extensive diffuse pigmented villonodular synovitis (PVNS) of large joints by isolated surgical resection is unsatisfactory, with high rates of local recurrence. Post-synovectomy adjuvant treatment with external beam radiation therapy or intra-articular injection of radioactive material as yttrium-90 (90Y) yielded better results. Between January 2005 and January 2007, 12 patients (eight men and four women aged 19–49 years) with extensive diffuse PVNS of the knee were treated. All patients had an adjuvant post-operative external beam radiation therapy (2,600–3,000 cGy) conventionally fractionated 200 cGy/fraction, five fractions/week, 6–8 weeks after surgery. Mean follow-up time was 27 months (range from 20 to 36 months). All patients were followed up using clinical assessment, magnetic resonance imaging, and plain X-ray. In all patients, neither evidence of disease recurrence nor progression of bone or articular destruction was noted. No complications were noticed after surgery or after post-operative external beam radiation therapy. A combination of debulking surgery using anterior and posterior approach with adjuvant post-operative external beam radiation therapy for extensive diffuse PVNS of the knee joint is a reliable treatment method, with good results in regard to the incidence of local recurrence and functional outcome.
Keywords: PVN, synovitis, radiosynovectomy, synovectomy
Introduction
Pigmented villonodular synovitis (PVNS) is a benign proliferative histiocytic disorder of the synovium. In 1941, Jaffe described it as a group of synovial, tenosynovial, and bursal lesions [1]. Localized and diffuse forms of synovial involvement were reported [2]. PVNS affects people in their third or fourth decades of life. In most cases, the disease is monoarticular and involves mainly the knee joint; the hip and ankle joints follow in frequency [3]. It has the potential to extensively invade local structures such as muscles, tendons, bones, and skin [4]. PVNS should be included in the differential diagnosis when arthritis with or without a mass presents in a single major joint in young patients. Joint aspiration reveals a brownish discoloration of the fluid due to the breakdown of blood products (hemosiderin) within the joint [5].
The classical appearance of PVNS on plain X-ray films is of a soft-tissue swelling or mass about the joint, with joint-space preservation. Peri-articular osteoporosis is not commonly seen [3]. Erosions or subchondral cysts are common and are more prevalent when PVNS occurs at “tight” joints such as the hip, ankle, or elbow in comparison to the knee [3]. Magnetic resonance imaging (MRI) will show the effusion, and the hemosiderin-laden soft-tissue masses will be seen as areas of low signal intensity on T1 and especially on T2 sequences. This is more pronounced on gradient echo than on spin-echo images [6]. Pathologically, the lesion shows dense infiltrate of polygonal or spindle cells with abundant cytoplasm and vesicular nuclei; some of the cells contain hemosiderin. Multinucleated giant cells are sometimes present, either scarcely or in large numbers. Aggregation of foamy cells can also be seen. Abundant production of collagen, fibrosis, and hyalinization may be evident in patients with long-standing disease [7].
The pathogenesis of PVNS is not clear; however, most authors believe it is caused by chronic inflammation [8]. Others think it is a neoplastic disorder such as a giant cell sarcoma arising near or inside the synovial space or tendon sheath. The latter theory is supported by monoclonality and chromosomal abnormalities [9]. Disturbances of metabolism, trauma, and hemorrhages are other possible etiologies [10].
Complete excision of the mass in the affected joint is the treatment of choice in the localized form. In extensive diffuse cases, total synovectomy is needed, but to carry out this procedure with “acceptable” joint damage is difficult and, in many cases, almost impossible to achieve [7]. This is the reason that other treatment modalities such as external beam radiation and intra-articular injection of 90Y have been tried and shown to be effective in reducing the rate of local recurrence with acceptable joint damage. The main long-term goal is to eradicate the synovial disease while avoiding the need for joint replacement in this characteristically young patient population. In this study, the effectiveness of a combination of debulking surgery using anterior and posterior approaches with adjuvant post-operative external beam radiation therapy for PVNS of the knee was evaluated. The specific aims of the study were to assess functional outcome of the knee at follow-up and to determine the rate of local recurrence [11].
