Abstract
Background
Many patients demonstrate psychological distress and reduced physical activity before coronary artery bypass graft surgery (CABG). Here we evaluated the addition of a brief, cognitive-behavioural intervention (the HeartOp Programme) to routine nurse counselling for people waiting for CABG surgery.
Methods
Randomised controlled trial comparing nurse counselling with the HeartOp programme to routine nurse counselling in 204 patients awaiting first time elective CABG. Primary outcome measures were: anxiety and length of hospital stay; secondary outcome measures were: depression, physical functioning, cardiac misconceptions and cost utility. Measures were collected prior to randomisation and after 8 weeks of their intervention prior to surgery, excepting length of hospital stay which was collected after discharge following surgery.
Results
100 patients were randomised to intervention, 104 to control. At follow-up there were no differences in anxiety or length of hospital stay. There were significant differences in depression (difference = 7.79, p = 0.008, 95% CI = 2.04–13.54), physical functioning (difference = 0.82, p = 0.001, 95%CI = 0.34–1.3) and cardiac misconceptions (difference = 2.56, p < 0.001, 95%CI = 1.64–3.48) in favour of the HeartOp Programme. The only difference to be maintained following surgery was in cardiac misconceptions. The HeartOp Programme was found to have an Incremental Cost Effectiveness Ratio (ICER) of £288.83 per Quality-Adjusted Life Year.
Conclusions
Nurse counselling with the HeartOp Programme reduces depression and cardiac misconceptions and improves physical functioning before bypass surgery significantly more than nurse counselling alone and meets the accepted criteria for cost efficacy.
Keywords: Pre-operative care, Coronary artery bypass, Self-care, Cognitive-behavioural treatment
1. Introduction
Many patients find the uncertainty and fear of waiting for coronary artery bypass (CABG) surgery to be more disturbing than their chest pain [1,2]. This may have long term disabling consequences, as patients adopt a sedentary lifestyle so that the normal routines of work and active hobbies are lost, sometimes forever [3]. As a result quality of life and physical and mental health may decline [4].
Cognitive-behavioural chronic disease management programmes have been shown to reduce anxiety and depression and readmissions after MI [5]. A brief cognitive-behavioural programme for patients with angina has been found to reduce psychological distress and self-reported episodes of angina as well as improving physical functioning [6].
Nurse-led educational programmes also reduce anxiety and depression and improve health behaviours in patients awaiting CABG. For example, an intervention based on motivational interviewing was found to reduce risk factors and improve physical and psychological functioning [7]. A preoperative, hospital based exercise programme reduced post-operative hospital stay and improved quality of life [8].
One of the problems of delivering pre-surgical interventions for these patients is that many live at a distance from the hospital where the surgery is to be conducted. A recent review of uptake of rehabilitation showed distance from the programme and transportation problems to be major barriers to attending hospital based rehabilitation programmes [9]. One solution is to deliver the intervention in the patients' home. A recent systematic review and meta-analysis of home-based rehabilitation showed it to be as effective as hospital based programmes [10].
The aim of the study reported here was to evaluate a brief, home-based cognitive-behavioural, phone facilitated programme (the HeartOp Programme) for patients awaiting elective CABG. Pre-operative nurse counselling for behaviour change is routine care in some centres within the UK. For that reason, we chose to compare the HeartOp Programme to routine preoperative nurse counselling, rather than compare it to “no intervention”, and give both interventions a similar amount of patient contact time. It was accepted that there may be some overlap in the interventions, and so any effects of the HeartOp Programme would be weakened, but we believed that it was important to test the programme against the current version of optimal care.
1.1. Objectives
To test the HeartOp Programme in a randomised controlled trial compared to preoperative nurse counselling.
1.1.1. Hypothesis
Patients taking part in the HeartOp Programme would be less anxious preoperatively and have a shorter length of stay following surgery compared to patients receiving a similar amount of time and attention from a specialist nurse.
2. Materials and methods
2.1. Patients and settings
Hull and East Riding local Research Ethics Committee approved the study, and all participants gave informed consent.
Patients who were placed on the elective waiting list for first time CABG in a tertiary centre in northern England were screened for eligibility using the following criteria:
Inclusion criteria: All patients admitted to the routine (non-urgent) waiting list for CABG at a cardiothoracic centre, ability to give informed consent.
Exclusion criteria: Exercise induced arrhythmias, loss of systolic BP greater than 20 mm Hg during exercise stress testing, unstable angina, a score of 4 on the Canadian Cardiovascular Society classification for angina or the New York Heart Association classification of heart failure, current psychiatric problems, dementia, self report of periods of dizziness or confusion, life threatening co-morbidities, concurrent participation in other research.
Patients meeting the criteria were invited into the study by a letter from their cardiac surgeon. Those wishing to participate attended an outpatient clinic where informed consent and baseline investigations were undertaken which included: New York Heart Association (NYHA) classification of breathlessness [11], Canadian Cardiovascular Society Angina Class (CCSAC) [12], systolic blood pressure (SBP), body mass index (BMI), smoking status (verified by expired carbon monoxide level), Step Test — a validated, safe and simple clinical instrument that strongly and reliably predicts VO2 max and is sensitive to change [13].
2.2. Interventions
Both interventions consisted of a 45–60 minute first interview conducted in the outpatients clinic by the nurse facilitator, followed by 10–15 minute phone calls to their home at weeks 1, 3 and 6 (+/− 1 week) and then monthly until they were admitted for their operation. As previously stated, it was accepted that there was a possibility of some contamination in the delivery of the interventions. For example, smokers in both arms of the study were advised to attend NHS smoking cessation groups as this is considered the best practice. In order to keep contamination between the interventions to a minimum, a prompt sheet was used to structure the interviews and a checklist of questions for the telephone follow-up was used for each intervention. The written materials were different for each intervention.
2.2.1. The HeartOp Programme (experimental) intervention
The HeartOp Programme comprises of a two-part patient-held booklet (the HeartOp Plan) which covers: cardiac myths and misconceptions, reducing risk factors for secondary prevention, and what to expect during the hospital stay and subsequent recovery period. The programme also includes a relaxation programme on audiotape or CD and a diary for recording activity and risk factor reduction goals. The ‘facilitator’ initially aims to dispel specific cardiac misconceptions (which have been shown to be predictive of psychological distress and poor coping [14,15]), and to then work with the patient to agree and set goals to reduce cardiovascular risk and increase activity levels. The HeartOp programme is introduced to the patient in a first interview and the goals are recorded in the diary, which the patient uses to record their progress every day. The facilitator follows-up the patient by telephone to check misconceptions, discuss the patient's progress and to set new goals (a method termed goal setting and pacing which uses problem solving techniques to set patient centred, achievable goals).
2.2.2. The nurse education and counselling (control) intervention
At the first interview patients were asked to describe their illness experience and were offered verbal advice on their risk factors and a description of the operation and after-care, which was accompanied by written information (British Heart Foundation booklets). No effort was made to elicit specific misconceptions, but if the patient asked questions that included these misconceptions, they were dispelled. Formal goal setting and pacing was not used, instead patients were given general advice on reducing risk factors. In the follow-up phone calls patients were asked how they were managing with their risk factor reduction and for their concerns.
Post-operatively all patients (both arms of the study) received written and verbal advice prior to discharge on self-management in the first 6 weeks, including advice on increasing activity, wound care, diet and responding to common concerns about their recovery. All patients were offered a cardiac rehabilitation programme commencing at 6 weeks post-operatively.
2.3. Outcomes
2.3.1. Primary endpoints
2.3.2. Secondary endpoints
-
1)
Depression (Cardiac Depression Scale [CDS] — a 26-item questionnaire found to be normally distributed, valid and reliable in people with CHD [18]),
-
2)
Physical functioning (Mobility scale of the Cardiovascular Limitations and Symptoms Profile — M-CLASP. This 4-item scale has been validated in people with CHD and demonstrates a better correlation with performance on a treadmill than the mobility scale of the Symptom Impact Profile. [19]),
-
3)
Cardiac misconceptions (pilot version of the York Cardiac Beliefs Questionnaire — pYCBQ). This is a 24-item questionnaire of common misconceptions about living with heart disease drawn from patient interviews. It has shown satisfactory internal reliability (Cronbach's alpha = 0.85) and test–retest stability (r = 0.88) when pilot tested on 100 people who had undergone CABG,
-
4)
Cost Utility (a record of costs such as GP visits and admissions to hospital were taken from self-completed questionnaires. Health related utility was measured using the EQ5D [20]).