Patients and methods
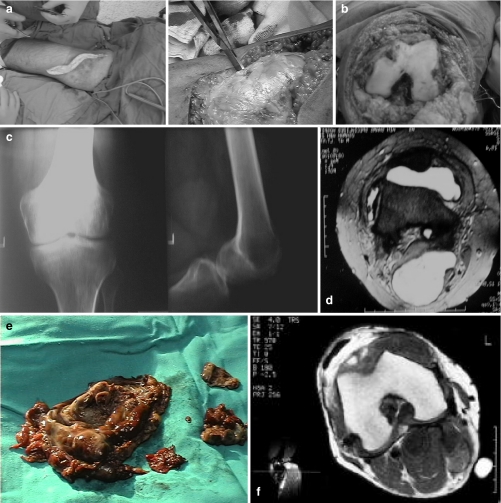
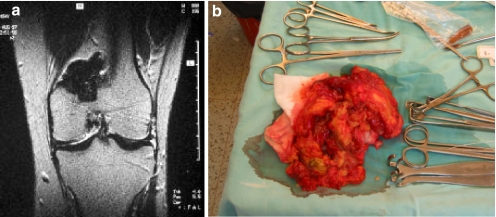
This study was conducted in the Orthopedic Department of Ain Shams University in Egypt. We treated 12 consecutive patients with extensive PVNS of the knee with no bony destruction evident in the pre-operative radiographs. The age of the patients at the time of surgery ranged from 19 to 49 years. There were eight men and four women. The follow-up periods after surgery ranged from 20 to 36 months (Table 1). After clinical examination, imaging studies were carried out to assess the extent of disease. Conventional X-rays was done to assess infiltration of adjacent tissues. MRI was done in all of the patients (Figs. 1d and 2a) and showed nodular intra-articular masses that had low signal intensity on T1- and T2-weighted images. A combination of plain films was used in pre-operative evaluation of all patients. This combination yielded an accurate diagnosis and mapped out the extent of disease prior to treatment.
Table 1.
Age, sex, and follow-up period
| Case no. | Age (years) | Sex | Follow-up period (months) |
|---|---|---|---|
| 1 | 23 | Female | 24 |
| 2 | 19 | Male | 20 |
| 3 | 35 | Female | 24 |
| 4 | 32 | Male | 36 |
| 5 | 19 | Male | 20 |
| 6 | 22 | Female | 36 |
| 7 | 29 | Female | 24 |
| 8 | 36 | Male | 20 |
| 9 | 42 | Male | 36 |
| 10 | 29 | Male | 24 |
| 11 | 49 | Male | 24 |
| 12 | 32 | Male | 36 |
Fig. 1.
a An intra-operative photo of the posterior approach. b An intra-operative photo of the anterior approach. c A pre-operative radiograph. d A pre-operative MRI. e The resected specimen is presented. f The follow-up MRI
Fig. 2.
a The pre-operative MRI of the second patient in the series and b the resected specimen
The surgical technique included combined anterior and posterior approaches to the knee in all cases as the first stage of treatment. The posterior approach was performed first to address the larger, posterior aspect of the lesion. For the posterior approach, the patient is positioned prone. The surgery was performed using a pneumatic tourniquet. General anesthesia was utilized with insertion of an epidural catheter for post-operative analgesia. The skin incision was S-shaped (Fig. 1a), with the upper medial and lower lateral limb meeting at a transverse part over the skin crease. Dissection was performed in layers saving cutaneous nerves, ligating all superficial veins, and avoiding opening the mass. Neurovascular structures were identified and protected. Removal of the mass was facilitated by retracting the heads of gastrocnemius with the knee in flexed position. Closure in layers was done with two suction drains to avoid collection in the resulting dead space. The patient is then turned to the supine position for the second part of surgery with re-draping. The anterior approach is the classic medial parapatellar approach carefully avoiding opening the synovium (Fig. 1b). After removal of the main bulk (Figs. 1e and 2b), small pieces of tissues are removed, and the edges of synovium were cauterized with electro cautery for ablation of very small shreds of synovium. All ligaments and the menisci were spared. Closure is then performed in layers with one suction drain. Post-operatively, no splint was used to allow early range of motion using a CPM machine and epidural analgesia. Assisted weight bearing was stared from the third day post-operative, and patients were discharged home at the fifth day.
Six to 8 weeks after surgery, all patients received adjuvant post-operative external beam radiation therapy. This consisted of 2,600–3,000 cGy conventionally fractionated as 200 cGy/fraction for five fractions per week. The radiation was delivered by a linear accelerator 6-MeV machine. The patients were supine, with immobilization of the joint using an air mattress. The limited fields encompassed the joint being treated only using two parallel opposed fields. The patient was observed twice weekly to assess any acute reactions (skin reaction, joint pain, etc).
For the post-treatment clinical evaluation, the patients were examined every month for 3–4 months. At every outpatient clinic visit (Orthopedic Oncology Clinic), the patient was examined by the authors (operating team and the oncology doctor thereafter) as regard to pain, tenderness, knee range of motion, effusion, and infection. No follow-up biopsies or arthroscopies were performed as it was simple to follow up these patients with clinical examinations, plain X-rays, and MRI in particular. More invasive procedures were reserved for those with suspected recurrence. The functional evaluation was performed using the standard system of The Musculoskeletal Tumor Society with the modifications developed by Enneking et al. [12] (Table 2), which is based on six parameters, including an assessment of pain, functional activities, emotional acceptance, the need for use of external support, walking ability, and gait. For each of the six factors, values of 0 to 5 are assigned based on established criteria. For each specific factor, values (0, 1, 3, or 5) are equated with certain level of achievement or performance. Intermediate values (2 or 4) are assigned based on the examiner’s judgment when the achievement or performance falls between the specific values. The result is expressed as the proportion of the expected normal function for the patient, i.e., a numerical score and percent rating (Table 2).