2.3.3. Data collection
T1: baseline (all data) and T2: All questionnaire measures were collected by postal survey after the 3rd phone call of the intervention (These would be received by the patient approximately 8 weeks after the baseline measures.). In order to standardise questionnaire data collection, the time for collection of T2 data was based on the mean time to operation of the surgeon with the shortest waiting time, as there were considerable differences in this among the four surgeons. Length of hospital stay was collected by case note review following discharge (or death) after surgery. Post-operatively, data were collected at 6 weeks, 3 months and 6 months.
2.4. Sample size
Over 600 people underwent CABG surgery at Hull and East Yorkshire Hospitals Trust in 2001. It was estimated that 400 patients would meet the inclusion criteria for the study during the recruitment phase (01/10/2003 to 31/12/2004). Allowing for 25% refusal, it was anticipated that approximately 300 patients would participate in the study.
2.4.1. Power analysis
All power analyses were carried out using α = 0.05, and assuming 150 patients in each of the two groups. All tests were two-tailed.
2.4.1.1. Anxiety
In the study by McHugh et al. [7] the proportion of individuals who scored 11+ on the HAD anxiety scale at follow-up were 89% (control) and 18% (intervention). The proposed sample size had 98% power to detect a difference in proportion of this size.
2.4.1.2. Length of hospital stay
The data presented by Arthur et al. [8] were not in a format which allows a power analysis to be carried out straight forwardly. If a survival analysis approach was employed, the sample size of 150 per group will provide 80% power, for a hazard ratio of 0.424, using a log-rank survival test.
2.4.2. Randomisation
This was undertaken by a researcher not otherwise involved in the study using computer-based random-sequence generation, stratified by the four surgeons. Remote randomisation to groups was via a remote telephone service manned by staff not otherwise involved in the study. Randomisation took place after patients agreed to the study and immediately prior to the interventions. Interventions were delivered by a nurse not involved in collecting follow-up data. All data entry and analysis were blind to group allocation.
2.5. Statistical methods
2.5.1. Data analysis
All analyses were intention to treat with linear interpolation of missing data. Data were analysed using analysis of covariance, with surgeon as a random factor, and controlling for the baseline (T1) variables: NYHA, CCSAC, BMI, systolic BP, smoking status, step-test time and T1 outcome variable. Comparison of length of hospital stay was undertaken using survival analyses.
2.6. Economic analysis
The analysis was carried out using baseline and preoperative data (8-weeks follow-up from baseline) using WinBUGs version 1.4 [21] in order to employ a Bayesian approach.
2.6.1. Measurement of resource use
The cost of patient materials used in the intervention arm was the only cost difference between the two interventions. The control group received BHF booklets (which are free to the NHS) and the intervention received the HeartOp Programme. Using the model of the Angina Plan [6], it was estimated that the cost of the intervention patient materials would be £10 per patient. The use of healthcare resources in terms of GP visits and hospital admissions were self-reported by participants at baseline and 8 weeks.
2.6.2. Unit costs
The cost effective analysis was carried out from the perspective of the Health Provider, the UK NHS. Prices were based on 2003–2004 costs, in pounds sterling. The unit cost of a single visit to a general practitioner (£22.19) were taken from a previous trial [22] and up rated. If the participant recorded a hospital admission it was assumed to be for one night in a cardiology ward (@ £481 per night). This cost was calculated from national averages [23] as a percentage of the fully allocated cost per day of a cardiology bed.
2.6.3. Utility measure
Quality-Adjusted Life Years (QALYs) were used as a measure of health outcome for the analysis. QALYs have the advantage of reflecting both health related quality of life and mortality into a single index. Individuals QALYs data were calculated using the EQ-5D questionnaire, a widely recognised and validated generic measure of health related quality of life. Individual's EQ-5D values were used to calculate their specific QALYs at 8 weeks using the area under the curve method.
Analyses were carried out to investigate the incremental costs and utilities associated with each intervention group in the form of the incremental cost effectiveness ratio (ICER). The ICER represents the additional cost that the decision maker (e.g. National Institute of Clinical Excellence in the UK) is (on average) expected to pay to achieve an additional QALY. As a rough guide, policy makers in the UK tend to recommend treatments costing £30,000 per QALY or less [24].
3. Results
3.1. Main analyses
3.1.1. Participant flow
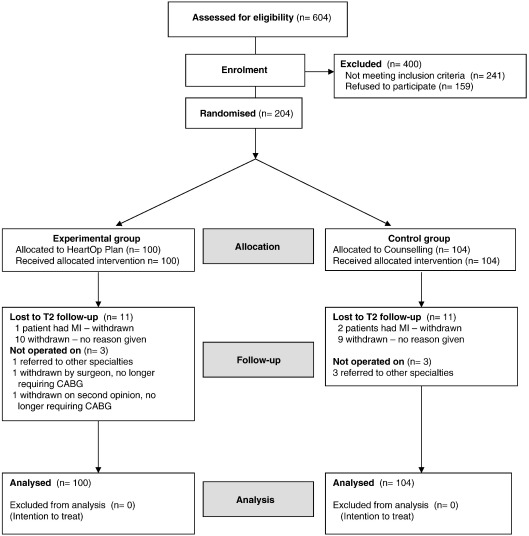
See Fig. 1.
Fig. 1.
Flow of participants through the study.
3.1.2. Recruitment
Took place from 01/10/2003 to 31/12/2004, with follow-up to 31/10/2005. 363 patients of the 600 who were listed for elective surgery during the recruitment phase met the study criteria; of whom 204 consented to take part and completed baseline data (100 were randomised to receive the HeartOp Programme and 104 to control). Completed data were received from 182 (89%) participants (88 HeartOp and 94 control) at T2. Six patients were not operated on during the time of study follow-up: 4 (1HeartOp, 3 Control) were awaiting referral to other specialities, 1(HeartOp) patient was withdrawn from surgery by the surgeon, as not requiring it, and 1 (HeartOp) patient withdrew from surgery after improving her fitness markedly, following further consultation with a cardiologist.
There were no significant differences between participants and non-participants for age (mean difference = 0.82 years, 95%CI = − .99–2.64, p = 0.37) or gender (Odds Ratio for male in study: 1.38, 95%CI = 0.84–2.27).
There were no significant differences between the study groups for any baseline characteristic or measure (Table 1). There was no significant difference in mean wait from entry to the study to operation, which was 112 (SD 44.83) days. Median length of hospital stay was 7 days.
Table 1.
Baseline characteristics of the groups
| HeartOp Plan (n = 100) | Control (n = 104) | |||
|---|---|---|---|---|
| Gender: male n (%) | 85 (85) | 79 (76) | ||
| Current smokers: n (%) | 10 (10) | 8 (8) | ||
| Mean (SD) | Mean (SD) | |||
| Age | 64.25 (8.81) | Range: 42–83 | 65.29 (8.51) | Range: 47–83 |
| NYHA class | 2.01 (0.83) | 2.15 (0.83) | ||
| Canadian angina class | 2.26 (0.68) | 2.17 (0.80) | ||
| Body mass index | 28.79 (4.21) | 29.28 (5.05) | ||
| Systolic BP | 145 (20) | 145 (21) | ||
| Step test time in minutes | 0:01:01 | 0:01:04 | ||
| State anxiety scale | 40.01 (12.30) | 41.52 (12.69) | ||
| Cardiac depression scale | 93.09 (22.12) | 96.78 (23.49) | ||
| Clasp mobility scale | 9.06 (2.69) | 9.33 (3.16) | ||
| Cardiac beliefs scale | 7.25 (4.18) | 8.13 (4.41) | ||
3.1.3. Primary endpoints
When controlling for NYHA, CCSAC, BMI, systolic BP, smoking status, step-test time and T1 dependent variable; there were no significant differences in anxiety (mean difference when controlling for all of the covariates: 1.07, p = 0.49, 95%CI − 1.98 to 4.12, Eta2 = 0) or length of hospital stay (HeartOp mean (SD): 7.61(2.69) vs. Control: 8.28(4.96)days) hazard ratio = 0.98, 95% CI = 0.72 to 1.34, p = 0.90).
3.1.4. Secondary endpoints
Using a similar analysis strategy there were significant differences for depression, physical functioning on CLASP mobility scale, and cardiac beliefs (Table 2). Cohen [25] suggested the following guidelines for evaluating the strength of Eta squared: 0.01 is a small effect, 0.06 a moderate effect and 0.14 a large effect.
Table 2.