Table 2.
Functional scoring system
| Score | Pain | Function | Emotional acceptance | Supports | Walking ability | Gait |
|---|---|---|---|---|---|---|
| 5 | None | No restriction | Enthused | None | Unlimited | Normal |
| 4 | Intermediate | Intermediate | Intermediate | Intermediate | Intermediate | Intermediate |
| 3 | Modest | Restriction in recreational activities | Satisfied | Brace | Limited | Minor cosmotic |
| 2 | Intermediate | Intermediate | Intermediate | Intermediate | Intermediate | Intermediate |
| 1 | Moderate | Partial disability | Accepts | One cane or crutch | Household | Major cosmotic minor handicap |
| 0 | Severe | Total disability | Dislikes | two canes or crutches | Unable to walk unaided | Major cosmotic Major handicap |
The radiographic assessment was performed at every visit and consisted of plain X-ray for detection of any soft-tissue shadow or bony erosions. After that, a semi-annual follow-up examination with the same protocol was performed. MRI was performed 6 months (Fig. 1f) after the operation and then once a year for detection of any local recurrence.
Results
During the period of follow-up with a mean of 27 months (range from 20 to 36 months), no evidence of local recurrence and no progressive bone and/or joint destruction were noted on clinical and imaging studies.
No complications were recorded after surgery or external beam radiotherapy: There were no post-operative infections, no wound healing problems, no deep vein thrombosis, and no skin complications such as radiation necrosis.
At the latest follow-up, the functional outcome of the involved joint in all patients was excellent so far according to Enneking’s criteria. The average post-operative score was 85% (80–90; Table 3).
Table 3.
Scoring of the patients
| Case no. | Score (%) |
|---|---|
| 1 | 90 |
| 2 | 80 |
| 3 | 80 |
| 4 | 90 |
| 5 | 80 |
| 6 | 90 |
| 7 | 80 |
| 8 | 90 |
| 9 | 80 |
| 10 | 90 |
| 11 | 80 |
| 12 | 90 |
Discussion
PVNS is a rare, relatively benign, intra-articular lesion characterized by a slowly progressive proliferation of synovial tissue. Patients affected by this condition are at risk for local recurrence. Factors that predict recurrence are not established [13]. The mainstay of treatment has been surgical or arthroscopic synovectomy. Arthroscopic synovectomy has reduced morbidity and is well tolerated by patients. Open surgical synovectomy causes stiffness and pain and has a long recovery time, mainly after procedures involving the knee joint. However, the relapse rates of both approaches are reported to be relatively high, ranging between 8% and 46% [10, 14]. As a result, surgical treatment of large joints alone without adjuvant therapy has been considered unsatisfactory. Synovectomy by radioisotopes has been practiced in clinical rheumatology in several countries for almost 50 years, although randomized clinical trials have never proved it to be effective. The most common target is the chronically inflamed knee joint of a patient with rheumatoid arthritis [16]. In the case of PVNS, post-synovectomy adjuvant treatment with external beam radiation therapy or intra-articular injection of yttrium-90 (90Y) are two adjuvant therapies that have yielded better results compared with surgical excision alone [15]. In this study, we report our experience with a combined open posterior and anterior synovectomy with adjuvant post-operative radiation therapy in patients with advanced PVNS of the knee.
Radiation therapy is usually applied for malignant tumors as a definitive or adjuvant treatment. Radiation therapy for non-malignant conditions is infrequently used. This method of treatment has been suggested for PVNS following partial resection, where salvage of subsequent recurrence may compromise function [16]. None of the reviewed articles compared low-dose radiotherapy with intra-articular injection of 90Y for PVNS. Moreover, the number of patients who were treated using each method was small, and hence, no firm conclusions can be drawn [11–14, 15].
There are few publications that deal with low-dose external beam radiation therapy for treatment of diffuse PVNS [16]. The technique involves treatment of the entire circumference of the limb at joint level with 3,000–4,000 rad. Most of these patients show improvement, although the average follow-up time is unclear. No long-term radiotherapy complications have been described. However, the long-term effects of radiation on soft tissues, bones, or joints, including the risk of secondary cancer, are well known. Since PVNS is still a benign disorder, the use of even low-dose radiotherapy should be considered with caution [16]. In our patients, no complications related to radiation were detected either locally or generally so far, yet long-term follow-up is required.