Comparisons on secondary endpoints preoperatively (T2)
| Score at baseline |
Score at t2 |
Mean diff at t2 | Mean diff† | Sig | Lower |
Upper |
Eta |
|||
|---|---|---|---|---|---|---|---|---|---|---|
| I | C | I | C | CI | CI | Sq | ||||
| t2 Cardiac depression scale | 93.09 | 96.78 | 81.69 | 93.37 | 11.68 | − 7.79 | 0.008 | 2.04 | 13.54 | 0.05 |
| t2 Clasp mobility | 9.06 | 9.33 | 8.10 | 9.05 | 0.95 | − 0.82 | 0.001 | 0.34 | 1.30 | 0.07 |
| t2 Cardiac beliefs | 7.25 | 8.13 | 4.10 | 7.61 | 3.50 | − 2.56 | <0.001 | 1.64 | 3.48 | 0.17 |
(I = Intervention, C = Control, † Mean difference controlling for all of the covariates, positive value means intervention group was higher, negative means lower. All measures: lower scores = better outcome.)
3.1.5. Adverse events
No patient died in the preoperative period, and the small number of people who suffered from non-fatal cardiac events (3/204 — 2 control, 1 intervention) are not amenable to statistical analysis. Two patients (1 intervention, 1 control) died from side-effects of the operation (1 control from cerebrovascular accident, and 1 intervention from infected heart valve).
3.1.6. Post-operative follow-up
There were no significant differences on any measure between the two groups at any post-operative follow-up, except on cardiac misconceptions, for which the significant difference was maintained to 6 months post-operatively (mean difference − 2.26, p = < 0.001, 95%CI 1.27 to 3.25). Anxiety and depression scores were reduced in both groups at 6 months post-operatively compared to T2 (Anxiety: mean difference = 9.5, t = 9.7, p < 0.001, 95%CI 7.53 to 11.38; Depression: mean difference = 25.13, t = 12.69, p < 0.001, 95%CI 21.09 to 28.86).
3.2. Economic statistical analysis
3.2.1. Resource use
Table 3 shows the results relating to the main healthcare resources use during the trial over the eight-week preoperative follow-up period. There was very little difference in resource use between the two groups (£22.37 vs. £24.10) with the intervention having a higher incremental mean cost of £1.73 (95% credibility intervals = − 17.73 to 20.63).
Table 3.
Resource use
| During 8 weeks follow-up | Number of cases (%) |
|
|---|---|---|
| Control (n = 104) | Intervention (n = 100) | |
| No. visits to NHS GP | ||
| 0 (includes missing) | 82 (78.9) | 75 (75.0) |
| 1–2 | 19 (18.3) | 21 (21.0) |
| ≥ 3 | 3 (2.9) | 4 (4.0) |
| No. admissions to NHS Hospital | ||
| 0 (includes missing) | 101 (97.1) | 99 (99.0) |
| 1 | 3 (2.9) | 1 (1.0) |
3.2.2. Utility measures
Mean QALYs at eight weeks were also similar for both groups (0.103 vs. 0.109), with a differential mean QALY favouring the intervention group of 0.006 (95% credibility intervals = − 0.002 to 0.015) (Table 4).
Table 4.
Cost utility figures for 8 week follow-up period
| Mean cost (£) (SD) | QALY (SD) | ||
|---|---|---|---|
| Control | n = 104 22.37 (6.7) | n = 94 0.103 (0.003) | |
| Intervention | n = 100 24.10 (6.9) | n = 88 0.109 (0.003) | |
| 95% CrI | |||
| Cost (£) | Diff intervention-control | 1.73 | − 17.73–20.63 |
| QALY | Diff intervention-control | 0.006 | − 0.002–0.015 |
| ICER (£/QALY) | £288.33 |
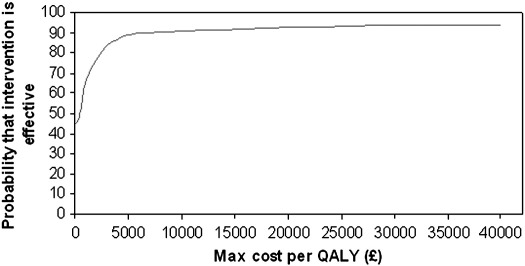
3.2.3. Cost effectiveness analysis
Data indicate that the intervention produced, on average, greater QALYs of 0.006 and that the intervention cost had slightly increased cost implications of £1.73. This corresponds to an ICER (i.e. differential cost/differential QALY) of £288.33. From the 95% credibility intervals (CrI) it can be seen that there is uncertainty around this estimate, however, the cost effectiveness acceptability curve (Fig. 2) suggests there is > 90% probability that a cost per QALY of < 30 k is achieved, thus the intervention is very likely to be considered cost effective in terms of £ per QALY.
Fig. 2.
Cost effectiveness acceptability curve.
4. Discussion
The programme did not provide all of the benefits we had hypothesised, specifically; days in hospital and anxiety were not reduced. The study did not reach the sample size suggested by the power analysis, and therefore may have been underpowered to show differences. This may have been particularly so for the length of hospital stay, as the effect size in Arthur et al.'s study [8] was atypically large. The probable reason why sample size was not reached was because the waiting times for heart surgery fell rapidly during the recruitment period, following a government initiative. Immediately prior to the study commencing, waiting times of over 6 months for non-urgent surgery were common. As the study concluded, the waiting times had fallen to 3 months. Taking into account the time it takes to recruit people, this may have reduced their motivation to participate, as surgery would seem close.
Arthur et al.'s exercise programme, which reduced days in hospital, was aimed at improving cardiovascular fitness [8]. Another possibility for the lack of effect on length of hospital stay in the study reported here, where exercise was based on daily walks, is that the programme was not intensive enough to increase fitness to the point where it could affect recovery time. It should be noted that the small numbers of adverse events during the preoperative period demonstrates the safety of such a (graded) walking programme for patients awaiting surgery. In future a more intensive home-based exercise programme might be tried. It should also be noted that the patients recruited for this study were people on a non-urgent list, which limits the applicability of the study to more complex patients. However, it is possible that more complex patients could benefit from the programme, as the exercise component was based on individual prescription through setting patient-centred goals.
The HeartOp Programme did not affect anxiety whilst having a positive effect on depression which may be thought unusual; the two are usually moderately related and change together [26]. It may be that the fact that patients were very close to the time of the operation meant that the intervention was swamped by the normal fears most patients have at this time. In part confirmation of this viewpoint, Arthur et al. also reported that their intervention had no effect preoperatively on anxiety [8], despite their intervention being compared with routine (no intervention) care.
The HeartOp programme did show positive effects preoperatively on depression and physical functioning, although the differences were small. It may be that changing the patient's misconceptions about heart disease, which is not part of usual nurse education procedures but which is a core component of the HeartOp Programme, helped. Many people with heart disease have misconceptions about their illness and how to cope with it. It has been found that people with heart disease who hold a number of common misconceptions are more anxious, depressed and physically limited [15,27], and that change in the number of misconceptions that people with angina hold is a greater predictor of physical functioning one year later than change in the frequency of angina.[14] These relationships between beliefs and outcome can be explained by Leventhal's Common Sense Model of Illness Behaviour [28], in which it is theorised that people build cognitive representations of their illness which engenders an emotional response. These parallel processes cause the adoption of certain coping behaviours which the person then appraises to assess their outcome. In this model, cardiac misconceptions can cause undue anxiety which provokes the adoption of avoidance coping with the consequence that fitness is lost and physical functioning reduced. The York Cardiac Beliefs Questionnaire is undergoing further testing at present in order to determine whether there are specific misconceptions about heart disease that predict poor outcome.
The significant differences between the two interventions were not maintained post-operatively. This is understandable as all patients who survived operation received a programme of advice about self-management during the immediate post-operative period, and all were offered a place (with a 74% take-up) on a post-operative cardiac rehabilitation programme. Thus the majority of patients received rehabilitation interventions with a similar focus to the HeartOp Plan in the post-operative period. As the benefits of cardiac rehabilitation are well-documented (for example, see the meta-analysis by Taylor et al. [29]), it is not surprising that differences between the groups were not maintained. There is a potential that delivering prehabilitation to all patients awaiting cardiac surgery may offset some of the problems of people not accessing cardiac rehabilitation post-operatively. The uptake of post-operative cardiac rehabilitation in this study was well above that documented in a recent audit of UK cardiac rehabilitation programmes [30], and therefore it was not possible to assess the effect of the programme on people who do not attend post-operative rehabilitation. Further research is needed to assess this potential.