We combined external beam radiation and a traditional open synovectomy by performing debulking, leaving behind a microscopic amount of disease to be treated with radiotherapy. In this way, we avoided the disadvantages of complete total synovectomy and the very high recurrence rate in such difficult cases.
This series is small, with variation of ages and affected joints, but it includes only extensive diffuse PVNS of these joints in young patients. This study is limited due to the small number of cases included, and it lacks comparison with other techniques dealing with the same cases. It did not include neither patient with small localized PVNS of the knee nor control groups. Comparison with intra-articular radiation using the so-called magic capsules or radiation pellets are lacking due to unavailability of such modality in our country and very high cost of importing them. The functional results might not be reliable, being based on subjective criteria, but this needs further evaluation on large number of cases.
The final common pathway of PVNS of the knee leads to total joint destruction, which eventually leads to the need for joint replacement. This should be avoided if possible, especially in these young and healthy patients. Combined surgical and radiosynovectomy is effective in treating extensive PVN lesions of the knee joint because of no reported recurrences and acceptable functional outcome and can be used as a cost-effective alternative to intra-articular radiotherapy.
Footnotes
Level of evidence: level IV—retrospective case series
References
- 1.Jaffe HL, Lichtenstein L, Sutro CJ (1941) Pigmented villonodular synovitis: bursitis and tenosynovitis. Arch Pathol 31:731–765
- 2.Flandry FC, Hughston JC (1987) Current concepts review: pigmented villonodular synovitis. J Bone Joint Surg 69:942 [PubMed]
- 3.Dorwart RH, Genant HK, Johnston WH et al (1984) Pigmented villonodular synovitis of synovial joints: clinical, pathologic and radiologic features. AJR Am J Roentgenol 143:877–885 [DOI] [PubMed]
- 4.Ray RA, Morton CC, Lipinski KK et al (1991) Cytogenetic evidence of clonality in a case of pigmented villonodular synovitis. Cancer 67:121–125 doi:10.1002/1097-0142(19910101)67:1<121::AID-CNCR2820670122>3.0.CO;2-P [DOI] [PubMed]
- 5.Rao AS, Vigorita VJ (1984) Pigmented villonodular synovitis (giant cell tumor of the tendon sheath and synovial membrane). A review of 81 cases. J Bone Joint Surg Am 66:76–94 [PubMed]
- 6.Bravo SM, Winalski CS, Weissman BN (1996) Pigmented villonodular synovitis. Radiol Clin North Am 34:311–326 [PubMed]
- 7.Schwartz HS, Unni KK, Pritchard DJ (1989) Pigmented villonodular synovitis. A retrospective review of affected large joints. Clin Orthop 247:243–255 [PubMed]
- 8.Sakkers RJ, deJong D, van der Heul RO (1991) X-chromosome inactivation in patients who have pigmented villonodular synovitis. J Bone Joint Surg Am 73:1532–536 [PubMed]
- 9.Choong PF, Willen H, Nilbert M et al (1995) Pigmented villonodular synovitis. Monoclonality and metastasis—a case for neoplastic origin? Acta Orthop Scand 66:64–68 [DOI] [PubMed]
- 10.Ohjimi Y, Iwasaki H, Ishiguro M et al (1996) Short arm of chromosome 1 aberration recurrently found in pigmented villonodular synovitis. Cancer Genet Cytogenet 90:80–85 doi:10.1016/0165-4608(96)00064-7 [DOI] [PubMed]
- 11.Franssen MJ, Boerbooms AM, Karthaus RP, Buijs WC et al (1989) Treatment of pigmented villonodular synovitis of the knee with yttrium-90 silicate: prospective evaluations by arthroscopy, histology and 99 mTc pertechnetate uptake measurements. Ann Rheum Dis 48:1007–1013 doi:10.1136/ard.48.12.1007 [DOI] [PMC free article] [PubMed]
- 12.Enneking WF, Dunham W, Gebhardt MC et al (1993) A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop 286:241–246 [PubMed]
- 13.Adem C, Sebo TJ, Riehle DL et al (2002) Recurrent and non-recurrent pigmented villonodular synovitis. Ann Pathol Dec 22(6):448–452 [PubMed]
- 14.Kat S, Kutz R, Elbracht T et al (2000) Radiosynovectomy in pigmented villonodular synovitis. Nucl Med 39(7):209–213 [PubMed]
- 15.Shabat S, Kollender Y, Merimsky O et al (2002) The use of surgery and yttrium 90 in the management of extensive and diffuse pigmented villonodular synovitis of large joints. Rheumatology (Oxford) 41(10):1113–1118, Oct [DOI] [PubMed]
- 16.Franke C (2000) Value of radiosynovectomy in rheumatology and orthopedics. Schweiz Med Wochenschr 130:77–83 [PubMed]