The HeartOp Programme appears to add worthwhile and cost effective benefits to a regime of nurse counselling and phone calls for patients awaiting coronary artery bypass surgery, and can be recommended as an additional tool for nurses working with patients in the pre-surgery period. The training to successfully facilitate the HeartOp Plan could be based on that used for a similar programme for people with angina — the Angina Plan. This training is delivered entirely by distance learning in a programme which takes between a week and a few months to complete — depending on the motivation of the student. This method has successfully trained over 800 facilitators, mainly in the UK but with some from countries across the world.
Acknowledgements
The cardiothoracic surgeons: Michael Cowen, Alex Cale, Stephen Griffin, Levant Guvendik; cardiologist: John Caplin; and local steering group members: Margaret Argent, Nicola Beaumont, Alan Fussey, Carol Hargreaves, Kirsteen Hasney, Jenny Rumsby, Anita Trotman Beasty are gratefully acknowledged.
Footnotes
This study was supported by a British Heart Foundation Project Grant (number PG/02/160/14787). Included in this support were GF's and 50% of KI's salary for the duration of the study, and for statistical and economic analysis support by JNVM and JCD.
Contributions to the study and manuscript: GF and RJPL designed the interventions; GF, RJPL and DT devised the study protocol and gained grant funding; GF and KI ran the study; JNVM and JCD undertook the analysis. All authors contributed to the final manuscript. The University of York acted as guarantor and sponsor for the study.
References
- 1.Bengtson A., Herlitz J., Karlsson T., Hjalmarson A. Distress correlates with the degree of chest pain: a description of patients awaiting revascularisation. Heart. 1996;75:257–260. doi: 10.1136/hrt.75.3.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Koivula M., Paunonen-Ilomen M., Tarkka M.-T., Tarkka M., Laippala P. Fear and anxiety in patients awaiting coronary artery bypass grafting. Heart Lung. 2001;30:302–311. doi: 10.1067/mhl.2001.116134. [DOI] [PubMed] [Google Scholar]
- 3.Sampalis J., Boukas S., Liberman M., Reid T., Dupuis G. Impact of waiting time on the quality of life of patients awaiting coronary artery bypass grafting. Can Med Assoc J. 2001;165:429–433. [PMC free article] [PubMed] [Google Scholar]
- 4.Underwood M.J., Firmin R.K., Jehu D. Aspects of psychological and social morbidity in patients awaiting coronary artery bypass grafting. Br Heart J. 1993;69:382–384. doi: 10.1136/hrt.69.5.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lewin B., Robertson I.H., Cay E.L., Irving J.B., Campbell M. Effects of self-help post-myocardial-infarction rehabilitation on psychological adjustment and use of health services. Lancet. 1992;339:1036–1040. doi: 10.1016/0140-6736(92)90547-g. [DOI] [PubMed] [Google Scholar]
- 6.Lewin R.J.P., Furze G., Robinson J. A randomised controlled trial of a self-management plan for patients with newly diagnosed angina. Br J Gen Pract. 2002;52:194–201. [PMC free article] [PubMed] [Google Scholar]
- 7.McHugh F., Lindsay G.M., Hanlon P. Nurse led shared care for patients on the waiting list for coronary artery bypass surgery: a randomised controlled trial. Heart. 2001;86:317–323. doi: 10.1136/heart.86.3.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arthur H.M., Daniels C., McKelvie R., Hirsh J., Rush B. Effect of a preoperative intervention on preoperative and postoperative outcomes in low-risk patients awaiting elective coronary artery bypass graft surgery. A randomized, controlled trial. Ann Intern Med. 2000;133:253–262. doi: 10.7326/0003-4819-133-4-200008150-00007. [DOI] [PubMed] [Google Scholar]
- 9.Daly J., Sindone A.P., Thompson D.R., Hancock K., Chang E., Davidson P. Barriers to participation in and adherence to cardiac rehabilitation programs: a critical review. Prog Cardiovasc Nurs. 2002;17:8–17. doi: 10.1111/j.0889-7204.2002.00614.x. [DOI] [PubMed] [Google Scholar]
- 10.Jolly K., Taylor R.S., Lip G.Y.H., Stevens A. Home-based cardiac rehabilitation compared with centre-based rehabilitation and usual care: a systematic review and meta-analysis. Int J Cardiol. 2006;111(3):343–351. doi: 10.1016/j.ijcard.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 11.The Criteria Committee of the New York Heart Association. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. 9th Edition. Boston: Little, Brown and Company 1994.
- 12.Campeau L. Grading of angina pectoris. Circulation. 1976;52:522–523. [PubMed] [Google Scholar]
- 13.Petrella R.J., Koval J.J., Cunningham D.A., Paterson D.A. A self-paced step test to predict aerobic fitness in older adults in the primary care clinic. J Am Geriatr Soc. 2001;49:632–638. doi: 10.1046/j.1532-5415.2001.49124.x. [DOI] [PubMed] [Google Scholar]
- 14.Furze G., Lewin R., Murberg T.A., Bull P., Thompson D. Does it matter what patients think? The relationship between changes in patients' beliefs about angina and their psychological and functional status. J Psychosom Res. 2005;59:323–329. doi: 10.1016/j.jpsychores.2005.06.071. [DOI] [PubMed] [Google Scholar]
- 15.Maeland J.G., Havik O.E. Measuring cardiac health knowledge. Scand J Caring Sci. 1987;7:23–31. doi: 10.1111/j.1471-6712.1987.tb00296.x. [DOI] [PubMed] [Google Scholar]
- 16.Spielberger CD, Gorusch RL, Lushene RE. State-trait anxiety inventory. Palo Alto, California: Consulting Psychologists Press 1970.
- 17.Grossi G., Perski A., Feleke E., Jakobson U. State anxiety predicts poor psychosocial outcome after coronary bypass surgery. Int J Behav Med. 1998;5(1):1–16. doi: 10.1207/s15327558ijbm0501_1. [DOI] [PubMed] [Google Scholar]
- 18.Hare D.L., Davis C.R. Cardiac Depression Scale: validation of a new depression scale for cardiac patients. J Psychosom Res. 1996;40:379–386. doi: 10.1016/0022-3999(95)00612-5. [DOI] [PubMed] [Google Scholar]
- 19.Lewin R.J.P., Thompson D.R., Martin C.R. Validation of the Cardiovascular Limitations and Symptoms Profile (CLASP) in chronic stable angina. J Cardpulm Rehabil. 2002;22:184–191. doi: 10.1097/00008483-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Brazier J., Jones N., Kind P. Testing the validity of the Euroqol and comparing it with the SF-36 Health Survey questionnaire. Qual Life Res. 1993;2:169–180. doi: 10.1007/BF00435221. [DOI] [PubMed] [Google Scholar]
- 21.Spiegelhalter D.J., Thomas A., Best N.G. Cambridge: MRC Biostatistics Unit; 1999. WinBUGS version 1.4 user manual. [Google Scholar]
- 22.Netten A., Dennett J., Knight J. University of Kent at Canterbury; Canterbury: 2004. Unit costs of health and social care. PSSRU. [Google Scholar]
- 23.The Chartered Institute of Public Finance and Accountancy (CIPFA). The Health Service Database 2002-03. Croyden: CIFPA 2003.
- 24.National Institute for Clinical Excellence. Guide to methods of technology appraisal. London: NICE; 2004. [PubMed]
- 25.Cohen J. Erlbaum; Hillsdale, NJ: 1988. Statistical power analysis for the behavioral sciences. [Google Scholar]
- 26.Watson D., Clark L.A., Weber K., Assenheimer J.S., Strauss M.E., McCormick R.A. Testing a tripartite model: II. Exploring the symptom structure of anxiety and depression in student, adult and patient samples. J Abnorm Psychol. 1995;104:15–25. doi: 10.1037//0021-843x.104.1.15. [DOI] [PubMed] [Google Scholar]
- 27.Furze G., Bull P., Lewin R., Thompson D.R. Development of the York angina beliefs questionnaire. J Health Psychol. 2003;8:307–316. doi: 10.1177/13591053030083002. [DOI] [PubMed] [Google Scholar]
- 28.Leventhal H., Benyamini Y., Brownlee S. Illness representations: theoretical foundations. In: Petrie K.J., Weinman J.A., editors. Perceptions of health and illness. Harwood Academic Publishers; Amsterdam: 1997. pp. 19–45. The Netherlands. [Google Scholar]
- 29.Taylor R.S., Brown A., Ebrahim S. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. The American Journal of Medicine. 2004;116(10):682–692. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 30.Lewin RJP for the National Audit Team of the British Heart Foundation Care & Education Research Group. The National Audit of Cardiac Rehabilitation: Annual Statistics Report 2007. London, BHF. 2007.